Abstract
Many of the morbid conditions associated with extreme immaturity are potentiated by an excess of free radicals occurring in infants who developmentally have decreased levels of antioxidants. The optimal oxygen saturation values for the resuscitation, stabilization, and ongoing care of the very low birth weight infant remain largely undefined. We have reviewed the currently available evidence for clinical oxygen use in the newborn period. Until the results of further studies are available, a reasonable approach to resuscitation would include initial resuscitation with 30–40% oxygen for very preterm infants using targeted SpO2 values and blended oxygen during the first 10 min. For ongoing management of preterm infants, SpO2 targets of 85–93% seem to be most appropriate, with alarm limits set within 1 to 2% of these targets with intermittent audits to ensure compliance. There is no strong evidence to support the use of altered limits for the infant who develops early evidence of retinopathy of prematurity. Further prospective studies are required to evaluate the effects of varied oxygen targets on long-term outcome.
Similar content being viewed by others
Main
Oxygen is essential for adequate cellular functioning and highly specialized systems have developed to maintain a delicate balance during conditions of relatively low to high levels of oxygen availability. However, despite such sophisticated controls prolonged or severe exposures to both excessively low and high oxygen levels may lead to tissue damage. The fetus normally exists in an environment of relatively low oxygen exposure and the mechanisms for managing high oxygen levels are not yet completely developed. Preterm birth alters the natural environmental oxygen exposure at a developmental stage less well adapted to handling oxidative stress. For a more complete review of the physiology of hypoxia and hyperoxia, please refer to the review by Saugstad in this series. The disease processes associated with prematurity frequently necessitate oxygen therapy as a main component of care. The actual acceptable range of oxygen exposure and requirement is not known and may vary by developmental stage. The history of oxygen therapy in neonatology has been described by Silverman as “the albatross of neonatal medicine” (1). The therapeutic index for oxygen use seems to be much narrower than previously realized, and we have yet to define the optimal oxygen exposure for the most premature infants.
Currently available information suggests that many of the morbid conditions associated with extreme immaturity are potentiated by an excess of free radicals occurring in infants who developmentally have decreased levels of antioxidants. During hypoxia, metabolic alterations prime hypoxic cells to produce free oxygen radicals when subsequently exposed to oxygen. Such reperfusion injury, in addition to increasing the production of free oxygen radicals, is associated with other metabolic changes, which may produce long lasting harmful effects. Silvers et al. (2) reported that low plasma antioxidant activity at birth in premature infants was an independent risk factor for mortality. Pulmonary oxygen toxicity, through the generation of reactive oxygen/nitrogen species in excess of antioxidant defenses, is believed to be a major contributor to the development of bronchopulmonary dysplasia (BPD) (3–5). Varsila et al. (6) noted that immaturity is the most important factor explaining free radical-mediated pulmonary protein oxidation in premature newborn infants and that oxidation of proteins is related to the development of chronic lung disease.
Retinopathy of prematurity (ROP) remains a significant cause of morbidity among extremely preterm infants and its occurrence is inversely proportional to gestational age and duration of oxygen exposure. It is known that ROP is increased by the prolonged use of supplemental oxygen from observations published in the 1950s (7), but early trials were unable to pinpoint the actual level of arterial PacO2, which was the threshold for triggering the pathophysiology of this disorder (8). Flynn et al. (9) evaluated transcutaneous oxygen monitoring in preterm infants and found ROP more likely when TcO2 values were >80 mm Hg than when they were <80 mm Hg. Continuous monitoring has allowed more frequent titration of the oxygen concentration administered. Pulse oximetry is currently the more commonly used method of continuous monitoring but values can be difficult to interpret because the correlation between SpO2 and PacO2 is dependent on the affinity of Hb for oxygen in various physiologic circumstances. The composition of the infant's Hb will affect these values such that the greater the amount of fetal Hb, the higher the SpO2 for any given PacO2 value (10). Castillo et al. reported the relationship between actual PacO2 and SpO2 values in preterm infants and found that for oxygen saturation values between 85 and 93%, the mean measured PacO2 was 56 ± 14.7 mm Hg. Within this SpO2 range, 86.8% of the samples had PacO2 values of 40 to 80 mm Hg, 8.6% had values of <40 mm Hg, and 4.6% had values of >80 mm Hg. When the SpO2 was >93% the mean PacO2 was 107.3 ± 59.3 mm Hg with 59.5% of values >80 mm Hg (11).
The hospitalized preterm infant has three distinct periods, which must be considered in the evaluation of oxygen use and monitoring techniques. These periods include the immediate transitional period after birth, the acute phase of preterm neonatal illness, and the recovery phase of neonatal illness. Clinical trials have provided information about supplemental oxygen use during resuscitation immediately after birth and during the recovery phase of preterm illness. Currently available information about risk of disease with different oxygenation levels during the acute illness comes from retrospective reviews of practice.
NEONATAL TRANSITION
The immediate period of transition from fetal to neonatal life requires a unique adjustment from lower to higher environmental oxygen exposure. Traditionally pure oxygen has been used as the primary gas administered with ventilation during resuscitation. With accumulating evidence suggesting that free radical exposure was linked with serious chronic disease states, studies began to challenge the assumption that 100% oxygen was the ideal resuscitating gas. Saugstad hypothesized that the use of 100% oxygen could be detrimental during recovery from asphyxia as this time represents a vulnerable period for reperfusion injury. A number of animal investigations using asphyxiated piglets demonstrated that animals resuscitated with 21% oxygen were able to normalize blood pressure, heart rate, acid-base status, plasma and brain microdialysate hypoxanthine levels, cerebral blood flow, and somatosensory-evoked potentials as quickly as animals resuscitated with 100% oxygen (12–15).
The first clinical trial to compare room air with oxygen for neonatal resuscitation of depressed term infants concluded that room air was as effective as 100% oxygen in achieving successful resuscitation (16). Saugstad et al. subsequently reported the results of a multicenter international trial of 609 mostly term infants from 10 centers, the Resair 2 study. In this trial, 288 infants were resuscitated with room air and 321 infants were resuscitated with pure oxygen (17). The primary outcome measure, death within 7 d of life and/or moderate or severe hypoxic-ischemic encephalopathy was not significantly different between the groups, 21.2% in the room air group and in 23.7% in the oxygen group. There were no differences in resuscitation failures between the 21% oxygen and 100% oxygen groups. The median times to first breath and first cry were shorter in the room air group. This study suggested that asphyxiated newly born infants were not harmed by resuscitation with room air and might actual have a shorter time to recovery compared with those resuscitated with pure oxygen.
To further evaluate the clinical and biochemical effects of the oxygen concentration used during resuscitation, Vento et al. (18) randomized resuscitated infants to 21 or 100% oxygen and measured reduced and oxidized glutathione concentrations and antioxidant enzyme activities (superoxide dismutase, catalase, and glutathione peroxidase) in blood during the immediate transitional period and at 72 h and 4 wk's postnatal age. Consistent with the Resair 2 results, the room-air resuscitated group needed significantly less time to achieve the first cry and to achieve sustained spontaneous breathing than the group resuscitated with 100% oxygen. The reduced-to-oxidized glutathione ratio, an index of oxidative stress, of the room air group was similar to that seen in control nonresuscitated infants at 28 d of postnatal life. However, it was significantly lower in the 100% oxygen group and the activities of superoxide dismutase and catalase in erythrocytes were 69 and 78% higher demonstrating protracted oxidative stress in the oxygen group compared with control infants at 28 d of postnatal life. In additional studies, this group reported that glutathione peroxidase, glutathione reductase, and glutathione-s-transferase activities were significantly activated in an attempt to regenerate reduced glutathione especially in the pure oxygen group (19). More recently, they reported that the use of 100% oxygen was associated with higher plasma cardiac troponins and urinary N-acetyl-glucosaminidase levels reflecting myocardial and renal damage (20).
Several meta-analyses of the available room air resuscitation trials have been published (21–23). Saugstad et al. (24) reviewed 10 trials comparing the use of 21 versus 100% oxygen and reported that the relative risk of mortality was less when 21% oxygen rather than 100% oxygen was used as the resuscitation gas (typical RR 0.69, 95% CI 0.54–0.88). Frequent criticisms of these studies have included that some were quasi randomized with patient allocation by day of birth and that many were performed in the developing world where the overall mortality rate would be expected to be higher than in industrialized nations. Analysis of the studies that were all strictly randomized as opposed to quasi randomized showed that the reduction in mortality risk remained significant with a typical RR 0.32, (95% CI 0.12–0.84). These strictly randomized trials were all performed in Europe, mostly in Spain, suggesting that this finding was consistent in both developing and industrialized countries.
The evaluation of oxygenation in the minutes after birth has largely been through examination of color. Fetal arterial oxygen saturation levels are known to be lower than neonatal arterial oxygen saturation levels with an average of 50% in fetal lambs (25) and may be less than 30% in a stressed fetus. The first studies using fetal pulse oximetry demonstrated that the fetal SpO2 was approximately 58 ± 10% during labor (26). The rate of change from fetal to neonatal values after birth has been demonstrated by multiple investigators to be more gradual than previously believed with actual SpO2 values reaching the expected neonatal levels after 5–15 min of life (27–31). House et al. (32) reported that average oxygen saturation was 59% at 1 min, 68% at 2 min, 82% at 5 min, and 90% at 15 min. Oxygen saturation was less than 30% in 12 neonates and less than 50% in 26 neonates at some time during the 15-min monitoring period. In term infants, preductal SpO2 values have been reported to be approximately 5–10% higher than postductal values in the first 5 min of life (33,34). Mariani et al. (35) confirmed the presence of such gradients for the first 15 min of life. Rabi et al. (36) reported that infants delivered by cesarean delivery had a 3% lower SpO2 than infants delivered by vaginal delivery and took longer to reach a stable SpO2 ≥85%. At 5 min of age, vaginally delivered infants had an SpO2 of 87% (80–95%) versus 81% (75–83%) for infants delivered by cesarean section. Kamlin et al. (37) reported that infants of less than 37 wk who did not require resuscitation reached an SpO2 of 75% after 4.2 min, and an SpO2 of 90% at 6.5 min whereas these values were reached at 2.5 and 4.7 min for term infants. Figure 1 demonstrates the approximate average SpO2 levels after delivery, based on these observations.
Extremely preterm infants were not included in the trials of oxygen use for resuscitation or in the evaluation of normal oxygen saturation in the first minutes of life. Although preterm infants frequently require assisted ventilation in the immediate newborn period, they are not necessarily delivered from a compromised intrauterine environment. Therefore, the results of studies of different resuscitation gases on asphyxiated term infants may not be relevant to the preterm nonasphyxiated infant. To review trends of oxygen saturation in the first minutes of life in the extremely preterm population, we were able to review SpO2 data that was obtained as a part of the prospective delivery room continuous positive airway pressure study for infants enrolled at the University of California San Diego site (38). All infants were less than 28 wk gestation and were resuscitated with 100% oxygen. The mean SpO2 level was 91% at 3 min and 97% at 5 min, which were much higher than the average SpO2 levels seen in any of the observations of infants transitioning without resuscitation. These values were also higher than those of asphyxiated infants resuscitated with either 21 or 100% oxygen in the resuscitation trials.
Over the last 2 yr, three small prospective randomized trials have evaluated the use of variable oxygen concentrations for resuscitation of very preterm infants. Escrig et al. studied infants of younger than 28 wk in need of active resuscitation in the delivery room as determined by the presence of bradycardia ≤80 beats/min, hypotonia or hyporeactivity, and inability to sustain breathing. The infants were randomly assigned to receive either 90% oxygen or 30% oxygen as the initial resuscitation gas (39). The concentration of oxygen was then adjusted according to the infant's heart rate and SpO2, increased for bradycardia and decreased for SpO2 greater than 95%. Forty-two infants were enrolled and no differences were found between the groups in relation to the type of ventilation administered and time to attain clinical stabilization. Those in the 30% group were exposed to less oxygen during the resuscitation. Wang et al. (40) randomized infants of ≤32 wk gestation to receive 21% versus 100% oxygen as the initial resuscitation gas. A targeted approach to adjusting oxygen concentration based on SpO2 levels was used in the experimental (21%) group. If the targets of 70% at 3 min of life and 85% at 5 min of life were not achieved, the oxygen concentration was increased in 25% increments. The oxygen concentration was increased to 100% immediately for severe bradycardia. Infants in the control group were ventilated with 100% oxygen until 5 min of life when oxygen concentration was decreased if the SpO2 was ≥95%. Of the 41 enrolled infants, all 18 infants assigned to the experimental group required an increase in oxygen concentration at or before 3 min of life. Thus, no infant could be successfully resuscitated with room air. An additional trial compared three different oxygen delivery strategies during resuscitation. In this trial, Rabi et al. (Room air versus oxygen administration during resuscitation of preterm infants [ROAR Study]. 2008 PAS Annual Meeting, May 3–6, 2008 Honolulu, Hawaii, 5127.5) evaluated preterm infants of ≤32 wk gestation and randomized the 106 participants to one of the following groups: 100% oxygen throughout, 100% initial and titrated to SpO2, or 21% initial and titrated to SpO2. The target SpO2 was 85–92% and at the conclusion of resuscitation, both titrated groups were receiving similar oxygen concentrations: 33% (range, 27–39%) and 36% (range, 27–45%). This is consistent with the oxygen concentrations used at the conclusion of resuscitation in the Escrig and Wang trials.
A recent report of the change in clinical practice of a unit in Australia confirms the findings of these clinical trials. Dawson et al. (41) evaluated their unit's experience after changing from a policy of beginning resuscitation with 100% to beginning with 21% oxygen. The practice of this unit was to change from 21 to 100% oxygen if the SpO2 was ≤70% at 5 min of life, if the heart rate was below 100 beats/min after 60 s of ventilation or if chest compressions were initiated. Of the 106 preterm infants provided 21% oxygen from the start, 97 (92%) infants were given supplemental oxygen at some point in the resuscitation. The median SpO2 for these infants at 2 and 5 min of life was 31% and 54%, respectively, and increased to 81% at 6 min of life, once 100% oxygen was administered. Conversely, the 20 infants evaluated before the practice change (resuscitated with 100% oxygen) had median SpO2 values of 84% and 94% at 2 and 5 min of life, respectively. The eight infants successfully resuscitated with 21% oxygen had median SpO2 of 71 and 87% at 2 and 5 min of life, respectively. These studies of oxygen use in preterm infants during the transition to extrauterine life suggest that most preterm infants require supplemental oxygen to achieve expected oxygenation levels within the first 20 min of life. Preterm infants frequently require assistance with ventilation due to pulmonary immaturity and frequently require some supplemental oxygen. Pure oxygen is associated with hyperoxemia whereas room air is associated with oxygen levels which do not increase above fetal levels. Although the long-term consequences of such differences in oxygenation are not known it seems likely that neither 21% or 100% will be optimal. Therefore, the recommendation to titrate oxygen concentration levels to saturation targets in the first minutes of life seems both sensible and practical.
ACUTE PERIOD OF NEONATAL CARE
Many of the observations of oxygen saturation values evaluated unit practices during the first 4–8 wk of life. Tin et al. retrospectively reviewed outcomes for infants admitted to various neonatal intensive care units in northern England from 1990 to 1994 with different pulse oximetry alarm limit policies. Infants cared for in units with the highest (88–98%) alarm limit settings had four times higher risk of developing severe ROP than infants cared for in units with the lowest (70–90%) alarm limit settings (42). Additionally, those managed in units with higher alarm limits had a longer average numbers of days on the ventilator, 31.4 versus 13.9 d and higher percentages of infants treated with oxygen at 36 wk adjusted gestational age, 46 versus 18%. Infants managed with these differing alarm limit policies did not have any differences in risk of mortality or neurodevelopmental impairment.
In addition to different alarm limit settings, variation in practice may include different methods of adjusting the oxygen concentration in response to saturation values outside the desired range. Chow et al. (43) reported trends in the incidence of ROP before and after the institution of a detailed oxygen management policy. The policy specified strict criteria for changing oxygen concentration and monitoring saturation levels and encompassed the entire hospitalization period including time in delivery room and intrahospital transport. The main objectives were to avoid hyperoxemia and repeated episodes of hypoxia-hyperoxia in infants between 500 and 1500-g birth weight. After the implementation of these new management strategies the incidence of ROP Grades 3 to 4 decreased consistently in a 5-yr period from 12.5% in 1997 to 2.5% in 2001 and the need for ROP laser treatment decreased from 4.5% in 1997% to 0% in the last 3 yr. The policy included an SpO2 alarm limit range of 85 to 95% for infants >32 wk gestation at birth, and 85 to 93% for infants <32 wk. As with any evaluation in practice, a change over time without contemporaneous controls makes it unclear whether the observed reductions in ROP were related to the new policy or to overall changes in management that may have occurred during the study period. Although the observed decreases in ROP incidence are encouraging, the authors did not report the neurodevelopmental outcome for these infants. Using the same policy Deulofeut et al. (44) reported the neurodevelopmental follow-up of a cohort of infants ≤1250 g birth weight cared for with a target saturation range of 85–93% compared with historical controls (saturation alarm limits 92–100%). These investigators reported less oxygen use at 36 wk adjusted age, lower ROP of all stages but no difference in stages III or IV, and higher Mental Developmental Index scores on the Bayley II at 18 mo in the second cohort. However, nearly one third of the infants in this cohort were not old enough for developmental evaluation and therefore were not included in the follow-up data at the time of this review. Additional reports have described reductions in the incidence and severity of ROP in units that have instituted policies regarding oxygen administration and monitoring (45,46).
In 2001, Anderson et al. (47) surveyed directors of neonatal intensive care units in the United States regarding pulse oximetry practices and ROP rates. Among the 142 responding NICUs, 87% had a policy regarding saturation limits though a wide range of monitoring limits existed. They reported a lowered rate of ablative eye surgery in units that used lower maximal SpO2 limits, with the lowest incidence seen in units that had a maximum SpO2 of <92%. The success of any unit in maintaining and monitoring oxygenation depends on the individuals at the bedside making ongoing adjustments. Nghiem et al. (48) reported the results of a survey of over 2800 nurses in 59 NICUs and found that the setting of oxygen saturation alarm limits by an individual nurse caring for an extremely preterm infant was dependent of several factors: the presence of an NICU policy with specified saturation limits, nurse group opinion, and individual nurse opinions. The presence of a policy reduced the influence of individual nurse opinion on targeted pulse oximeter saturation limits and reduced variation among nurse target limits within NICUs. Clucas et al. performed a practice audit of alarm limit compliance. In this unit, preterm infants were to be managed with target SpO2 between 88 and 92%, and alarm limits set at 85 and 94% (49). For 144 preterm infants on oxygen, 1073 alarm limits were collected. The lower alarm limit was set correctly 91.1% of the time, whereas the upper alarm limit was set correctly only 23.3% of the time. The upper limit was set too high 76.5% of the time and 23.8% of the time it was set at 100%. Correctly set limits were more likely for infants with lower birth weight, gestational age, postmenstrual age, and postnatal age. Infants who required ventilation and higher inspired oxygen concentrations were also more likely to have a correctly set upper alarm limit.
Even if alarm limit policies are followed, it may not always be possible to achieve the desired oxygenation levels. Hagadorn et al. (50) enrolled 84 infants from 14 centers in three countries who were <28 wk gestation and ≤96 h of age in a prospective, multicenter cohort study. They collected oximetry data using masked oximeters for a 72-h period in each of the first 4 wk of life. Unit oxygen saturation policy limits ranged between 83 and 92% for lower limits and 92 and 98% for upper limits. The median pulse oximeter saturation level achieved was 95% for all infants requiring respiratory support. The center-specific median levels were within the intended range at 12 centers. Infants were maintained within the intended range 16 to 64% of the time and were above range 20 to 73% of the time. Achievement of desired targets was associated with wider target ranges, higher target upper range limits, policies that kept alarm limits within 1 to 2% of the desired range, and lower gestational age.
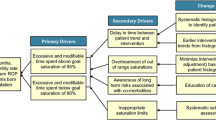
There have not been any completed prospective randomized trials, which have compared different SpO2 target ranges for the acute management of extremely preterm infants. However, there are trials currently enrolling patients intended to address this issue. One component of the ongoing SUPPORT trial compares two target ranges of SpO2, 85 to 89% versus 91 to 95% using specially developed masked oximeters, which display the SpO2 as 88 to 92% when the actual SpO2 is either 85 to 89% or 91 to 95% allowing care providers to be blinded to the targeted SpO2 range (the clinical protocol is available at http://clinicaltrials.gov/ct2/show/NCT00233324?term=neonatal+cpap&rank=7, Accessed Nov 3, 2008). A number of additional trials, which use the identical altered oximeters, will also evaluate the different SpO2 target ranges on the outcome of survival without ROP and survival without neurodevelopmental impairment at 2 yr of age. All of these trials have agreed to a prospective individual patient meta-analysis, which should provide a powerful assessment of the different SpO2 target ranges.
RECOVERY PERIOD OF PRETERM CARE
Trials that have prospectively randomized infants to different pulse oximeter saturation targets began randomization beyond the acute phase of preterm illness and were intended to determine whether higher saturation targets at that point would improve either ophthalmic outcome or growth and developmental outcomes. The STOP-ROP trial randomized infants with already established prethreshold retinopathy and an SpO2 less than 94% on room air to two ranges of SpO2 (89–94% versus 96–99%), for at least 2 wk and until both eyes were at study endpoints. The hypothesis was that increasing oxygenation at a time when retinopathy had already begun could inhibit vascular proliferation and therefore might decrease risk of further progression of the disease. The study enrolled 649 infants from 30 centers, 92% of whom completed ophthalmologic follow-up at 3 mo. The higher range of SpO2 was associated with a nonsignificant decrease in the progression of ROP, but was associated with a greater need for oxygen and more exacerbations of BPD (51). The subgroup of infants without plus disease did have a lower rate of progression to threshold disease with higher saturation targets (lower targets, 46% versus higher targets, 32%, p = 0.004). Another randomized trial compared SpO2 ranges of 91–94% versus 95–98% in 358 infants of less than 30 wk gestation who remained oxygen dependent at 32 wk (52). The purpose of this study was to test the hypothesis that increasing oxygenation would be beneficial to growth and development. The primary outcomes were growth and neurodevelopmental measures at a corrected age of 12 mo. The additional oxygen supplementation did not improve survival, growth, or the occurrence of cerebral palsy at 18 to 24 mo but resulted in an increased duration of oxygen supplementation. The high-saturation group received oxygen for a longer period after randomization (median, 40 d versus. 18 d; p < 0.001) and had a significantly higher rate of dependence on supplemental oxygen at 36 wk of postmenstrual age and a significantly higher frequency of home-based oxygen therapy. These studies suggest that the use of a high oxygen saturation target during the recovery phase of preterm illness does not have any obvious benefit with the possible exception of less progression of ROP for infants without plus disease. However, the cost of using such higher oxygen saturation targets includes an increased incidence and possibly severity of BPD.
CONCLUSIONS
In an effort to translate information from basic science and clinical research into clinical practice, the clinician must make judgments about how to apply various findings even when definitive answers are not available. Currently, the best information available would suggest the following approach to clinical practice.
For resuscitation of the preterm infant <32 wk, an initial oxygen concentration of 30–40% may be most appropriate until further evidence is available. During resuscitation, it is feasible to adjust the oxygen concentration to achieve a gradually increasing SpO2 over the first 10 min of life. Reasonable SpO2 targets during transition seem to be approximately 70% at 3 min of life and 80% at 5 min of life mimicking the values achieved by well transitioning infants. If an infant's SpO2 is lower and not increasing over several minutes, the resuscitation team should consider an increase in the concentration of oxygen.
For the ongoing management of preterm infants in the NICU who require oxygen, each unit should have agreed upon target range with alarm limits set close to this range and all staff should be aware of these values. Without the benefit of prospective trials during the acute phase of illness, an SpO2 target range of 85–93% seems most reasonable at this time. Intermittent audit of compliance with alarm limits and occasional review of the oximeter data sets may provide additional supportive information to help maintain and encourage appropriate monitoring limits. In addition, the presence of guidelines for the immediate response to intermittent desaturations including suggested increases in FiO2 may further reduce exposures to both low and high SpO2 values. Although there is some evidence that the use of a higher target in the recovery phase of preterm illness may be of value for infants with evidence of prethreshold ROP, this practice seems to increase pulmonary morbidity, which may outweigh any benefit. Further prospective studies are required to evaluate the long-term outcome of infants treated with different oxygen targeting strategies.
Abbreviations
- BPD:
-
bronchopulmonary dysplasia
- PaO2:
-
partial pressure of arterial oxygen tension
- ROP:
-
retinopathy of prematurity
- SpO2:
-
pulse oxygen saturation
- SUPPORT:
-
Surfactant Positive Airway Pressure and Pulse Oximetry Trial
- TcO2:
-
transcutaneous oxygen tension
References
Silverman WA 2004 A cautionary tale about supplemental oxygen: the albatross of neonatal medicine. Pediatrics 113: 394–396
Silvers KM, Gibson AT, Russell JM, Powers HJ 1998 Antioxidant activity, packed cell transfusions, and outcome in premature infants. Arch Dis Child Fetal Neonatal Ed 78: F214–F219
Saugstad OD 1997 Bronchopulmonary dysplasia and oxidative stress: are we closer to an understanding of the pathogenesis of BPD?. Acta Paediatr 86: 1277–1282
Luo XP, Jankov RP, Ning Q, Liao LJ, Tanswell AK 2002 Oxygen-mediated parenchymal and vascular lung injury. Acta Pharmacol Sin 23: 22–28
Davis JM 2002 Role of oxidant injury in the pathogenesis of neonatal lung disease. Acta Paediatr Suppl 91: 23–25
Varsila E, Pesonen E, Andersson S 1995 Early protein oxidation in the neonatal lung is related to development of chronic lung disease. Acta Paediatr 84: 1296–1299
Kinsey VE 1955 Etiology of retrolental fibroplasia and preliminary report of the Cooperative Study of Retrolental Fibroplasia. Trans Am Acad Ophthalmol Otolaryngol 59: 15–24
Kinsey VE, Arnold HJ, Kalina RE, Stern L, Stahlman M, Odell G, Driscoll JM, Elliott JH, Payne J, Patz A 1977 PaO2 levels and retrolental fibroplasia: a report of the cooperative study. Pediatrics 60: 655–668
Flynn JT, Bancalari E, Snyder ES, Goldberg RN, Feuer W, Cassady J, Schiffman J, Feldman HI, Bachynski B, Buckley E 1992 A cohort study of transcutaneous oxygen tension and the incidence and severity of ROP. N Engl J Med 326: 1050–1054
Shiao SY, Ou CN, Pierantoni H 2006 The measurement of accurate fetal hemoglobin and related oxygen saturation by the hemoximeter. Clin Chim Acta 374: 75–80
Castillo A, Sola A, Baquero H, Neira F, Alvis R, Deulofeut R, Critz A 2008 Pulse oxygen saturation levels and arterial oxygen tension values in newborns receiving oxygen therapy in the neonatal intensive care unit: is 85% to 93% an acceptable range?. Pediatrics 121: 882–889
Poulsen JP, Oyasaeter S, Saugstad OD 1993 Hypoxanthine, xanthine, uric acid in newborn pigs during hypoxemia followed by resuscitation with room air or 100% oxygen. Crit Care Med 21: 1058–1065
Rootwelt T, Loberg EM, Moen A, Oyasaeter S, Saugstad OD 1992 Hypoxemia and reoxygenation with 21% or 100% oxygen in newborn pigs: changes in blood pressure, base deficit, and hypoxanthine and brain morphology. Pediatr Res 32: 107–113
Rootwelt T, Odden J-P, Hall C, Saugstad OD 1993 Cerebral blood flow and evoked potentials during reoxygenation with 21% or 100% oxygen in newborn pigs. J Appl Physiol 75: 2054–2060
Solberg R, Andresen JH, Escrig R, Vento M, Saugstad OD 2007 Resuscitation of hypoxic newborn piglets with oxygen induces a dose-dependent increase in markers of oxidation. Pediatr Res 62: 559–563
Ramji S, Ahuja S, Thirupuram S, Rootwelt T, Rooth G, Saugstad OD 1993 Resuscitation of asphyxic newborn infants with room air or 100% oxygen. Pediatr Res 34: 809–812
Saugstad OD, Rootwelt T, Aalen O 1998 Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study. Pediatrics 102: E1
Vento M, Asensi M, Sastre J, Garcia-Sala F, Pallardo FV, Vina J 2001 Resuscitation with room air instead of 100% oxygen prevents oxidative stress in moderately asphyxiated term neonates. Pediatrics 107: 642–647
Vento M, Asensi M, Sastre J, Garcia-Sala F, Miñana JB, Viña J 2002 Hyperoxemia caused by resuscitation with pure oxygen may alter intracellular redox status by increasing oxidized glutathione in asphyxiated newly born infants. Semin Perinatol 26: 406–410
Vento M, Sastre J, Asensi MA, Vina J 2005 Room-air resuscitation causes less damage to heart and kidney than 100% oxygen. Am J Respir Crit Care Med 172: 1393–1398
Saugstad OD, Ramji S, Vento M 2005 Resuscitation of depressed newborn infants with ambient air or pure oxygen: a meta-analysis. Biol Neonate 87: 27–34
Tan A, Schulze A, O'Donnell CP, Davis PG 2005 Air versus oxygen for resuscitation of infants at birth. Cochrane Database Syst Rev
Davis PG, Tan A, O'Donnell CP, Schulze A 2004 Resuscitation of newborn infants with 100% oxygen or air: a systematic review and meta-analysis. Lancet 364: 1329–1333
Saugstad OD, Ramji S, Soll RF, Vento M 2008 Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and meta-analysis. Neonatology 94: 176–182
Nijland R, Jongsma HW, Nijhuis JG, van den Berg PP, Oeseburg B 1995 Arterial oxygen saturation in relation to metabolic acidosis in fetal lambs. Am J Obstet Gynecol 172: 810–819
Dildy GA, van den Berg PP, Katz M, Clark SL, Jongsma HW, Nijhuis JG, Loucks CA 1994 Intrapartum fetal pulse oximetry: fetal oxygen saturation trends during labor and relation to delivery outcome. Am J Obstet Gynecol 171: 679–684
Sendak MJ, Harris AP, Donham RT 1986 Use of pulse oximetry to assess arterial oxygen saturation during newborn resuscitation. Crit Care Med 14: 739–740
Maxwell LG, Harris AP, Sendak MJ, Donham RT 1987 Monitoring the resuscitation of preterm infants in the delivery room using pulse oximetry. Clin Pediatr (Phila) 26: 18–20
Reddy VK, Holzman IR, Wedgwood JF 1999 Pulse oximetry saturations in the first 6 hours of life in normal term infants. Clin Pediatr (Phila) 38: 87–92
Meier-Stauss P, Bucher HU, Hurlimann R, Konig V, Huch R 1990 Pulse oximetry used for documenting oxygen saturation and right-to-left shunting immediately after birth. Eur J Pediatr 149: 851–855
Harris AP, Sendak MJ, Donham RT 1986 Changes in arterial oxygen saturation immediately after birth in the human neonate. J Pediatr 109: 117–119
House JT, Schultetus RR, Gravenstein N 1987 Continuous neonatal evaluation in the delivery room by pulse oximetry. J Clin Monit 3: 96–100
Dimich I, Singh PP, Adell A, Hendler M, Sonnenklar N, Jhaveri M 1991 Evaluation of oxygen saturation monitoring by pulse oximetry in neonates in the delivery system. Can J Anaesth 38: 985–988
Toth B, Becker A, Seelbach-Gobel B 2002 Oxygen saturation in healthy newborn infants immediately after birth measured by pulse oximetry. Arch Gynecol Obstet 266: 105–107
Mariani G, Brener P, Ezquer A, Aguirre A, Esteban ML, Perez C, Jonusas SF, Fustinana C 2007 Pre-ductal and post-ductal O-2 saturation in healthy term neonates after birth. J Pediatr 150: 418–421
Rabi Y, Yee W, Chen SY, Singhal N 2006 Oxygen saturation trends immediately after birth. J Pediatr 148: 590–594
Kamlin CO, O'Donnell CP, Davis PG, Morley CJ 2006 Oxygen saturation in healthy infants immediately after birth. J Pediatr 148: 585–589
Finer NN, Carlo WA, Duara S, Fanaroff AA, Donovan EF, Wright LL, Kandefer S, Poole WK 2004 Delivery room continuous positive airway pressure/positive end-expiratory pressure in extremely low birth weight infants: a feasibility trial. Pediatrics 114: 651–657
Escrig R, Arruza L, Izquierdo I, Villar G, Saenz P, Gimeno A, Moro M, Vento M 2008 Achievement of targeted saturation values in extremely low gestational age neonates resuscitated with low or high oxygen concentrations: a prospective, randomized trial. Pediatrics 121: 875–881
Wang CL, Anderson C, Leone TA, Rich W, Govindaswami B, Finer NN 2008 Resuscitation of preterm neonates using room air or 100% oxygen. Pediatrics 121: 1083–1089
Dawson JA, Kamlin CO, Wong C, Te Pas A, O'Donnell CP, Donath SM, Davis PG, Morley CJ 2008 Oxygen saturation and heart rate during delivery room resuscitation of infants <30 weeks gestation with air or 100% oxygen. Arch Dis Child Fetal Neonatal Ed. August 14 [Epub ahead of print]
Tin W, Milligan DW, Pennefather P, Hey E 2001 Pulse oximetry, severe retinopathy, and outcome at one year in babies of less than 28 weeks gestation. Arch Dis Child Fetal Neonatal Ed 84: F106–F110
Chow LC, Wright KW, Sola A 2003 Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants?. Pediatrics 111: 339–345
Deulofeut R, Critz A, Adams-Chapman I, Sola A 2006 Avoiding hyperoxia in infants of <1250 g is associated with improved short- and long-term outcomes. J Perinatol 26: 700–705
VanderVeen DK, Mansfield TA, Eichenwald EC 2006 Lower oxygen saturation alarm limits decrease the severity of retinopathy of prematurity. J AAPOS 10: 445–448
Wright KW, Sami D, Thompson L, Ramanathan R, Joseph R, Farzavandi S 2006 A physiologic reduced oxygen protocol decreases the incidence of threshold retinopathy of prematurity. Trans Am Ophthalmol Soc 104: 78–84
Anderson CG, Benitz WE, Madan A 2004 Retinopathy of prematurity and pulse oximetry: a national survey of recent practices. J Perinatol 24: 164–168
Nghiem TH, Hagadorn JI, Terrin N, Syke S, MacKinnon B, Cole CH 2008 Nurse opinions and pulse oximeter saturation target limits for preterm infants. Pediatrics 121: e1039–e1046
Clucas L, Doyle LW, Dawson J, Donath S, Davis PG 2007 Compliance with alarm limits for pulse oximetry in very preterm infants. Pediatrics 119: 1056–1060
Hagadorn JI, Furey AM, Nghiem TH, Schmid CH, Phelps DL, Pillers DA, Cole CH 2006 Achieved versus intended pulse oximeter saturation in infants born less than 28 weeks' gestation: the AVIOx study. Pediatrics 118: 1574–1582
STOP-ROP Multicenter Study Group 2000 Supplemental therapeutic oxygen for prethreshold retinopathy of prematurity (STOP-ROP), a randomized, controlled trial. I. Primary outcomes. Pediatrics 105: 295–310
Askie LM, Henderson-Smart DJ, Irwig L, Simpson JM 2003 Oxygen-saturation targets and outcomes in extremely preterm infants. N Engl J Med 349: 959–967
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Finer, N., Leone, T. Oxygen Saturation Monitoring for the Preterm Infant: The Evidence Basis for Current Practice. Pediatr Res 65, 375–380 (2009). https://doi.org/10.1203/PDR.0b013e318199386a
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e318199386a
This article is cited by
-
Oxygen saturation and heart rate in healthy term and late preterm infants with delayed cord clamping
Pediatric Research (2022)
-
Cerebral regional tissue Oxygen Saturation to Guide Oxygen Delivery in preterm neonates during immediate transition after birth (COSGOD III): an investigator-initiated, randomized, multi-center, multi-national, clinical trial on additional cerebral tissue oxygen saturation monitoring combined with defined treatment guidelines versus standard monitoring and treatment as usual in premature infants during immediate transition: study protocol for a randomized controlled trial
Trials (2019)
-
Predicting 2-y outcome in preterm infants using early multimodal physiological monitoring
Pediatric Research (2016)
-
Fully automated predictive intelligent control of oxygenation (PRICO) in resuscitation and ventilation of preterm lambs
Pediatric Research (2015)
-
Performance Evaluation of New-Generation Pulse Oximeters in the NICU: Observational Study
Cardiovascular Engineering and Technology (2015)