Abstract
Children surviving premature birth have a high risk of cognitive and learning disabilities and attention deficit. In turn, adverse outcomes are associated with persistent reductions in cerebral growth on magnetic resonance imaging (MRI). It is striking that modern care has been associated with a dramatic reduction in the risk of cystic white matter damage, but modest improvements in terms of neurodevelopmental impairment. This review will explore the hypothesis that the disability is primarily associated with impaired neural connectivity rather than cell death alone. Very preterm infants exhibit reduced thalamocortical connectivity and cortical neuroplasticity compared with term-born controls. In preterm fetal sheep, moderate cerebral ischemia with no neuronal loss, but significant diffuse failure of maturation of cortical pyramidal neurons, was associated with impaired dendritic growth and synapse formation, consistent with altered connectivity. These changes were associated with delayed decline in cortical fractional anisotropy (FA) on MRI. Supporting these preclinical findings, preterm human survivors showed similar enduring impairment of microstructural development of the cerebral cortex defined by FA, consistent with delayed formation of neuronal processes. These findings offer the promise that better understanding of impairment of neural connectivity may allow us to promote normal development and growth of the cortex after preterm birth.
Similar content being viewed by others
Main
Premature birth is one of the leading causes of morbidity and mortality. Approximately 6–13% of all births are preterm (1), and in the United States, this has been estimated to cost the community more than $26.2 billion in 2005 alone (1). Most of this cost is related not to acute care but to cerebral palsy and long-term neurodevelopmental disability in surviving very premature (≤30 wk gestation) infants. Disability is highly associated with greater prematurity (2,3), but even in “late preterm” infants at 34–36 wk gestation, the risks of injury and disability are increased sevenfold or more compared with term infants (4). Although there is evidence for modest overall improvements in survival without disability in recent cohorts (2,3), others found no apparent improvement in disability after extremely preterm (<25 wk gestation) birth (5).
Historically, preterm human autopsy cases typically showed severe necrotic white matter injury (WMI) with evidence of axonal degeneration and loss of cortical neurons (6,7). This necrosis in turn was associated with cerebral palsy. The greater risk of long-term disability in boys is correlated with greater risk of WMI (8). Encouragingly, there is now evidence of a progressive reduction in the severest form of cystic WMI over time (9). In modern cohorts, severe WMI is seen in only ˜1% of cases, whereas less severe (nonnecrotic), diffuse WMI is now common (9,10).
It is striking that despite this apparent marked reduction in the severity of WMI, that even less severe forms of WMI injury are associated with impaired brain development and disability (10). Preterm survivors have a high risk of neurobehavioral disturbances and intellectual disabilities related to learning, cognition, visuospatial integration, attention deficit, and socialization (11,12,13). Given that the brain is still growing and maturing at this stage of life, we might predict that preterm infants would show a greater ability to return to normal (14). In marked contrast with this postulate, long-term follow-up up to 16 y of age shows that preterm infants without apparent neonatal brain injury show reduced verbal and performance intelligence quotient levels (11). Furthermore, modern imaging shows that preterm birth is associated with perturbations of the trajectory of cerebral development at least up to adolescence, with reduced thinning of the gray matter and reduced white matter growth (15), and evidence of long-lasting changes in connectivity (16).
These persistently adverse outcomes in the setting of diffuse WMI suggests the hypothesis that primary disturbances in neuronal processing may occur in multiple cortical and subcortical gray matter structures, in addition to disturbances in connectivity related to cerebral WMI. In the present review, we will critically dissect the underlying neuropathology of preterm brain injury, including the importance of acute white and gray matter damage in a subset of infants, the association of hypoxia–ischemia and infection/inflammation with adverse outcomes, the timing of injury, and the impact on the ability of the preterm brain to continue to develop after injury.
Timing and Etiology of Preterm Brain Injury
In historical cohorts, the major lesions associated with premature birth were cystic periventricular leukomalacia and unilateral periventricular–intraventricular hemorrhage. These severe lesions damaged the descending white matter tracts and were associated with chorioamnionitis, prolonged rupture of membranes, asphyxia, sepsis, hypocarbia, and in turn with the diplegic form of cerebral palsy (6). Both lesions have become much less common in modern cohorts. Periventricular–intraventricular hemorrhage in particular may be reduced by maternal glucocorticoid therapy (17).
Early imaging and postmortem data suggest that cerebral injury occurs in the immediate perinatal period in approximately two-thirds of cases, and an appreciable number of cases occur before the onset of labor; in contrast, injury after the early neonatal period represents only ˜10% of cases (18,19). Strongly consistent with this, acute electroencephalogram (EEG) abnormalities are reported in the early perinatal period in the majority of infants and were highly predictive of long-term outcome (20). The precise etiology of injury remains surprisingly unclear; however, it is likely to involve both hypoxia–ischemia and infection/inflammation (6).
Acute, profound asphyxia occurs in a small minority of premature births (21) and so cannot possibly account for the overall burden of disability after preterm birth. Nevertheless, there is some evidence for a role of subtle insults, as shown, e.g., by depressed Apgar scores at birth (22). More recently, the Extremely Low Gestational Age Newborns (ELGAN) study reported that severe intrauterine growth restriction and evidence of placental vascular thrombosis consistent with long-standing, prenatal hypoxemia were associated with impaired neurodevelopmental outcome at 2 y of age (23). After birth, although low blood pressure is common, the evidence for an association between hypotension and adverse outcomes is limited, as reviewed in ref. (24). The ELGAN study, for example, suggests that neither vasopressor treatment nor blood pressure in the lowest quartile for gestational age were independently associated with neurodevelopmental outcome (25).
There is increasing evidence that exposure to in utero infection at critical stages of brain development can significantly increase the risk of neurodevelopment abnormalities. As with asphyxia, although overt severe infection is strongly linked with neural injury, subclinical infection is more common and also highly associated with adverse outcomes (26). Clinical studies support a role for both prenatal and postnatal infection (27,28). For example, increased cord blood levels of tumor necrosis factor-α have been associated with depression of the EEG in the first few days of life, WMI on cranial ultrasound, and risk of handicap at 2 y of age (27). In the ELGAN study, although placental bacteria were not associated with neurodevelopmental outcome at 2 y of age (23), necrotizing enterocolitis, or bacteremia combined with ventilation on d 14 after birth were strongly associated with impaired development (29). Strikingly, the combination of intrauterine growth retardation with increased inflammatory markers in the first 2 wk of life was associated with greater increase in risk of severe neurodevelopmental impairment compared with either alone (30). These findings support that both hypoxia–ischemia and infection/inflammation impair brain development and may interact to increase damage.
The Pattern of Preterm Brain Damage in Modern Cohorts
Long-term follow-up studies using quantitative magnetic resonance imaging (MRI) show that preterm birth is associated with long-term reductions in cortical surface area, volume and folding, and reductions in volume of subcortical regions (31,32). Neurodevelopmental outcomes are independently correlated with both WMI and the magnitude of the gray matter deficits (32). Similarly, decreased caudate, cortical, and hippocampal volumes were correlated with lower intelligence quotient in preterm infants at 7–8 y of age (33,34), and reduced hippocampal volume correlated with some aspects of memory impairment in children in early adolescence (35).
After long-term follow-up of preterm infants from 4 to 6 y of age, neurocognitive impairment was associated with preceding WMI (and reductions in gray matter volumes), whereas children who had not had WMI appeared to have normal neurocognitive development (36). It is unclear whether this relationship reflected a direct effect of WMI on cortical development or some common mechanism affecting both the white and the gray matter. Prematurely born children who had no overt neonatal WMI were reported to have altered neural connectivity at 12 y of age on white matter diffusion tensor imaging and volumetric imaging compared with term controls (16). Further follow-up up to 16 y of age confirmed that the preterm children showed extensive changes in both microstructure and total cerebral white matter volume and that measures of language development were closely related to microstructural integrity (11). Intriguingly, whereas at 12 y, there were marked regional sex differences in fractional anisotropy (FA) measurements that correlated with verbal intelligence quotient and vocabulary measures, few sex effects were found at 16 y (11). Similarly, at 6 y of age, others found little effect of adjustment for sex on risk of performance impairments (36). It is likely that much larger cohorts will be required to disentangle the effects of sex and the risk of diffuse WMI at birth on long-term outcomes.
Does Acute Neuronal loss Contribute to Impaired Connectivity?
It is surprisingly unclear whether preterm birth is commonly associated with overt neuronal loss. Postmortem cases of infants dying in the early neonatal period show that at least the most severely affected infants have significant neuronal loss (19,37,38). MRI of preterm infants exposed to known severe perinatal hypoxia has demonstrated a consistent pattern of acute subcortical damage involving the thalamus and basal ganglia, in addition to cerebellar infarction combined with diffuse periventricular WMI, but sparing of the cortex (39).
Although now in the minority, infants with cystic WMI appear to have reduced numbers of cortical neurons compared with infants without cystic injury (7). Furthermore, a detailed postmortem analysis suggested that neuronal loss occurred in a third or more of cases of cystic WMI, whereas there was no apparent neuronal loss in infants with only chronic, noncystic WMI (40). Similarly, in human autopsy cases with acute noncystic diffuse WMI, few acutely degenerating cells were observed in the cerebral cortex in contrast to the situation in the cerebral white matter. A quantitative analysis of neuroprostanes, specific biomarkers of neuronal oxidative damage, found no evidence of acute neuronal degeneration in these cases (41). It is unclear whether this cortical deficit represents neuronal injury or a secondary consequence of white matter damage. Regardless, the evidence that infants with diffuse WMI have little neuronal loss supports the hypothesis that additional mechanisms are involved in impaired gray matter development.
Connectivity and the “Connectome”
A key area of modern research will be to understand how function relates to the changes in connectivity of the brain. A “connectome” is a map of neural connections in the brain and can be created by using advanced MRI-based tractography (42). Ball et al. recently reported that in term and preterm infants (median gestation at birth 28 wk), at term-equivalent age, there was a significant association between frontal and temporal lobe volumes and thalamic and cortical tissue reduction and the loss of microstructural integrity in the connective white matter tracts (43). Subsequent tractography demonstrated that connectivity between the thalamus and cortex was significantly reduced (44). Similarly, there was a close relationship between cerebellar injury in premature infants and subsequent reduced growth of the contralateral cerebral hemisphere by term-equivalent age (45). In a cross-sectional study, resting-state functional connectivity MRI demonstrated that term infants have strong resting-state networks involving the thalamus, sensorimotor cortex, brainstem, and cerebellar vermis, whereas preterm infants at term-equivalent age showed much more limited connections (46). Supporting these findings, recent evidence shows that both early and late premature birth were associated with reduced long-term depression-like responses to noninvasive transcranial magnetic brain stimulation in adolescence (47), consistent with impaired cortical neuroplasticity. Furthermore, prematurely born adolescents with MRI evidence of WMI showed reduced magnetoencephalographic brain activation over the right parietal cortex in response to specific stimuli (48), consistent with a link between early WMI and long-term altered cortical function.
Preclinical Evidence that Mild Cerebral Ischemia Impairs Brain Development
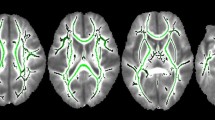
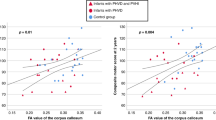
Late fetal human development is associated with a dramatic expansion of the cerebral cortex, at least in part due to prolific sprouting of neuronal dendrites, which in turn mediates the interconnection of neurons (49). Dean et al. recently found that reversible cerebral ischemia in preterm fetal sheep at 0.65 gestation, which did not cause acute neuronal loss, was associated with impaired expansion of the dendritic arbor and reduced synaptic density of cortical projection neurons in all cortical layers after 4 wk recovery (as illustrated in Figure 1 ) (50). Strikingly, these histological changes were associated with impairment of cortical growth and the normal maturational decline in cortical FA on ex vivo MRI scans. Mathematically, these changes in FA after ischemia were consistent with the changes in the growth of dendritic arbor of cortical pyramidal neurons compared with that in controls. These findings are in contrast with the finding in P3 rats that unilateral hypoxia–ischemia leads to markedly reduced FA in the ipsilateral injured cortex (51). This severe, focal insult causes infarction of the cortex in the territory of the middle cerebral artery, with disruption of the radial organization, whereas there is no overt cortical injury in the sheep model or in typical preterm brain injury in human infants (52).
Flow diagram outlining the hypothesized relationship between hypoxia and infection/inflammation in the developing brain and long-term reduction in regional brain growth. These mechanisms combine to reduce neuronal arborization (see examples taken 4 wk after sham control or hypoxia–ischemia (HI) studies in preterm fetal sheep (50)), leading to persistently impaired connectivity.
Supporting the findings in preterm sheep, human survivors of preterm birth show a similar delayed decline in cortical FA, consistent with impaired microdevelopment of cortical gray matter (53,54), whereas FA is reduced in white matter regions (16). The delayed maturational decline in cortical FA before 38 wk was proportional to the severity of prematurity and strongly associated both with impaired cortical growth and with neurodevelopmental outcomes at 2 y of age (54).
Preclinical Evidence that Mild/Chronic Systemic Inflammation Impairs Brain Development
There is strong evidence for a causal linkage between acute, severe exposure to lipopolysaccharide (LPS), a purified polysaccharide from the outer wall of Gram-negative bacteria, and impaired neural development. For example, acute intravenous exposure of preterm fetal sheep to LPS was associated with substantial white and gray matter injury (55), followed by impaired brain growth and loss of the normal maturational increase in cortical EEG amplitude 10 d later (56). However, as discussed above, such overt infection is relatively uncommon in preterm infants. Recently, we reported that a stable, low-dose infusion of LPS to preterm fetal sheep older than 5 d, which did not perturb fetal blood gases, carotid blood flow, or arterial blood pressure, still markedly impaired the maturation of the cortical EEG (57). LPS infusion was associated with loss of the normal maturational shift to higher-frequency EEG activity, with reduced alpha and beta power and increased delta power, compared with saline controls, from 6 to 10 d (i.e., after the end of the LPS infusion). This impaired cortical maturation developed in the presence of low-grade inflammation, with a transient increase in serum interleukin-6, induction of microglia, and greater expression of tumor necrosis factor-α positive cells in the frontoparietal cortex, consistent with the hypothesis that exposure to proinflammatory cytokines directly contributed to the EEG dysmaturation.
In vitro studies show that proinflammatory cytokines mediate synaptic dysfunction, in part indirectly through adenosine and gamma aminobutyric acid (58). These effects appear to be dose dependent, with synaptic inhibition at lower concentrations (59). Furthermore, tumor necrosis factor-α was reported to inhibit growth and branching of neurons in vitro, which could be reversed by tumor necrosis factor-α receptor blockade (60). Similarly, exposure to interferon-γ, an inflammatory marker that is induced by injury and many inflammatory conditions, is associated with both inhibition of initial dendritic outgrowth in culture and retraction of existing dendrites (61). Thus, it is highly plausible that chronic low levels of cerebral cytokines associated with infection, or with traumatic events such as ventilation, can reduce neural excitability and impair connectivity in the cortex. Further long-term studies are essential to confirm this hypothesis.
Synergy with other Insults: Sensitization and Tolerance
This apparent association between prenatal hypoxia and perinatal infection/inflammation may reflect a combined or even synergistic effect on neuronal development. There are parallels from experimental data in rodents that exposure to mild infection or inflammation can sensitize the brain so that short or milder periods of hypoxia–ischemia, which do not normally injure the developing brain, can in combination trigger severe damage (62). The effect is complex and time dependent. Nevertheless, recent data suggest that prenatal exposure to inflammation exacerbates ventilation-mediated brain injury (63), and thus it is highly plausible that multiple insults impair perinatal brain development.
Other Factors
Although this is not the focus of the present review, it is important to appreciate that neonatal care may also affect brain development. Likely factors include nutritional compromise (64), sedation (65), and the abnormal environment. For example, procedural pain has been associated with reduced subcortical gray matter N-acetylaspartate/choline ratio (a measure of neuronal viability) and white matter FA (66); however, other studies have reported that preemptive morphine infusions did not reduce the frequency of WMI and prolonged therapy may have had adverse effects (67). Glucocorticoids, whether exogenous or endogenously induced by stress, have profound effects on brain structure, including simplification of dendrites and shrinkage of dendritic spines (68). The relatively prolonged postnatal courses of glucocorticoid treatment used for lung maturation have been associated with greater risk of developmental delay and cerebral palsy (69). Furthermore, postnatal treatment with hydrocortisone (which has mixed glucocorticoid and mineralocorticoid effects) or dexamethasone was associated with impaired cerebellar growth, whereas antenatal maternal betamethasone was not associated with any change in infants’ cerebellar volume (70). These findings may contribute to at least part of the complexity of clinical outcomes.
What is the link between Cortical Maturation and WMI?
Cells are “social” beings, and their survival is tightly linked to extrinsic signals from neighboring cells and synaptic activity (71). Disruption of early contact between the cortex and thalamus may also disrupt connectivity and lead to remodeling of cortical circuitry due to target deprivation-induced (“Wallerian”) neurodegeneration (72). Nevertheless, although historical data demonstrate axonal injury within and around periventricular white matter necrosis (9), there does not appear to be significant axonal damage in nonnecrotic fetal ovine WMI (73). Similarly, in a postmortem cohort of preterm infants, axonal degeneration was only seen in necrotic foci, in association with microglial activation, but not in areas of diffuse WMI (9). Although microscopic necrosis and axonopathy did occur, they affected less than 5% of the area of the periventricular white matter. Rather, WMI was characterized by diffuse astrogliosis with expansion in the total population of oligodendrocyte progenitors, but reduced myelination, consistent with arrest of the maturation of oligodendrocytes. Buser et al. (9) speculated that acute preoligodendrocyte death may trigger diffuse astrogliosis, as part of the neuroinflammatory responses, leading to an aberrant regenerative response that contributes to an impaired maturation of oligodendrocytes and consequent reduced myelination, as illustrated in Figure 1 . This process may be mediated by inhibitory effects of astrogliosis and the induction of microglia through several mechanisms. These include inhibitory effects of hyaluronic acid and its digestion products on preoligodendrocyte maturation (74,75).
Hyaluronic acid digestion products likely act in concert with other signals in demyelinated lesions to prevent remyelination, many of which may be linked to reactive astrogliosis. For example, reactive astrocytes in spinal cord injuries increase their expression of bone morphogenetic proteins that inhibit oligodendrocyte progenitor cell differentiation, with concurrent promotion of astrocyte differentiation. Astrocyte-derived bone morphogenetic proteins inhibit oligodendrocyte progenitor differentiation with concurrent promotion of astrocyte differentiation (76). Similarly, the Notch ligand Jagged1 is elevated on reactive astrocytes in demyelinating lesions and activates Notch signaling on oligodendrocyte progenitors, preventing their maturation (77). Astrocytes also generate complement proteins that modulate synaptic pruning (78). Oligodendrocytes secrete trophic factors that influence the survival and function of neighboring neurons (79), enhance the number of functional synapses between neurons, and can directly regulate neuronal activity (80). Thus, impaired maturation of oligodendroglia may contribute to the impaired maturation of the developing gray matter and vice versa.
Conclusion
The most striking concept to emerge from recent clinical and experimental studies of the very immature brain has been that early WMI is associated with a reduction in cortical complexity and volume and, in turn, with neurodevelopmental impairment but that gray matter damage due to loss of connections—rather than cell loss—is also a major factor in long-term disability, as summarized in Figure 1 . Focused experimental and clinical studies are essential to dissect the relative contributions of these mechanisms to establish whether they are independent or synergistic, in addition to finding ways to reverse them or stimulate normal development. Advanced neuroimaging techniques now offer the opportunity to track the long-term impact on the preterm brain and to assess neurodevelopmental outcomes and thereby provide novel opportunities for early interventions.
Statement of Financial Support
The authors’ work reported in this review has been supported by the Health Research Council of New Zealand, Lottery Health Board of New Zealand, the Auckland Medical Research Foundation, the March of Dimes Birth Defects Foundation (to L.B., S.A.B.), the US National Institute of Neurological Disorders and Stroke (Bethesda, MD) grants 1RO1NS054044, R37NS045737-06S1/06S2 (to S.A.B.), and a Grant-in-Aid from the American Heart Association (to S.A.B.).
Disclosure:
The authors have no conflicts of interest to declare.
References
Committee on Understanding Premature Birth and Assuring Healthy Outcomes. Preterm Birth: Causes, Consequences, and Prevention. In: Behrman RE, Butler AS, eds. Washington, DC: Institute of Medicine of the National Academies, 2007. (http://books.nap.edu/openbook.php?record_id=11622&page=1.) Accessed 1 March 2013.
Moore T, Hennessy EM, Myles J, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. BMJ (Clinical research ed.) 2012;345:e7961.
Schlapbach LJ, Adams M, Proietti E, et al.; Swiss Neonatal Network & Follow-up Group. Outcome at two years of age in a Swiss national cohort of extremely preterm infants born between 2000 and 2008. BMC Pediatr 2012;12:198.
Baron IS, Erickson K, Ahronovich MD, Baker R, Litman FR . Cognitive deficit in preschoolers born late-preterm. Early Hum Dev 2011;87:115–9.
Hintz SR, Kendrick DE, Wilson-Costello DE, et al.; NICHD Neonatal Research Network. Early-childhood neurodevelopmental outcomes are not improving for infants born at <25 weeks’ gestational age. Pediatrics 2011;127:62–70.
Perlman JM . White matter injury in the preterm infant: an important determination of abnormal neurodevelopment outcome. Early Hum Dev 1998;53:99–120.
Andiman SE, Haynes RL, Trachtenberg FL, et al. The cerebral cortex overlying periventricular leukomalacia: analysis of pyramidal neurons. Brain Pathol 2010;20:803–14.
Rose J, Butler EE, Lamont LE, Barnes PD, Atlas SW, Stevenson DK . Neonatal brain structure on MRI and diffusion tensor imaging, sex, and neurodevelopment in very-low-birthweight preterm children. Dev Med Child Neurol 2009;51:526–35.
Buser JR, Maire J, Riddle A, et al. Arrested preoligodendrocyte maturation contributes to myelination failure in premature infants. Ann Neurol 2012;71:93–109.
Hamrick SE, Miller SP, Leonard C, et al. Trends in severe brain injury and neurodevelopmental outcome in premature newborn infants: the role of cystic periventricular leukomalacia. J Pediatr 2004;145:593–9.
Mullen KM, Vohr BR, Katz KH, et al. Preterm birth results in alterations in neural connectivity at age 16 years. Neuroimage 2011;54:2563–70.
Marlow N, Hennessy EM, Bracewell MA, Wolke D ; EPICure Study Group. Motor and executive function at 6 years of age after extremely preterm birth. Pediatrics 2007;120:793–804.
Rogers CE, Anderson PJ, Thompson DK, et al. Regional cerebral development at term relates to school-age social-emotional development in very preterm children. J Am Acad Child Adolesc Psychiatry 2012;51:181–91.
Kennard MA . Age and other factors in motor recovery from precentral lesions in monkeys. Am J Physiol 1936;115:138–46.
Ment LR, Kesler S, Vohr B, et al. Longitudinal brain volume changes in preterm and term control subjects during late childhood and adolescence. Pediatrics 2009;123:503–11.
Constable RT, Ment LR, Vohr BR, et al. Prematurely born children demonstrate white matter microstructural differences at 12 years of age, relative to term control subjects: an investigation of group and gender effects. Pediatrics 2008;121:306–16.
Bennet L, Davidson JO, Koome M, Gunn AJ . Glucocorticoids and preterm hypoxic-ischemic brain injury: the good and the bad. J Pregnancy 2012;2012:751694.
de Vries LS, Eken P, Groenendaal F, Rademaker KJ, Hoogervorst B, Bruinse HW . Antenatal onset of haemorrhagic and/or ischaemic lesions in preterm infants: prevalence and associated obstetric variables. Arch Dis Child Fetal Neonatal Ed 1998;78:F51–6.
Bell JE, Becher JC, Wyatt B, Keeling JW, McIntosh N . Brain damage and axonal injury in a Scottish cohort of neonatal deaths. Brain 2005;128(Pt 5):1070–81.
Kubota T, Okumura A, Hayakawa F, et al. Combination of neonatal electroencephalography and ultrasonography: sensitive means of early diagnosis of periventricular leukomalacia. Brain Dev 2002;24:698–702.
Low JA, Killen H, Derrick EJ . Antepartum fetal asphyxia in the preterm pregnancy. Am J Obstet Gynecol 2003;188:461–5.
Weinberger B, Anwar M, Hegyi T, Hiatt M, Koons A, Paneth N . Antecedents and neonatal consequences of low Apgar scores in preterm newborns: a population study. Arch Pediatr Adolesc Med 2000;154:294–300.
Helderman JB, O’Shea TM, Kuban KC, et al.; ELGAN study Investigators. Antenatal antecedents of cognitive impairment at 24 months in extremely low gestational age newborns. Pediatrics 2012;129:494–502.
Bennet L, Booth LC, Drury PP, Quaedackers JS, Gunn AJ . Preterm neonatal cardiovascular instability: does understanding the fetus help evaluate the newborn? Clin Exp Pharmacol Physiol 2012;39:965–72.
Logan JW, O’Shea TM, Allred EN, et al.; ELGAN Study Investigators. Early postnatal hypotension is not associated with indicators of white matter damage or cerebral palsy in extremely low gestational age newborns. J Perinatol 2011;31:524–34.
Wu YW, Colford JM Jr . Chorioamnionitis as a risk factor for cerebral palsy: a meta-analysis. JAMA 2000;284:1417–24.
Wikström S, Ley D, Hansen-Pupp I, Rosén I, Hellström-Westas L . Early amplitude-integrated EEG correlates with cord TNF-alpha and brain injury in very preterm infants. Acta Paediatr 2008;97:915–9.
Stoll BJ, Hansen NI, Adams-Chapman I, et al.; National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004;292:2357–65.
O’Shea TM, Shah B, Allred EN, et al.; ELGAN Study Investigators. Inflammation-initiating illnesses, inflammation-related proteins, and cognitive impairment in extremely preterm infants. Brain Behav Immun 2013;29:104–12.
Leviton A, Fichorova RN, O’Shea TM, et al.; ELGAN Study Investigators. Two-hit model of brain damage in the very preterm newborn: small for gestational age and postnatal systemic inflammation. Pediatr Res 2013;73:362–70.
Rathbone R, Counsell SJ, Kapellou O, et al. Perinatal cortical growth and childhood neurocognitive abilities. Neurology 2011;77:1510–7.
Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE . Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med 2006;355:685–94.
Abernethy LJ, Cooke RW, Foulder-Hughes L . Caudate and hippocampal volumes, intelligence, and motor impairment in 7-year-old children who were born preterm. Pediatr Res 2004;55:884–93.
Isaacs EB, Edmonds CJ, Chong WK, Lucas A, Morley R, Gadian DG . Brain morphometry and IQ measurements in preterm children. Brain 2004;127(Pt 12):2595–607.
Giménez M, Junqué C, Narberhaus A, et al. Hippocampal gray matter reduction associates with memory deficits in adolescents with history of prematurity. Neuroimage 2004;23:869–77.
Woodward LJ, Clark CA, Bora S, Inder TE . Neonatal white matter abnormalities an important predictor of neurocognitive outcome for very preterm children. PLoS ONE 2012;7:e51879.
Felderhoff-Mueser U, Rutherford MA, Squier WV, et al. Relationship between MR imaging and histopathologic findings of the brain in extremely sick preterm infants. AJNR Am J Neuroradiol 1999;20:1349–57.
Takizawa Y, Takashima S, Itoh M . A histopathological study of premature and mature infants with pontosubicular neuron necrosis: neuronal cell death in perinatal brain damage. Brain Res 2006;1095:200–6.
Barkovich AJ, Sargent SK . Profound asphyxia in the premature infant: imaging findings. AJNR Am J Neuroradiol 1995;16:1837–46.
Pierson CR, Folkerth RD, Billiards SS, et al. Gray matter injury associated with periventricular leukomalacia in the premature infant. Acta Neuropathol 2007;114:619–31.
Back SA, Luo NL, Mallinson RA, et al. Selective vulnerability of preterm white matter to oxidative damage defined by F2-isoprostanes. Ann Neurol 2005;58:108–20.
Tymofiyeva O, Hess CP, Ziv E, et al. Towards the “baby connectome”: mapping the structural connectivity of the newborn brain. PLoS ONE 2012;7:e31029.
Ball G, Boardman JP, Rueckert D, et al. The effect of preterm birth on thalamic and cortical development. Cereb Cortex 2012;22:1016–24.
Ball G, Boardman JP, Aljabar P, et al. The influence of preterm birth on the developing thalamocortical connectome. Cortex 2013;49:1711–21.
Limperopoulos C, Chilingaryan G, Guizard N, Robertson RL, Du Plessis AJ . Cerebellar injury in the premature infant is associated with impaired growth of specific cerebral regions. Pediatr Res 2010;68:145–50.
Smyser CD, Inder TE, Shimony JS, et al. Longitudinal analysis of neural network development in preterm infants. Cereb Cortex 2010;20:2852–62.
Pitcher JB, Riley AM, Doeltgen SH, et al. Physiological evidence consistent with reduced neuroplasticity in human adolescents born preterm. J Neurosci 2012;32:16410–6.
Pavlova M, Marconato F, Sokolov A, Braun C, Birbaumer N, Krägeloh-Mann I . Periventricular leukomalacia specifically affects cortical MEG response to biological motion. Ann Neurol 2006;59:415–9.
de Graaf-Peters VB, Hadders-Algra M . Ontogeny of the human central nervous system: what is happening when? Early Hum Dev 2006;82:257–66.
Dean JM, McClendon E, Hansen K, et al. Prenatal cerebral ischemia disrupts MRI-defined cortical microstructure through disturbances in neuronal arborization. Sci Transl Med 2013;5:168ra7.
Sizonenko SV, Camm EJ, Garbow JR, et al. Developmental changes and injury induced disruption of the radial organization of the cortex in the immature rat brain revealed by in vivo diffusion tensor MRI. Cereb Cortex 2007;17:2609–17.
Back SA, Riddle A, Dean J, Hohimer AR . The instrumented fetal sheep as a model of cerebral white matter injury in the premature infant. Neurotherapeutics 2012;9:359–70.
Vinall J, Grunau RE, Brant R, et al. Slower postnatal growth is associated with delayed cerebral cortical maturation in preterm newborns. Sci Transl Med 2013;5:168ra8.
Ball G, Srinivasan L, Aljabar P, et al. Development of cortical microstructure in the preterm human brain. Proc Natl Acad Sci USA 2013;110:9541–6.
Mallard C, Welin AK, Peebles D, Hagberg H, Kjellmer I . White matter injury following systemic endotoxemia or asphyxia in the fetal sheep. Neurochem Res 2003;28:215–23.
Dean JM, van de Looij Y, Sizonenko SV, et al. Delayed cortical impairment following lipopolysaccharide exposure in preterm fetal sheep. Ann Neurol 2011;70:846–56.
Keogh MJ, Bennet L, Drury PP, et al. Subclinical exposure to low-dose endotoxin impairs EEG maturation in preterm fetal sheep. Am J Physiol Regul Integr Comp Physiol 2012;303:R270–8.
Hellstrom IC, Danik M, Luheshi GN, Williams S . Chronic LPS exposure produces changes in intrinsic membrane properties and a sustained IL-beta-dependent increase in GABAergic inhibition in hippocampal CA1 pyramidal neurons. Hippocampus 2005;15:656–64.
Luk WP, Zhang Y, White TD, et al. Adenosine: a mediator of interleukin-1beta-induced hippocampal synaptic inhibition. J Neurosci 1999;19:4238–44.
Summers deLuca L, Gommerman JL . Fine-tuning of dendritic cell biology by the TNF superfamily. Nat Rev Immunol 2012;12:339–51.
Kim IJ, Beck HN, Lein PJ, Higgins D . Interferon gamma induces retrograde dendritic retraction and inhibits synapse formation. J Neurosci 2002;22:4530–9.
Eklind S, Mallard C, Arvidsson P, Hagberg H . Lipopolysaccharide induces both a primary and a secondary phase of sensitization in the developing rat brain. Pediatr Res 2005;58:112–6.
Polglase GR, Miller SL, Barton SK, et al. Initiation of resuscitation with high tidal volumes causes cerebral hemodynamic disturbance, brain inflammation and injury in preterm lambs. PLoS ONE 2012;7:e39535.
Gibson A, Carney S, Wales JK . Growth and the premature baby. Horm Res 2006;65 Suppl 3:75–81.
Ng E, Taddio A, Ohlsson A . Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev 2012;6:CD002052.
Brummelte S, Grunau RE, Chau V, et al. Procedural pain and brain development in premature newborns. Ann Neurol 2012;71:385–96.
Anand KJ, Hall RW, Desai N, et al.; NEOPAIN Trial Investigators Group. Effects of morphine analgesia in ventilated preterm neonates: primary outcomes from the NEOPAIN randomised trial. Lancet 2004;363:1673–82.
Tanokashira D, Morita T, Hayashi K, et al. Glucocorticoid suppresses dendritic spine development mediated by down-regulation of caldesmon expression. J Neurosci 2012;32:14583–91.
Halliday HL, Ehrenkranz RA, Doyle LW . Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 2010:CD001146.
Tam EW, Chau V, Ferriero DM, et al. Preterm cerebellar growth impairment after postnatal exposure to glucocorticoids. Sci Transl Med 2011;3:105ra105.
Goldberg JL, Barres BA . The relationship between neuronal survival and regeneration. Annu Rev Neurosci 2000;23:579–612.
Molnár Z, Kurotani T, Higashi S, Yamamoto N, Toyama K . Development of functional thalamocortical synapses studied with current source-density analysis in whole forebrain slices in the rat. Brain Res Bull 2003;60:355–71.
Riddle A, Maire J, Gong X, et al. Differential susceptibility to axonopathy in necrotic and non-necrotic perinatal white matter injury. Stroke 2012;43:178–84.
Back SA, Tuohy TM, Chen H, et al. Hyaluronan accumulates in demyelinated lesions and inhibits oligodendrocyte progenitor maturation. Nat Med 2005;11:966–72.
Preston M, Gong X, Su W, et al. Digestion products of the PH20 hyaluronidase inhibit remyelination. Ann Neurol 2013;73:266–80.
Wang Y, Cheng X, He Q, et al. Astrocytes from the contused spinal cord inhibit oligodendrocyte differentiation of adult oligodendrocyte precursor cells by increasing the expression of bone morphogenetic proteins. J Neurosci 2011;31:6053–8.
John GR, Shankar SL, Shafit-Zagardo B, et al. Multiple sclerosis: re-expression of a developmental pathway that restricts oligodendrocyte maturation. Nat Med 2002;8:1115–21.
Chung WS, Barres BA . The role of glial cells in synapse elimination. Curr Opin Neurobiol 2012;22:438–45.
Dai X, Lercher LD, Clinton PM, et al. The trophic role of oligodendrocytes in the basal forebrain. J Neurosci 2003;23:5846–53.
Alvarez-Maubecin V, Garcia-Hernandez F, Williams JT, Van Bockstaele EJ . Functional coupling between neurons and glia. J Neurosci 2000;20:4091–8.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Dean, J., Bennet, L., Back, S. et al. What brakes the preterm brain? An arresting story. Pediatr Res 75, 227–233 (2014). https://doi.org/10.1038/pr.2013.189
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.189
This article is cited by
-
Oxygen toxicity: cellular mechanisms in normobaric hyperoxia
Cell Biology and Toxicology (2023)
-
Neuroprotective therapies in the NICU in preterm infants: present and future (Neonatal Neurocritical Care Series)
Pediatric Research (2023)
-
Tumor necrosis factor inhibition attenuates white matter gliosis after systemic inflammation in preterm fetal sheep
Journal of Neuroinflammation (2020)
-
Neuroinflammation in preterm babies and autism spectrum disorders
Pediatric Research (2019)
-
Altered white matter development in children born very preterm
Brain Structure and Function (2018)