Abstract
Cirrhotic ascites results from sinusoidal hypertension and sodium retention, which is secondary to a decreased effective arterial blood volume. Transjugular intrahepatic portosystemic shunt (TIPS) placement is currently indicated in cirrhotic patients with refractory ascites who require large-volume paracentesis (LVP) more than two or three times per month. TIPS placement is associated with normalization of sinusoidal pressure and a significant improvement in urinary sodium excretion that correlates with suppression of plasma renin activity, which is, itself, indicative of an improvement in effective arterial blood volume. Compared with serial LVP, placement of an uncovered TIPS stent is more effective at preventing ascites from recurring; however, increased incidence of hepatic encephalopathy and shunt dysfunction rates after TIPS placement are important issues that increase its cost. Although evidence suggests that TIPS placement might result in better patient survival, this needs to be confirmed, particularly in light of the development of polytetrafluoroethylene-covered stents. Favorable results apply to centers experienced in placing the TIPS, with the aim being to decrease the portosystemic gradient to <12 mmHg but >5 mmHg. This article reviews the pathophysiologic basis for the use of a TIPS in patients with refractory ascites, the results of controlled trials comparing TIPS placement (using uncovered stents) versus LVP, and a systematic review of predictors of death after TIPS placement for refractory ascites.
Key Points
-
In most patients with cirrhosis, ascites responds to diuretic therapy
-
TIPS placement corrects the mechanisms that lead to ascites formation and has been compared with LVP for the treatment of patients with ascites refractory to diuretics
-
TIPS placement is more effective than LVP at preventing the recurrence of ascites, but is accompanied by a higher rate of encephalopathy, despite no difference in mortality
-
Serum bilirubin is the best predictor of death in patients who undergo TIPS placement for the treatment of refractory ascites
Similar content being viewed by others
Introduction
Ascites is the most common complication of cirrhosis and its appearance marks the transition from compensated to decompensated cirrhosis. The cumulative probability of developing ascites ranges from 35% to 50% within 5 years of the diagnosis of compensated cirrhosis1,2 and the development of ascites has been shown to be the most common decompensating event.2
As shown in Figure 1, in patients with cirrhosis, ascites develops as a result of hepatic sinusoidal hypertension, which is caused by a postsinusoidal obstruction secondary to structural abnormalities related to cirrhosis (fibrosis and compression from regenerating nodules). In addition to the presence of these permanent structural abnormalities, there is a functional component to the development of sinusoidal hypertension: active vasoconstriction that (in an experimental model of cirrhosis with ascites) has been shown to occur mostly in the postsinusoidal area.3 As is necessary for the formation of varices, a threshold sinusoidal pressure of 12 mmHg needs to be reached for ascites to develop.4,5 Indeed, significantly fewer patients develop ascites if their hepatic venous pressure gradient (HVPG; a measure of sinusoidal pressure) decreases to below 12 mmHg or by more than 20% from the baseline value.6 In a longitudinal study of 122 patients in whom a transjugular intrahepatic portosystemic shunt (TIPS) was placed for variceal hemorrhage, the portosystemic pressure gradient increased above 12 mmHg in all patients who developed ascites after TIPS placement.7 Indirect confirmation of this threshold comes from studies of the serum–ascites albumin gradient (a measurement that correlates with the HVPG) in the differential diagnosis of ascites; the serum–ascites albumin gradient cutoff level for cirrhotic ascites is greater than 11 g/l, which corresponds to an HVPG of 11–12 mmHg.8
Cirrhosis leads to hepatic venous outflow block, which is both anatomical (regenerative nodules and fibrosis) and functional (increased postsinusoidal intrahepatic vascular tone) and, therefore, leads to an increased sinusoidal pressure. In addition, portal hypertension leads to splanchnic and systemic arteriolar vasodilatation, decreased effective arterial blood volume, increased activity of sodium-retaining hormones, sodium and water retention and, consequently, plasma-volume expansion. Sinusoidal hypertension drives fluid out of the sinusoids and into the peritoneal cavity while the intravascular fluid is continuously replenished by the process of plasma-volume expansion. The TIPS acts as a side-to-side portocaval shunt, thereby decompressing the hepatic sinusoids. In addition, the TIPS also increases the effective arterial blood volume by shunting portal venous blood into the systemic circulation. Abbreviation: TIPS, transjugular intrahepatic portosystemic shunt.
The formation of ascites would be a limited process if sinusoidal hypertension was the only mechanism responsible for its development, because the development would cease once the intravascular volume became depleted. A second important mechanism that must occur in cirrhotic patients, therefore, is the replenishment of the intravascular volume (plasma volume expansion) through sodium retention. Sodium retention occurs secondary to splanchnic and systemic vasodilation, which is common in patients with cirrhosis (particularly when their cirrhosis is at an advanced stage). The vasodilation leads to a decrease in the effective arterial blood volume and the activation of neurohumoral systems (e.g. the renin–angiotensin–aldosterone system) that cause sodium retention (Figure 1).9 Nitric oxide is a potent vasodilator that has been proposed as a major mediator of the arterial dilation and hyperdynamic circulation in patients with cirrhosis.10 In experimental cirrhosis, inhibition of endothelial nitric oxide synthase (sufficient to normalize systemic vascular resistance) was associated with a reversal of the elevation in plasma renin activity (PRA) and aldosterone concentration, an increase in sodium and water excretion, and a decrease in ascites volume.11 This is proof of concept that vasodilation has an important role in sodium retention in the setting of cirrhotic ascites.
In most cases, cirrhotic ascites is resolved through dietary sodium restriction and/or the use of diuretics to achieve a negative sodium balance. In 10–20% of cirrhotic patients, however, ascites becomes refractory to diuretics and sodium restriction, either because diuretic-induced complications prevent the dose of diuretic from being increased or because the ascites persists despite administration of the maximum dose of diuretics (400 mg spironolactone plus 160 mg furosemide per day).12 The development of refractory ascites denotes that the liver disease is more advanced, with further vasodilation and activation of neurohumoral systems and a increased mortality rate.13 For patients with refractory ascites, therapies other than diuretics need to be considered as a temporary measure until liver transplantation is possible.
Pathophysiologic basis for tips placement
The placement of surgical portosystemic shunts decreases the development of ascites.14 The side-to-side and end-to-side portocaval shunts are both effective for the treatment of variceal hemorrhage through decompression of the portal venous system. The side-to-side shunt is, however, more effective than the end-to-side shunt in decreasing ascites formation, as shown experimentally15 and in humans.16
By connecting the side of the portal vein to the low-pressure inferior vena cava, the side-to-side shunt effectively decompresses not only the extrahepatic portal venous system but also the sinusoids. The end-to-side shunt decompresses the portal system and decreases flow into the hepatic sinusoids, but it does not effectively decompress them, particularly in patients with advanced cirrhosis, for whom the portal vein becomes an outflow tract. In this situation, placement of an end-to-side shunt closes off this decompressing outflow tract, resulting in a higher sinusoidal pressure and increased ascites formation. Given the high operative morbidity and mortality rates in patients with advanced cirrhosis and refractory ascites, and the high rate of severe hepatic encephalopathy, the surgical side-to-side portocaval shunt is not used for the treatment of refractory ascites.
TIPS placement is a nonsurgical, percutaneous procedure. A portosystemic shunt is established inside the liver parenchyma by connecting a main portal branch with a large hepatic vein. The parenchymal tract is kept open by an expandable metallic stent. This portosystemic shunt decompresses both the portal venous system and the sinusoids, effectively acting as a side-to-side portocaval shunt, but without the morbidity and mortality rates associated with major surgery. Given the threshold portal pressure gradient of 12 mmHg that is necessary for the formation of ascites, the TIPS should be expanded to a diameter sufficient to decrease the portosystemic gradient to levels below this threshold.
In addition to sinusoidal decompression, TIPS placement has the advantage of increasing the effective arterial blood volume, at least transiently, by transferring blood volume from the splanchnic to the systemic circulation (Figure 1).
Effect of a tips on hemodynamics and sodium retention
Table 1 summarizes the changes that occur in cirrhotic patients who have refractory ascites and then undergo TIPS placement. Immediately after TIPS placement, there is an increase in cardiac output, a decrease in systemic vascular resistance (which is already decreased at baseline in these patients), and a worsening of liver synthetic function (as shown by an increase in Child–Turcotte–Pugh [CTP] score; Table 2).17 These changes are no longer present 3 months or more after TIPS insertion.17,18,19,20 Although it could be argued that the decrease in calculated systemic vascular resistance might just be an effect of the increase of cardiac output, after TIPS placement there is an increase in flow that leads to increased shear stress, an increase in nitric oxide, and an increase in vasodilation. In turn, this increase in vasodilation leads to volume expansion and to an increase in cardiac output. The mean portosystemic pressure gradient is significantly reduced, compared with baseline, up to 14 months after TIPS placement, although this effect seems to decrease progressively over time, probably as a result of dysfunction of the stent.18
Despite deterioration of the hyperdynamic circulatory state and of liver synthetic function, urinary sodium excretion increases significantly as soon as 7 days21 and not later than 1 month after TIPS placement.19,20,22,23 The increase in urinary sodium excretion correlates closely with a decrease in PRA and aldosterone levels,17,18,19,20,21,23 indicating that there is an improvement in the effective arterial blood volume. The increase in urinary sodium excretion persists 7–14 months after TIPS placement18,20 and, at this time point, the CTP score is improved (compared with that seen before TIPS placement),18,20 probably as a result of the resolution of ascites, which is one component of the score.
These beneficial effects led to several uncontrolled trials of TIPS placement in patients with refractory ascites, which showed that TIPS placement eliminates ascites or makes it easier to manage in approximately 70% of patients, although almost all patients still need to use diuretics.24
Disadvantages of the tips
Despite all the beneficial effects of a TIPS, the diversion of blood flow away from the liver through the shunt can lead to the development of liver failure and/or hepatic encephalopathy. New or worse encephalopathy occurs in approximately a third of patients who undergo TIPS placement for refractory ascites,25 a rate not unlike that described in trials of TIPS placement for the treatment of variceal hemorrhage. A history of pre-TIPS encephalopathy has been found to be the most predictive parameter of post-TIPS encephalopathy,26,27,28 followed by age greater than 65 years,29,30 and a low post-TIPS portosystemic gradient.28,29 So, although the goal of TIPS placement is to reduce the portosystemic gradient to less than 12 mmHg, too low a reduction (e.g. to levels <5 mmHg) might precipitate encephalopathy.28 Interestingly, loss of portal perfusion (i.e. hepatofugal flow) has been identified as a negative predictor of post-TIPS encephalopathy.30 It should be mentioned that most patients with post-TIPS encephalopathy respond to standard therapy and only about 3–10% develop intractable encephalopathy that might require stent narrowing.26,29
Another problem, at least with the use of uncovered stents, is the frequent rate of TIPS dysfunction caused by narrowing or occlusion of the stent. TIPS dysfunction progresses with time so that, by the first year after TIPS placement, more than half the patients require stent revision.7
It has been shown that both TIPS dysfunction and encephalopathy decrease significantly with the use of polytetrafluoroethylene-covered stents;31 however, all data presented in this article refer to uncovered stents because the trials published so far precede the advent of covered stents.
The procedural complications of TIPS placement in patients with refractory ascites is around 9%, with intraperitoneal hemorrhage being the most common complication.32
Controlled trials of an uncovered tips versus LVP
Large-volume paracentesis (LVP) is the standard treatment for refractory ascites.33 It is a local therapy that does not modify any of the mechanisms that lead to ascites formation. Recurrence of ascites is, therefore, practically universal in patients who undergo LVP, unless there is an improvement in liver disease (e.g. resolution of alcoholic hepatitis). In addition, LVP causes further deterioration in the hemodynamic status of cirrhotic patients, leading to the condition of 'postparacentesis circulatory dysfunction'—defined by an increase in PRA 6 days after LVP. Postparacentesis circulatory dysfunction leads to faster reaccumulation of ascites, a higher susceptibility to the development of renal dysfunction, and a higher mortality rate compared with patients who do not develop this condition.34,35 The incidence of postparacentesis circulatory dysfunction is lowest (∼15%) when LVP is associated with the concomitant intravenous albumin infusion.34,36
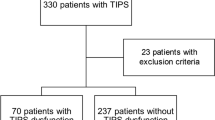
So far, five prospective, randomized trials comparing TIPS placement (using uncovered stents) with LVP plus albumin have been published in full.23,37,38,39,40 The studies include a total of 330 patients, whose baseline characteristics are described in Table 3. Not unexpectedly, all five trials demonstrate that TIPS placement is more effective than LVP in preventing the recurrence of ascites (Table 4) and, with the exception of one study,37 all studies demonstrate a higher incidence of encephalopathy23,39 or severe encephalopathy38,40 in patients treated with a TIPS. Results on mortality are more heterogeneous. The earliest trial, published by Lebrec et al. in 1996, is the only one to show a higher mortality in patients randomly assigned to receive a TIPS, compared with those undergoing LVP.23 This study also had the highest rate of technical failures and reported the lowest reduction in portosystemic pressure (Table 1), suggesting that expertise in terms of performing the procedure might have been limited at this time, compared with subsequent trials. Two of the later trials, published in 2002 and 2003 by Gines et al. and Sanyal et al., respectively, include the largest number of patients and show no significant difference in mortality between the TIPS and LVP groups.38,39 The most recent of these trials, by Salerno et al. in 2004, shows a significant survival benefit in favor of the TIPS group.40 In the remaining trial, by Rossle et al., TIPS placement was independently predictive of a better survival, but differences in survival probability were not statistically different between TIPS and LVP.37 Overall, (considering the median effect of the five trials) ascites recurs in 48% of patients treated with an uncovered TIPS (compared with 84% of patients treated with LVP), new or worse encephalopathy occurs in 42% (23% in the LVP group), the stent becomes dysfunctional in 41%, and the mortality rate is 48% (51% in the LVP group) (Table 4). The 51% pooled death rate in the control LVP group is higher than the 30–35% expected from sample-size calculations of these studies; the highest mortality rate was seen in the study by Rossle et al., and the lowest (37%) in the study by Sanyal et al. The higher mortality rate in the Rossle study is difficult to explain, but the lower rate in the Sanyal study probably related to lower creatinine levels (patients with a creatinine levels >15 mg/l were excluded) and a high rate of liver transplantation in the study population.
There have been four separate meta-analyses of the TIPS versus LVP plus albumin trials: one when four of the studies had been published,41 and three including all five trials42,43,44 All reached the same conclusion, that is, that TIPS placement is more effective than LVP for the control of refractory ascites and that it increases the occurrence of encephalopathy, without significantly affecting mortality.
Interestingly, the 16% difference in risk of encephalopathy between patients undergoing LVP or TIPS placement (30% for LVP, 46% for TIPS) is the same difference in risk as has been described between 'conventional' treatment and TIPS placement in studies of TIPS placement for variceal hemorrhage (19% for conventional treatment, 35% for TIPS).45 Higher baseline rates of encephalopathy in studies of patients with refractory ascites indicate that these are sicker patients than those with variceal hemorrhage.
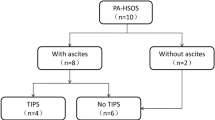
Regarding mortality rates, two meta-analyses recognized the presence of heterogeneity among the trials,43,44 and in one of them,43 multivariate metaregression analysis for mortality identified an outlier trial23 (Figure 2). Re-analysis after exclusion of this trial showed a clear trend for better survival after treatment with a TIPS, compared with LVP (Figure 2)43 and identified the serum bilirubin concentration as the only pre-TIPS predictor of survival (Figure 3). Unfortunately, owing to missing data, this metaregression analysis did not include other potentially important prognostic parameters, such as urinary sodium concentrations. In the two trials that showed a survival benefit, TIPS patients had elevated urinary sodium levels at baseline37,40 (Table 3), which are indicative of reduced activation of sodium-retaining neurohumoral systems and, therefore, of less vasodilatation and less-advanced liver disease. On univariate analysis, there was a significant association between the urinary sodium level and the risk of death after TIPS placement (D'Amico, personal communication). Of note, these two trials37,40 also included a proportion of patients with 'recidivant ascites' (Table 3). Unlike refractory ascites (defined as a less than 200 g weight loss per day, despite maximal diuretic therapy), recidivant ascites is the recurrence of tense ascites at least three times in the course of 12 months. Patients with recidivant ascites still respond to diuretics, however, and have, at least theoretically, less-severe liver disease.
Pooled odds ratio for the recurrence of ascites, the development of encephalopathy, death in all five trials and death excluding the outlier trial are shown. Pooled odds ratios to the left of the equivalence line (odds ratio = 1) indicate a benefit with TIPS placement, while pooled odds ratios to the right of the equivalence line indicate harm with TIPS placement. The numbers represent the pooled odds ratio (95% CI). Although the heterogeneity test was significant for death, it was no longer significant when an outlier trial was excluded. Abbreviation: TIPS, transjugular intrahepatic portosystemic shunt. Figure modified with permission from reference 43 © (2005) the American Gastroenterological Association.
Each trial is represented by an open circle and the area of each circle is proportional to the variance of each log-odds ratio estimate. Serum bilirubin was the only pre-TIPS parameter that was independently predictive of death. Abbreviation: TIPS, transjugular intrahepatic portosystemic shunt. Figure kindly provided by Dr D'Amico and reproduced with permission from reference 43 © (2005) the American Gastroenterological Association.
In the one randomized, controlled trial that evaluated quality of life using the SF-36 questionnaire, similar changes in the quality of life of both study groups were seen.39 Further analysis of this issue shows that the competing effects of hepatic encephalopathy (more frequent in the TIPS group), requirement for repeated LVP (more frequent in the LVP group), and need for hospitalization (more frequent in the TIPS group) explain similar changes in the quality of life between the two groups.46
The one randomized, controlled trial that has evaluated cost showed that the calculated costs were greater for TIPS placement than LVP (both in the US and Spain). This finding is probably related to a high rate of TIPS dysfunction requiring shunt revision.30
Unresolved issues, particularly determining whether there is a survival benefit of TIPS placement in the setting of refractory ascites, justify the performance of future trials of TIPS using covered stents that, as mentioned previously, have been associated with less-frequent development of shunt dysfunction and hepatic encephalopathy.31 These trials should stratify patient groups by predictors of post-TIPS placement mortality (see below) and assess the quality-of-life and cost factors associated with TIPS placement.
Predictors of mortality after tips placement
Table 5 shows the results of nine studies that have assessed predictors of long-term (>6 months) mortality, after TIPS placement, by multivariable analysis of data from patients who underwent TIPS placement for refractory ascites.43,47,48,49,50,51,52,53,54 One of these studies is the previously mentioned meta-analysis of five randomized trials of TIPS placement versus LVP, in which metaregression multivariable analysis for mortality was performed.43
As seen in Table 5, the two most common independent predictors of death after TIPS placement were the serum bilirubin level and the serum creatinine level, both of which were introduced in the multivariable analysis of all nine studies and were significant independent predictors of post-TIPS mortality in five of them (56%).
The three largest trials noted a significantly higher mortality rate in patients for whom the indication for TIPS placement was refractory ascites, compared with those who underwent TIPS placement for variceal hemorrhage;48,50,54 the validity of predictors obtained from studies combining these two populations is, therefore, somewhat questionable. This combining of patient populations and data overfitting (when the ratio of the number of deaths to the number of variables <10), which occurred in most of the studies, further decrease the validity of these predictors (Table 5). The common methodologic errors of combining patients at different stages of disease and of overfitting have been discussed in a systematic review of predictors of death in patients with cirrhosis.55
Perhaps the most reliable information is obtained by analyzing the two studies that included only those patients in whom a TIPS was placed for the management of refractory ascites,43,51 particularly the paper whose results are derived from the meta-analysis of the five randomized trials.43 In both these studies, the serum bilirubin level was the only independent pre-TIPS predictor of death (Figure 3). It has been suggested that the cutoff level that identifies a higher mortality rate is a bilirubin concentration greater than 51.3 µmol/l.56
Candidates for tips placement
Consensus recommendations, mainly based on the five randomized, controlled trials described above, propose that LVP plus albumin be used as the first-line treatment for patients with refractory ascites, and that TIPS placement be considered in patients intolerant of repeated LVP48 or when the frequency of LVP is greater than 2–3 times per month.33
Consensus recommendations also suggest that an age greater than 70 years, pre-existing cardiac dysfunction, and a CTP score greater than 11 should be considered as contraindications to TIPS placement in the setting of refractory ascites.33
Although the MELD score was initially designed to predict survival 3 months after TIPS placement,48 it is now mostly used in clinical practice to allocate organs for liver transplantation, rather than to determine TIPS candidacy. In addition, in the initial MELD study,48 only 25% of patients had a TIPS placed for the management of refractory ascites (Table 5) and the results, therefore, might not be applicable to this patient population. The CTP score is more practical and applicable in the clinical setting and has been shown to be equivalent to the MELD score in predicting survival 1 month, 3 months, and 1 year after TIPS placement.50 Although, as discussed above, the CTP score has not been found to be an independent predictor of mortality after TIPS placement, a component of the CTP score—the serum bilirubin concentration—seems to be the strongest predictor of long-term survival. In addition, the serum bilirubin concentration might be the decisive factor in reaching the CTP cutoff score of 11, because patients with refractory ascites have, by definition, the highest score for ascites (i.e. tense ascites) and most have the highest score for albumin (i.e. a level <28 g/l) (Table 2). Of note, a CTP cutoff of 11 was used as an exclusion criterion in the only trial to show a survival benefit for TIPS placement over LVP.40
Monitoring after tips placement
Although studies report that patients treated with a TIPS require lower doses of diuretics, it seems that all patients continue to require diuretics, probably because TIPS placement improves, but does not normalize, sodium excretion.18 The use of diuretics immediately after the procedure is advisable because, at least theoretically, diuretics will increase flow through the shunt by reducing central pressure more than portal pressure.
Serial assessments of stent patency might be warranted when TIPS placement is indicated for variceal hemorrhage; however, when TIPS placement is performed for refractory ascites, serial evaluation of the functionality of the stent is not necessary unless there is recurrence of ascites, a clinically obvious event that is indicative of stent dysfunction.
In a randomized, controlled trial published in 2005, prophylactic therapy for hepatic encephalopathy (with lactitol or rifaximin) was shown to be ineffective in preventing the development of hepatic encephalopathy in the month after TIPS placement and this prophylaxis is, therefore, not recommended.49
Another study indicates that patients who received uncovered TIPS stents are at greater risk of developing hepatocellular carcinoma than controls matched for cause and severity of liver disease.50 This finding suggests that patients who receive uncovered stents have need of a stricter hepatocellular carcinoma surveillance program, but this should not be considered a reason not to perform TIPS placement, particularly since these results have not been confirmed, and concerns regarding selection bias in this study have been raised.51
Conclusions
Since 1993, when the first pilot study of TIPS placement for the treatment of refractory ascites was published,57 a number of studies have helped elucidate the mechanism of action underlying TIPS placement, and have helped place the TIPS in the context of therapy for refractory ascites. Although the placement of uncovered TIPS stents improves ascites, it is associated with greater encephalopathy rates than LVP and high rates of stent dysfunction. In the treatment of refractory ascites, the placement of uncovered TIPS stents is, therefore, currently relegated to a secondary position, after LVP plus albumin. TIPS placement seems to be associated with a better survival in a subpopulation of patients with ascites, however, and, over the next decade, clinical trials that include coated stents for TIPS and use risk stratification will help elucidate the best candidates for TIPS placement.
Review criteria
PubMed was searched for relevant articles in October 2005 using the terms “transjugular” and “ascites”. Papers from the author's personal collection were also included. For the analysis of predictors of survival after TIPS placement the following MEDLINE search terms were used: “(survival [ALL] OR mortality [ALL] OR predictor [ALL] OR prognosis [ALL] OR prognostic [ALL]) AND (multivariate OR Cox OR Cox's OR adjusted OR adjustment OR logistic [ALL]) AND transjugular AND ascites”. Papers were considered if they were published in English, if survival analysis was reported, and if a multivariable analysis of prognostic indicators of death risk was performed.
References
Gines P et al. (1987) Compensated cirrhosis: natural history and prognosis. Hepatology 7: 122–128
D'Amico G et al. (1986) Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci 31: 468–475
Loureiro-Silva MR et al. (2003) Deficit in nitric oxide production in cirrhotic rat livers is located in the sinusoidal and postsinusoidal areas. Am J Physiol Gastrointest Liver Physiol 284: G567–G574
Rector WG (1986) Portal hypertension: a permissive factor only in the development of ascites and variceal bleeding. Liver 6: 221–226
Morali GA et al. (1992) Is sinusoidal portal hypertension a necessary factor for the development of hepatic ascites? J Hepatol 16: 249–250
Abraldes JG et al. (2003) Hemodynamic response to pharmacological treatment of portal hypertension and long-term prognosis of cirrhosis. Hepatology 37: 902–908
Casado M et al. (1998) Clinical events after transjugular intrahepatic portosystemic shunt: correlation with hemodynamic findings. Gastroenterology 114: 1296–1303
Hoefs JC (1983) Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patients with chronic liver disease. J Lab Clin Med 102: 260–273
Schrier RW et al. (1988) Peripheral arterial vasodilation hypothesis—a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 8: 1151–1157
Martin PY et al. (1998) Nitric oxide as a mediator of hemodynamic abnormalities and sodium and water retention in cirrhosis. N Engl J Med 339: 533–541
Martin PY et al. (1998) Nitric oxide synthase (NOS) inhibition for one week improves renal sodium and water excretion in cirrhotic rats with ascites. J Clin Invest 101: 235–242
Arroyo V et al. (1996) Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology 23: 164–176
Salerno F et al. (1993) Survival and prognostic factors of cirrhotic patients with ascites: a study of 134 outpatients. Am J Gastroenterol 88: 514–519
Castells A et al. (1994) Impact of shunt surgery for variceal bleeding in the natural history of ascites in cirrhosis: a retrospective study. Hepatology 20: 584–591
Orloff MJ et al. (1997) Experimental, clinical, and metabolic results of side-to-side portacaval shunt for intractable cirrhotic ascites. J Am Coll Surg 183: 557–570
Voorhees ABJ et al. (1970) Portasystemic shunting procedures for portal hypertension. Twenty-six year experience in adults with cirrhosis of the liver. Am J Surg 119: 501–505
Wong F et al. (1995) Transjugular intrahepatic portosystemic stent shunt: effects on hemodynamics and sodium homeostasis in cirrhosis and refractory ascites. Ann Intern Med 122: 816–822
Quiroga J et al. (1995) Transjugular intrahepatic portal-systemic shunt in the treatment of refractory ascites: effect on clinical, renal, humoral, and hemodynamic parameters. Hepatology 21: 986–994
Wong F et al. (1997) The mechanism of the initial natriuresis after transjugular intrahepatic portosystemic shunt. Gastroenterology 112: 899–907
Wong W et al. (1999) Long-term renal sodium handling in patients with cirrhosis treated with transjugular intrahepatic portosystemic shunts for refractory ascites. Am J Med 106: 315–322
Gerbes AL et al. (1998) Renal effects of transjugular intrahepatic portosystemic shunt in cirrhosis: comparison of patients with ascites, with refractory ascites or without ascites. Hepatology 28: 683–688
Somberg KA et al. (1995) Transjugular intrahepatic portosystemic shunts for refractory ascites: assessment of clinical and hormonal response and renal function. Hepatology 21: 709–716
Lebrec D et al. (1996) Transjugular intrahepatic portosystemic shunts: comparison with paracentesis in patients with cirrhosis and refractory ascites: a randomized trial. J Hepatol 25: 135–144
Garcia-Tsao G (2005) Transjugular intrahepatic portosystemic shunt in the management of refractory ascites. Semin Interventional Rad 22: 278–286
Russo MW et al. (2003) Transjugular intrahepatic portosystemic shunt for refractory ascites: an analysis of the literature on efficacy, morbidity, and mortality. Am J Gastroenterol 98: 2521–2527
Sanyal AJ et al. (1994) Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology 20: 46–54
Nolte W et al. (1998) Portosystemic hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in patients with cirrhosis: clinical, laboratory, psychometric, and electroencephalographic investigations. Hepatology 28: 1215–1225
Riggio O et al. (2005) Pharmacological prophylaxis of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt: a randomized controlled study. J Hepatol 42: 674–679
Riggio O et al. (1996) Hepatic encephalopathy after transjugular intrahepatic portosystemic shunt. Incidence and risk factors. Dig Dis Sci 41: 578–584
Hassoun Z et al. (2001) Relationship between pre-TIPS liver perfusion by the portal vein and the incidence of post-TIPS chronic hepatic encephalopathy. Am J Gastroenterol 96: 1205–1209
Bureau C et al. (2004) Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology 126: 469–475
Boyer TD and Haskal ZJ (2005) The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology 41: 386–400
Moore KP et al. (2003) The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology 38: 258–266
Gines A et al. (1996) Randomized trial comparing albumin, dextran-70 and polygeline in cirrhotic patients with ascites treated by paracentesis. Gastroenterology 111: 1002–1010
Ruiz del Arbol L et al. (1997) Paracentesis-induced circulatory dysfunction: mechanism and effect on hepatic hemodynamics in cirrhosis. Gastroenterology 113: 579–586
Sola-Vera J et al. (2003) Randomized trial comparing albumin and saline in the prevention of paracentesis-induced circulatory dysfunction in cirrhotic patients with ascites. Hepatology 37: 1147–1153
Rossle M et al. (2000) A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med 342: 1701–1707
Gines P et al. (2002) Transjugular intrahepatic portosystemic shunting versus repeated paracentesis plus intravenous albumin for refractory ascites in cirrhosis: a multicenter randomized comparative study. Gastroenterology 123: 1839–1847
Sanyal AJ et al. (2003) The North American Study for the Treatment of Refractory Ascites. Gastroenterology 124: 634–641
Salerno F et al. (2004) Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology 40: 629–635
Saab S et al. (2004) TIPS versus paracentesis for cirrhotic patients with refractory ascites. The Cochrane Database of Systematic Reviews, Issue 3, Art. No CD004889
Deltenre P et al. (2005) Transjugular intrahepatic portosystemic shunt in refractory ascites: a meta-analysis. Liver Int 25: 349–356
D'Amico G et al. (2005) Uncovered transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis. Gastroenterology 129: 1282–1293
Albillos A et al. (2005) A meta-analysis of transjugular intrahepatic portosystemic shunt versus paracentesis for refractory ascites. J Hepatol 43: 990–996
Luca A et al. (1999) TIPS for prevention of recurrent bleeding in patients with cirrhosis: meta-analysis of randomized clinical trials. Radiology 212: 411–421
Campbell MS et al. (2005) Quality of life in refractory ascites: transjugular intrahepatic portal-systemic shunting versus medical therapy. Hepatology 42: 635–640
Chalasani N et al. (2000) Determinants of mortality in patients with advanced cirrhosis after transjugular intrahepatic portosystemic shunting. Gastroenterology 118: 138–144
Malinchoc M et al. (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31: 864–871
Russo MW et al. (2002) Predictors of mortality and stenosis after transjugular intrahepatic portosystemic shunt. Liver Transpl 8: 271–277
Angermayr B et al. (2003) Child–Pugh versus MELD score in predicting survival in patients undergoing transjugular intrahepatic portosystemic shunt. Gut 52: 879–885
Thuluvath PJ et al. (2003) TIPS for management of refractory ascites: response and survival are both unpredictable. Dig Dis Sci 48: 542–550
Alessandria C et al. (2004) Application of the model for end-stage liver disease score for transjugular intrahepatic portosystemic shunt in cirrhotic patients with refractory ascites and renal impairment. Eur J Gastroenterol Hepatol 16: 607–612
ter Borg PC et al. (2004) Transjugular intrahepatic portosystemic shunts: long-term patency and clinical results in a patient cohort observed for 3–9 years. Radiology 231: 537–545
Membreno F et al. (2005) Differences in long-term survival after transjugular intrahepatic portosystemic shunt for refractory ascites and variceal bleed. J Gastroenterol Hepatol 20: 474–481
D'Amico G et al. (2006) Natural history and prognostic indicators of survival in cirrhosis. A systematic review of 118 studies. J Hepatol 44: 217–231
Gerbes AL and Gulberg V (2005) Benefit of TIPS for patients with refractory or recidivant ascites: serum bilirubin may make the difference. Hepatology 41: 217
Ferral H et al. (1993) Refractory ascites: early experience with transjugular intrahepatic portosystemic shunt. Radiology 189: 795–80155
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing financial interests.
Rights and permissions
About this article
Cite this article
Garcia-Tsao, G. The transjugular intrahepatic portosystemic shunt for the management of cirrhotic refractory ascites. Nat Rev Gastroenterol Hepatol 3, 380–389 (2006). https://doi.org/10.1038/ncpgasthep0523
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpgasthep0523