Abstract
Epilepsy is a disorder in which the balance between cerebral excitability and inhibition is tipped toward uncontrolled excitability. There is now clear evidence that there are distinct differences between the immature and mature brain in the pathophysiology and consequences of seizures. Both the enhanced excitability of the immature brain compared with the mature brain and the unique pathologic consequences of seizures are related to the sequential development and expression of essential signaling pathways. Although the immature brain is less vulnerable than the mature brain to seizure-induced cell death, seizures in the developing brain can result in irreversible alterations in neuronal connectivity. Developing novel strategies to treat and avert the consequences of seizures in children will require further understanding of the unique mechanisms of seizure initiation and propagation in the immature brain.
Similar content being viewed by others
Main
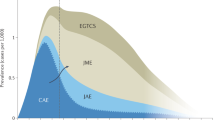
As originally described by J. Hughlings Jackson in 1870, a seizure is an “excessive discharge of nerve tissue on muscle”(1). Jackson went on to say that “this discharge occurs in all degrees, it occurs with all sorts of conditions of ill health, at all ages, and under innumerable circumstances.” These comments by Jackson are as true now as they were 130 years ago. Epileptic seizures are one of the most common, and frightening, neurologic conditions that occur in children. The incidence of seizures in children is significantly higher than in adults, with the highest incidence during the first year of life (2). Although there are many common features of the disorder across age groups, it has become clear that there are also significant differences between young children and adults in both the pathogenesis and consequences of epilepsy.
Partial seizures, the most common seizure type to occur in both children and adults, will be reviewed in this article. The pathogenesis and consequences of recurrent brief seizures and status epilepticus will be reviewed. The mechanisms of generalized seizures, such as absences, are quite different and will not be reviewed here. Interested readers are referred to a review article by Snead (3).
Basic mechanisms of partial seizures. The core physiologic feature of epileptic seizures is hyperexcitability of CNS neurons. When a sufficient number of neurons synchronously depolarize and generate action potentials, a seizure begins. Both the location of the initial event and the propagation pattern of the discharge will determine the behavioral changes that occur. The hallmark of this synchronous discharge of neurons in the epileptic focus is the PDS, which is a large and sustained depolarization of the neuron. During a PDS, the cell membrane near the soma undergoes a high-voltage (approximately 10–15 mV) and long (100–200 ms) depolarization. This depolarization is much longer than the depolarization seen with normal EPSP, in which the duration is in the range of 10–16 ms. This long depolarization has the effect of generating a train of action potentials that are conducted away from the soma along the axon of the neuron. The PDS would correspond to a spike on the EEG (Fig. 1). The PDS is followed by a large hyperpolarization, which serves to limit the duration of interictal paroxysms. This hyperpolarization is generated by current through a number of ionic channels, including GABA and Ca2+-activated K+ channels. During a seizure, the epileptic neurons undergo a prolonged depolarization with continuous bursts of action potentials without an intervening repolarization. The behavioral correlate of this prolonged depolarization is the tonic phase of the seizure. An EEG recorded at this time on the surface of the brain would demonstrate continuous spikes. During the next stage, large inhibitory potentials occur and alternate with recurrent rhythmic PDS. This pattern coincides with the clonic stage of the seizure. During this stage of the seizure, generalized spike-and-wave discharges would be present on the EEG.
Diagram of cellular events corresponding to behavioral and electroencephalographic changes during the interictal and ictal periods. The bottom diagram demonstrates the PDS, a large and prolonged depolarization with generation of action potential spikes (arrow)(VM is the voltage across the membrane). The horizontal bars at the bottom of the figure represent the period during which the particular channel is open (gNa+, gCa2+, gK+ refer to conductances of the ions across the membrane), the beginning of the bar indicates the opening of the channel and the end of the bar its closure. At the onset of the PDS, the AMPA channel opens, which allows Na+ to enter the cell and begin the process of depolarization. The NMDA channel then opens allowing both Na+ and Ca2+ to enter. Following depolarization, there is opening of the K+ and activation of GABA channels with Cl– entering the cell. Both the influx of Cl– and efflux of K+ lead to hyperpolarization on the cell. The PDS corresponds to a spike or sharp wave on the EEG (top of diagram). During an actual seizure (ictus), there is a failure of adequate inhibitory mechanisms and no hyperpolarization following the PDS occurs. This prolonged depolarization with action potentials corresponds to the tonic phase of the seizure. When inhibition is reinitiated, there are brief periods of depolarization following by hyperpolarization. This period corresponds to the clonic phase of the seizure. Modified from Kandel ER, Schwartz JH, Jessell TM 2000 Principles of Neural Science, 4th Ed. McGraw-Hill, with permission.
Although the PDS has been useful in increasing our understanding of cellular physiology in epilepsy, the PDS can be recorded in only a limited number of models. However, in virtually all animal models of epilepsy there is some form of cellular “burst” discharge. Presumably, it is this enhanced cell excitability, or decreased inhibition, and synchrony that are responsible for both the “epileptic” EEG pattern and behavioral change. Although it is clear that seizures begin at the cellular level, epilepsy is a disorder of a network of neurons that synchronously discharge together.
The mechanisms responsible for the transition from interictal to ictal activity are not entirely understood. Factors such as a change in the ionic microenvironment of the epileptic focus, decreases in GABAergic function, increases in synaptic excitation, alteration in K+ or Ca2+ currents, or changes in the extracellular ion concentrations may trigger the prolonged depolarization. Even less is known about why seizures stop. Seizures may end when there is activation of inhibitory circuits in the neuronal network or changes in the ionic environment, such as reduction of extracellular K+, elimination of intracellular Ca2+, or reduced release of glutamate.
Seizures, brain damage and plasticity in the adult brain. It has long been known that severe seizures are associated with brain damage and cell loss in children. Studies using animal models have enabled investigators to determine some of the mechanisms involved and their long-term consequences on the network. Although seizures can induce changes in multiple areas of the brain, the hippocampus has been particularly well studied inasmuch as this is the brain area that is frequently the most vulnerable to seizure-induced injury. In the adult animal, status epilepticus causes neuronal loss in hippocampal fields CA1, CA3, dentate granule cell layer, and the dentate hilus (4–8). Cellular damage occurs from excessive excitatory neurotransmitter release, which activates NMDA receptors and voltage-activated Ca2+ channels, allowing Ca2+ to enter the cell. Ca2+ and other ionic changes result in a cascade of biochemical changes eventually resulting in cell death (9). High Ca2+ leads to generation of reactive oxygen species via activation of nitric oxide synthase, uncouples oxidative phosphorylation in mitochondria, and activates a large range of enzymes, such as lipases, proteases, endonucleases, and other catabolic enzymes that collectively have adverse consequences for cell function (10).
Seizures in the adult brain lead to various forms of synaptic plasticity, including long-term potentiation of synaptic responses, a process that is reminiscent of that occurring in memory processes (11). This is followed by alterations in the cortical network that result in a reduction of seizure threshold. Seizures have been shown to activate hundreds of genes that lead to axonal growth and neosynaptogenesis (reviewed in (12)). Thus, prolonged seizures can cause synaptic reorganization with aberrant growth (sprouting) of granule cell axons (the so-called mossy fibers) in the supragranular zone of the fascia dentata and infrapyramidale region of CA3 in the supragranular zone of the fascia dentata (13, 14) and infrapyramidale region of CA3 (14). Because glutamate is the neurotransmitter of the mossy fibers, it is likely that this sprouting results in an excessive degree of excitation of dentate granule cells and, perhaps more importantly, CA3 pyramidal neurons. A further indication of the role of excitability in the generation of synaptic plasticity is the observation that blocking one of the glutamate subreceptors (NMDA) retards the development of mossy fiber development (15, 16). Sprouting and neosynapse formation occur in other brain regions—notably the CA1 pyramidal neurons, where it has been recently shown that newly formed synapses produce an enhanced frequency of glutamatergic spontaneous synaptic currents (17). Therefore, these alterations appear to be a general response of cortical networks to hyperactivity; the consequences of the seizures far outlasting the effects of the initiating event.
Immature neurons are more susceptible to seizure generation but less vulnerable to its pathologic consequences. It is well recognized that children are at higher risk for seizures than adults. In addition to the higher incidence of epilepsy in children than adults, precipitating factors such as fever are far more likely to induce a seizure in a young child than in an adult. Children also have a significantly higher likelihood of entering remission than adults, further suggesting that the brain becomes less excitable with age. Results from animal studies parallel clinical studies demonstrating that the immature brain is more susceptible to seizures than the adult brain. Kindling, a process in which recurrent electrical stimulations that initially result only in brief electrical discharges and mild behavioral changes but result progressively in more prolonged and intense electrical and behavioral seizures, occurs at all ages. Young animals kindle more rapidly than mature animals (18). In addition, a shorter period of postictal refractoriness in young animals leads to a quick progression through early stages of kindling and results in rapid generalization of seizures (19). Immature rats are more likely to develop seizures with hypoxia than mature rats (20). Similarly, the dosage of the convulsant kainic acid needed to induce seizures in immature animals is significantly lower than that required to induce seizures of similar intensity and duration in the mature rat (21).
Although the threshold for seizure generation is lower in the immature brain than in the adult brain, developing neurons are less vulnerable, in terms of neuronal damage and cell loss, than adult neurons to a wide variety of pathologic insults. For example, immature hippocampal neurons will continue responding to synaptic stimuli in a fully anoxic environment for longer durations than adult ones; likewise, longer anoxic episodes are required to irreversibly destroy neural pathways in young animals (22). Young animals are less vulnerable to cell loss following a prolonged seizure than mature animals (21, 23–28). Likewise, sprouting of mossy fibers is less prominent following prolonged seizures in young animals than seizures of similar duration in older animals (29, 30).
The immature brain appears to be more “resistant” to the toxic effects of glutamate than the mature brain (31–33). Marks et al.(33) found that the degree of Ca2+ entry into the hippocampal subfield CA1 and subsequent damage was directly related to age. In postnatal d 1–3 neurons glutamate increased intracellular Ca2+ minimally, whereas in postnatal d 21–23 neurons glutamate resulted in marked increases in intracellular Ca2+ and caused severe swelling of the cell and retraction of dendrites into the soma of the neuron. This relative resistance is thought to be due to the smaller density of active synapses, lower energy consumption, and, in general, the relative immaturity of biochemical cascades that lead to cell death following insults.
Behavioral consequences following status epilepticus are also related to age of the animal at the time of the status; adult animals surviving status epilepticus have significant deficits in learning, memory, and behavior (27) whereas young rats following status epilepticus have fewer deficits in learning, memory, and behavior (27, 34). Likewise, spontaneous seizures following status epilepticus are more likely to occur in older animals experiencing status epilepticus than in younger animals (35–37).
Why is the immature brain so prone to seizure generation? The enhanced excitability of the immature brain compared with the mature brain, like the pathologic consequences of seizures, is related to the sequential development and expression of essential signaling pathways. Thus, in the adult brain, glutamate is the primary excitatory neurotransmitter and GABA is the principal inhibitory transmitter. Synaptic transmission is mediated by glutamate that is released from the pyramidal neurons and depolarizes and excites the target neurons via ionotropic receptors [NMDA (AMPA) and KA]. Although all of the glutamate subreceptors respond to glutamate, they have individual characteristics. The AMPA receptor rapidly responds to glutamate with opening of the channel to allow Na+ to enter the cell and depolarize the membrane. The NMDA channel has characteristics of both a neurotransmitter or ligand-activated and voltage-sensitive channel. Mg2+ sits in the channel blocking the flow of ions. Only with depolarization of the membrane is Mg2+ displaced and Na+ and Ca2+ ions are able to cross the channel. The rise of intracellular Ca2+ is an essential signal for memory processes, hence NMDA receptor plays an important role in learning and plasticity. Activation of GABAA and GABAB results in hyperpolarization of the membrane and a reduction of excitability and action potential generation.
During development, these receptors are not functionally expressed simultaneously, but rather in a sequence of GABAA-NMDA-AMPA. Recently it was found that, at birth, pyramidal neurons of the CA1 region of the hippocampus are of three types. They are silent (no synaptic currents), express only GABAergic currents, or express GABA and glutamatergic currents (Fig. 2). These three different types of CA1 neurons have different morphologic appearances: silent neurons have a soma and an axon, but no dendrites; GABA only neurons have a soma, axon, and small dendrite; and GABA and glutamate neurons have a soma, axon, and extended apical and basal dendrites. GABAergic synapses therefore form before glutamatergic ones, presumably on the apical dendrites of the principal neurons (38). This sequence is of particular importance as GABA provides the main excitatory drive to hippocampal neurons at early stages of postnatal development because of a high Cl– content in immature neurons. Opening of the Cl– channels with efflux of Cl– leads to depolarization of young neurons, rather than the hyperpolarization observed in adults (Fig. 3). Consequently, in the immature brain, GABAA responses result in Cl– efflux, depolarization, and subsequent activation of voltage-dependent Na+ and Ca2+ channels (39). The depolarization produced by GABA is sufficient to remove the voltage-dependent Mg2+ block from NMDA channels, thereby inducing large Ca2+ influx into immature neurons. Initially discovered in the hippocampus, this effect of GABA has now been described in all brain structures studied (40). The effects of GABA include, however, an inhibitory component due to its shunting action. This explains why drugs such as phenobarbital or diazepam that work at the GABAA receptor do not cause seizures in the immature brain. More recent studies by Ben-Ari et al. suggest that in the embryonic monkey GABA is first excitatory, the shift occurring around embryonic d 100–120 (41). These findings suggest that the effects of epileptogenic agents will be strongly age, species, and structure dependent.
Example of three types of pyramidal neurons at P0. These three different types of CA1 neurons have different morphologic appearances: silent neurons have a cell body and an axon but no dendrites; GABA-only neurons have a cell body, axon, and small dendrites; and GABA and glutamate neurons have a cell body, axon, and extended apical and basal dendrites. The arrow points to the axons and the arrowhead points to the dendrites. Modified from (38) with permission.
Comparison of excitatory and inhibitory channels in neonate and adult. In the adult, AMPA responds to glutamate by opening and allowing Na+ to enter cell. With depolarization, Mg2+ is displaced from the channel and Na+ and Ca2+ enter the cell. With membrane depolarization, voltage-gated channels (VDNa+ and VDCa2+) also open. GABAA and GABAB, through Cl– and K+ ionic flow, serve to hyperpolarize the cell. In the neonate, AMPA receptors, although present, are not functional (designated as white). NMDA channels, because of the block with Mg2+, do not function at normal membrane resting potentials. Because of the higher Cl– content of the immature brain, GABA activation results in an efflux of Cl– that serves to depolarize the cell. With depolarization, the NMDA and voltage-gated channels can open. GABAB (designated white in the neonate's brain), like AMPA, develops later and provides little postsynaptic inhibition in the neonate. Modified from (40) with permission.
The other major postsynaptic inhibitory system, the postsynaptic GABAB, adenosine, and 5-hydroxytryptamine-G protein coupled K+ channels, also have a delayed maturation, suggesting that the neonatal circuit operates without transmitter-gated inhibition. In contrast, presynaptic inhibition, mediated by adenosine, GABAB, or other metabotropic receptors, is fully operational at birth; evidence that the major form of inhibition in the neonatal circuit is the control of transmitter release. If there is interference of these presynaptic controls of inhibition, pronounced seizures may occur. For example, it has recently been demonstrated that caffeine, an adenosine blocker, can be highly epileptogenic during hypoxia in the immature but not the adult rat (42).
In summary, the immature brain is more prone to seizures than the mature brain because of a developmental mismatch between the delicate balance of excitation and inhibition. The depolarizing effects of GABA during early development combined with a delay in postsynaptic inhibitory systems result in a situation in which seizures are easily elicited.
Deleterious effects of seizures to the developing brain. In spite of the relative resistance of immature neurons to epilepsy-induced brain damage, seizures in the developing brain do produce significant and often irreversible alterations of the developing brain. Kindling during the first weeks of life results in lifelong increases in seizure susceptibility (43). Using two models of neonatal seizures, pentylenetetrazol and flurothyl, we recently demonstrated that recurrent seizures during the neonatal period result in subsequent increases in mossy fiber growth in both the supragranular region and CA3 hippocampal subfield (44–46). Recurrent seizures also result in alterations of neuronal pathways activated during seizures (46); animals undergoing a series of seizures have a progressive increase in the extent of neuronal activation as evidenced by early gene activation of c-fos. In addition to the anatomical changes, neonatal seizures have also been shown to result in impairment of visual-spatial memory when the animals are tested as adults (44).
The aberrant network set up by recurrent seizures increase brain vulnerability to future injury. Schmid et al.(47) produced status epilepticus using either KA or perforant pathway stimulation in adolescent rats with a history of 25 seizures during the first 4 d of life. The authors found no cell loss in animals that had neonatal seizures only. Animals that had neonatal seizures, however, had significantly more severe brain injury following both KA and perforant pathway stimulation than did animals without a history of neonatal seizures. Although the mechanism behind this enhanced susceptibility to injury is not yet known, the study provides further evidence that neonatal seizures alter the brain in a maladaptive manner.
Seizures may perturb a wide range of developmental phenomena that are activity dependent, including cell division, migration, sequential expression of receptors, formation, and probably stabilization of synapses (48). Indeed seizures can modify—slow down or accelerate—a wide range of unique processes that take place during development and are essential for the correct formation and wiring of the circuitry. The migration of neurons, the arborization of the neurites, the formation of synapses, or the removal of redundant processes are all essential processes that are activity dependent and may be disturbed by seizures. Thus, recurrent activation of NMDA receptors accelerates neuronal migration (49) and may lead to the formation of aberrant connections. In addition, as noted above, most of the receptor proteins or second messenger cascades that have been studied are modified during development, and there are good reasons to believe that aberrant hyperactivity may alter the pattern and sequence of expression. Thus, the expression of AMPA receptors appears to be activity dependent with synchronized activity being required to facilitate its expression, much like plasticity in adult synapses (50). Aberrant episodes of hyperactivity will modify this sequence.
It is known that synaptic activity in the developing brain develops as a result of slow waves of depolarization that spread throughout the brain. Initially described in the hippocampus, GDP have now been observed in every neuronal structure studied (neocortex, retina, thalamus, spinal cord, etc.). GDP are generated by the combined excitatory actions of GABA and glutamate in developing circuits. Studies in intact hippocampi in vitro in rodents have shown that, in the rat, epileptogenic discharges can be generated within days of birth (51) and that GDP can be significantly altered by epileptogenic activity (52).
It now appears clear that prolonged or recurrent seizure activity, through activity-dependent mechanisms, can irreversibly alter the way the immature brain develops and forms synapses. These alterations in normal neuronal connectivity can result in long-term consequences in seizure susceptibility, learning and memory, and risk for subsequent seizure-induced injury.
CONCLUSIONS
The highest risk for seizures occurs during the first decade of life. This increased susceptibility to seizures is related to a developmental imbalance between excitatory and inhibitory processes. Although the immature brain is less vulnerable to seizure-induced injury than the mature brain, there are a number of developmental processes that appear to be permanently altered by the seizures.
Abbreviations
- AMPS:
-
α-amino-3-hydroxy-5-methylisoxazole-4-proprionic acid (AMPA)
- EPSP:
-
excitatory postsynaptic potentials
- GABA:
-
γ-aminobutyric acid, GDPs, giant depolarizing potentials
- KA:
-
kainic acid
- NMDA:
-
N-methyl-d-aspartate, PDS, paroxysmal depolarization shift
References
Jackson JH 1870 A study of convulsions. Transactions of the Saint Andrews Graduate Association 3: 162–204
Hauser WA 1995 Epidemiology of epilepsy in children. Neurosurg Clin North Am 6: 419–429
Snead OC 1995 Basic mechanisms of generalized absence seizures. Ann Neurol 37: 146–157
Nadler JV, Perry BW, Cotman CW 1978 Intraventricular kainic acid preferentially destroys hippocampal pyramidal cells. Nature 271: 676–677
Olney JW, Fuller T, De Gubareff T 1979 Acute dendrotoxic changes in the hippocampus of kainate treated rats. Brain Res 176: 91–100
Sloviter RS, Dean E, Sollas AI, Goodman JH 1996 Apoptosis and necrosis induced in different hippocampal neuron populations by repetitive perforant path stimulation in the rat. J Comp Neurol 366: 516–533
Ben-Ari Y, Tremblay E, Ottersen OP 1980 Injections of kainic acid into the amygdaloid complex of the rat: an electrographic, clinical and histological study in relation to the pathology of epilepsy. Neuroscience 5: 515–528
Ben-Ari Y 1985 Limbic seizure and brain damage produced by kainic acid: mechanisms and relevance to human temporal lobe epilepsy. Neuroscience 14: 375–403
Lipton SA, Rosenberg PA 1994 Excitatory amino acids as a final common pathway for neurologic disorders. N Engl J Med 330: 613–222
De Keyser J, Sulter G, Luiten PG 1999 Clinical trials with neuroprotective drugs in acute ischaemic stroke: are we doing the right thing?. Trends Neurosci 22: 535–540
Ben-Ari Y, Gho M 1988 Long-lasting modification of the synaptic properties of rat CA3 hippocampal neurones induced by kainic acid. J Physiol 404: 365–384
Represa A, Ben-Ari Y 1997 Molecular and cellular cascades in seizure-induced neosynapse formation. Adv Neurol 72: 25–34
Tauck D, Nadler JV 1985 Evidence of functional mossy fiber sprouting in the hippocampal formation of kainic acid-treated rats. J Neurosci 5: 1016–1022
Represa A, Tremblay E, Ben-Ari Y 1987 Kainate binding sites in the hippocampal mossy fibers: localization and plasticity. Neuroscience 20: 739–748
Sutula T, Koch J, Golarai G, Watanabe Y, McNamara JO 1996 NMDA receptor dependence of kindling and mossy fiber sprouting: evidence that the NMDA receptor regulates patterning of hippocampal circuits in the adult brain. J Neurosci 16: 7398–7406
McNamara RK, Routtenberg A 1995 NMDA receptor blockade prevents kainate induction of protein F1/GAP-43 mRNA in hippocampal granule cells and subsequent mossy fiber sprouting in the rat. Mol Brain Res 33: 22–28
Esclapez M, Hirsch J, Ben-Ari Y, Bernard C 1999 Newly formed excitatory pathways provide a substrate for hyperexcitability in experimental temporal lobe epilepsy. J Comp Neur 408: 449–60
Moshé SL 1981 The effects of age on the kindling phenomenon. Dev Psychobiol 14: 75–81
Holmes GL, Thompson JL 1987 Rapid kindling in the prepubescent rat. Brain Res 433: 281–284
Jensen FE, Applegate CD, Holzman D, Belin TR, Burchfiel JL 1991 Epileptogenic effect of hypoxia in the immature rodent brain. Ann Neurol 29: 629–637
Tremblay E, Nitecka L, Berger ML, Ben-Ari Y 1984 Maturation of kainic acid seizure-brain damage syndrome in the rat. I. Clinical, electrographic and metabolic observations. Neuroscience 13: 1051–1072
Cherubini E, Ben-Ari Y, Krnjevic K 1989 Anoxia produces smaller changes in synaptic transmission, membrane potential and input resistance in immature rat hippocampus. J Neurophysiol 62: 882–895
Albala BJ, Moshé SL, Okada R 1984 Kainic-acid-induced seizures: a developmental study. Dev Brain Res 13: 139–148
Berger ML, Tremblay E, Nitecka L, Ben-Ari Y 1984 Maturation of kainic acid seizure-brain damage syndrome in the rat. III. Postnatal development of kainic acid binding sites in the limbic system. Neuroscience 13: 1095–104
Nitecka L, Tremblay E, Charton G, Bouillot JP, Berger M, Ben-Ari Y 1984 Maturation of kainic acid seizure-brain damage syndrome in the rat. II. Histopathological sequelae. Neuroscience 13: 1073–1094
Holmes GL, Thompson JL, Marchi T, Feldman DS 1988 Behavioral effects of kainic acid administration on the immature brain. Epilepsia 29: 721–730
Stafstrom CE, Chronopoulos A, Thurber S, Thompson JL, Holmes GL 1993 Age-dependent cognitive and behavioral deficits following kainic acid-induced seizures. Epilepsia 34: 420–432
Hirsch E, Baram TZ, Snead OC 1992 Ontogenic study of lithium-pilocarpine-induced status epilepticus in rats. Brain Res 583: 120–126
Yang Y, Tandon P, Liu Z, Sarkisian MR, Stafstrom CE, Holmes GL 1998 Synaptic reorganization following kainic acid-induced seizures during development. Dev Brain Res 107: 169–177
Sperber EF, Haas KZ, Stanton PK, Moshé SL 1991 Resistance of the immature hippocampus to seizure-induced synaptic reorganization. Dev Brain Res 60: 88–93
Bickler PE, Gallego SM, Hansen BM 1993 Developmental changes in intracellular calcium regulation in rat cerebral cortex during hypoxia. J Cereb Blood Flow Metab 13: 811–819
Liu Z, Stafstrom CE, Sarkisian M, Tandon P, Yang Y, Hori A, Holmes GL 1996 Age-dependent effects of glutamate toxicity in the hippocampus. Dev Brain Res 97: 178–184
Marks JD, Friedman JE, Haddad GG 1996 Vulnerability of CA1 neurons to glutamate is developmentally regulated. Dev Brain Res 97: 194–206
Liu Z, Gatt A, Mikati M, Holmes GL 1995 Long-term behavioral deficits following pilocarpine seizures in immature rats. Epilepsy Res 19: 191–204
Sankar R, Shin DH, Liu H, Mazarati A, Pereira de Vasconcelos A, Wasterlain CG 1998 Patterns of status epilepticus-induced neuronal injury during development and long-term consequences. J Neurosci 18: 8382–8393
Cronin J, Dudek FE 1988 Chronic seizures and collateral sprouting of dentate mossy fibers after kainic acid treatment in rats. Brain Res 474: 181–184
Stafstrom CE, Thompson JL, Holmes GL 1992 Kainic acid seizures in the developing brain: status epilepticus and spontaneous recurrent seizures. Dev Brain Res 65: 227–236
Tyzio R, Represa A, Jorquera I, Ben-Ari Y, Gozlan H, Aniksztejn L 1999 The establishment of GABAergic and glutamatergic synapses on CA1 pyramidal neurons is sequential and correlates with the development of the apical dendrite. J Neurosci 10372–82
Leinekugel X, Medina I, Khalilov R, Ben-Ari Y, Khazipov R 1997 Leinekugel X, Medina I, Khalilov R, Ben-Ari Y, Khazipov R 1997 Ca++ oscillations mediated by the synergistic excitatory actions of GABAA and NMDA receptors in the neonatal hippocampus. Neuron 18: 243–255
Ben-Ari Y, Khazipov R, Leinekugel X, Caillard O, Gaiarsa J-L 1997 GABAA, NMDA and AMPA receptors: a developmentally regulated “ménage à trois.”. TINS 20: 523–529
Khazipov R, Esclapez M, Caillard O, Bernard C, Hirsch E, Leinekugel X, Berger B, Ben-Ari Y 1999 Early maturation of hippocampal network in the fetal cynomolgus monkey. Soc Neurosci 25: 2266( abstr)
Dzhala V, Desfreres L, Melyan Z, Ben-Ari Y, Khazipov R 1999 Epileptogenic action of caffeine during anoxia in the neonatal rat hippocampus. Ann Neurol 46: 95–102
Moshé SL, Albala BJ 1982 Kindling in developing rats: persistence of seizures into adulthood. Dev Brain Res 4: 67–71
Holmes GL, Gaiarsa J-L, Chevassus-Au-Louis N, Ben-Ari Y 1998 Consequences of neonatal seizures in the rat: morphological and behavioral effects. Ann Neurol 44: 845–857
Holmes GL, Sarkisian M, Ben-Ari Y, Chevassus-Au-Louis N 1999 Mossy fiber sprouting following recurrent seizures during early development in rats. J Comp Neurol 404: 537–553
Liu Z, Yang Y, Silveira DC, Sarkisian MR, Tandon P, Huang L-T, Stafstrom CE, Holmes GL 1999 Consequences of recurrent seizures during early brain development. Neuroscience 92: 1443–1454
Schmid R, Tandon P, Stafstrom CE, Holmes GL 1999 Effects of neonatal seizures on subsequent seizure-induced brain injury. Neurology 53: 1754–1761
Holmes GL, Ben-Ari Y 1998 Seizures in the developing brain: perhaps not so benign after all. Neuron 21: 1–20
Komuro H, Rakic P 1993 Modulation of neuronal migration by NMDA receptors. Science 260: 95–97
Durand GM, Kovalchuk Y, Konnerth A 1996 Long-term potentiation and functional synapse induction in developing hippocampus. Nature 381: 71–75
Khalilov I, Dzhala V, Medina I, Leinekugel X, Melyan Z, Lamsa K, Khazipov R, Ben-Ari Y 1999 Maturation of kainate-induced epileptiform activities in interconnected intact neonatal limbic structures in vitro. Eur J Neurosci 11: 3468–3480
Leinekugel X, Khalilov I, Ben-Ari Y, Khazipov R 1998 Giant depolarizing potentials: the septal pole of the hippocampus paces the activity of the developing intact septohippocampal complex in vitro. J Neurosci 18: 6349–6357
Author information
Authors and Affiliations
Additional information
Supported by the Emily P. Rogers Research Fund and grants from the NINDS (NS27984) and the French Medical Research Council.
Rights and permissions
About this article
Cite this article
Holmes, G., Ben-Ari, Y. The Neurobiology and Consequences of Epilepsy in the Developing Brain. Pediatr Res 49, 320–325 (2001). https://doi.org/10.1203/00006450-200103000-00004
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200103000-00004
This article is cited by
-
Effect of Taurine on the Manifestations of Audiogenic Epilepsy in Rats with Pendulum Movements
Neuroscience and Behavioral Physiology (2023)
-
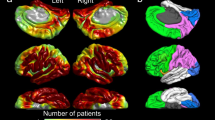
Children with epilepsy demonstrate macro- and microstructural changes in the thalamus, putamen, and amygdala
Neuroradiology (2020)
-
Down syndrome cell adhesion molecule like-1 (DSCAML1) links the GABA system and seizure susceptibility
Acta Neuropathologica Communications (2020)
-
Mechanistic insights into autocrine and paracrine roles of endothelial GABA signaling in the embryonic forebrain
Scientific Reports (2019)
-
Neuroprotective Effects of AG490 in Neonatal Hypoxic-Ischemic Brain Injury
Molecular Neurobiology (2019)