Abstract
The aim of the study was to assess the association between bronchopulmonary dysplasia (BPD) and polymorphisms of genes coding for vascular endothelial growth factor (VEGF), transforming growth factor (TGF-β1), insulin-like growth factor (IGF-1), and 5,10-methylenetetrahydrofolate reductase (MTHFR). A sample of 181 newborns with mean gestational age of 28 wk was prospectively evaluated. Molecular analysis of TGF-β1 −800G>A, −509C>T, 10T>C, 25G>C, VEGF −460T>C and 405G>C and MTHFR 677C>T polymorphisms were performed and the number of CA repeats in the promoter region of IGF-1 gene was assessed. The frequency of all TGF-β1, IGF-1, and MTHFR polymorphisms, as well as the frequency of VEGF 405G>C polymorphism was similar in all groups. The newborns with −460TT and −460CT genotypes were significantly overrepresented in the BPD groups compared with the no BPD group. Multivariate analysis revealed that carrying T allele increased the risk of BPD by 9% (95%CI: 2–14%) above the baseline risk established for given gestational age, length of oxygen therapy, and sex. Based on our data from a single center, we propose that VEGF −460T>C polymorphism may influence the risk of BPD.
Similar content being viewed by others
Main
An increase in survival of extremely preterm infants has been associated with an increased incidence of bronchopulmonary dysplasia (BPD) (1), which has become a major clinical challenge because of its serious health consequences. Surviving infants with BPD are at higher risk for recurrent respiratory infections, bronchial hyperreactivity, repeated hospitalizations, and neurodevelopmental abnormalities (1,2).
The current consensus is that BPD is a complex disease: the interaction of a susceptible host with a multitude of external risk factors underlies its pathogenesis. It is still unclear why BPD progresses to severe disease in one group of very low birth weight (VLBW) infants but regresses spontaneously in other infants with similar clinical characteristics. This difference in BPD development may result from differences in reactions to inflammatory stimuli and varied ability to tolerate oxidative stress and inflammation. Genetic foundations for the development of BPD are implicated in twin studies, which reveal highly significant concordance rates for BPD: 3.69-fold in monozygotic and 1.4-fold in dizygotic twins (3).
The criteria for selection of BPD candidate genes in the present study were their potential involvement in angiogenesis and alveolarization regulating mechanisms, as well as their involvement in free radical elimination.
The first factor worth examining is vascular endothelial growth factor (VEGF). VEGF is a relatively specific endothelial cell mitogen that regulates endothelial cell differentiation and angiogenesis, and plays a central role in vascular repair. VEGF has multiple roles in vascular development and maintenance and is essential for the formation of embryonic vasculature (4,5). The absence of VEGF results in impaired fetal lung microvascular development. The VEGF gene is also a good candidate because there are a considerable number of known polymorphisms (6,7), some of which are associated with altered VEGF production (6,8–10). Awata et al. (9) has shown (in vivo) that VEGF serum levels are significantly higher in +405CC carriers than in those with other genotypes of the same polymorphism. This finding is consistent with data presented by Lambrechts et al. (10) (in vitro). The authors found that the +405G allele reduces internal ribosome entry site mediated VEGF expression and also reduces translation of the large L-VEGF isoform. Watson et al. (7) observed a significant correlation between lipopolysaccharide-stimulated peripheral blood mononuclear cell VEGF protein production and the genotype for the +405 polymorphism (+405G carriers showed higher VEGF production). This information has been confirmed by Stevens et al. (8).
As interstitial fibrosis in the lungs plays a key role in the pathogenesis of BPD, transforming growth factor-β (TGF-β) seems to be another likely candidate for selection. Recent data have shown that TGF-β is involved in adult pulmonary fibrosis and inhibition of branching morphogenesis in embryonic lung development. Animal models have revealed that overexpression of TGF-β1 induces pathology that closely resembles that seen in human neonates with BPD (11).
IGF (IGF-1) is also involved in growth and injury repair processes in many organs, including the lungs. IGF-1 expression is altered by inflammatory cytokines and oxidants. However, the correlation between abnormal lung growth and maturation and the local production of IGF-1 has been poorly explored in humans (12,13).
As BPD is still classified as a free radical disease, the second possible group of candidate genes is of those coding for molecules involved in free radical elimination. One of the systems acting as free radical scavengers is the homocysteine-methionine metabolic complex. The activity of the system strongly depends on remethylation of homocysteine to methionine. 5,10-Methylenetetrahydrofolate reductase (5,10-MTHFR) is an enzyme, which catalyzes the reduction of 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, the major methyl group donor for the conversion of homocysteine to methionine. In individuals homozygous for the 677C>T polymorphism, specific 5,10-MTHFR enzyme activity is reduced to approximately one third. In addition, the 5,10-MTHFR enzyme is more unstable than the normal isoform. In consequence, the plasma homocysteine level almost doubles. There is now firm evidence that an elevated plasma homocysteine level is an independent risk factor for many diseases, including cardiovascular diseases (vascular thrombosis, myocardial infarctions, strokes), neurodegenerative diseases (Alzheimer and Parkinson disease), neural tube defects, and carcinomas (particularly colon carcinoma). We chose the 5,10-MTHFR gene as a candidate gene for BPD, because numerous studies have demonstrated the correlation between hyperhomocysteinemia and increased production of reactive oxygen species and oxidant stress (14–16).
The main objective of the study was to assess genetic risk factors for BPD development by analyzing its association with polymorphisms of the following candidate genes: VEGF, TGF-β1, IGF-1, and 5,10-MTHFR.
METHODS
Patients.
A prospective study was conducted in the Neonatal Intensive Care Unit of the Polish-American Children's Hospital between May 21, 2003 and October 31, 2006. The entry criteria were: 1) preterm birth at 24–32 wk gestational age; 2) birthweight ≤1500 g (VLBW); and 3) a need for mechanical ventilation or noninvasive respiratory support (nasal continuous positive airway pressure—nCPAP) during the first 3 d of life. Children with major congenital defects were excluded from the study.
Detailed perinatal history (birth weight, gestational age, Apgar score at 1, and 5 min after birth) and history of treatment in the referral hospital (mechanical ventilation, oxygen therapy, surfactant treatment, diagnoses) were taken on admission. Gestational age assessment was performed by two physicians based on the Ballard scale. A discrepancy of 3 wk or more between the two assessments excluded the newborn from the study. The study had been approved by the Ethics Committee of Jagiellonian University, Faculty of Medicine.
Laboratory evaluation.
After obtaining informed consent from the parents, one blood sample (0.3 mL) was collected from each patient. Subsequently, DNA was extracted from the peripheral leukocytes by means of a QIAamp DNA Blood Mini Kit (QIAGEN). Appropriate DNA fragments of the 5,10-MTHFR gene (GenBank accession number NM005957), TGF-β1 gene (GenBank accession number ×05839), VEGF gene (GenBank accession number M63971), and IGF-1 gene (GenBank accession number AY260957) were amplified using PCR and analyzed using either PCR-RFLP, DHPLC (denaturing HPLC), or direct sequencing. Table 1 presents details on the techniques used.
After interim analysis (May 2004), VEGF, TGF-β1, and IGF-1 serum concentrations were additionally measured in the 2nd and 4th week of life to assess the functional role of the gene polymorphisms. Blood samples were drawn (0.4 mL), centrifuged, and the serum frozen at −70°C until the time of testing. Growth factor concentrations were measured using commercially available kits based on the ELISA method (R&D System, Minneapolis, USA). The measurements were performed according to instructions provided by the manufacturer. The samples were coded by a person not involved in the clinical part of the study and the assays were anonymous.
Outcome variables.
Scheduled examinations were performed on all patients. The procedures of oxygen therapy in the examined group were consistent throughout the study with the goal of maintaining Hb saturation between 88 and 96%. BPD severity was graded according to criteria proposed by Jobe and Bancalari (17). Four cohorts of children were identified based on examination at age 36 wk post conception or on discharge. Mild BPD was defined as a need for supplemental oxygen for > or = 28 d, but not at 36 wk' postmenstrual age (PMA) or discharge. Moderate BPD was defined as a need for supplemental oxygen for > or = 28 d plus treatment with <30% oxygen at 36 wk' PMA. And, severe BPD as a need for supplemental oxygen for > or = 28 d plus > or = 30% oxygen supplementation and/or positive pressure at 36 wk' PMA. Infants treated with oxygen >21% and/or positive pressure for nonrespiratory disease (e.g., central apnea or diaphragmatic paralysis) were not included in the BPD group unless they also developed parenchymal lung disease and exhibited clinical features of respiratory distress. Treatment with oxygen >21% and/or positive pressure at 36-wk PMA due to an “acute” event was not a criterion for BPD. The evaluation of oxygen requirement was performed by a staff member blinded to biochemical and molecular studies results.
Statistical methods.
Comparison between the groups was performed using t test, Kruskal–Wallis test, or Fisher's exact test, as appropriate. Next, different factors (gestational age, length of oxygen therapy, PDA, surfactant treatment, length of parenteral nutrition, intraventricular hemorrhage) associated with BPD in univariate analyses were entered as covariates for logistic regression analysis. Logistic regression was used to estimate odds ratios for developing BPD, depending on VEGF −460C>T genotype, and controlling for confounding variables. Statistical significance was defined at the two sided p = 0.05 level. Data were analyzed using SAS Software (2006 by SAS Institute Inc., Cary, NC).
If a study tests more than one hypothesis, the probability of finding at least one test to be statistically significant due to chance, and to incorrectly declare a difference to be valid (type I error) increases. Our study evaluated eight different SNPs. Had no correction been applied, the multiple testing would have increased the probability of type I error to 0.3366 (33.66%). Correction for the multiple tests was therefore performed using Sidak's adjustment for correlated variables. First, a matrix of the correlations between the different SNPs was generated, and the mean correlation computed.
An online calculator, found at: http://www.kursus.kvl.dk/shares/vetgen/_Popgen/genetik/applets/kitest.htm, was used to test for deviation from the Hardy-Weinberg equilibrium in samples of no BPD (control) and BPD patients.
Sample size estimations were difficult to perform with only limited information on the polymorphism frequencies in the studied population of preterm babies, and on the exact nature of their clinical effect.
Sample size estimations were based on the assumption that the frequency of common alleles ranged between 50–90%. The inclusion criteria were established in such a way as to ensure approximately 50% prevalence of BPD in the studied population, with the aim of obtaining a similar number of cases and controls (i.e., a case–control ratio of 1). We calculated that if the frequency of common alleles differed by 15% in the BPD group, we would have an 80% chance of detecting this difference (with probability of type I error; two-sided test α = 0.05) with 90 infants in each group (total 180 infants). Sample size calculation was performed using PS Power and Sample Size Calculations software (Version 2.1.30, February 2003, http://www.mc.vanderbilt.edu/prevmed/ps/index.htm).
RESULTS
One hundred eighty-one newborns were included in the study (90 boys and 91 girls). The study population was homogenous; it included only whites, all children were born of Polish parents. The mean birth weight was 1054 g (SD: 233), and the mean gestational age was 28.1 wk (SD: 2.39). The majority of pregnancies terminated with abrupt deliveries. Only 64 (35%) mothers received antenatal steroids. A considerable percentage of neonates (41%) were born by vaginal delivery. As many as 148 (82%) newborns required mechanical ventilation during the first 3 d of life. Mechanical ventilation lasted 20 d (median) and oxygen therapy lasted 41 d (median). Sixty-seven (37%) newborns received surfactant treatment.
During the follow-up period, BPD was diagnosed in 118 (65%) infants, including 58 (32%) children with mild disease, 23 (13%) with moderate and 37 (20%) with severe BPD. Sixty-three babies served as a control group (no BPD).
Groups were similar regarding the use of antenatal steroids, sex, Apgar score, and mode of delivery. The infants in the BPD group were of lower birthweight and gestational age. As shown in Table 2, more infants in the BPD group received surfactant treatment, had persistent ductus arteriosus, intraventricular hemorrhage, and necrotizing enterocolitis (grade II or III according to Bell's classification) (all p < 0.05). Moreover, infants in the BPD group received more days of ventilation, oxygen, parenteral nutrition, and/or postnatal steroids (all p < 0.05).
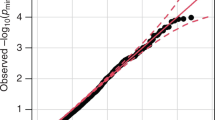
The allele frequencies of all studied polymorphisms remained within the Hardy-Weinberg equilibrium (detailed data on request). The allele frequencies of all TGF-β1, IGF-1, and 5,10-MTHFR gene polymorphisms were similar in all groups (detailed data on request). The frequency of the VEGF 405G>C polymorphism was also similar in all groups. The carriers of the polymorphic allele −460 T were significantly overrepresented in all the groups of BPD newborns compared with the control group (48.7 versus 35.7%; OR: 1.71: 95% CI:1.1–2.7) (Table 3). Moreover, this carrier state was an independent risk factor (Table 4). Multivariate analysis showed that carrying the T allele increased the risk of BPD by about 9% (95%CI: 2–14%) from the baseline risk (as estimated by gestational age, length of oxygen therapy and sex—Figs. 1–2). The risk of BPD was lowest in the babies homozygous for the −460 C allele (adjusted OR: 0.147: 95% CI: 0.03–0.86, adjusted for multiple testing p = 0.048). The observed serum concentrations of VEGF in patients with different 405G>C and −460T>C genotypes are presented in Table 5. VEGF serum concentrations in patients ascribed to different groups according to the 405G>C genotype were similar. VEGF serum concentrations in children with different −460T>C genotypes were not statistically different.
A, Probability of bronchopulmonary dysplasia among patients with VEGF genotypes −460CC and −460CT/TT—correlation with gestational age. B, Probability of severe bronchopulmonary dysplasia among—patients with VEGF genotypes −460CC and −460CT/TT—correlation with gestational age. ▴ TT or CT genotypes; • CC genotype.
A, Probability of bronchopulmonary dysplasia among patients with VEGF genotypes −460CC and −460CT/TT—correlation with length of oxygen therapy. B, Probability of severe bronchopulmonary dysplasia among patients with VEGF genotypes −460CC and −460CT/TT—correlation with length of oxygen therapy. ▴ TT or CT genotypes; • CC genotype.
DISCUSSION
Identification of genetic predisposing factors to diseases such as BPD could help in the development of new treatments and might allow for targeting of this treatment on a “high-risk” subgroup, reducing unnecessary exposure to potentially harmful therapies. The use of postnatal steroids is a good example of such treatment. It is well known that short-term steroid therapy in 2- to 3-wk-old neonates with a high risk of severe BPD may improve respiratory condition, without increasing the risk of cerebral palsy. However, it is still difficult to predict which neonate will develop to severe BPD.
Searching for BPD risk factors, we conducted a prospective study of 181 VLBW newborns. This was a prospective study, which is extremely important considering the definition of BPD adopted by the study. It deserves attention that the NICU where the study was conducted admits a highly selective group of newborns from primary and secondary level centers who require intensive care. Thus, the study focused on a high-risk population for BPD development (Table 2). The specific character of the studied population might have influenced the results obtained; namely, it was biased toward a statistically significant difference. The prevalence of BPD in the study group may also lead to difficulties in generalizing the results and implementing them into everyday practice.
The most significant observation in the present study is the association between the −460T>C VEGF gene polymorphism and the risk of BPD. We found that VEGF −460CC homozygotes have a lower risk than babies with −460TT or −460TC genotypes. Two VEGF polymorphisms were chosen in this study because they occur at a relatively high minor allele frequency in the general population. These single nucleotide polymorphisms also alter VEGF expression. Haplotypes containing the common polymorphisms at −460C in the promoter and +405G have a 71% higher basal promoter activity when compared with the wild-type sequence (8). Therefore, we can speculate that the most plausible mechanism is that the −460C VEGF allele is a part of a promoter haplotype with increased activity, either under basal conditions or in response to stimuli such as hypoxia, cytokines or lipopolysaccharides. To validate this finding we tried to measure VEGF serum concentrations. The results of VEGF serum concentrations within different allele carrier groups did not confirm the potential protective character of this genotype.
Multitesting procedures can increase the probability of type I error. In our study, the corrected alpha level based on mean correlation factor 0.13 between different genotypes equaled 0.0083. The unadjusted p value for different VEGF −460 alleles and the risk of BPD was 0.013 (Table 3). Thus, multiple test correction increased the risk of type I error to 7.8%. However, the unadjusted p value for comparison of BPD frequency between −460 CC carriers with −460CT or −460TT carriers equaled 0.005, so the risk of type I error was lower than 5%.
If the chance of making a type I error, in an individual test is reduced the chance of making a type II error is increased that is, finding no statistical difference, when in fact there is one. As indicated by the data on the allele frequencies of the −460C>T VEGF gene obtained in the present study, the estimated power to reveal the difference in allele frequencies between the BPD and no BPD groups was 80.3%.
However, the observed differences in allele frequencies of other studied polymorphisms (IGF-1, TGFβ-1, and 5,10-MTHFR) were smaller than those used in our sample size estimation; therefore, we cannot rule out the possibility of a type II error in the population studied. It should be noted, that if a difference does exist, it is lower than 15%, which, in our opinion, makes it clinically insignificant. Recruiting larger numbers of infants within a reasonable timeframe from a single center is very difficult. Hence, replication of our results in larger, multicenter center studies is necessary.
It is known that alternative splicing may result in at least four transcripts encoding mature monomeric VEGF containing 121, 165, 189, and 206 amino acid residues (VEGF121, VEGF165, VEGF189, and VEGF206). VEGF121 and VEGF165 are diffusible proteins, but VEGF189 and VEGF206 have a high affinity for heparin and are mostly bound to heparin-containing proteoglycans in the extracellular matrix. In the present study, the ELISA Quantikine system was used, which detects only the VEGF165 form. Such study protocol raises the question of whether serum concentration reflects lung VEGF concentration. Moreover, little is known about the correlation between gene polymorphism and the production of all four isoforms.
The frequency of the VEGF −460C allele in the studied cohort is similar to that found in studies evaluating the association between VEGF encoding gene polymorphisms and the risk of retinopathy of prematurity (18,19). Shastry et al. (19) have demonstrated that the frequency of the VEGF −460C allele is similar in preterm and term newborns. This suggests little effect of this allele on the incidence of preterm birth.
Ethnicity greatly influences the distribution of gene polymorphisms. The first studies describing the role of the 460 T>C polymorphism were conducted on Asians (20,21). Their results indicated that the frequency of the T allele was about 75%, and the frequency of the C allele was about 25%. Further studies included other ethnic groups. Most of the studies on European populations revealed the frequency of the T allele to range between 45 and 55% (7,18,22,23). Recently published results obtained from Turkish population show that in this group the T allele occurs in “merely” 38% (24). Therefore, caution should be exercised when extrapolating our findings to other populations.
We found that the VEGF genotype was predictive even after controlling for variables such as gestational age, length of oxygen therapy, sex, persistent ductus arteriosus, surfactant treatment, length of parenteral nutrition, and intraventricular hemorrhage. However, −460CC homozygosity only decreases the risk of BPD. Interestingly, the effect of this polymorphism and probably the effect of VEGF in general may occur early in the course of the disease rather than later.
Our study, which evaluated 181 VLBW infants, has not confirmed any association between the IGF-1, TGF-β1, or 5,10-MTHFR gene polymorphisms and the risk of BPD. There are a few possible explanations for our negative results. We can speculate that metabolic and nutritional changes during postnatal life have a greater effect on growth factor levels than gene polymorphism. A good example is the changes in serum IGF-1 levels observed in VLBW infants. Hellstrom et al. showed that serum IGF-1 levels in premature infants may be reduced by poor nutrition, acidosis, hypothyroxinemia, and sepsis (14).
The role of genetic factors in the development of BPD is unclear. Functional polymorphisms in growth factor genes may alter angiogenesis and alveolarization, and contribute to the development of BPD. However, few studies have dealt with this issue. Adcock et al. (25) failed to find any association of TNF-α –308, MCP-1 –2518 (Monocyte Chemoattractant Protein-1), and TGF-β1 + 915 gene polymorphisms with the risk of BPD. In a small sample, there was a significantly increased frequency of the SP-A1 (Surfactant Protein) polymorphism 6A6 in newborns with BPD (26). Makri et al. (27) have shown that the frequency of BPD was higher in a group of preterm infants carrying the genetic variations of polymorphism within intron 4 of the surfactant protein B gene compared with preterm infants with the intron 4 wild type. In another study, after controlling for race and gender, BPD cases were less likely to be homozygous for the more efficient Val/Val allele of glutathione S-transferase P1 and more likely to have the less efficient Ile isoform (28). Recently, Strassberg failed to find any association of five common polymorphisms of TNF-α with BPD (29).
Finally, lung injury and the subsequent maladaptive repair process that leads to the development of BPD are complex, with numerous factors that interact to determine outcome. It is very likely that genetic differences other than growth factor gene polymorphisms play a role in determining the risk of BPD. Genetic variation in surfactant protein genes may also influence the severity of respiratory distress syndrome and subsequent development of BPD (30,31). Polymorphisms in cytokines and their receptors, bacterial pattern recognition molecules, surfactant proteins, and heme oxygenase-1 are all known to alter the course of other pulmonary diseases in adults and children. The potential role of these factors in the development of BPD in premature infants should therefore be examined.
In conclusion, our selection of genes encoding growth factors (VEGF, TGF-β1, and IGF-1) as well as those involved in free radical elimination (5,10-MTHFR) as candidate genes for BPD was based on their potential involvement in angiogenesis regulating mechanisms. Genetic polymorphisms of these genes show no significant association with the incidence of BPD, except the VEGF −460T>C polymorphism. We found that VEGF −460CC homozygotes are at a lower risk than babies with −460TT or −460TC genotypes.
The results of phenotype-genotype analysis revealed no correlation between studied VEGF gene polymorphisms and VEGF serum concentrations. Further studies are needed to create bases for genetic screening of newborns and to look for populations with the high-risk genotype. These bases will potentially provide the means for better BPD prevention and treatment.
Abbreviations
- 5,10-MTHFR:
-
5,10-methylenetetrahydrofolate reductase
- BPD:
-
bronchopulmonary dysplasia
- PDA:
-
patent ductus arteriosus
- PMA:
-
postmenstrual age
- SNP:
-
single nucleotide polymorphism
- VLBW:
-
very low birthweight
References
Christou H, Brodsky D 2005 Lung injury and bronchopulmonary dysplasia in newborn infants. J Intensive Care Med 20: 76–87
Bancalari E 2006 Bronchopulmonary dysplasia: old problem, new presentation. J Pediatr (Rio J) 82: 2–3
Bhandari V, Bizzarro MJ, Shetty A, Zhong X, Page GP, Zhang H, Ment LR, Gruen JR 2006 Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics 117: 1901–1906
Asikainen TM, Waleh NS, Schneider BK, Clyman RI, White CW 2006 Enhancement of angiogenic effectors through hypoxia-inducible factor in preterm primate lung in vivo. Am J Physiol Lung Cell Mol Physiol 291: L588–L595
Lassus P, Ristimaki A, Ylikorkala O, Viinikka L, Andersson S 1999 Vascular endothelial growth factor in human preterm lung. Am J Respir Crit Care Med 159: 1429–1433
Brogan IJ, Khan N, Isaac K, Hutchinson JA, Pravica V, Hutchinson IV 1999 Novel polymorphisms in the promoter and 5′ UTR regions of the human vascular endothelial growth factor gene. Hum Immunol 60: 1245–1249
Watson CJ, Webb NJ, Bottomley MJ, Brenchley P 2000 Identification of polymorphisms within the vascular endothelial growth factor (VEGF) gene: correlation with variation in VEGF protein production. Cytokine 12: 1232–1235
Stevens A, Soden J, Brenchley PE, Ralph S, Ray DW 2003 Haplotype analysis of the polymorphic human vascular endothelial growth factor gene promoter. Cancer Res 63: 812–816
Awata T, Inoue K, Kurihara S, Ohkubo T, Watanabe M, Inukai K, Inoue I, Katayama S 2002 A common polymorphism in the 5′-untranslated region of the VEGF gene is associated with diabetic retinopathy in type 2 diabetes. Diabetes 51: 1635–1639
Lambrechts D, Storkebaum E, Morimoto M, Del-Favero J, Desmet F, Marklund SL, Wyns S, Thijs V, Andersson J, van Marion I, Al-Chalabi A, Bornes S, Musson R, Hansen V, Beckman L, Adolfsson R, Pall HS, Prats H, Vermeire S, Rutgeerts P, Katayama S, Awata T, Leigh N, Lang-Lazdunski L, Dewerchin M, Shaw C, Moons L, Vlietinck R, Morrison KE, Robberecht W, Van Broeckhoven C, Collen D, Andersen PM, Carmeliet P 2003 VEGF is a modifier of amyotrophic lateral sclerosis in mice and humans and protects motoneurons against ischemic death. Nat Genet 34: 383–394
Gauldie J, Galt T, Bonniaud P, Robbins C, Kelly M, Warburton D 2003 Transfer of the active form of transforming growth factor-beta 1 gene to newborn rat lung induces changes consistent with bronchopulmonary dysplasia. Am J Pathol 163: 2575–2584
Chetty A, Andersson S, Lassus P, Nielsen HC 2004 Insulin-like growth factor-1 (IGF-1) and IGF-1 receptor (IGF-1R) expression in human lung in RDS and BPD. Pediatr Pulmonol 37: 128–136
Hellstrom A, Engstrom E, Hard AL, Albertsson-Wikland K, Carlsson B, Niklasson A, Lofqvist C, Svensson E, Holm S, Ewald U, Holmstrom G, Smith LE 2003 Postnatal serum insulin-like growth factor I deficiency is associated with retinopathy of prematurity and other complications of premature birth. Pediatrics 112: 1016–1020
van Bockxmeer FM, Mamotte CD, Vasikaran SD, Taylor RR 1997 Methylenetetrahydrofolate reductase gene and coronary artery disease. Circulation 95: 21–23
Isotalo PA, Wells GA, Donnelly JG 2000 Neonatal and fetal methylenetetrahydrofolate reductase genetic polymorphisms: an examination of C677T and A1298C mutations. Am J Hum Genet 67: 986–990
Yamada K, Chen Z, Rozen R, Matthews RG 2001 Effects of common polymorphisms on the properties of recombinant human methylenetetrahydrofolate reductase. Proc Natl Acad Sci USA 98: 14853–14858
Jobe AH, Bancalari E 2001 Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163: 1723–1729
Vannay A, Dunai G, Banyasz I, Szabo M, Vamos R, Treszl A, Hajdu J, Tulassay T, Vasarhelyi B 2005 Association of genetic polymorphisms of vascular endothelial growth factor and risk for proliferative retinopathy of prematurity. Pediatr Res 57: 396–398
Shastry BS, Qu X 2007 Lack of association of the VEGF gene promoter (−634 G–>C and −460 C–>T) polymorphism and the risk of advanced retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol 245: 741–743
Kim SH, Choi YM, Choung SH, Jun JK, Kim JG, Moon SY 2005 Vascular endothelial growth factor gene +405 C/G polymorphism is associated with susceptibility to advanced stage endometriosis. Hum Reprod 20: 2904–2908
Yim HE, Bae IS, Yoo KH, Hong YS, Lee JW 2007 Genetic control of VEGF and TGF-beta 1 gene polymorphisms in childhood urinary tract infection and vesicoureteral reflux. Pediatr Res 62: 183–187
Vannay A, Vasarhelyi B, Kornyei M, Treszl A, Kozma G, Gyorffy B, Tulassay T, Sulyok E 2006 Single-nucleotide polymorphisms of VEGF gene are associated with risk of congenital valvuloseptal heart defects. Am Heart J 151: 878–881
Van Der Meer P, De Boer RA, White HL, Van Der Steege G, Hall AS, Voors AA, Van Veldhuisen DJ 2005 The VEGF +405 CC promoter polymorphism is associated with an impaired prognosis in patients with chronic heart failure: a MERIT-HF substudy. J Card Fail 11: 279–284
Onen IH, Konac E, Eroglu M, Guneri C, Biri H, Ekmekci A 2008 No association between polymorphism in the vascular endothelial growth factor gene at position-460 and sporadic prostate cancer in the Turkish population. Mol Biol Rep 35: 17–22
Adcock K, Hedberg C, Loggins J, Kruger TE, Baier RJ 2003 The TNF-alpha-308, MCP-1-2518 and TGF-beta1 +915 polymorphisms are not associated with the development of chronic lung disease in very low birth weight infants. Genes Immun 4: 420–426
Weber B, Borkhardt A, Stoll-Becker S, Reiss I, Gortner L 2000 Polymorphisms of surfactant protein A genes and the risk of bronchopulmonary dysplasia in preterm infants. Turk J Pediatr 42: 181–185
Makri V, Hospes B, Stoll-Becker S, Borkhardt A, Gortner L 2002 Polymorphisms of surfactant protein B encoding gene: modifiers of the course of neonatal respiratory distress syndrome?. Eur J Pediatr 161: 604–608
Manar MH, Brown MR, Gauthier TW, Brown LA 2004 Association of glutathione-S-transferase-P1 (GST-P1) polymorphisms with bronchopulmonary dysplasia. J Perinatol 24: 30–35
Strassberg SS, Cristea IA, Qian D, Parton LA 2007 Single nucleotide polymorphisms of tumor necrosis factor-alpha and the susceptibility to bronchopulmonary dysplasia. Pediatr Pulmonol 42: 29–36
Hallman M, Haataja R 2006 Surfactant protein polymorphisms and neonatal lung disease. Semin Perinatol 30: 350–361
Pavlovic J, Papagaroufalis C, Xanthou M, Liu W, Fan R, Thomas NJ, Apostolidou I, Papathoma E, Megaloyianni E, DiAngelo S, Floros J 2006 Genetic variants of surfactant proteins A, B, C, and D in bronchopulmonary dysplasia. Dis Markers 22: 277–291
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by unrestricted grants of Polish Ministry of Science (grant number 3 PO5E 024 24) and Jagiellonian University Research Grant (grant number 4103/424/2/2005/WL/NKL/96/L).
Rights and permissions
About this article
Cite this article
Kwinta, P., Bik-Multanowski, M., Mitkowska, Z. et al. Genetic Risk Factors of Bronchopulmonary Dysplasia. Pediatr Res 64, 682–688 (2008). https://doi.org/10.1203/PDR.0b013e318184edeb
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e318184edeb
This article is cited by
-
Bronchopulmonary dysplasia and wnt pathway-associated single nucleotide polymorphisms
Pediatric Research (2022)
-
Verification of immunology-related genetic associations in BPD supports ABCA3 and five other genes
Pediatric Research (2022)
-
Genetic and Epidemiological Similarities, and Differences Between Postoperative Intraperitoneal Adhesion Development and Other Benign Fibro-proliferative Disorders
Reproductive Sciences (2022)
-
Association of a vascular endothelial growth factor polymorphism with the development of bronchopulmonary dysplasia in Japanese premature newborns
Scientific Reports (2014)
-
Association of surfactant protein B gene polymorphisms (C/A-18, C/T1580, intron 4 and A/G9306) and haplotypes with bronchopulmonary dysplasia in chinese han population
Journal of Huazhong University of Science and Technology [Medical Sciences] (2013)