Abstract
Bronchopulmonary dysplasia (BPD) and cystic fibrosis (CF) are two common serious chronic respiratory disorders without specific treatments affecting children. BPD is characterized by an arrest in alveolar growth in premature infants requiring respiratory support. CF is the most common fatal inherited genetic disorder characterized by abnormally thick mucus secretions, recurrent infection and ultimately lung destruction. One commonality between these two diseases is the promise of utilizing stem cells therapeutically. Indeed, the use of exogenous cells to supplement the natural repair mechanisms or the possibility of genetic manipulation in vitro before administration are appealing therapeutic options for these diseases. Increasing attention has been focused on the use of adult bone marrow-derived stem cells (BMSC) to regenerate damaged organs such as the heart, the brain, and the liver. However, due to the lung's complexity as well as the low rate of cellular turnover within the lung, progress has been slower in this area compared with the skin or liver. Initial work suggests that BMSC can engraft and differentiate into a variety of lung cells, but these findings have been challenged recently. This article critically reviews the current advances on the therapeutic use of stem cells for lung regeneration.
Similar content being viewed by others
Main
The current promise that stem cells hold for tissue regeneration is immense. The belief that once irreversibly damaged tissue can be restored to a normal functional capacity is providing great optimism for novel treatments in many diseases. However, this research is not without its controversies. There are ethical and moral issues surrounding the use of stem cells derived from embryos. Recent research is starting to unravel the potential for adult derived stem cells that was initially described more than 20 y ago. While the initial results from numerous disease models outside the lung show great potential for a cell replacement therapy, there is heated debate over numerous concerns within the stem cell field. The mechanism of action, the plasticity, the source, the phenotype, and the “stemness” of the stem cells used are all contentious issues. Furthermore, stem cell research has been markedly slower in lung diseases due to the complexity of the lung. The lung possesses numerous anatomical areas (upper airways, bronchioles, alveoli and their underlying capillaries) each of which contains a unique cellular population with drastically different functions.
There are two common, serious pediatric lung diseases without current treatments that stem cells hold potential promise for: bronchopulmonary dysplasia (BPD) and cystic fibrosis (CF). BPD is the chronic lung disease of prematurity that follows ventilator support. BPD is characterized by an arrest in alveolar and vascular growth (1, 2). The long-term consequences of this halted lung growth are still unknown. Therefore, the potential of a stem cell to restore or protect the alveolar epithelium is very attractive as this may reduce the morbidity and mortality associated with BPD. CF results from mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene and affects 1 in 3200 live births (3). There are five classes of gene defects in CF: 1) defective protein production; 2) aberrant intracellular protein trafficking; 3) defective regulation of chloride transport; 4) reduced chloride transport function; 5) reduced protein expression. The most common cause of CF occurs within class 2 (4). The aberrant intracellular protein trafficking is caused by the deletion of an amino acid, commonly referred to as ΔF508 (3, 4). Pulmonary complications are typically the most serious and life-threatening manifestations of CF. Major advances in the multidisciplinary management of CF have contributed to prolong the life span of affected patients to the mid 30s, but quality of life and other CF-related complications justify the search for a cure. Stem cells have the potential to act as a vehicle for corrective gene therapy, thereby restoring normal organ function. Ultimately, lung stem cell therapy may also be applicable to other devastating lung disorders such as pulmonary hypoplasia.
This review will critically analyze the controversial literature investigating the use of exogenously administered stem cells for lung diseases.
DEFINITION OF STEM CELLS
Stem cells may be artificially classified into three categories: embryonic stem (ES) cells, adult bone marrow derived stem cells (BMSC), and tissue progenitor cells (Table 1). ES cells are pluripotent cells derived from the inner cell mass of blastocyst-stage embryos (5). They are able to form tissue within each of the germ layers (the endoderm, mesoderm, and ectoderm) and have thus enormous therapeutic potential to regenerate any damaged tissue; but ES cells are also mired in great controversy due to the present need of destroying an embryo to harvest pluripotent cells (6). Conversely, progenitor cells are thought to reside within a tissue and are stimulated for repair after injury. It is these tissue progenitor cells that give the liver (the hepatic oval cell) its robust regenerative ability (7, 8). In the lung, type II alveolar epithelial cells (AEC) are the putative distal progenitor cells responsible for repair after injury (9, 10). Side population (SP) cells, identified by their ability to efflux Hoechst dye, and tracheal epithelial basal cells, are putative progenitor cells in the upper airways (11). While the pluripotency of ES and further characterization of resident lung stem cells (12, 13) hold promise for novel therapeutic approaches for lung diseases, this review will focus on the adult bone-marrow derived stem cell and their exogenous administration in various models of lung diseases.
The bone marrow contains several population of primitive cells: 1) Hematopoeitic stem cells (HSCs); 2) mesenchymal stem cells (MSCs); 3) endothelial stem/progenitor cells (EPC); 4) SP cells; and 5) multipotent adult progenitor cells (MAPC). Among these, the HSCs are the best characterized of the adult stem cells (14). HSCs are multipotent and have the ability to maintain or restore the mature circulating blood cells (erythrocytes and leukocytes). Recent evidence suggest that bone-marrow derived cells have the ability to cross lineage barriers and generate differentiated tissue beyond their own tissue boundaries to form functional components of other tissues, expressing tissue-specific proteins in organs such as heart, liver, brain, skeletal muscle, and vascular endothelium (15). A true potential for adult derived stem cells lies with the multipotent MSCs and these cells have been extensively used in lung stem cell research. This potential was first proposed in the 1970s by Friedenstein et al. (16). This initial report showed that plastic adherent cells, previously believed to be committed to a specific tissue type (i.e. bone marrow), had the ability to form cells within the osteogenic, chondrogenic, and adipogenic lineages (16). There have been numerous reports characterizing the phenotype of these MSCs in both humans (17, 18) and mice (16, 19). However, it was not until over 20 y after Friedenstein's first report that the true potential of these cells were made apparent. In 2001, Krause et al. reported that a single bone-marrow derived stem cell had the ability to engraft into numerous organs as well as having a “tremendous differentiative capacity” by adopting the phenotype of epithelial cells within the liver, lung, GI tract, and skin (20).
This initial report from Krause has led to extensive study of these cells in the heart (21–24), liver (25–27), brain (28), kidney (29), and endothelium (30). And while these initial results show great promise in providing new therapies for numerous diseases, these studies have also generated great controversy and highlight the discrepancies that exist within adult stem cell research. These controversies include the source and phenotype of the stem cells used, the experimental model of injury, the mechanism of effect, and the methods used to determine efficacy. While stem cell research in the lung has been less prolific than in cardio-vascular or neurologic diseases, the same controversies apply and will be discussed below.
STEM CELL THERAPIES TO PREVENT LUNG INJURY
The 2001 report from Krause et al. opened the door to the potential that there may be an ethically appealing option in using stem cells for tissue replacement. Based on their previous work showing the potential of CD34+ lin− for regenerating hepatocytes (27), Krause et al. extended their observation to the lung. Myelo-ablation was induced in female mice by total body irradiation of 1050–1100 cGy (an otherwise lethal dose if the bone marrow is not reconstituted; in most cases of irradiation the lungs are also injured). CD34+ lin− cells from male donor mice were administered intravenous (IV) (20). Fluorescent in situ hybridization (FISH) to track the Y-chromosome showed 20% of AEC being derived from a donor animal. Donor derived BMSC persisted up to 11 mo post-transplant (20).
Consistent with this first observation, Kotton et al. reported that plastic adherent MSCs (1–2 × 106 injected IV) from transgenic mice overexpressing lacZ, allowing tracking of the cells via X-gal staining, were able to engraft and form type I AEC in experimental lung fibrosis induced by intratracheal (IT) bleomycin (31). Bleomycin is one of the most extensively studied and reproducible experimental models for lung fibrosis. When bleomycin is given into the airway, it produces lung epithelial injury, followed by an inflammatory response over several days, followed by lung fibrosis that eventually resolves (32). Engrafted cells had morphologic features of type I AEC (i.e. flattened with ovoid nuclei bulging into alveolar lumen and adjacent to type II AEC) and expressed type I AEC specific markers such as Lycopersicon esculentum lectin and T1α (31). The proportion of donor derived MSCs contributing to the type I AEC population was not assessed. Interestingly however, all bleomycin injured-mice (4/4) showed engraftment when compared with PBS injected controls (2/9), suggesting that prior injury amplifies stem cell engraftment, as has been observed in other tissues (7). Furthermore, there were no donor-derived type II AECs, even in lungs harvested 1 and 2.5 d postinjection. In vitro, 10% of plastic adherent donor bone marrow cells cultured for one week expressed T1α and aquaporin 5, used as markers for type I AEC, (but are not solely confined to these cells) (33–35), but not surfactant protein C (SP-C), a type II AEC specific marker (36) suggesting that cultured bone marrow cells can serve as type I AEC precursors (31).
These two reports form the prototypes for most of the experiments on BMSC in the lung that have followed. In 2002, Theise et al. reported that donor-markers for either whole bone marrow or CD34+ lin− cells were detected in 14% of type II AEC after 1200 cGy total body irradiation (37). Engraftment was still present 6 months later (for total bone marrow injection) and 8 mo later for CD34+ lin− cells, detectable by FISH. In another study, administration of MAPC to nonobese diabetic/severe combined immunodeficiency (NOD/SCID) mice following mild irradiation of 250 cGy accounted for 4% of the alveolar epithelium assessed by β-galactosidase immunofluorescence (38). In another elegant study, Abe et al. generated parabiotic mice by surgically joining green fluorescent protein (GFP) transgenic mice and wild-type littermates (39). These mice develop a common circulation (approximately 50% green cells in blood) by 2 wk after surgery. The wild-type mouse was either uninjured or irradiated or received IT elastase (a well accepted emphysema model) or the combination of radiation with IT elastase injection. Radiation or the combination of radiation with elastase significantly increased the proportion of bright green cells in the lungs of wild-type mice. These cells resembled morphologically, interstitial monocytes/macrophages, subepithelial fibroblast-like interstitial cells, and type I AEC. Approximately 5 to 20% of lung fibroblasts primary cultured from injured wild-type mice expressed GFP.
Ortiz et al. used plastic adherent and purified, magnetic bead immunodepleted MSCs from male bleomycin-resistant BALB/c mice expressing CD34, CD45, and CD11b in bleomycin (4 U/kg)-induced pulmonary fibrosis in female bleomycin-sensitive C57BL/6 recipients (40). The purified MSCs (5 × 105) were injected into the jugular vein. Lung engraftment quantified by real-time PCR showed that male DNA accounted for 2.21 × 10−5% of the total lung DNA in control-treated mice but prior injury with bleomycin increased engraftment by 23-fold. FISH revealed that engrafted male cells were localized to areas of bleomycin-induced injury and exhibited an epithelium-like morphology, suggesting that stem cells homed specifically to sites of injury. Furthermore, immediate administration of MSCs was able to protect the lung from the bleomycin-induced inflammation, as assessed by collagen deposition, and matrix metalloproteinase (MMP) activation (40) as compared with animals that received MSCs one week following bleomycin, indicating the importance of timing of stem cell therapy, as observed in myocardial infarct (41). The low numbers of donor-derived cells engrafting the lung did not appear sufficient to account for the therapeutic response, suggesting that donor stem cells may have other local effects.
Rojas et al. used a model in which before bleomycin injury, the animals also underwent myelosuppression via a single administration of busulfan (42). Myelosuppression increased the susceptibility to bleomycin injury, suggesting that an intact bone marrow serves to limit the extent of lung injury. After this suppression of the bone marrow, plastic adherent and immuno-depleted MSCs were given IV MSCs administration improved survival when compared with untreated animals. Furthermore, within the MSC administered group, there were a “substantial number” of donor cells within the lungs 2 wk following bleomycin insult with characteristics of AEC I and II, fibroblasts, and endothelial cells. In the bleomycin+busulfan group, 29% of cells were derived from donor MSCs. Interestingly, circulating levels of granulocyte-macrophage colony-stimulating factor (GM-CSF) and granulocyte colony stimulating factor (G-CSF) (factors known to stimulate stem cell mobilization from the bone marrow), were higher in bleomycin-injured animals receiving MSC. This suggests that, besides lung engraftment, humoral factors may also contribute to stem cell-induced tissue protection. This is consistent with the greater protection conferred by stem cell transplant in bone marrow sufficient (no busulfan) animals.
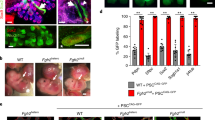
Preliminary data in oxygen-induced experimental BPD in newborn rats also suggest a protective role of MSC. Rats exposed to 95% oxygen from birth to 14 d postnatal during the alveolar period of lung development have an irreversible arrest in lung development (43). In this preliminary study, MSC were given IT, a situation that is clinically relevant since premature infants at risk are routinely given surfactant via this route and which has been used successfully with other experimental therapies (44). CFSE (a green fluorescent marker)-labeled MSC given at 4 d postnatal in hyperoxic-exposed animals prevented stunted alveolar growth, engrafted and expressed the type II AEC specific marker SP-C (unpublished data).
These studies demonstrate the potential of BMSC to home to the injured lung, engraft, and adopt the phenotype of one or many of the lung cells. These reports also illustrate the numerous methods that exist in culturing and selecting BMSC (Table 2). The differences in experimental design and the numerous techniques to determine treatment efficacy (engraftment, differentiation, improvement in lung histology) further render the interpretation of these results difficult.
Furthermore, there are numerous studies that do not support the plasticity of adult stem cells in different organs. Wagers et al. attempted to determine the fate of “prospectively isolated, long-term reconstituting HSCs” by using either a chimeric animal, produced via bone marrow ablation and reconstitution with GFP HSCs, or using a parabiotic model, joining the circulation of a transgenic GFP mouse with the circulation of a wild type mouse (45). While the BM ablated group showed robust reconstitution of circulating HSCs, and the parabiotic animals had robust hematopoietic chimerism, there was little evidence for stem cell engraftment and transdifferentiation. Only one cell of 13.2 × 106 cells examined within the brain, and seven cells of 4.7 × 105 cells examined within the liver co-expressed the donor marker GFP as well as a tissue specific marker (albumin for hepatocytes) in the BM ablation group (45). There was no evidence for engraftment and transdifferentiation in the lung. Moreover, the parabiotic model had no indication of HSC engraftment and transdifferentation in any of the tissues analyzed (45).
In addition, two recent reports have challenged the engraftment potential of adult-derived stem cells in the lung. These two studies take advantage of transgenic mouse that express a marker protein ubiquitously or under the control of the type II AEC specific promoter SP-C (46, 47). Chang et al. transplanted bone marrow (2.0 × 107 cells) from transgenic mice expressing the LacZ or eGFP gene ubiquitously (under the control of the actin promoter), or under the control of the human SP-C promoter into irradiated, neonatal mice. The lungs of recipients transplanted with bone marrow from transgenic mice that ubiquitously express eGFP or LacZ showed cells whose morphology and location were compatible with type II AEC (46). These green cells also co-localized with pro-SP-C. These initial results indicated that the eGFP BMSC were contributing to the alveolar epithelium. Flow cytometric analysis of SP-C immunostained cells with eGFP indicated that eGFP-fluorescent cells accounted for 50–55% of all lung cells, as well as 70% of type II AECs 2 wk after bone marrow transplantation (46). One month post-transplantation, eGFP+ cells only comprised 2-25% of total lung cells with 0% to 8% of type II AECs being donor-derived. However, upon analysis with cyto-centrifugation, the phenotype of the eGFP+ SP-C+ cells displayed a small, round cell type with a scant cytoplasm which is not congruent with the normal type II AEC phenotype of larger, cuboidal cells with an abundant cytoplasm (48). Moreover, mice that received SP-C-eGFP bone marrow transplant showed no eGFP expression, indicating that the transplanted cells are not adopting the type II AEC phenotype (46). This result led to retrospectively analyze the lungs from mice receiving actin-eGFP bone marrow transplantation using deconvolution microscopy. Deconvolution microscopy was able to generate a three dimensional image of the lung allowing to determine that the co-expression of SP-C and eGFP was a false positive: the pro-SP-C signal resided just outside the eGFP+ cells, with a difference between the two signals less than 300 nm, and this phenomenon was not apparent until the three dimensional image was viewed from multiple angles (46).
Kotton et al. also used SP-C-eGFP mice, but investigated both unfractionated BM as well as BM-derived SP cells (47). SP cells were purified from the femurs, tibias, and iliac crests and identified using a model of Hoechst dye efflux. These cells are enriched for HSC activity. Adult mice underwent myeloablation via either a single dose of 11 or 12 Gy radiation or two doses of 7 Gy (total of 14 Gy). The bone marrow was then reconstituted with either a whole bone marrow transplant or transplantation of the highly enriched HSCs SP cells from SP-C-eGFP donor mice. Three months post-transplantation, with robust blood reconstitution, the mice were challenged with a bleomycin injury (0.05 units) and engraftment was assessed 1 mo post-transplant. Using three antibody independent assays, fluorescent activated cell sorting (FACS), fluorescent microscopy, and real time PCR, the authors showed no evidence of donor cells becoming type II AECs (47).
In humans, BMSC repopulation also seems to contribute minimally to the type II AECs after cross-gender lung transplantation (49). Sequential immunohistochemistry and FISH performed on lung biopsy specimens from male recipients of transplanted lungs from female donors showed Y-chromosome–containing type II AEC in 9 of 25 biopsy specimens from five of seven gender mismatched male lung transplant recipients, that accounted for 0% to 0.553% of type II AEC (49). The number of type II AEC of male karyotype showed a statistically significant relationship to the cumulative number of episodes of acute cellular rejection. This study also suggests that BMSC contribute minimally to the type II AEC proliferation that is often present in these patients as a sequela to alveolar injury (49).
STEM CELL THERAPIES TO REPLACE DEFICIENT GENES IN THE LUNG
The use of stem cells for CF is still at the conceptual stage, therefore there are currently very few reports on the use of adult derived stem cells for CF. However, the idea that adult derived stem cells could be used as a vehicle for gene therapy is very appealing. Firstly, this method of administration would give the physician a controlled method of administering the corrected gene, circumventing some of the problems that have been seen using viral mediated gene therapy (50). Secondly, a stem cell could potentially provide a synergistic mechanism. Not only would the stem cell deliver the corrected CFTR gene to the lung of a CF patient, but these cells could also help replenish destroyed tissue.
Grove et al. first showed the potential for a marrow derived cell as a vehicle for gene delivery to the pulmonary epithelium (51). MSCs were expanded in vitro after harvest from the bone marrow by being grown in a defined basal bone marrow media supplemented with human IL-6 (IL-6), murine IL-3, murine stem cell factor, and polybrene. These cells were then transduced with a retroviral vector (MND-eGFP-SN) that has been optimized for long-term expression of eGFP in other cell lines. Following transduction, the eGFP marrow stem cells were then injected via the tail vein into mice that had received 600 cGY of radiation for 2 consecutive days. This resulted in 1% to 7% of AEC derived from donor eGFP stem cells (51).
More recently, the possibility of transforming in vitro MSCs from CF patients with a viral transcript to correct the defective CFTR gene was reported (52). MSCs were first obtained from healthy volunteers as well as CF volunteers with the ΔF508 homozygous mutation. MSCs expressing GFP, co-cultured with human airway epithelium, adopted a cuboidal or columnar shape similar to epithelial cells, as well as the expression of cytokeratin-18 (CK-18) a marker of epithelial cells. When directly mixed with primary human AECs, control MSC expressed the tight junction protein occludin. Moreover, FACS was used to isolate the GFP+ cells from the co-culture system. These cells, when co-cultured with normal human AEC or with AEC from ΔF508 homozygous patients, expressed wild type CFTR, which were either not detected in MSCs before or that were not co-cultured. These experiments strongly suggest that MSCs, when exposed to AECs, are able to adopt the phenotype of AECs and show the importance of the microenvironment in inducing tissue-specific transdifferentiation. While these results are very promising and lend credence to the ability of MSC transdifferentiation into AEC, the true potential for MSC in CF are as vehicles for gene delivery. MSCs from 3 ΔF508 homozygous patients were transduced with a viral vector for expression of CFTR (vesicular stomatitis virus glycoprotein pseudotyped Moloney murine leukemia virus-CFTR-neo). In this construct, the human CFTR gene was linked by internal ribosome entry site to the neo gene to allow for selection of the corrected MSCs based on G418-resistance (a sulphate antibiotic) and drug-resistant stem cell expansion. Insertion of the gene had no effect on the multitpotency (based on adipogenic, chondrogenic, and osteogenic cell differentiation), doubling times, and numbers of colony-forming units (CFUs) compared with control MSCs. ΔF508 corrected MSCs showed improved chloride efflux in vitro. Furthermore, after co-culture with AECs, the corrected ΔF508 MSCs were able to secrete a significantly larger amount of chloride when compared with uncorrected MSCs from ΔF508 CF patients. Corrected ΔF508 MSCs responded to IBMX and forskolin (adenylate cyclase activators) to a larger degree than the uncorrected ΔF508 MSCs (52). While this in vitro proof of concept study is very exciting, definitive answers cannot be concluded until this is tested in vivo in an animal model of CF.
There is one report to date attempting to use adult BMSC for CF in vivo. In this report, Loi et al. used both plastic adherent MSCs and total bone marrow harvested from transgenic mice over-expressing GFP (53). The authors subsequently ablated the bone marrow of CFTR knockout mice using 800 rads total body irradiation and injected either the MSCs (106 cells/mouse) or total bone marrow (20 × 106 cells/mouse) via the tail vein. They also used an intraperitoneal dose of naphthalene (275 mg/kg) either three days before MSC administration or one month after bone marrow reconstitution with total bone marrow cells to induce lung injury and stimulate migration of the transplanted bone marrow cells to the lung. Stromal marrow cells were able to engraft into the alveolar epithelium and to confer CFTR mRNA to the knock-out mice, but the engraftment occurred at such a low rate (0.025% chimeric airway epithelial cells, of which 0.01% expressed CFTR protein) that it is unlikely that this method would correct the trans-epithelial chloride deficit. Naphthalene-induced airway remodeling did not significantly increase the number of chimeric airway epithelial cells expressing CFTR.
These two reports highlight the potential for BM-derived stem cell based gene therapy in CF and the need for new strategies for enhancing airway epithelial engraftment to exert a beneficial effect.
CONCLUSION
The use of stem cells in the lung is at the crossroads of understanding. Over the last decade, numerous studies have demonstrated the ability of adult BM-derived cells to differentiate into non-hematopoietic lineages, including neural, skeletal muscle, hepatic, cardiac and vascular lineages and to repair these tissues. With regard to lung repair, the literature is sparser. Initial promising reports showing adult BM-derived cell homing, engraftment, and lung phenotype adoption are now challenged. This highlights the need for more reliable techniques and assays to assess adult BM-derived cells lung engraftment and transdifferentiation. Other challenges before moving to the clinical application with this promising therapeutic strategy include: improved characterization of putative BM-derived stem cells, determining mechanisms of homing, engraftment and transdifferentiation, as well as the alternate mechanisms of action beyond pure tissue replacement, rigorous assessment of therapeutic success combining lung histology and function, and lastly and more importantly determining the long term safety of these MSCs. The potential for teratomas and other cancers is too high a risk without certain evidence that the exogenous administration of adult BM-derived stem cells is safe.
Abbreviations
- AEC:
-
alveolar epithelial cell;
- BMSC:
-
bone marrow-derived stem cell;
- BPD:
-
bronchopulmonary dysplasia;
- CF:
-
cystic fibrosis;
- CFTR:
-
cystic fibrosis transmembrane conductance regulator;
- eGFP:
-
enhanced green fluorescent protein;
- ES cell:
-
embryonic stem cell;
- GFP:
-
green fluorescent protein;
- HSC:
-
hematopoietic stem cell;
- MSC:
-
mesenchymal stem cell;
- SP cell:
-
sidepopulation cell;
- SP-C:
-
surfactant protein C
References
Abman SH 2001 Bronchopulmonary dysplasia: “a vascular hypothesis”. Am J Respir Crit Care Med 164: 1755–1756
Jobe AJ 1999 The new BPD: an arrest of lung development. Pediatr Res 46: 641–643
Orenstein DM, Stern RC, Rosenstein BJ 2000 Cystic Fibrosis: Medical Care. Lippincott Williams & Wilkins, Philadelphia, pp 1–21.
Vankeerberghen A, Cuppens H, Cassiman JJ 2002 The cystic fibrosis transmembrane conductance regulator: an intriguing protein with pleiotropic functions. J Cyst Fibros 1: 13–29
Evans MJ, Kaufman MH 1981 Establishment in culture of pluripotential cells from mouse embryos. Nature 292: 154–156
McLaren A 2001 Ethical and social considerations of stem cell research. Nature 414: 129–131
Hatch HM, Zheng D, Jorgensen ML, Petersen BE 2002 SDF-1alpha/CXCR4: a mechanism for hepatic oval cell activation and bone marrow stem cell recruitment to the injured liver of rats. Cloning Stem Cells 4: 339–351
Michalopoulos GK, DeFrances MC 1997 Liver regeneration. Science 276: 60–66
Mason RJ, Williams MC, Moses HL, Mohla S, Berberich MA 1997 Stem cells in lung development, disease, and therapy. Am J Respir Cell Mol Biol 16: 355–363
Warburton D, Wuenschell C, Flores-Delgado G, Anderson K 1998 Commitment and differentiation of lung cell lineages. Biochem Cell Biol 76: 971–995
Pitt BR, Ortiz LA 2004 Stem cells in lung biology. Am J Physiol Lung Cell Mol Physiol 286: L621–L623
Driscoll B, Buckley S, Bui KC, Anderson KD, Warburton D 2000 Telomerase in alveolar epithelial development and repair. Am J Physiol Lung Cell Mol Physiol 279: L1191–L1198
Reddy R, Buckley S, Doerken M, Barsky L, Weinberg K, Anderson KD, Warburton D, Driscoll B 2004 Isolation of a putative progenitor subpopulation of alveolar epithelial type 2 cells. Am J Physiol Lung Cell Mol Physiol 286: L658–L667
Wagers AJ, Weissman IL 2004 Plasticity of adult stem cells. Cell 116: 639–648
Blau HM, Brazelton TR, Weimann JM 2001 The evolving concept of a stem cell: entity or function?. Cell 105: 829–841
Friedenstein AJ, Gorskaja JF, Kulagina NN 1976 Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol 4: 267–274
Gronthos S, Zannettino AC, Hay SJ, Shi S, Graves SE, Kortesidis A, Simmons PJ 2003 Molecular and cellular characterisation of highly purified stromal stem cells derived from human bone marrow. J Cell Sci 116: 1827–1835
Jones EA, Kinsey SE, English A, Jones RA, Straszynski L, Meredith DM, Markham AF, Jack A, Emery P, McGonagle D 2002 Isolation and characterization of bone marrow multipotential mesenchymal progenitor cells. Arthritis Rheum 46: 3349–3360
Tropel P, Noel D, Platet N, Legrand P, Benabid AL, Berger F 2004 Isolation and characterisation of mesenchymal stem cells from adult mouse bone marrow. Exp Cell Res 295: 395–406
Krause DS, Theise ND, Collector MI, Henegariu O, Hwang S, Gardner R, Neutzel S, Sharkis SJ 2001 Multi-organ, multi-lineage engraftment by a single bone marrow-derived stem Cell. Cell 105: 369–377
Amado LC, Saliaris AP, Schuleri KH, St John M, Xie JS, Cattaneo S, Durand DJ, Fitton T, Kuang JQ, Stewart G, Lehrke S, Baumgartner WW, Martin BJ, Heldman AW, Hare JM 2005 Cardiac repair with intramyocardial injection of allogeneic mesenchymal stem cells after myocardial infarction. Proc Natl Acad Sci U S A 102: 11474–11479
Kajstura J, Rota M, Whang B, Cascapera S, Hosoda T, Bearzi C, Nurzynska D, Kasahara H, Zias E, Bonafe M, Nadal-Ginard B, Torella D, Nascimbene A, Quaini F, Urbanek K, Leri A, Anversa P 2005 Bone marrow cells differentiate in cardiac cell lineages after infarction independently of cell fusion. Circ Res 96: 127–137
Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, Pickel J, McKay R, Nadal-Ginard B, Bodine DM, Leri A, Anversa P 2001 Bone marrow cells regenerate infarcted myocardium. Nature 410: 701–705
Yoon YS, Wecker A, Heyd L, Park JS, Tkebuchava T, Kusano K, Hanley A, Scadova H, Qin G, Cha DH, Johnson KL, Aikawa R, Asahara T, Losordo DW 2005 Clonally expanded novel multipotent stem cells from human bone marrow regenerate myocardium after myocardial infarction. J Clin Invest 115: 326–338
Jang YY, Collector MI, Baylin SB, Diehl AM, Sharkis SJ 2004 Hematopoietic stem cells convert into liver cells within days without fusion. Nat Cell Biol 6: 532–539
Petersen BE, Bowen WC, Patrene KD, Mars WM, Sullivan AK, Murase N, Boggs SS, Greenberger JS, Goff JP 1999 Bone marrow as a potential source of hepatic oval cells. Science 284: 1168–1170
Theise ND, Badve S, Saxena R, Henegariu O, Sell S, Crawford JM, Krause DS 2000 Derivation of hepatocytes from bone marrow cells in mice after radiation-induced myeloablation. Hepatology 31: 235–240
Kopen GC, Prockop DJ, Phinney DG 1999 Marrow stromal cells migrate throughout forebrain and cerebellum, and they differentiate into astrocytes after injection into neonatal mouse brains. Proc Natl Acad Sci U S A 96: 10711–10716
Kale S, Karihaloo A, Clark PR, Kashgarian M, Krause DS, Cantley LG 2003 Bone marrow stem cells contribute to repair of the ischemically injured renal tubule. J Clin Invest 112: 42–49
Zhao YD, Courtman DW, Deng Y, Kugathasan L, Zhang Q, Stewart DJ 2005 Rescue of monocrotaline-induced pulmonary arterial hypertension using bone marrow-derived endothelial-like progenitor cells: efficacy of combined cell and eNOS gene therapy in established disease. Circ Res 96: 442–450
Kotton DN, Ma BY, Cardoso WV, Sanderson EA, Summer RS, Williams MC, Fine A 2001 Bone marrow-derived cells as progenitors of lung alveolar epithelium. Development 128: 5181–5188
Jones AW, Reeve NL 1978 Ultrastructural study of bleomycin-induced pulmonary changes in mice. J Pathol 124: 227–233
Krane CM, Fortner CN, Hand AR, McGraw DW, Lorenz JN, Wert SE, Towne JE, Paul RJ, Whitsett JA, Menon AG 2001 Aquaporin 5-deficient mouse lungs are hyperresponsive to cholinergic stimulation. Proc Natl Acad Sci U S A 98: 14114–14119
Rishi AK, Joyce-Brady M, Fisher J, Dobbs LG, Floros J, VanderSpek J, Brody JS, Williams MC 1995 Cloning, characterization, and development expression of a rat lung alveolar type I cell gene in embryonic endodermal and neural derivatives. Dev Biol 167: 294–306
Williams MC 2003 Alveolar type I cells: molecular phenotype and development. Annu Rev Physiol 65: 669–695
Horowitz S, Watkins RH, Auten RL, Mercier CE, Cheng ER 1991 Differential accumulation of surfactant protein A, B, and C mRNAs in two epithelial cell types of hyperoxic lung. Am J Respir Cell Mol Biol 5: 511–515
Theise ND, Henegariu O, Grove J, Jagirdar J, Kao PN, Crawford JM, Badve S, Saxena R, Krause DS 2002 Radiation pneumonitis in mice: a severe injury model for pneumocyte engraftment from bone marrow. Exp Hematol 30: 1333–1338
Jiang Y, Jahagirdar BN, Reinhardt RL, Schwartz RE, Keene CD, Ortiz-Gonzalez XR, Reyes M, Lenvik T, Lund T, Blackstad M, Du J, Aldrich S, Lisberg A, Low WC, Largaespada DA, Verfaillie CM 2002 Pluripotency of mesenchymal stem cells derived from adult marrow. Nature 418: 41–49
Abe S, Lauby G, Boyer C, Rennard SI, Sharp JG 2003 Transplanted BM and BM side population cells contribute progeny to the lung and liver in irradiated mice. Cytotherapy 5: 523–533
Ortiz LA, Gambelli F, McBride C, Gaupp D, Baddoo M, Kaminski N, Phinney DG 2003 Mesenchymal stem cell engraftment in lung is enhanced in response to bleomycin exposure and ameliorates its fibrotic effects. Proc Natl Acad Sci U S A 100: 8407–8411
Vandervelde S, van Luyn MJ, Tio RA, Harmsen MC 2005 Signaling factors in stem cell-mediated repair of infarcted myocardium. J Mol Cell Cardiol 39: 363–376
Rojas M, Xu J, Woods CR, Mora AL, Spears W, Roman J, Brigham KL 2005 Bone marrow-derived mesenchymal stem cells in repair of the injured lung. Am J Respir Cell Mol Biol 33: 145–152
Wilson WL, Mullen M, Olley PM, Rabinovitch M 1985 Hyperoxia-induced pulmonary vascular and lung abnormalities in young rats and potential for recovery. Pediatr Res 19: 1059–1067
Thebaud B, Ladha F, Michelakis ED, Sawicka M, Thurston G, Eaton F, Hashimoto K, Harry G, Haromy A, Korbutt G, Archer SL 2005 Vascular endothelial growth factor gene therapy increases survival, promotes lung angiogenesis, and prevents alveolar damage in hyperoxia-induced lung injury: evidence that angiogenesis participates in alveolarization. Circulation 112: 2477–2486
Wagers AJ, Sherwood RI, Christensen JL, Weissman IL 2002 Little evidence for developmental plasticity of adult hematopoietic stem cells. Science 297: 2256–2259
Chang JC, Summer R, Sun X, Fitzsimmons K, Fine A 2005 Evidence that bone marrow cells do not contribute to the alveolar epithelium. Am J Respir Cell Mol Biol 33: 335–342
Kotton DN, Fabian AJ, Mulligan RC 2005 Failure of bone marrow to reconstitute lung epithelium. Am J Respir Cell Mol Biol 33: 328–334
Shannon JM, Mason RJ, Jennings SD 1987 Functional differentiation of alveolar type II epithelial cells in vitro: effects of cell shape, cell-matrix interactions and cell-cell interactions. Biochim Biophys Acta 931: 143–156
Zander DS, Baz MA, Cogle CR, Visner GA, Theise ND, Crawford JM 2005 Bone marrow-derived stem-cell repopulation contributes minimally to the Type II pneumocyte pool in transplanted human lungs. Transplantation 80: 206–212
Davies JC, Alton EW 2005 Airway gene therapy. Adv Genet 54: 291–314
Grove JE, Lutzko C, Priller J, Henegariu O, Theise ND, Kohn DB, Krause DS 2002 Marrow-derived cells as vehicles for delivery of gene therapy to pulmonary epithelium. Am J Respir Cell Mol Biol 27: 645–651
Wang G, Bunnell BA, Painter RG, Quiniones BC, Tom S, Lanson NA, Spees JL, Bertucci D, Peister A, Weiss DJ, Valentine VG, Prockop DJ, Kolls JK 2005 Adult stem cells from bone marrow stroma differentiate into airway epithelial cells: potential therapy for cystic fibrosis. Proc Natl Acad Sci U S A 102: 186–191
Loi R, Beckett T, Goncz KK, Suratt BT, Weiss DJ 2006 Limited Restoration of cystic fibrosis lung epithelium in vivo with adult marrow derived cells. Am J Respir Crit Care Med 173: 171–179
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Thébaud is supported by the Canada Foundation for Innovation, the Alberta Heart and Stroke Foundation (H&SF), the Alberta Hertiage Foundation for Medical Research (AHFMR), the Canadian Institutes for Health Research (CIHR) and the Stollery Children's Hospital Foundation.Tim van Haaften is supported by the CIHR-funded Torch (Tomorrow's Research Cardiovascular Health Professionals) and MFN (Maternal-Fetal-Newborn Health) programs.
Rights and permissions
About this article
Cite this article
Van Haaften, T., Thébaud, B. Adult Bone Marrow-Derived Stem Cells for the Lung: Implications for Pediatric Lung Diseases. Pediatr Res 59 (Suppl 4), 94–99 (2006). https://doi.org/10.1203/01.pdr.0000203550.50258.5a
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000203550.50258.5a
This article is cited by
-
Bone marrow stem cells accelerate lung maturation and prevent the LPS-induced delay of morphological and functional fetal lung development in the presence of ErbB4
Cell and Tissue Research (2020)
-
Therapeutic potential of mesenchymal stem cell transplantation in a nitrofen-induced congenital diaphragmatic hernia rat model
Pediatric Surgery International (2014)
-
Prevention and Treatment of Bronchopulmonary Dysplasia: Contemporary Status and Future Outlook
Lung (2008)
-
Bone Marrow-Derived Cells Participate in Stromal Remodeling of the Lung Following Acute Bacterial Pneumonia in Mice
Lung (2008)
-
New Insights into the Pathogenesis and Treatment of Idiopathic Pulmonary Fibrosis: A Potential Role for Stem Cells in the Lung Parenchyma and Implications for Therapy
Pharmaceutical Research (2007)