Abstract
The evolutionarily conserved Hedgehog (Hh) signaling pathway is essential for correct embryogenesis and is misregulated in several malignancies. In cell culture, Hh-sensitive cells display a striking dependence on cell density with active Hh signaling requiring cell-to-cell contact. As the Hippo/YAP system is tightly linked to cell density control and contact inhibition, we investigated the cross-talk between the two pathways. Our data reveal that the suppression of Hh signaling in the absence of cellular contacts is independent of primary cilia and is mediated by the YAP oncogene. Overexpression of YAP blocks Hh signaling whereas RNA interference-mediated knockdown of YAP enhances Hh/GLI activity. Despite this negative regulation, Hh signaling promotes YAP activity through post-transcriptional mechanisms, resulting in a negative feedback loop. In vivo, we found strong nuclear YAP immunoreactivity restricted to compartments with low Hh pathway activity in human and mouse pancreatic cancer. Finally, we identified protease-activated receptors (PARs) as molecules being able to override the inverse Hippo/Hh regulation, potentially giving tumors a mechanism to utilize both oncogenic pathways in parallel.
Similar content being viewed by others
Introduction
The control of cellular density is of utmost importance for proper embryonic development and for the determination of organ size. In the past years, a serine/threonine kinase cascade (the Hippo pathway) has been identified as a major regulator of cell density control in vivo and in vitro.1, 2, 3, 4 The Hippo pathway eventually controls the transcriptional co-activator YAP (Yes-associated protein) and its paralog TAZ. Under conditions of low cell density, the Hippo pathway is inactive and YAP/TAZ enter the nucleus to induce target gene transcription.5 In contrast, under conditions of high cellular density, the Hippo cascade is turned on, resulting in the phosphorylation of YAP/TAZ by LATS (large tumor suppressor) kinases and their subsequent inactivation by cytoplasmic retention. In order to achieve their biological effects, nuclear YAP/TAZ partner with several transcription factors, of which members of the TEAD family are best studied.6 These phenomena are recapitulated in an in vitro process termed contact inhibition, indicating the growth arrest that normal cells undergo when they have reached full confluency in a culture plate. This process is also dependent on and regulated by Hippo/YAP activity. In line with Hippo/YAP activity controlling cellular (over-) growth, several cancers have been linked to elevated nuclear YAP presence.1,3,7
Another developmentally important pathway that is deregulated in cancer is the Hedgehog (Hh) signaling cascade.8,9 By binding to their PTCH1/2 receptors, Hh ligands derepress the transmembrane protein Smoothened (SMO) that initiates additional steps to activate the GLI (glioma-associated oncogene) family of transcription factors. At least in culture, Hh signaling is dependent on cell-to-cell contacts and high Hh pathway activity can only be achieved under confluent conditions.10 Moreover, as an oncogenic signaling entity, Hh signaling is able to override the contact inhibition of normal fibroblasts.11,12 Given these density-controlled processes, we investigated the molecular cross-talk between the Hippo/YAP and the Hh/GLI systems. We could find that YAP binds to and negatively controls the activity of GLI transcription factors, leading to a repression of Hh pathway target genes. In contrast, Hh pathway activity promotes YAP post-transcriptionally by increasing its protein levels, suggestive of a negative feedback loop. In line with a negative Hippo-to-Hh regulation, we found active (nuclear) YAP in tumor compartments displaying low Hh pathway activity in pancreatic cancer specimens, but only very little nuclear YAP in compartments with high Hh activity.
Assuming that additional potential molecular cues exist that allow for the simultaneous activation of both oncogenic pathways, we identified the protease-activated receptor (PAR) system as a means to overcome the negative Hippo/Hh cross-talk. Thus, the PAR system might represent a promising novel drug target in Hippo/Hh double-positive tumors.
Results and discussion
The Hh pathway is controlled in a density-dependent manner
Previous reports established that Hh signaling in cultured cells is most functional under high cellular densities.10 We repeated this experiment using Ptch1−/− mouse embryonic fibroblasts (MEFs) that show constitutive high Hh signaling because of the loss of the negative regulator Ptch1. The Ptch1 gene knockout in these cells was achieved by insertion of a lacZ reporter sequence into the endogenous Ptch1 locus. This placed the lacZ expression cassette under the control of the endogenous Ptch1 regulatory elements and Hh pathway activity can thus be measured by detecting lacZ enzyme activity.10 To our surprise, plating Ptch1−/− MEFs in different cell densities and staining for β-galactosidase activity (blue color in Figure 1a) revealed that only cells that encountered the highest cell densities, such as those in the center of cell foci, displayed clear Hh pathway activation (Figure 1a). The density-dependent regulation of Hh signaling in Ptch1−/− MEFs was also verified on the expression level (Figure 1b): Hh target genes (Gli1, Angpt4, and Hsd11b1) were upregulated in cultures with high cell density compared with low density cultures. In contrast, the density-regulated Hippo/YAP transcriptional targets Ctgf, Cyr61 or Inhba were downregulated upon higher confluency, suggesting an inverse relationship between Hh and Hippo target gene expression. Next, we verified our results on density control of the Hh pathway in ShhL2 cells, a clonal NIH3T3 cell line stably expressing a luciferase Hh/GLI reporter construct.13 As expected, the Hh pathway induction by addition of the SMO agonist SAG13 was strongly density dependent (Figure 1c). Importantly, primary cilium frequencies remained similar across the different culture densities, demonstrating that the observed density-dependent pathway control was not mediated by altered cilium formation. As before, the density control could be verified on the target gene expression level for the Hh (Gli1, Ptch1, Rasl11b, and Angpt4) as well as the Hippo (Ctgf, Cyr61 and Inhba) system (Figure 1d). Again, Hh target genes were upregulated by high cell densities, whereas YAP target genes were suppressed under these conditions. A similar inverse mode of density-dependent regulation could also be found in other cell lines, for instance, in human pancreatic adenocarcinoma cells: the Hh target genes (GLI1 and E-CADHERIN (ECAD)14 were induced by high cell density, whereas the YAP target genes (CTGF, AREG, and AMOTL2) were downregulated (Figure 1e). Taken together, these experiments showed that high Hh pathway activity is strongly density regulated, is not mediated by altered primary cilium frequency and is paralleled by an inverse modulation of YAP activity.
The expression of Hh target genes is density dependent and is inversely correlated with Hippo target genes. (a) X-gal staining for β-galactosidase activity (blue) of Ptch1−/− MEFs plated in different cellular densities. Blue color indicates active Hh signaling. (b) Hh and Hippo target gene expression in Ptch1−/− MEFs (plated in low (subconfluent) and high (confluent) densities with 1% fetal bovine serum (FBS)) as measured by quantitative PCR (Qpcr). The inset depicts the GLI1 protein levels in relationship to Ptch1−/− culture confluency. (c) Cell density-dependent Hh reporter activity in ShhL2 cells. The cells were plated in different densities (1% FBS) and induced with the SMO agonist SAG (100 nM for 48 h). Also shown is the (cell density independent) frequency of primary cilia in these cells, as measured by acetylated tubulin staining (Sigma-Aldrich, Taufkirchen, Germany, T6793) (1% FBS). (d) Hh and Hippo target gene expression in ShhL2 cells plated in different cell densities. (e) Hh and Hippo target gene expression in human Panc1 cells plated in different cell densities (1% FBS). *P<0.05; **P<0.005; ***P<0.0005 (two-tailed Student's t-test).
Increased YAP levels suppress Hh/GLI activity
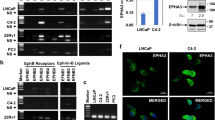
In order to elucidate whether YAP is causally involved in regulation of the Hh pathway, we generated Hek293T cells stably expressing a dominant active version of YAP (YAP2(5SA), a mutant form of the YAP2 splice variant with increased protein stability and nuclear presence3). In agreement with a suppressive functional role of YAP on the Hh pathway, cells expressing YAP2(5SA) displayed a significant reduction in Hh pathway target gene expression (GLI1, PTCH1, and HIP1), demonstrating that YAP expression is sufficient for this effect and that no other upstream Hippo pathway elements are required (Figure 2a). Next, we wondered whether the YAP presence directly impinged on the transcriptional activity of GLI transcription factors. To this end, we performed a Hh reporter assay in human fibroblasts (pancreatic stellate cells15) expressing GLI1 (or its naturally occurring splice variant GLI1ΔN16). As shown in Figure 2b, the expression of the dominant active YAP mutant strongly reduced GLI1 activity, whereas the expression of wild-type YAP had no effect, implying that it was nuclear YAP that repressed GLI1 activity. YAP2(5SA) could also potently inhibit GLI1ΔN that lacks one of the two binding sites for Suppressor of Fused (SUFU, a major negative regulator of the pathway17), strongly suggesting that the mechanism of inhibition does not involve SUFU. The antagonistic behavior of YAP2(5SA) on GLI1 activity could additionally be verified in other cell lines (Supplementary Figure S1). Furthermore, the repression of the Hh pathway in pancreatic stellate cells was also documented on the mRNA level upon transient transfection with dominant active YAP (Figure 2c). Finally, expression of nuclear YAP inhibited endogenous Hh signaling in SAG-stimulated NIH3T3 cells as measured by a luminometric Hh reporter assay (Figure 2d).
YAP overexpression suppresses Hh signaling. (a) Hh and Hippo target gene expression in Hek293T cells stably overexpressing a dominant active mutant of YAP (YAP2_5SA). The inset shows an immunoblot of these cells verifying YAP overexpression (bands were cropped from the same blot). (b) Hh reporter activity in transiently transfected human pancreatic stellate cells (PSCs). Cells were transfected with full-length GLI1 (GLI1_fl) or N-terminally truncated GLI1 (GLI1_dN) plus the indicated constructs (plasmid ratio GLI1/YAP was 1:3). (c) GLI1 and PTCH1 mRNA expression in transiently transfected PSCs as measured by quantitative PCR (qPCR). (d) Hh reporter assay measuring endogenous Hh pathway activity in NIH3T3 cells. The cells were either transfected with empty vector control (pcDNA3.1) or dominant active YAP (YAP2_5SA) and were subsequently stimulated with SAG. (e) Co-immunoprecipitation of Flag-tagged GLI1 and EGFP-tagged Yes-associated protein 1 (YAP1) in Hek293T cells. Immunoprecipitation (IP): α-Flag; western blot (WB): α-GFP. (f) Co-immunoprecipitation of endogenous YAP and endogenous GLI1 in Hek293T cells. IP: α-YAP; WB: α-GLI1. *P<0.05; **P<0.005; ***P<0.0005 (two-tailed Student's t-test).
Mechanistically, we found that both exogenous and endogenous GLI1 and YAP proteins could be co-immunoprecipitated from cellular lysates (Figures 2e and f), suggesting a direct interaction. This result was also verified in a second cell line (Supplementary Figure S2A). Moreover, YAP overexpression did not sequester GLI1 away from the nucleus (Supplementary Figure S2B), implying a nuclear YAP/GLI interaction that is responsible for the negative Hh pathway modulation.
Knockdown of endogenous YAP increases Hh pathway activity
Next, we went on to investigate whether endogenous YAP levels could regulate endogenous Hh pathway activity. To this end, we knocked down Yap mRNA by means of a pool of RNA interference sequences in MEF cells stably expressing the Sonic Hedgehog (SHH) ligand (MEF[SHH] cells18). As can be seen in Figure 3a, knockdown of Yap increased the protein expression of GLI1, indicative of Hh pathway derepression. A similar finding was made in Hek293T cells stably expressing a short hairpin RNA construct targeting YAP (Figure 3b). In addition, human pancreatic stellate cells transfected with small interfering RNA against YAP upregulated GLI1 mRNA. Interestingly, knocking down the YAP paralog TAZ also resulted in Hh pathway derepression, suggesting that YAP and TAZ have overlapping functions with respect to Hh. These findings were verified by separating the small interfering RNA pool into its individual small interfering RNA constructs (Supplementary Figure S3A).
RNA interference (RNAi)-mediated knockdown of endogenous YAP promotes Hh signaling. (a) Western blot depicting the protein levels of endogenous GLI1 and YAP in MEF[SHH] cells after transfection with control small interfering RNA (siRNA) or a pool of four different Yap-specific siRNA constructs (Dharmacon ‘SMARTpool’; Dharmacon GE Healthcare, Lafayette, CO, USA). (b) Western blot depicting the protein levels of endogenous GLI1 and YAP in Hek293T cells stably expressing control- or YAP-directed short hairpin RNA (shRNA) (293T[shCon] and 293T[shYAP], respectively). (c) Hh and Hippo target gene expression in pancreatic stellate cells (PSCs) transfected with control siRNA or siRNA against YAP/TAZ. (d) Effects of siYAP/siTAZ transfection on the GLI1 and CTGF mRNA expression level in Panc1 cells. The knockdown efficiency is also depicted. (e) Protein levels of YAP and GLI1 in NIH3T3 cells treated with SAG. (f) Hh pathway activation by means of SAG addition increases the expression of Hippo target genes (Ctgf and Inhba) without altering the expression levels of Yap or Taz (NIH3T3 cells). (g) Immunoblotting of endogenous YAP protein in NIH3T3 cells exposed to SAG (100 nM) and treated for different time periods with cycloheximide (CHX; 100 μg/ml). *P<0.05; **P<0.005; ***P<0.0005 (two-tailed Student's t-test).
Most importantly, pronounced suppression of Hippo target genes (CTGF and ANKRD1) was only achieved after dual YAP/TAZ knockdown (Figure 3c). In contrast, GLI1 upregulation was already seen upon single knockdown of either YAP or TAZ, implying that it was YAP or TAZ itself—and not their target genes—that was responsible for Hh pathway control (Figure 3c). A similar derepression of GLI1 expression was also observed in Panc1 cells after combined knockdown of YAP/TAZ (Figure 3d).
Having analyzed the effects of Hippo signaling on the Hh pathway, we wanted to analyze the effect of Hh signaling on the Hippo pathway. Immunoblot experiments revealed that YAP protein levels were significantly induced in NIH3T3 cells treated with the SMO agonist SAG (Figure 3e). In addition, YAP target genes (Ctgf and Inhba) were upregulated by SAG exposure (Figure 3f). Intriguingly, the increase in YAP levels was not mediated by a transcriptional upregulation of Yap (or Taz) mRNA levels (Figure 3f), suggesting post-transcriptional mechanisms. Identical findings were made using NIH3T3[SHH] cells in which the active Hh pathway was blocked by addition of the SMO antagonist SANT1(ref. 13) ( (Supplementary Figures S3B and C). Following up on these results, we observed that Hh pathway activation by SAG extended the half-life of endogenous YAP protein from ∼2.5 h to ∼4.5 h (Figure 3g). In general, these findings are in agreement with reports on Hh signaling being able to overcome contact inhibition in culture.11,12
Taken together, we postulate that endogenous YAP (and TAZ), which is under the control of cellular density, regulates the Hh pathway at the level of GLI transcription factors.
PARs can activate YAP and GLI
In light of the inverse correlation between YAP and Hh/GLI activity, we wanted to investigate the distribution of YAP in tumors with active Hh signaling. We focused on ductal pancreatic adenocarcinoma (PDAC), a tumor entity for which the Hh/GLI activity pattern has been well described. Specifically, epithelial PDAC tumor cells secrete Hh ligands, but do not respond to the ligand and thus display a comparatively low Hh pathway activity. In contrast, the desmoplastic stromal fibroblasts surrounding the tumor cells are actively responding to the Hh ligands and therefore express high GLI1 levels.19, 20, 21 In agreement with our in vitro data, the pattern of YAP immunoreactivity was inversely arranged to the Hh pathway activity: whereas there was a strong nuclear signal (indicating YAP activity) in the epithelial PDAC tumor compartment, there was only a weak staining of some cells in the tumor stroma. These findings were made in tissue sections from a PDAC mouse model22 (Figure 4a) as well as in human PDAC samples (Figure 4b).
Activation of PAR overcomes the inverse Hippo/Hh cross-talk. (a) Anti-YAP immunohistochemistry (Cell Signaling Technologies, Danvers, MA, USA; no. 4912, 1:100) on tissue sections from mouse pancreatic tumors (‘KPC’ mouse model). S, tumor stroma; T, tumor epithelium. (b) Anti-YAP immunohistochemistry on tissue sections from human patients suffering from pancreatic cancer. (c) Hh (GLI1 and PTCH1) and Hippo (CTGF and AREG) target gene expression in Hek293A cells exposed to PAR-2 ligand (SLIGRL-NH2, Sigma-Aldrich S9317, 5 μM) for the indicated time periods. (d) Cell number change in Hek293A cells transfected with the indicated short hairpin RNA (shRNA) constructs followed by PAR-2 ligand exposure (5 μM for 5 days, 1% fetal bovine serum (FBS)). (e) Schematic diagram depicting the major findings of this work. *P<0.05; **P<0.005 (two-tailed Student's t-test).
Because YAP/TAZ activity had been described in several malignancies in which Hh pathway activation had also been reported,7,23, 24, 25, 26, 27 we searched for potential mechanisms that could bypass the inverse regulation between YAP and GLI and lead to a simultaneous activation of both oncogenes. Here, we focused on PARs that were shown to activate YAP/TAZ through the heterotrimeric G12/13 proteins.28 In addition, the α subunit of G13 has been shown to promote GLI activation in a SMO-independent manner.29 In agreement with these reports, we could induce Hh (GLI1 and PTCH1) as well as Hippo/YAP (CTGF and AREG) target genes in Hek293A cells by exposure to a synthetic peptide PAR-2 agonist (Figure 4c). Similar results were obtained with Panc1 cells (Supplementary Figure S4A). As both YAP and GLI1 have been associated with enhanced proliferation and survival, we found that PAR-2 activation results roughly in a twofold increase in cell number within 72 h (Supplementary Figure S4C). Based on these results, we asked whether the experimental removal of YAP and GLI1 would abrogate the proliferation-promoting effects of PAR activation. To this end, we transfected Hek293A cells with short hairpin RNA constructs targeting YAP1, GLI1 (for knockdown efficiency, see Supplementary Figures S4D and E) or the combination of both and treated the cells with PAR-2 ligand. As can be seen in Figure 4d, PAR-2 activation doubled the cell number in cells receiving control short hairpin RNA. In cells transfected with shYAP or shGLI1, only a 1.5-fold increase in cell number by PAR-2 ligand treatment was achieved. When knocking down YAP and GLI1 in parallel, the PAR-2 activation was nonfunctional and there was no increase in cell number, indicating that PAR activation promotes simultaneous upregulation of YAP and GLI1 that results in enhanced cellular proliferation.
In summary, we describe an antagonistic impact of Hippo/YAP on Hh/GLI, and a positive effect of Hh on YAP. Regarding the negative regulation, YAP can directly interact with GLI1 and can hypothetically interfere with the correct built-up of transcriptional complexes around GLI1. It is intriguing that Hippo/YAP has been shown to inhibit mammalian WNT signaling, a pathway with close evolutionary ties to Hh.30,31
Concerning a positive modulation of YAP by Hh signaling, we found post-transcriptional mechanisms at play that increase the amounts of YAP protein. Although further studies are needed to decipher the exact molecular steps, our data suggest that this process represents a major event in the Hh-driven loss of cellular contact inhibition.
Of note, several reports link YAP/TAZ activity to the formation of a stem cell phenotype1,5,32 and in mechanosensation. As stem cells are routinely cultured in nonadherent spheres, it will be interesting to learn whether the dense culture conditions within the sphere center differentially affect YAP and GLI functions. Similarly, questions on mechanical stress and Hh/GLI activity will await further investigations.
Eventually, evidence gathered from medulloblastoma23 argues that the activation of both YAP and GLI oncogenes is feasible. Based on these findings, we anticipated mechanisms that could simultaneously promote both factors and identified the PAR system as a dual driver of YAP/GLI activity. Eliminating YAP plus GLI almost completely abrogated the PAR-2 ligand-induced stimulation in cell proliferation, arguing that these two proteins exert much of the biological growth-promoting impact of PAR.
Abbreviations
YAP, Yes-associated protein; Hh, Hedgehog; SHH, Sonic Hedgehog; GLI1, glioma-associated oncogene 1; PDAC, pancreatic ductal adenocarcinoma.
References
Camargo FD, Gokhale S, Johnnidis JB, Fu D, Bell GW, Jaenisch R et al. YAP1 increases organ size and expands undifferentiated progenitor cells. Curr Biol 2007; 17: 2054–2060.
Zhao B, Tumaneng K, Guan KL . The Hippo pathway in organ size control, tissue regeneration and stem cell self-renewal. Nat Cell Biol 2011; 13: 877–883.
Zhao B, Wei X, Li W, Udan RS, Yang Q, Kim J et al. Inactivation of YAP oncoprotein by the Hippo pathway is involved in cell contact inhibition and tissue growth control. Genes Dev 2007; 21: 2747–2761.
Yu FX, Guan KL . The Hippo pathway: regulators and regulations. Genes Dev 2013; 27: 355–371.
Barry ER, Camargo FD . The Hippo superhighway: signaling crossroads converging on the Hippo/Yap pathway in stem cells and development. Curr Opin Cell Biol 2013; 25: 247–253.
Liu-Chittenden Y, Huang B, Shim JS, Chen Q, Lee SJ, Anders RA et al. Genetic and pharmacological disruption of the TEAD-YAP complex suppresses the oncogenic activity of YAP. Genes Dev 2012; 26: 1300–1305.
Zender L, Spector MS, Xue W, Flemming P, Cordon-Cardo C, Silke J et al. Identification and validation of oncogenes in liver cancer using an integrative oncogenomic approach. Cell 2006; 125: 1253–1267.
Robbins DJ, Fei DL, Riobo NA . The hedgehog signal transduction network. Sci Signal 2012; 5: re6.
Briscoe J, Therond PP . The mechanisms of Hedgehog signalling and its roles in development and disease. Nat Rev Mol Cell Biol 2013; 14: 416–429.
Taipale J, Chen JK, Cooper MK, Wang B, Mann RK, Milenkovic L et al. Effects of oncogenic mutations in smoothened and patched can be reversed by cyclopamine. Nature 2000; 406: 1005–1009.
Lauth M, Bergstrom A, Shimokawa T, Toftgard R . Inhibition of GLI-mediated transcription and tumor cell growth by small-molecule antagonists. Proc Natl Acad Sci USA 2007; 104: 8455–8460.
Kimura H, Stephen D, Joyner A, Curran T . Gli1 is important for medulloblastoma formation in Ptc1+/− mice. Oncogene 2005; 24: 4026–4036.
Chen JK, Taipale J, Young KE, Maiti T, Beachy PA . Small molecule modulation of Smoothened activity. Proc Natl Acad Sci USA 2002; 99: 14071–14076.
Joost S, Almada LL, Rohnalter V, Holz PS, Vrabel AM, Fernandez-Barrena MG et al. GLI1 inhibition promotes epithelial-to-mesenchymal transition in pancreatic cancer cells. Cancer Res 2012; 72: 88–99.
Jesnowski R, Furst D, Ringel J, Chen Y, Schrodel A, Kleeff J et al. Immortalization of pancreatic stellate cells as an in vitro model of pancreatic fibrosis: deactivation is induced by matrigel and N-acetylcysteine. Lab Invest 2005; 85: 1276–1291.
Shimokawa T, Tostar U, Lauth M, Palaniswamy R, Kasper M, Toftgard R et al. Novel human glioma-associated oncogene 1 (GLI1) splice variants reveal distinct mechanisms in the terminal transduction of the hedgehog signal. J Biol Chem 2008; 283: 14345–14354.
Svard J, Heby-Henricson K, Persson-Lek M, Rozell B, Lauth M, Bergstrom A et al. Genetic elimination of Suppressor of fused reveals an essential repressor function in the mammalian Hedgehog signaling pathway. Dev Cell 2006; 10: 187–197.
Lipinski RJ, Bijlsma MF, Gipp JJ, Podhaizer DJ, Bushman W . Establishment and characterization of immortalized Gli-null mouse embryonic fibroblast cell lines. BMC Cell Biol 2008; 9: 49.
Tian H, Callahan CA, DuPree KJ, Darbonne WC, Ahn CP, Scales SJ et al. Hedgehog signaling is restricted to the stromal compartment during pancreatic carcinogenesis. Proc Natl Acad Sci USA 2009; 106: 4254–4259.
Lauth M, Bergstrom A, Shimokawa T, Tostar U, Jin Q, Fendrich V et al. DYRK1B-dependent autocrine-to-paracrine shift of Hedgehog signaling by mutant RAS. Nat Struct Mol Biol 2010; 17: 718–725.
Nolan-Stevaux O, Lau J, Truitt ML, Chu GC, Hebrok M, Fernandez-Zapico ME et al. GLI1 is regulated through Smoothened-independent mechanisms in neoplastic pancreatic ducts and mediates PDAC cell survival and transformation. Genes Dev 2009; 23: 24–36.
Hingorani SR, Wang L, Multani AS, Combs C, Deramaudt TB, Hruban RH et al. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell 2005; 7: 469–483.
Fernandez LA, Northcott PA, Dalton J, Fraga C, Ellison D, Angers S et al. YAP1 is amplified and up-regulated in hedgehog-associated medulloblastomas and mediates Sonic hedgehog-driven neural precursor proliferation. Genes Dev 2009; 23: 2729–2741.
Bhat KP, Salazar KL, Balasubramaniyan V, Wani K, Heathcock L, Hollingsworth F et al. The transcriptional coactivator TAZ regulates mesenchymal differentiation in malignant glioma. Genes Dev 2011; 25: 2594–2609.
Overholtzer M, Zhang J, Smolen GA, Muir B, Li W, Sgroi DC et al. Transforming properties of YAP, a candidate oncogene on the chromosome 11q22 amplicon. Proc Natl Acad Sci USA 2006; 103: 12405–12410.
Zhang X, George J, Deb S, Degoutin JL, Takano EA, Fox SB et al. The Hippo pathway transcriptional co-activator, YAP, is an ovarian cancer oncogene. Oncogene 2011; 30: 2810–2822.
Lamar JM, Stern P, Liu H, Schindler JW, Jiang ZG, Hynes RO . The Hippo pathway target, YAP, promotes metastasis through its TEAD-interaction domain. Proc Natl Acad Sci USA 2012; 109: E2441–E2450.
Mo JS, Yu FX, Gong R, Brown JH, Guan KL . Regulation of the Hippo-YAP pathway by protease-activated receptors (PARs). Genes Dev 2012; 26: 2138–2143.
Douglas AE, Heim JA, Shen F, Almada LL, Riobo NA, Fernandez-Zapico ME et al. The alpha subunit of the G protein G13 regulates activity of one or more Gli transcription factors independently of smoothened. J Biol Chem 2011; 286: 30714–30722.
Jacob LS, Wu X, Dodge ME, Fan CW, Kulak O, Chen B et al. Genome-wide RNAi screen reveals disease-associated genes that are common to Hedgehog and Wnt signaling. Sci Signal 2011; 4: ra4.
Nusse R . Wnts and Hedgehogs: lipid-modified proteins and similarities in signaling mechanisms at the cell surface. Development 2003; 130: 5297–5305.
Cordenonsi M, Zanconato F, Azzolin L, Forcato M, Rosato A, Frasson C et al. The Hippo transducer TAZ confers cancer stem cell-related traits on breast cancer cells. Cell 2011; 147: 759–772.
Acknowledgements
This work was supported by grants obtained from the German Cancer Aid (No. 109481 to ML and No. 109215/109929 to GF), the University Medical Center Giessen and Marburg (UKGM to ML), the German Research Foundation (DFG LA 2829/1-1 to ML) and the European Community’s Seventh Framework Program (FP7-2007-2013) under grant agreement HEALTH-F2-2011-256986 (to GF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Oncogenesis website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Tariki, M., Dhanyamraju, P., Fendrich, V. et al. The Yes-associated protein controls the cell density regulation of Hedgehog signaling. Oncogenesis 3, e112 (2014). https://doi.org/10.1038/oncsis.2014.27
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/oncsis.2014.27
This article is cited by
-
Role of Hippo pathway dysregulation from gastrointestinal premalignant lesions to cancer
Journal of Translational Medicine (2024)
-
Proliferation-driven mechanical compression induces signalling centre formation during mammalian organ development
Nature Cell Biology (2024)
-
Hippo signaling activates hedgehog signaling by Taz-driven Gli3 processing
Cell Regeneration (2023)
-
Hippo pathway dysregulation in gastric cancer: from Helicobacter pylori infection to tumor promotion and progression
Cell Death & Disease (2023)
-
Cell population balance of cardiovascular spheroids derived from human induced pluripotent stem cells
Scientific Reports (2019)