Abstract
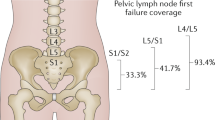
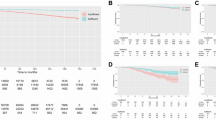
Pelvic lymph node dissection is the only reliable method of staging for clinically localized prostate cancer. Despite the obvious prognostic advantages conferred by accurate staging, pelvic lymph node dissection is associated with significant morbidity and prolonged operative time. A substantial decrease in the sensitivity to lymph node metastasis occurs by simple reduction of the dissection area to the obturator fossa. Radioguided sentinel lymph node dissection provides accurate staging despite use of a minimal-area dissection template. Results from studies in prostate cancer indicate that this method has a high sensitivity for very early detection of lymphatic spread. A substantial number of the detected metastases are of a small size, solitary and widely distributed throughout the pelvic lymph nodes. These features make metastases undetectable by preoperative imaging modalities, and by the current, standard method of lymph node dissection limited to the obturator fossa.
Key Points
-
Radioguided sentinel lymph node (SLN) dissection is a reliable method of staging for clinically localized prostate cancer
-
Clinical application of SLN staging in prostate cancer is associated with reduced surgical complexity and a reduced complication rate compared with extended lymph node dissection, while retaining maximal sensitivity for detection of lymphatic metastases
-
SLN staging is not affected by the size of a metastatic lesion and, therefore, detects even micrometastases effectively
-
Awareness of prostate lymph drainage anatomy, and technical considerations related to radiopharmaceutical properties and detection technique, are of pivotal importance for the successful clinical application of prostate cancer SLN staging
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Cerny JC et al. (1975) An evaluation of lymphangiography in staging carcinoma of the prostate. J Urol 3: 367–370
Golimbu M et al. (1979) Extended pelvic lymphadenectomy for prostatic cancer. J Urol 5: 617–620
Raghavaiah NV and Jordan WR (1979) Prostatic lymphography. J Urol 2: 178–181
Allaf ME et al. (2004) Anatomical extent of lymph node dissection: impact on men with clinically localized prostate cancer. J Urol 5: 1840–1844
Bader P et al. (2003) Disease progression and survival of patients with positive lymph nodes after radical prostatectomy. Is there a chance of cure? J Urol 3: 849–854
Clark T et al. (2003) Randomized prospective evaluation of extended versus limited lymph node dissection in patients with clinically localized prostate cancer. J Urol 1: 145–147
Cabanas RM (1977) An approach for the treatment of penile carcinoma. Cancer 39: 456–466
Pettaway CA et al. (1995) Sentinel lymph node dissection for penile carcinoma: the MD Anderson Cancer Center experience. J Urol 6: 1999–2003
Morton DL et al. (1992) Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 4: 392–399
Alex JC and Krag DN (1993) Gamma-probe guided localization of lymph nodes. Surg Oncol 2: 137–143
Veronesi U et al. (2003) A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 349: 546–553
Horenblas S et al. (2000) Detection of occult metastasis in squamous cell carcinoma of the penis using a dynamic sentinel node procedure. J Urol 1: 100–104
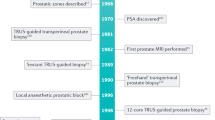
Wawroschek F et al. (1999) The sentinel lymph node concept in prostate cancer—first results of gamma probe-guided sentinel lymph node identification. Eur Urol 6: 595–600
Strand SE and Persson BR (1979) Quantitative lymphoscintigraphy: basic concepts for optimal uptake of radiocolloids in the parasternal lymph nodes of rabbits. J Nucl Med 10: 1038–1046
Paganelli G et al. (1998) Optimized sentinel node scintigraphy in breast cancer. QJ Nucl Med 1: 49–53
Brossner C et al. (2001) Lymphatic drainage of prostatic transition and peripheral zones visualized on a three-dimensional workstation. Urology 2: 389–393
Zuckier LS et al. (1990) Technetium-99m antimony sulphide colloid lymphoscintigraphy of the prostate by direct transrectal injection. Nucl Med Commun 9: 589–596
Wawroschek F et al. (2003) Prostate lymphoscintigraphy for sentinel lymph node identification in canines: reproducibility, uptake, and biokinetics depending on different injection strategies. Urol Res 3: 152–158
Wawroschek F et al. (2003) Prostate lymphoscintigraphy and radio-guided surgery for sentinel lymph node identification in prostate cancer. Technique and results of the first 350 cases. Urol Int 4: 303–310
Mattei A et al. (2006) Number of prostatic sentinel lymph nodes outside of the areas of “limited” versus “extended” pelvic dissection [abstract #614]. Scientific programme of the 21st Annual Congress of the European Association of Urology.
Corvin S et al. (2006) Laparoscopic sentinel lymph node dissection—a novel technique for the staging of prostate cancer. Eur Urol 2: 280–285
Tiourina T et al. (1998) Evaluation of surgical gamma probes for radioguided sentinel node localisation. Eur J Nucl Med 9: 1224–1231
Häcker A et al. Detection of pelvic lymph node metastases in patients with clinically localized prostate cancer: comparison of FCH PET/CT and laparoscopic radioisotope-guided sentinel lymph node dissection. J Urol, in press
Querleu D et al. (1991) Laparoscopic pelvic lymphadenectomy in the staging of early carcinoma of the cervix. Am J Obstet Gynecol 2: 579–581
Schuessler WW et al. (1991) Transperitoneal endosurgical lymphadenectomy in patients with localized prostate cancer. J Urol 5: 988–991
Parra RO et al. (1992) Staging laparoscopic pelvic lymph node dissection. Experience and indications. Arch Surg 11: 1294–1297
Kerbl K et al. (1993) Staging pelvic lymphadenectomy for prostate cancer: a comparison of laparoscopic and open techniques. J Urol 2: 396–398
Kavoussi LR et al. (1993) Complications of laparoscopic pelvic lymph node dissection. J Urol 2: 322–325
Jeschke S et al. (2005) Detection of early lymph node metastases in prostate cancer by laparoscopic radioisotope guided sentinel lymph node dissection. J Urol 6: 1943–1946
Epstein JI et al. (1986) Frozen section detection of lymph node metastases in prostatic carcinoma: accuracy in grossly uninvolved pelvic lymphadenectomy specimens. J Urol 6: 1234–1237
Partin AW et al. (1997) Combination of prostate-specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer. A multi-institutional update. JAMA 277: 1445–1451
Brenot-Rossi I et al. (2005) Limited pelvic lymphadenectomy using the sentinel lymph node procedure in patients with localised prostate carcinoma: a pilot study. Eur J Nucl Med Mol Imaging 6: 635–640
Weingartner K et al. (1996) Anatomical basis for pelvic lymphadenectomy in prostate cancer: results of an autopsy study and implications for the clinic. J Urol 6: 1969–1971
Takashima H et al. (2004) Validity of sentinel lymph node concept for patients with prostate cancer. J Urol 6: 2268–2271
Wawroschek F et al. (2001) Radioisotope guided pelvic lymph node dissection for prostate cancer. J Urol 5: 1715–1719
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Beri, A., Janetschek, G. Technology Insight: radioguided sentinel lymph node dissection in the staging of prostate cancer. Nat Rev Urol 3, 602–610 (2006). https://doi.org/10.1038/ncpuro0625
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpuro0625
This article is cited by
-
99mTc-PSMA targeted robot-assisted radioguided surgery during radical prostatectomy and extended lymph node dissection of prostate cancer patients
Annals of Nuclear Medicine (2022)
-
Non-invasive mapping of deep-tissue lymph nodes in live animals using a multimodal PET/MRI nanoparticle
Nature Communications (2014)
-
Rational design for multifunctional non-liposomal lipid-based nanocarriers for cancer management: theory to practice
Journal of Nanobiotechnology (2013)
-
De schildwachtklierprocedure bij prostaatkanker
Tijdschrift voor Urologie (2012)
-
Purging metastases in lymphoid organs using a combination of antigen-nonspecific adoptive T cell therapy, oncolytic virotherapy and immunotherapy
Nature Medicine (2008)