Abstract
Acute kidney injury (AKI) involves nephron injury leading to irreversible nephron loss, ie, chronic kidney disease (CKD). Both AKI and CKD are associated with distinct histological patterns of tissue injury, but kidney atrophy in CKD involves tissue remodeling with interstitial inflammation and scarring. No doubt, nephron atrophy, inflammation, fibrosis, and renal dysfunction are associated with each other, but their hierarchical relationships remain speculative. To better understand the pathophysiology, we provide an overview of the fundamental danger response programs that assure host survival upon traumatic injury from as early as the first multicellular organisms, ie, bleeding control by coagulation, infection control by inflammation, epithelial barrier restoration by re-epithelialization, and tissue stabilization by mesenchymal repair. Although these processes assure survival in the majority of the populations, their dysregulation causes kidney disease in a minority. We discuss how, in genetically heterogeneous population, genetic variants shift balances and modulate danger responses toward kidney disease. We further discuss how classic kidney disease entities develop from an insufficient or overshooting activation of these danger response programs. Finally, we discuss molecular pathways linking, for example, inflammation and regeneration or inflammation and fibrosis. Understanding the causative and hierarchical relationships and the molecular links between the danger response programs should help to identify molecular targets to modulate kidney injury and to improve outcomes for kidney disease patients.
Similar content being viewed by others
Main
The pathology of kidney diseases is exceptionally diverse because of the complex cellular composition and anatomy of the nephrons. It is largely characterized by a mix of intrinsic injurious pathomechanisms destroying some nephrons together with concomitant healing responses that try to stabilize the other nephrons. Still, a variety of different triggers can induce similar histopathological lesions in the kidney, for example, glomerular crescents, focal segmental glomerulosclerosis (FSGS), mesangial proliferation, thrombotic microangiopathy, tubular necrosis, or interstitial fibrosis. Therefore, a kidney biopsy often displays non-specific lesions, which require clinical and laboratory correlation for a definite diagnosis. In addition, kidney pathology manifests with distinct patterns of structural abnormalities, raising the question of potential causative hierarchical relationships. In this review, we address this topic taking the approach of evolutionary medicine to better understand why kidney injury generates distinct histological lesions and how they are causatively related. This conceptual approach appears superior in delineating the most likely molecular and cellular targets to therapeutically modulate kidney disease for better outcomes. In particular, we focus on the molecular links between distinct danger response programs as these may be most powerful in modulating complex disease processes.
DANGER RESPONSE PROGRAMS SAVE LIFE, USUALLY
Both plants and animals control traumatic injuries either by regeneration or repair.1 Traumatic injuries disrupt epithelial barriers, which imply a number of dangers to homeostasis, including the risks of fluid loss and microbial infection. These dangers required control mechanisms (constraints) from early on in the evolution of multicellular organisms and those that were maintained during evolution up to humans obviously resulted in significant survival benefits that outweigh collateral injuries or tissue remodeling. Such trade-offs under certain conditions can translate into pathomechanisms and drive disease progression. In the following paragraphs, we will introduce the four major danger response programs: coagulation, inflammation, re-epithelialization, and mesenchymal repair and discuss their pathogenic roles in kidney disease.2
Vascular Injury Induces Coagulation Rapidly to Minimize Bleeding
Traumatic injury of blood vessels causes bleeding. Clotting minimizes the risk of hemorrhagic shock, eg, hemolymph aggregation in arthropods, and presents as a more complex interplay of activated endothelial cells, coagulation factors, and platelets in vertebrates.3 Although clotting minimizes short-term risks, intravascular coagulation or thromboembolism can create subsequent side effects (conflicts), such as tissue hypoperfusion and ischemia.4, 5
Epithelial Barrier Injuries and Coagulation Induce Inflammation as a Functional Barrier Against infection
The evolution of multicellular organisms is strongly influenced by the balance between microbial virulence factors and antimicrobial host defense.6 Wounds disrupt barriers that protect from pathogen entry; vice versa, wounding implies the risk for infection. Hence, inflammatory response intends to rapidly install a functional barrier against pathogen entry and spreading.7, 8 Pathogen-derived pathogen-associated molecular patterns (PAMPs) and intrinsic cell death-related damage-associated molecular patterns (DAMPs) activate the identical pattern-recognition receptors either in infectious or in sterile inflammation.9, 10, 11, 12, 13 There is a close link between clotting (the process that changes blood from liquid to gel) and inflammation, as platelet activation and aggregation induces release of cytokines and chemokines from platelet granules that promote recruitment of leukocytes and local inflammation, a process referred to as immunothrombosis.14, 15, 16, 17 For example, platelet-derived chemokines foster neutrophil recruitment that eventually undergo NETosis, a form of pathogen-induced cell death during which neutrophil extracellular traps (NETs) are released and which further fuels into inflammation.18, 19, 20 The inflammatory response triggers immunopathology and loss of parenchymal cells similar to pyoderma gangrenosum but the same occurs inside the kidney.21 In sepsis, massive activation of cytokine release (cytokine storm) is the major factor and cause of mortality in early sepsis, while the compensatory downregulation of innate immunity accounts for secondary infection-related mortality in late sepsis.22
Epithelial Injury Requires Re-Epithelialization to Minimize Fatal Infection And Fluid Loss
Epithelial injuries require rapid regeneration of the barrier to limit fluid losses and pathogen entry similar to skin burns or ulcerative enteritis.23, 24 Similarly, glomerular epithelial defects cause proteinuria. Furthermore, epithelial transport is another important function of the epithelium to facilitate nutrient absorption (gut), gas exchange (lungs), or solute secretion/reabsorption (kidney). Upon injury, rapid restoration is needed to maintain the function of the corresponding organ, eg, by signals inducing re-epithelialization from wound edges. Already coagulation produces mitogenic factors activating proliferation of surviving epithelial cells.25 Mediators that link coagulation, inflammation, and re-epithelialization include growth factors (epidermal growth factor (EGF), FGFs, hepatocyte growth factor (HGF), TGF-β), cytokines (IL-6, IL-17, IL-22), chemokines (fractalkine, CXCL10) and microRNAs triggering proliferation of epithelial cells with regenerative capacities.26, 27, 28, 29, 30, 31, 32 In the past years, an important contribution of miRNA to cutaneous wound healing has been described.33 These miRNAs are involved in different physiological processes, such as human monocyte/macrophage differentiation (miR-424), Toll-like receptor (TLR)-associated signaling events (miR-147), collagen deposition, and TGF-β-mediated wound contraction (miR-21) or modulating p63 expression (miR-203) during keratinocyte differentiation and in epithelial development.34, 35, 36, 37 Modulating the expression of these miRNA will allow the development of new therapeutic opportunities in wound healing.
The intrinsic regenerative capacity for re-epithelialization largely relates to local progenitor cells committed to the specific epithelial lineage phenotype.23, 38, 39 Insufficient re-epithelialization is associated with persistence of chronic wounds, increasing the risk for infection. In contrast, uncoordinated epithelial hyperplasia can become a pathological mechanism, such as in glomerular crescent formation.40
Tissue Defects Induce Mesenchymal Repair to Restore Tissue Integrity
The reconstitution of parenchymal cell losses requires stabilizing scaffolds that guide parenchymal reconstitution to rebuild structural organization. This scaffold is created by mesenchymal elements within the tissue, eg, fasciae, periosteum, nerve sheaths, vascular pericytes, or interstitial fibroblasts. Therefore, epithelial growth factors driving epithelial healing are released together with mesenchymal growth factors that drive a concurrent mesenchymal healing response that may be transient, depending on epithelial healing completion. If epithelial healing remains incomplete, persistent release of mesenchymal growth factors can promote fibrosis.41 For example, insufficient reconstitution of renal epithelial cells is associated with mesenchymal healing. Epithelial–mesenchymal transition (EMT) and arrest in the G2/M phase of the cell cycle is associated with pro-fibrotic TGF-β cytokine secretion.42 Collagen-producing fibroblasts accumulate mainly via recruitment from bone marrow-derived precursors or by proliferation of resident fibroblasts transforming to myofibroblasts,43, 44, 45 while the mesenchymal transition of pericytes or endothelial cells generate a minor contribution to the collagen-producing cells after injury.46, 47, 48 Hence, interstitial fibrosis supports survival of the renal parenchyma and healing process but also stiffens the tissue, which is called 'sclerosis'.49 Insufficient mesenchymal healing destabilizes tissues during reconstitution, whereas overshooting mesenchymal healing produces lesions, such as keloid in the skin.
WHY DANGER CONTROL PROGRAMS CAN TURN INTO PATHOMECHANISMS
The genetic heterogeneity underlying the spectrum of clinical phenotypes usually follows a bell-shaped pattern. Accordingly, within the population certain individuals will respond to injury either with insufficient or exaggerated coagulation, inflammation, re-epithelialization, and scarring, respectively (Figure 1). For example, genetic defects in complement inhibitors lead to exaggerated complement-related renal inflammation driving the renal pathology of atypical hemolytic uremic syndrome (aHUS).50, 51 Although being a genetic disorder, aHUS does not develop without a trigger of an aHUS episode, usually an infection. Physiological complement activation is necessary for pathogen clearance in most people, but in individuals with a complement-inhibitor deficiency the exaggerated complement activation turns the life-saving immune response into a destructive response (mechanism) damaging the kidney. It is likely that most kidney diseases result from various degrees of imbalance in danger control programs (adaptations with multiple effects), whereas, in healthy conditions, these processes operate in a proper manner during the tissue homeostasis. Thus, in patients with kidney pathology, it is necessary to know why these specific programs are altered.
Danger response programs as pathomechanisms of kidney disease. Evolution has developed four adaptive (danger) response programs to survive (traumatic) injuries and infections, ie, clotting, inflammation, and epithelial and mesenchymal healing. In healthy conditions, these operate in an invisible manner during the processes of tissue homeostasis, including epithelial cell turnover or control of the body’s microbiota. Injuries such as a skin laceration activate all four programs to quickly regain homeostasis. However, background genetic variants and environmental influences as well as repetitive or persistent triggers of injury can modulate danger responses and as a by-product cause kidney disease. Patients with kidney pathology experience the effects of one or more imbalances in the danger programs. Examples are given for those kidney diseases in which either insufficient or exaggerated danger responses predominate. It is important to understand the reasons why the specific program is dysregulated. Furthermore, before trying to modulate it, it is important to clarify if a certain dysregulated program is upstream or downstream of nephron loss. For example, if renal scarring is secondary to insufficient epithelial healing, it may be more important to improve epithelial healing rather than blocking fibrosis to protect avoid further nephron loss.
Monogenetic disorders may represent the far end of the spectrum, where one genetic defect activates multiple adaptation responses. This implies that in the future our standard renal pathology evaluation should be supplemented with genetic analysis and perhaps algorithms of risk profiles derived from sequencing results for personalized treatment strategies.
The Two Sides of the Coin—Coagulation
Exaggerated clotting as a predominant pathomechanism
Overshooting coagulation is the central pathogenic mechanism of thrombotic microangiopathies. Triggered by an abnormal insult to microvascular endothelial cells, activation of platelets and released plasma coagulation factors can lead to diffuse coagulation in the renal microvasculature.52 As a result, thrombotic microangiopathies cause renal ischemia and necrosis. In contrast, in crescentic glomerulonephritis, glomerular basement membrane (GBM) rupture, leads to plasma leakage, vascular necrosis, and hematuria.53 Such glomerular vascular injuries activate clotting inside glomerular capillaries, which becomes evident by fibrin deposition in capillary loops.54 The link between clotting and inflammation is also named immunothrombosis.16, 55 In addition, in Alport nephropathy progressive GBM disintegration is associated with hematuria, fibrinogen conversion to fibrin, and plasma leakage into Bowman's space.40 During this process, activated platelets release pro-inflammatory and mitogenic factors with numerous effects on glomerular pathology.
Insufficient clotting in kidney disease
Persistent bleeding indicates an insufficient vascular healing by coagulation. Many glomerular diseases are associated with persistent microhematuria, ie, persistent bleeding. Capillary wall injury in few glomeruli can produce hematuria.56, 57 It remains uncertain if persistent hematuria always originates from vascular lesions of the same glomeruli that do not heal or whether clots stop bleeding in some glomeruli, whereas others start to bleed with persistent hematuria as a net effect. IgA nephropathy as well as other renal disorders present with episodes of intermittent macrohematuria that can last several days, suggesting insufficient clotting.58 One reason for this tendency of persistent bleeding can be the fibrinolytic activity of urokinase expression in the urinary tract.59
The Two Sides of the Coin—Inflammation
Exaggerated inflammation as a predominant pathomechanism
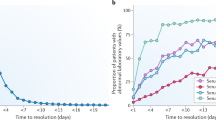
Inflammation as a major strategy of host defense often turns into the predominant pathomechanism of host defense; especially in sterile settings the downside of inflammation outweighs its minimal benefits for the host. Sterile inflammation is very common in kidney disease, eg, in autoimmune glomerulonephritis, alloimmunity of the renal transplant, renal cell necrosis, interstitial nephritis, and during tissue remodeling in progressive CKD (Figure 2a). Mononuclear phagocytes, both resident and infiltrating, express all sorts of innate pattern-recognition receptors in the kidney that translate pathogen- and cell death-related danger signals into a rapid inflammatory response.60 Mesangial cells, endothelial cells, podocytes, tubular cells, and fibroblasts express a limited number of pattern-recognition receptors and, hence, produce fewer amounts of pro-inflammatory cytokines.61 For example, renal parenchymal cells do not express TLR7 and TLR9 and, therefore, do not participate to the same extent to the immune recognition of immunostimulatory nucleic acids.62 Renal cells produce only little IL-1beta upon activation of the NLRP3 inflammasome.63, 64, 65, 66
Inflammation as a pathomechanism of kidney disease. (a) Interstitial nephritis is often a sterile form of renal inflammation involving large numbers of eosinophils (black arrow) within mixed leukocyte cell infiltrates in the interstitium. Hematoxylin–eosin staining × 400. (b) Inflammation is an important mechanism of host defense during bacterial pyelonephritis. Neutrophils attack uropathogenic bacteria ascending from the urinary tract, which results in tubular white cell casts (black arrow) but also in diffuse infiltrates in the interstitium. Hematoxylin–eosin × 100.
During sterile renal inflammation, renal cell necrosis releases endogenous ligands to pattern-recognition receptors. For example, tubular cell necrosis releases high-mobility group box 1 protein, an agonist to TLR2 and TLR4 and driver of inflammation during AKI.67, 68, 69 Tamm–Horsfall protein/uromodulin is exclusively expressed within the distal tubule and activates interstitial dendritic cells via TLR4 and NLRP3 whenever tubular injury promotes its leakage into the renal interstitium.70 Toll-like receptors and inflammasome-mediated immune recognition of necrotic cell death is a central element of rapidly progressive glomerulonephritis (RPGN), thrombotic microangiopathies, and acute tubular necrosis (ATN) as the release of TNF-alpha induces further cell necrosis, eg, necroptosis.71 Necroptosis is a caspase-independent form of cell death, highly immunogenic, that causes plasma membrane rupture and requires receptor-interacting serine-threonine kinase 3-mediated phosphorylation of the mixed lineage kinase domain-like pseudokinase. This auto-amplification loop of necrosis-related inflammation and inflammation-related necrosis was recently named 'Necroinflammation'.72 The molecular mechanisms of renal necroinflammation need to be counterbalanced to avoid widespread renal necrosis. Several molecules inhibit TLR signaling in renal immune and non-immune cells and thereby limit immune-mediated kidney diseases.73, 74, 75 Extracellular histones are another central element of necroinflammation.76 Histones are released into the extracellular space during cell necrosis where they elicit cytotoxic effects on other cells by direct charge-mediated plasma membrane disruption.77 As such, renal cell necrosis induces further histone-mediated necroinflammation.78, 79 Neutrophils undergoing NETosis are an important source of extracellular histones killing endothelial cells, eg, in septic ATN or in crescentic glomerulonephritis.80
Extrarenal infections often trigger flares of chronic glomerulonephritis or renal vasculitis but how? Circulating bacterial or viral products ligate pattern-recognition receptors in intrarenal dendritic cells and macrophages, a process triggering intrarenal production of cytokines, type I interferons that increase local inflammation and tissue damage. This process can set off renal cell loss or death, especially of podocytes.81, 82 A similar mechanism take places in lupus nephritis where the release of hypomethylated DNA or small nuclear RNA by pathogens activate dendritic cells, macrophages, and B cells.83, 84, 85 Especially the release of interferon-alpha sets off a coordinated 'pseudoantiviral' immune response, which explains why clinical manifestations of viral infections and systemic lupus are so similar.86 Also, mesangial cells and glomerular endothelial cells recognize nucleic acids and secrete type I interferons, which promotes podocyte loss and promotes glomerular scarring, eg, during viral glomerulonephritis.87, 88, 89
Intrarenal chemokine expression facilitates the sequential recruitment of various subsets of leukocytes. Thus the local microenvironment determines the functional differentiation of macrophages, T cells, and B cells into functionally distinct subsets that enforce and modulate the ongoing danger control programs.90, 91 As mentioned before, PAMPs and DAMPs turn non-activated intrarenal immune cells into effector phenotypes that confer tissue damage, eg, bacterial products induce neutrophils to undergo NETosis92 or macrophages into the M1 pro-inflammatory phenotype.93 Blocking the CC-chemokine CCL2 or its receptor CCR2 prevents the recruitment and expansion of such classically activated macrophages and thereby reduces renal immunopathology in glomeruli and the tubulointerstitium.94, 95, 96
Together, PAMPs and necrosis-related DAMPs activate renal cells to produce cytokines that drive inflammation and further regulate necrosis. Extracellular histones drive both inflammation and necrosis and leads to an auto-amplification loop of necroinflammation that largely contributes to AKI, eg, in necrotizing glomerulonephritis or ATN. Persistent renal inflammation is driven by adaptive immunity, eg, in autoimmune diseases or renal transplantation. The result is irreversible nephron loss as the central component of long-term outcomes after AKI. Therefore, suppressing renal necroinflammation is as an important therapeutic strategy to prevent nephron loss.
Insufficient inflammation in the kidney
At first, TLR-mediated renal inflammation is important for host defense during renal infection. Immune activation is absolutely necessary to suppress BK virus replication and infection in kidney allografts.97, 98 The same applies to the control of Escherichia coli and other uropathogenic bacteria during bacterial pyelonephritis99 (Figure 2b). Inflammation-mediated pathogen killing limits pathogen spreading to systemic infection, as it happens in TLR4-mutant mice. However, host defense implies collateral tissue injury such as renal abscess formation and scarring, which is absent in TLR4-mutant mice with impaired host defense.100 This inherent impaired innate immunity protects from immune-mediated kidney injury at the expense of insufficient pathogen control at the entry site and the associated risk of fatal Gram-negative sepsis. Along the same line, TLR2 recognizes leptospiral outer membrane proteins in proximal tubular epithelial cells with similar implication for leptospirosis.101
Together, evolution found a balance between the risks of overacting and insufficient inflammation as an essential danger response program. However, for some individuals either too much inflammation or insufficient inflammation becomes the predominant pathomechanism of their kidney disease.
The Two Sides of the Coin—Re-Epithelialization
Although developmentally derived from the mesenchyme, the kidneys are epithelial organs because renal functions entirely depend on the epithelial cell monolayer that covers the nephron from the glomerular tuft to the nephron segment connecting to the ureteric bud-derived collecting duct. Epithelial injuries require re-epithelialization, a process that is supported by surviving epithelial cells via cell division (proliferation=regeneration) or increasing of cell size without cell division (hypertrophy=reconstitution). Although not formally proven by lineage-tracing clonal analysis, it is widely assumed that functional recovery after ATN is associated with sufficient tubular epithelial cell regeneration.102, 103 Growth factors such as platelet-derived growth factor, EGF, HGF, and bone morphogenetic proteins induce re-epithelialization of injured epithelial monolayers.104, 105 The cell cycle regulator murine double minute-2 supports cell cycle entry of surviving tubular cells by inhibiting p53-dependent cell cycle arrest.106 Re-epithelialization requires first the resolution of inflammation because many effector elements of inflammation interfere with epithelial healing.107 The phenotype switch from 'pro-inflammatory' (M1) to 'wound healing' (M2) macrophages is important in this process. M2 macrophage-related CSF-1 secretion drives local M2 macrophage proliferation in an autocrine manner.108, 109, 110 However, a tight regulation of re-epithelialization is mandatory because overshooting as well as insufficient epithelial healing can cause disease.
Exaggerated epithelial healing as a predominant pathomechanism
When those cells with intrinsic regenerative capacity receive mitotic signals but lack those for epithelial cell differentiation, the process of regeneration can turn into a maladaptive pathomechanism and create additional renal pathology. For example, in RPGN, renal progenitors within the parietal epithelial cell (PEC) layer do no longer differentiate into podocytes but their massive hyperplasia creates cellular crescents that obstruct the Bowman's space111, 112 (Figure 3a). Crescent formation does not absolutely require inflammation because plasma leakage from injured capillaries is sufficient to drive epithelial hyperplasia, conceptually similar to the mitogenic effect of serum supplements on cultured epithelial cells in vitro.40 Indeed, in vivo glomerular epithelial cells are never exposed to serum apart from vascular injury.
Exaggerated and insufficient epithelial healing in the glomerulus. (a) Podocytes are postmitotic cells that remain with us for life. Podocyte loss can lead to massive proteinuria, hence, the denudated GBM needs to be covered in either of the three ways: (1) hypertrophy of neighboring podocytes, (2) podocyte regeneration or (3) sealing of the ‘wound’ by a scar. Not infrequently, podocyte hypertrophy and regeneration are not sufficient to fully re-epithelialize the outer aspect of the glomerular capillaries; hence, focal scarring stabilizes and partially seals the defect (arrow). However, the altered hemodynamics and the associated stress on the remaining podocytes can turn insufficient epithelial healing into a pathomechanism for FSGS. PAS × 400. (b) Sometimes, podocyte loss occurs together with rupture of glomerular capillaries, eg, in crescentic glomerulonephritis. Plasma leakage is a very strong mitogenic stimulus for parietal epithelial cells, causing parietal epithelial cell hyperplasia, ie, crescent formation. Because this process destroys the glomerulus, epithelial healing becomes a pathomechanism for small vessel vasculitis. Silver staining × 400.
Insufficient epithelial regeneration as the predominant pathomechanism
Insufficient re-epithelialization of lost glomerular podocytes is the predominant cause for CKD, its progression to end-stage kidney disease, and the spontaneous glomerulosclerosis in the aging kidney.113 The central role of podocyte loss in the pathogenesis of CKD relates to the inability of differentiated podocytes to complete mitosis for repair. Podocytes use all their cytoskeleton to maintain the secondary foot processes and the slit diaphragm along the glomerular filtration barrier, while mitosis would require simplifying cell shape and reorganizing the cytoskeleton to form the mitotic spindle. Thus podocyte loss can only be compensated by hypertrophy of surviving podocytes or by generation of de novo podocytes from podocyte progenitor cells.114 For hypertrophy, podocytes enter the S phase of the cell cycle, and cell cycle restriction points assure that they do not pass into mitosis. In case these restriction points are bypassed, podocytes detach and die, a process referred to as mitotic catastrophe.115, 116 The hypertrophy of surviving podocytes seems able to compensate a loss of up to 20–30% of podocytes; higher loss results in FSGS.117 The emergence of de novo podocytes was clearly demonstrated by lineage tracing using the podocyte-specific tomato-GFP reporter.118 However, the source of new podocytes remains under debate. Some studies suggest that bone marrow-derived progenitor cells are able to replace lost podocytes,119, 120, 121 while others propose that podocytes originate from local podocyte progenitor cells within the PECs.122, 123 Podocyte progenitors surely contribute to renal development and podocyte expansion during kidney growth in childhood but their capacity to replace lost podocytes in the adult kidney is limited. Notch and Wnt signaling, EGF, and SDF-1/CXCL12 regulate the behavior of PECs in glomerular injury.124, 125 Histone H3K9, H3K23 (acetylation), H3K4 (dimethylation), and H3K4 phosphorylation at serine 10 are associated with incomplete podocyte recovery and glomerulosclerosis.126, 127
Insufficient re-epithelialization in the tubule results in tubular atrophy. Repetitive or persistent triggers of tubule injury together with persisting classically activated macrophages impair tubular re-epithelialization after ATN. Tubular cell-derived CSF-1 enforces the local expansion of macrophages inside the kidney after injury but also drives re-epithelialization of tubuli.128 In addition, severe tubular necrosis may also eradicate tubular progenitor cells that are scattered along the tubule and that are more resistant to cell death.129 The idea that bone marrow stem cell invade the injured tubule to replace tubular cells by differentiation was experimentally excluded, but such cells still may provide paracrine support from outside the regenerating tubule.130, 131 Inability to reform the tubular epithelial monolayer leads to tubular atrophy and finally loss of the entire nephron (Figure 3b).
Together, both insufficient and exaggerated epithelial healing contributes to kidney disease. Identifying the predominant pathomechanism in individual patients and identifying specific drugs to correct the abnormal response remains a challenge.
The Two Sides of the Coin—Fibrosis/Sclerosis
Mesenchymal structures stabilize the functional units of the kidney. Mesangial cells stabilize the glomerular tuft of capillaries that confer the filtration process. Interstitial fibroblasts stabilize the tubular part of the nephron by producing interstitial matrix. In addition, mesenchymal pericytes contribute to vascular reconstruction upon injury, a process involving TIMP3 and ADAMTS1.132 Injury to the nephron or the microvasculature activates these mesenchymal elements to proliferate and produce more matrix to enforce tissue stabilization and to support the scaffold for parenchymal regeneration.1 Once parenchymal elements get irreversibly lost during the injury process, mesenchymal elements fill the space with extracellular matrix, eg, Kimmelstiel–Wilson nodules upon diabetic mesangiolysis or interstitial fibrosis upon tubular atrophy (Figure 4a).133 However, fibrosis implies stiffness (sclerosis), which may affect physiological dynamics, eg, in the glomerular tuft.134, 135
Insufficient epithelial regeneration drives renal scarring, which may or may not be a pathomechanism. (a) When parietal epithelial cells in a cellular crescent undergo epithelial–mesenchymal transition, they lose their epithelial polarity and start to produce extracellular matrix around themselves, similar to mesenchymal cells, such as mesangial cells, fibroblasts, or smooth muscle cells. This creates honeycomb-like lesions in Bowman's space, which are irreversible and lead to nephron loss. Masson Trichrome staining × 400. (b) CKD is often associated with more or less confluent interstitial fibrosis together with tubular atrophy. Trichrome × 25. What is the cause and what is the effect in this association is debated. Following activation of the fibrosis danger control program mainly stabilizes the remaining nephrons and fills the spaces left behind by degenerated nephrons. This process is associated with tissue stiffness (sclerosis). An individual’s genetic background may certainly exaggerate fibrogenesis in rare cases, thus turning mesenchymal healing into a pathomechanism contributing to tubular injury. The relevance of such an exaggerated fibrosis for the progression of most CKD cases remains questionable.
Exaggerated mesenchymal healing as a predominant pathomechanism
Mesangial regeneration upon injury can originate from several sources: surviving mesangial cells, from renin-producing cells of the extraglomerular mesangial, and from the bone marrow.136, 137, 138, 139, 140 Mesangial repair upon mesangiolysis is often studied using the rat anti-Thy1.1 model. Mesangial hyperplasia is a hallmark of so-called 'mesangioproliferative' and 'membranoproliferative glomerulonephritis', a consequence of mesangial injury in the first place.141 The stabilizing function of scars is also obvious upon insufficient podocyte regeneration. When lost podocytes cannot be replaced by PECs, focal adhesions to the Bowman’s capsule are formed. Subsequently, PECs migrate onto the glomerular tuft and lay down extracellular matrix, leading to segmental sclerosis, ie, FSGS.142 This implies that PECs not only contribute to epithelial but also to mesenchymal repair.143 Adhesions between glomerular capillaries and the Bowman’s capsule stabilize the rest of the glomerular tuft and minimize protein loss across the denudated GBM.144 However, the dynamics of hyperfiltration-related additional stress on the remaining podocytes can foster further podocyte loss and drive the progression to global glomerulosclerosis.
The extent of interstitial fibrosis correlates well with poor outcomes of primary glomerular disorders (Figure 4b). Somehow this association has led to the assumption that fibrosis could drive nephron loss and CKD progression, instead of simply being a marker of preceding nephron loss.145 There is little evidence on primary fibrotic diseases of the kidney, scleroderma does not present with renal fibrosis, and even genome-wide association studies on CKD populations did not identify risk genes pointing toward fibrogenesis.146 Nevertheless, renal fibrosis is a common finding, a process most likely driven primarily by a lack of rapid and sufficient epithelial healing, for example, tubular epithelial cells unable to regenerate get arrested in the G2/M phase and produce tumor growth factor-beta as it occurs in Chinese herb nephropathy.42 Bone marrow progenitor cells and leukocytes contribute to mesenchymal healing of the kidney as evidenced by interventions that inhibit leukocyte recruitment that can prevent directly or indirectly renal fibrogenesis.147, 148, 149, 150, 151, 152 More specifically, inhibition, deletion, or depletion of alternatively activated macrophages reduces renal fibrogenesis.153, 154, 155, 156 Ly6G+ collagen-producing 'fibrocytes' from the bone marrow invade the kidney via CCL21–CCR7 and contribute to local collagen secretion.157, 158 Also pericytes produce collagen and contribute to renal interstitial fibrosis and sclerosis.159
Insufficient mesenchymal repair in the kidney
A lack of sufficient scarring is poorly defined in renal pathology. Any form of mesangiolysis on a renal biopsy implicates an insufficient regeneration from mesangial cell progenitor cells in the extracellular mesangium.160 Persistent injury to mesangial cells and mesangial cell progenitors can be induced by massive local complement activity, eg, in atypical hemolytic uremic syndrome, immune complex glomerulonephritis, or C3 glomerulopathy.161 Also, diabetes is known to limit progenitor-driven mesangial healing. Indeed, Kimmelstiel–Wilson nodules in diabetic nephropathy are thought to result from focal mesangiolysis and secondary nodular matrix deposition.162
Together, mesenchymal repair is needed to stabilize and rebuild tissues after injury, especially after loss of parenchymal tissue. By contrast, insufficient scarring is rarely a problem in the kidney. Although being a popular concept, there is little evidence that renal fibrogenesis is really a pathogenic mechanism in the progression of CKD.163, 164, 165 Most of the quoted evidence does either not specifically target fibrogenesis (but rather inflammation or re-epithelialization) or does not report renal function as outcome parameter. It is likely that in some patients gene variants lead to overactive fibrogenesis, which could have the potential to CKD progression,166, 167 but until proven otherwise the presence of renal fibrosis in most CKD patients does not necessarily indicate it to be upstream of nephron loss.
SUMMARY AND PERSPECTIVE
Renal pathology is a cumulative expression of renal injury displaying the body's response to injury, especially in CKD. Intrinsic danger responses can be dissected into four distinct programs, ie, healing through coagulation, inflammation, re-epithelialization, and mesenchymal healing. These are all evolutionarily conserved for life-saving benefits upon traumatic injury. Each disease involves one or several of these responses to a different extent depending on the trigger mechanism. Genetic variants impairing or exaggerating these responses programs contribute to the heterogeneity of disease presentations and the predominant pathomechanism and histopathological lesion. Understanding the evolution and origin of histopathological lesions can help to avoid misconceptions in nephrology, eg, the idea that fibrosis may drive the progression of CKD, while it is nothing more than a secondary consequence of insufficient tubular regeneration and nephron loss in most patients. This concept can help to focus our research activities on how to prevent nephron loss. However, a number of questions remain and deserve further study (Table 1). Identifying the predominant pathomechanism in individual patients and identifying specific drugs to correct the abnormal tissue response remains a challenge for the future.
References
Gurtner GC, Werner S, Barrandon Y et al. Wound repair and regeneration. Nature 2008;453:314–321.
Velnar T, Bailey T, Smrkolj V . The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res 2009;37:1528–1542.
Smith SA, Travers RJ, Morrissey JH . How it all starts: initiation of the clotting cascade. Crit Rev Biochem Mol Biol 2015;28:1–11.
Jennewein C, Paulus P, Zacharowski K . Linking inflammation and coagulation: novel drug targets to treat organ ischemia. Curr Opin Anaesthesiol 2011;24:375–380.
Damman J, Bloks VW, Daha MR et al. Hypoxia and complement-and-coagulation pathways in the deceased organ donor as the major target for intervention to improve renal allograft outcome. Transplantation 2015;99:1293–1300.
Buchmann K . Evolution of innate immunity: clues from invertebrates via fish to mammals. Front Immunol 2014;5:459.
Medzhitov R . Origin and physiological roles of inflammation. Nature 2008;454:428–435.
Hickey MJ, Kubes P . Intravascular immunity: the host-pathogen encounter in blood vessels. Nat Rev Immunol 2009;9:364–375.
Anders HJ . Toll-like receptors and danger signaling in kidney injury. J Am Soc Nephrol 2010;21:1270–1274.
Leventhal JS, Schröppel B . Toll-like receptors in transplantation: sensing and reacting to injury. Kidney Int 2012;81:826–832.
Chan JK, Roth J, Oppenheim JJ et al. Alarmins: awaiting a clinical response. J Clin Invest 2012;122:2711–2719.
Kaczmarek A, Vandenabeele P, Krysko DV . Necroptosis: the release of damage-associated molecular patterns and its physiological relevance. Immunity 2013;38:209–223.
McCarthy CG, Goulopoulou S, Wenceslau CF et al. Toll-like receptors and damage-associated molecular patterns: novel links between inflammation and hypertension. Am J Physiol Heart Circ Physiol 2014;306:H184–H196.
Niessen F, Schaffner F, Furlan-Freguia C et al. Dendritic cell PAR1-S1P3 signalling couples coagulation and inflammation. Nature 2008;452:654–658.
Delvaeye M, Conway EM . Coagulation and innate immune responses: can we view them separately? Blood 2009;114:2367–2374.
Engelmann B, Massberg S . Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol 2013;13:34–45.
Wu Y . Contact pathway of coagulation and inflammation. Thromb J 2015;13:17.
Palabrica T, Lobb R, Furie BC et al. Leukocyte accumulation promoting fibrin deposition is mediated in vivo by P-selectin on adherent platelets. Nature 1992;359:848–851.
Semple JW, Italiano JE, Freedman J . Platelets and the immune continuum. Nat Rev Immunol 2011;11:264–274.
Martinod K, Wagner DD . Thrombosis: tangled up in NETs. Blood 2014;123:2768–2776.
Ahronowitz I, Harp J, Shinkai K . Etiology and management of pyoderma gangrenosum: a comprehensive review. Am J Clin Dermatol 2012;13:191–211.
Hotchkiss RS, Coopersmith CM, McDunn JE et al. The sepsis seesaw: tilting toward immunosuppression. Nat Med 2009;15:496–497.
Plikus MV, Gay DL, Treffeisen E et al. Epithelial stem cells and implications for wound repair. Semin Cell Dev Biol 2012;23:946–953.
Sun BK, Siprashvili Z, Khavari PA . Advances in skin grafting and treatment of cutaneous wounds. Science 2014;346:941–945.
Nurden AT . Platelets, inflammation and tissue regeneration. Thromb Haemos 2011;105:S13–S33.
Braun RK, Ferrick C, Neubauer P et al. IL-17 producing gammadelta T cells are required for a controlled inflammatory response after bleomycin-induced lung injury. Inflammation 2008;31:167–179.
Ishida Y, Gao JL, Murphy PM . Chemokine receptor CX3CR1 mediates skin wound healing by promoting macrophage and fibroblast accumulation and function. J Immunol 2008;180:569–579.
Pickert G, Neufert C, Leppkes M et al. STAT3 links IL-22 signaling in intestinal epithelial cells to mucosal wound healing. J Exp Med. 2009;206:1465–1472.
Ebihara N, Matsuda A, Nakamura S et al. Role of the IL-6 classic- and trans-signaling pathways in corneal sterile inflammation and wound healing. Invest Ophthalmol Vis Sci 2011;52:8549–8557.
Kroeze KL, Boink MA, Sampat-Sardjoepersad SC et al. Autocrine regulation of re-epithelialization after wounding by chemokine receptors CCR1, CCR10, CXCR1, CXCR2, and CXCR3. J Invest Dermatol 2012;132:216–225.
Chen L, Guo S, Ranzer MJ et al. Toll-like receptor 4 has an essential role in early skin wound healing. J Invest Dermatol 2013;133:258–267.
McGee HM, Schmidt BA, Booth CJ et al. IL-22 promotes fibroblast-mediated wound repair in the skin. J Invest Dermatol 2013;133:1321–1329.
Lai WF, Siu PM . MicroRNAs as regulators of cutaneous wound healing. J Biosci 2014;39:519–524.
Rosa A, Ballarino M, Sorrentino A et al. The interplay between the master transcription factor PU.1 and miR-424 regulates human monocyte/macrophage differentiation. Proc Natl Acad Sci USA 2007;104:19849–19854.
Lena AM, Shalom-Feuerstein R, Rivetti di Val Cervo P et al. miR-203 represses 'stemness' by repressing DeltaNp63. Cell Death Differ 2008;15:1187–1195.
Liu G, Friggeri A, Yang Y et al. miR-147, a microRNA that is induced upon Toll-like receptor stimulation, regulates murine macrophage inflammatory responses. Proc Natl Acad Sci USA 2009;106:15819–15824.
Wang T, Feng Y, Sun H et al. miR-21 regulates skin wound healing by targeting multiple aspects of the healing process. Am J Pathol 2012;181:1911–1920.
Sallustio F, Costantino V, Cox SN et al. Human renal stem/progenitor cells repair tubular epithelial cell injury through TLR2-driven inhibin-A and microvesicle-shuttled decorin. Kidney Int 2013;83:392–403.
Vaughan AE, Brumwell AN, Xi Y et al. Lineage-negative progenitors mobilize to regenerate lung epithelium after major injury. Nature 2015;517:621–625.
Ryu M, Migliorini A, Miosge N et al. Plasma leakage through glomerular basement membrane ruptures triggers the proliferation of parietal epithelial cells and crescent formation in non-inflammatory glomerular injury. J Pathol 2012;228:482–494.
Wynn TA . Common and unique mechanisms regulate fibrosis in various fibroproliferative diseases. J Clin Invest 2007;117:524–529.
Yang L, Besschetnova TY, Brooks CR et al. Epithelial cell cycle arrest in G2/M mediates kidney fibrosis after injury. Nat Med 2010;16:535–543.
Niedermeier M, Reich B, Rodriguez Gomez M et al. CD4+ T cells control the differentiation of Gr1+ monocytes into fibrocytes. Proc Natl Acad Sci USA 2009;106:17892–17897.
Chen G, Lin SC, Chen J et al. CXCL16 recruits bone marrow-derived fibroblast precursors in renal fibrosis. J Am Soc Nephrol 2011;22:1876–1886.
Xia Y, Yan J, Jin X et al. The chemokine receptor CXCR6 contributes to recruitment of bone marrow-derived fibroblast precursors in renal fibrosis. Kidney Int 2014;86:327–337.
Humphreys BD, Lin SL, Kobayashi A et al. Fate tracing reveals the pericyte and not epithelial origin of myofibroblasts in kidney fibrosis. Am J Pathol 2010;176:85–97.
LeBleu VS, Taduri G, O'Connell J et al. Origin and function of myofibroblasts in kidney fibrosis. Nat Med 2013;19:1047–1053.
Falke LL, Gholizadeh S, Goldschmeding R et al. Diverse origins of the myofibroblast—implications for kidney fibrosis. Nat Rev Nephrol 2015;11:233–244.
Vielhauer V, Kulkarni O, Reichel CA et al. Targeting the recruitment of monocytes and macrophages in renal disease. Semin Nephrol 2010;30:318–333.
Martinez-Barricarte R, Pianetti G, Gautard R et al. The complement factor H R1210C mutation is associated with atypical hemolytic uremic syndrome. J Am Soc Nephrol 2008;19:639–646.
Hofer J, Janecke AR, Zimmerhackl LB et al. Complement factor H-related protein 1 deficiency and factor H antibodies in pediatric patients with atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol 2013;8:407–415.
Chapman K, Seldon M, Richards R . Thrombotic microangiopathies, thrombotic thrombocytopenic purpura, and ADAMTS-13. Semin Thromb Hemost 2012;38:47–54.
Srivastava A, Rao GK, Segal PE et al. Characteristics and outcome of crescentic glomerulonephritis in patients with both antineutrophil cytoplasmic antibody and anti-glomerular basement membrane antibody. Clin Rheumatol 2013;32:1317–1322.
Sorensen I, Susnik N, Inhester T et al. Fibrinogen, acting as a mitogen for tubulointerstitial fibroblasts, promotes renal fibrosis. Kidney Int 2011;80:1035–1044.
Loof TG, Morgelin M, Johansson L et al. Coagulation, an ancestral serine protease cascade, exerts a novel function in early immune defense. Blood 2011;118:2589–2598.
Vivante A, Calderon-Margalit R, Skorecki K . Hematuria and risk for end-stage kidney disease. Curr Opin Nephrol Hypertens 2013;22:325–330.
Yuste C, Rubio-Navarro A, Barraca D et al. Haematuria increases progression of advanced proteinuric kidney disease. PLoS One 2015;10:e0128575.
Gutiérrez E, Egido J, Rubio-Navarro A et al. Oxidative stress, macrophage infiltration and CD163 expression are determinants of long-term renal outcome in macrohematuria-induced acute kidney injury of IgA nephropathy. Nephron Clin Pract 2012;121:c42–c53.
Degen JL, Bugge TH, Goguen JD . Fibrin and fibrinolysis in infection and host defense. J Thromb Haemost 2007;5:24–31.
Nelson PJ, Rees AJ, Griffin MD et al. The renal mononuclear phagocytic system. J Am Soc Nephrol 2012;23:194–203.
Anders HJ, Banas B, Schlondorff D . Signaling danger: Toll-like receptors and their potential roles in kidney disease. J Am Soc Nephrol. 2004;15:854–867.
Anders HJ, Schlondorff D . Toll-like receptors: emerging concepts in kidney disease. Curr Opin Nephrol Hypertens 2007;16:177–183.
Anders HJ, Muruve DA . The inflammasomes in kidney disease. J Am Soc Nephrol 2011;22:1007–1018.
Lichtnekert J, Kulkarni OP, Mulay SR et al. Anti-GBM glomerulonephritis involves IL-1 but is independent of NLRP3/ASC inflammasome-mediated activation of caspase-1. PLoS One 2011;6:e26778.
Abais JM, Xia M, Li G et al. Nod-like receptor protein 3 (NLRP3) inflammasome activation and podocyte injury via thioredoxin-interacting protein (TXNIP) during hyperhomocysteinemia. J Biol Chem 2014;289:27159–27168.
Shahzad K, Bock F, Dong W et al. Nlrp3-inflammasome activation in non-myeloid-derived cells aggravates diabetic nephropathy. Kidney Int 2015;87:74–84.
Wu H, Ma J, Wang P et al. HMGB1 contributes to kidney ischemia reperfusion injury. J Am Soc Nephrol. 2010;21:1878–1890.
Mudaliar H, Pollock C, Komala MG et al. The role of Toll-like receptor proteins (TLR) 2 and 4 in mediating inflammation in proximal tubules. Am J Physiol Renal Physiol 2013;305:F143–F154.
R Nair A, Ebenezer PJ, Saini Y et al. Angiotensin II-induced hypertensive renal inflammation is mediated through HMGB1-TLR4 signaling in rat tubulo-epithelial cells. Exp Cell Res 2015;S0014-4827:00191–00193.
Säemann MD, Weichhart T, Zeyda M et al. Tamm-Horsfall glycoprotein links innate immune cell activation with adaptive immunity via a Toll-like receptor-4-dependent mechanism. J Clin Invest 2005;115:468–475.
Linkermann A, Green DR . Necroptosis. N Engl J Med 2014;370:455–465.
Linkermann A, Stockwell BR, Krautwald S et al. Regulated cell death and inflammation: an auto-amplification loop causes organ failure. Nat Rev Immunol 2014;14:759–767.
Noris M, Cassis P, Azzollini N et al. The Toll-IL-1R member Tir8/SIGIRR negatively regulates adaptive immunity against kidney grafts. J Immunol 2009;183:4249–4260.
Lech M, Avila-Ferrufino A, Allam R et al. Resident dendritic cells prevent postischemic acute renal failure by help of single Ig IL-1 receptor-related protein. J Immunol 2009;183:4109–4118.
Lassen S, Lech M, Rommele C et al. Ischemia reperfusion induces IFN regulatory factor 4 in renal dendritic cells, which suppresses postischemic inflammation and prevents acute renal failure. J Immunol 2010;185:1976–1983.
Allam R, Kumar SV, Darisipudi MN et al. Extracellular histones in tissue injury and inflammation. J Mol Med (Berl) 2014;92:465–472.
Xu J, Zhang X, Pelayo R et al. Extracellular histones are major mediators of death in sepsis. Nat Med 2009;15:1318–1321.
Allam R, Scherbaum CR, Darisipudi MN et al. Histones from dying renal cells aggravate kidney injury via TLR2 and TLR4. J Am Soc Nephrol 2012;23:1375–1388.
Allam R, Darisipudi MN, Tschopp J et al. Histones trigger sterile inflammation by activating the NLRP3 inflammasome. Eur J Immunol 2013;43:3336–3342.
Kumar SV, Kulkarni OP, Mulay SR et al. Neutrophil extracellular trap-related extracellular histones cause vascular necrosis in severe GN. J Am Soc Nephrol 2015;26:2399–2413.
Ryu M, Kulkarni OP, Radomska E et al. Bacterial CpG-DNA accelerates Alport glomerulosclerosis by inducing an M1 macrophage phenotype and tumor necrosis factor-alpha-mediated podocyte loss. Kidney Int 2011;79:189–198.
Brahler S, Ising C, Hagmann H et al. Intrinsic proinflammatory signaling in podocytes contributes to podocyte damage and prolonged proteinuria. Am J Physiol Renal Physiol 2012;303:F1473–F1485.
Leadbetter EA, Rifkin IR, Hohlbaum AM et al. Chromatin-IgG complexes activate B cells by dual engagement of IgM and Toll-like receptors. Nature 2002;416:603–607.
Wen ZK, Xu W, Xu L et al. DNA hypomethylation is crucial for apoptotic DNA to induce systemic lupus erythematosus-like autoimmune disease in SLE-non-susceptible mice. Rheumatology (Oxford) 2007;46:1796–1803.
Villanueva E, Yalavarthi S, Berthier CC et al. Netting neutrophils induce endothelial damage, infiltrate tissues, and expose immunostimulatory molecules in systemic lupus erythematosus. J Immunol 2011;187:538–552.
Migliorini A, Anders HJ . A novel pathogenetic concept-antiviral immunity in lupus nephritis. Nat Rev Nephrol 2012;8:183–189.
Flur K, Allam R, Zecher D et al. Viral RNA induces type I interferon-dependent cytokine release and cell death in mesangial cells via melanoma-differentiation-associated gene-5: implications for viral infection-associated glomerulonephritis. Am J Pathol 2009;175:2014–2022.
Hagele H, Allam R, Pawar RD et al. Double-stranded DNA activates glomerular endothelial cells and enhances albumin permeability via a Toll-like receptor-independent cytosolic DNA recognition pathway. Am J Pathol 2009;175:1896–1904.
Migliorini A, Angelotti ML, Mulay SR et al. The antiviral cytokines IFN-α and IFN-β modulates parietal epithelial cells and promotes podocyte loss: implications for IFN toxicity, viral glomerulonephritis, and glomerular regeneration. Am J Pathol 2013;183:431–440.
Anders HJ, Ryu M . Renal microenvironments and macrophage phenotypes determine progression or resolution of renal inflammation and fibrosis. Kidney Int 2011;80:915–925.
Lech M, Grobmayr R, Weidenbusch M et al. Tissues use resident dendritic cells and macrophages to maintain homeostasis and to regain homeostasis upon tissue injury: the immunoregulatory role of changing tissue environments. Mediators Inflamm 2012;2012:951390.
Brinkmann V, Reichard U, Goosmann C et al. Neutrophil extracellular traps kill bacteria. Science 2004;303:1532–1535.
Anders HJ, Banas B, Linde Y et al. Bacterial CpG-DNA aggravates immune complex glomerulonephritis: Role of TLR9-mediated expression of chemokines and chemokine receptors. J Am Soc Nephrol 2003;14:317–326.
Sayyed SG, Ryu M, Kulkarni OP et al. An orally active chemokine receptor CCR2 antagonist prevents glomerulosclerosis and renal failure in type 2 diabetes. Kidney Int 2011;80:68–78.
Urushihara M, Ohashi N, Miyata K et al. Addition of angiotensin II type 1 receptor blocker to CCR2 antagonist markedly attenuates crescentic glomerulonephritis. Hypertension 2011;57:586–593.
Seok SJ, Lee ES, Kim GT et al. Blockade of CCL2/CCR2 signalling ameliorates diabetic nephropathy in db/db mice. Nephrol Dial Transplant 2013;28:1700–1710.
Babel N, Volk HD, Reinke P . BK polyomavirus infection and nephropathy: the virus-immune system interplay. Nat Rev Nephrol 2011;7:399–406.
Ribeiro A, Wornle M, Motamedi N et al. Activation of innate immune defense mechanisms contributes to polyomavirus BK-associated nephropathy. Kidney Int 2012;81:100–111.
Anders HJ, Patole PS . Toll-like receptors recognize uropathogenic Escherichia coli and trigger inflammation in the urinary tract. Nephrol Dial Transplant 2005;20:1529–1532.
Patole PS, Schubert S, Hildinger K et al. Toll-like receptor-4: renal cells and bone marrow cells signal for neutrophil recruitment during pyelonephritis. Kidney Int 2005;68:2582–2587.
Yang CW, Hung CC, Wu MS et al. Toll-like receptor 2 mediates early inflammation by leptospiral outer membrane proteins in proximal tubule cells. Kidney Int 2006;69:815–822.
Bonventre JV . Dedifferentiation and proliferation of surviving epithelial cells in acute renal failure. J Am Soc Nephrol 2003;14:S55–S61.
Duffield JS, Park KM, Hsiao LL et al. Restoration of tubular epithelial cells during repair of the postischemic kidney occurs independently of bone marrow-derived stem cells. J Clin Invest 2005;115:1743–1755.
Werner S, Grose R . Regulation of wound healing by growth factors and cytokines. Physiol Rev 2003;83:835–870.
Sugimoto H, Lebleu VS, Bosukonda D et al. Activin-like kinase 3 is important for kidney regeneration and reversal of fibrosis. Nat Med 2012;18:396–404.
Mulay SR, Thomasova D, Ryu M et al. MDM2 (murine double minute-2) links inflammation and tubular cell healing during acute kidney injury in mice. Kidney Int 2012;81:1199–1211.
Weidenbusch M, Anders HJ . Tissue microenvironments define and get reinforced by macrophage phenotypes in homeostasis or during inflammation, repair and fibrosis. J Innate Immun 2012;4:463–477.
Duffield JS, Forbes SJ, Constandinou CM et al. Selective depletion of macrophages reveals distinct, opposing roles during liver injury and repair. J Clin Invest 2005;115:56–65.
Alikhan MA, Jones CV, Williams TM et al. Colony-stimulating factor-1 promotes kidney growth and repair via alteration of macrophage responses. Am J Pathol 2011;179:1243–1256.
Iwata Y, Boström EA, Menke J et al. Aberrant macrophages mediate defective kidney repair that triggers nephritis in lupus-susceptible mice. J Immunol. 2012;188:4568–4580.
Smeets B, Angelotti ML, Rizzo P et al. Renal progenitor cells contribute to hyperplastic lesions of podocytopathies and crescentic glomerulonephritis. J Am Soc Nephrol 2009;20:2593–2603.
Bollee G, Flamant M, Schordan S et al. Epidermal growth factor receptor promotes glomerular injury and renal failure in rapidly progressive crescentic glomerulonephritis. Nat. Med 2011;17:1242–1250.
Hodgin JB, Bitzer M, Wickman L et al. Glomerular aging and focal global glomerulosclerosis: a podometric perspective. J Am Soc Nephrol 2015;26:3162–3178.
Lasagni L, Romagnani P . Basic research: podocyte progenitors and ectopic podocytes. Nat Rev Nephrol 2013;9:715–716.
Liapis H, Romagnani P, Anders HJ . New insights into the pathology of podocyte loss: mitotic catastrophe. Am J Pathol 2013;183:1364–1374.
Mulay SR, Thomasova D, Ryu M et al. Podocyte loss involves MDM2-driven mitotic catastrophe. J Pathol 2013;230:322–335.
Fukuda A, Chowdhury MA, Venkatareddy MP et al. Growth-dependent podocyte failure causes glomerulosclerosis. J Am Soc Nephrol 2012;23:1351–1363.
Wanner N, Hartleben B, Herbach N et al. Unraveling the role of podocyte turnover in glomerular aging and injury. J Am Soc Nephrol 2014;25:707–716.
Sugimoto H, Mundel TM, Sund M et al. Bone-marrow-derived stem cells repair basement membrane collagen defects and reverse genetic kidney disease. Proc Natl Acad Sci USA 2006;103:7321–7326.
Prodromidi EI, Poulsom R, Jeffery R et al. Bone marrow-derived cells contribute to podocyte regeneration and amelioration of renal disease in a mouse model of Alport syndrome. Stem Cells 2006;24:2448–2455.
Zoja C, Garcia PB, Rota C et al. Mesenchymal stem cell therapy promotes renal repair by limiting glomerular podocyte and progenitor cell dysfunction in adriamycin-induced nephropathy. Am J Physiol Renal Physiol 2012;303:F1370–F1381.
Lasagni L, Romagnani P . Glomerular epithelial stem cells: the good, the bad, and the ugly. J Am Soc Nephrol 2010;21:1612–1619.
Shankland SJ, Pippin JW, Duffield JS . Progenitor cells and podocyte regeneration. Semin Nephrol 2014;34:418–428.
Lasagni L, Ballerini L, Angelotti ML et al. Notch activation differentially regulates renal progenitors proliferation and differentiation toward the podocyte lineage in glomerular disorders. Stem Cells 2010;28:1674–1685.
Darisipudi MN, Kulkarni OP, Sayyed SG et al. Dual blockade of the homeostatic chemokine CXCL12 and the proinflammatory chemokine CCL2 has additive protective effects on diabetic kidney disease. Am J Pathol 2011;179:116–124.
Gaikwad AB, Sayyed SG, Lichtnekert J et al. Renal failure increases cardiac histone h3 acetylation, dimethylation, and phosphorylation and the induction of cardiomyopathy-related genes in type 2 diabetes. Am J Pathol 2010;176:1079–1083.
Sayyed SG, Gaikwad AB, Lichtnekert J et al. Progressive glomerulosclerosis in type 2 diabetes is associated with renal histone H3K9 and H3K23 acetylation, H3K4 dimethylation and phosphorylation at serine 10. Nephrol Dial Transplant 2010;25:1811–1817.
Menke J, Iwata Y, Rabacal WA et al. CSF-1 signals directly to renal tubular epithelial cells to mediate repair in mice. J Clin Invest 2009;119:2330–2342.
Angelotti ML, Ronconi E, Ballerini L et al. Characterization of renal progenitors committed toward tubular lineage and their regenerative potential in renal tubular injury. Stem Cells 2012;30:1714–1725.
Humphreys BD, Czerniak S, DiRocco DP et al. Repair of injured proximal tubule does not involve specialized progenitors. Proc Natl Acad Sci USA 2011;108:9226–9231.
Romagnani P . Family portrait: renal progenitor of Bowman’s capsule and its tubular brothers. Am J Pathol 2011;178:490–493.
Schrimpf C, Xin C, Campanholle G et al. Pericyte TIMP3 and ADAMTS1 modulate vascular stability after kidney injury. J Am Soc Nephrol 2012;23:868–883.
Campanholle G, Ligresti G, Gharib SA et al. Cellular mechanisms of tissue fibrosis. 3. Novel mechanisms of kidney fibrosis. Am J Physiol Cell Physiol 2013;304:C591–C603.
Grgic I, Campanholle G, Bijol V et al. Targeted proximal tubule injury triggers interstitial fibrosis and glomerulosclerosis. Kidney Int 2012;82:172–183.
Zoja C, Abbate M, Remuzzi G . Progression of renal injury toward interstitial inflammation and glomerular sclerosis is dependent on abnormal protein filtration. Nephrol Dial Transplant 2015;30:706–712.
Imasawa T, Utsunomiya Y, Kawamura T et al. The potential of bone marrow-derived cells to differentiate to glomerular mesangial cells. J Am Soc Nephrol 2001;12:1401–1409.
Ikarashi K, Li B, Suwa M et al. Bone marrow cells contribute to regeneration of damaged glomerular endothelial cells. Kidney Int 2005;67:1925–1933.
Daniel C, Albrecht H, Lüdke A et al. Nestin expression in repopulating mesangial cells promotes their proliferation. Lab Invest 2008;88:387–397.
Pippin JW, Sparks MA, Glenn ST et al. Cells of renin lineage are progenitors of podocytes and parietal epithelial cells in experimental glomerular disease. Am J Pathol 2013;183:542–557.
Starke C, Betz H, Hickmann L et al. Renin lineage cells repopulate the glomerular mesangium after injury. J Am Soc Nephrol 2015;26:48–54.
Sethi S, Fervenza FC . Membranoproliferative glomerulonephritis—a new look at an old entity. N Engl J Med 2012;366:1119–1131.
Smeets B, Kuppe C, Sicking EM et al. Parietal epithelial cells participate in the formation of sclerotic lesions in focal segmental glomerulosclerosis. J Am Soc Nephrol 2011;22:1262–1274.
Shankland SJ, Anders HJ, Romagnani P . Glomerular parietal epithelial cells in kidney physiology, pathology, and repair. Curr Opin Nephrol Hypertens 2013;22:302–309.
D'Agati VD, Kaskel FJ, Falk RJ . Focal segmental glomerulosclerosis. N Engl J Med 2011;365:2398–2411.
Zeisberg M, Neilson EG . Mechanisms of tubulointerstitial fibrosis. J Am Soc Nephrol 2010;21:1819–1834.
Böger CA, Gorski M, Li M et al. Association of eGFR-related loci identified by GWAS with incident CKD and ESRD. PLoS Genet 2011;7:e1002292.
Anders HJ, Vielhauer V, Schlondorff D . Chemokines and chemokine receptors are involved in the resolution or progression of renal disease. Kidney Int 2003;63:401–415.
Vielhauer V, Berning E, Eis V et al. CCR1 blockade reduces interstitial inflammation and fibrosis in mice with glomerulosclerosis and nephrotic syndrome. Kidney Int 2004;66:2264–2278.
Anders HJ, Ninichuk V, Schlondorff D . Progression of kidney disease: blocking leukocyte recruitment with chemokine receptor CCR1 antagonists. Kidney Int 2006;69:29–32.
Furuichi K, Gao JL, Murphy PM . Chemokine receptor CX3CR1 regulates renal interstitial fibrosis after ischemia-reperfusion injury. Am J Pathol 2006;169:372–387.
Clauss S, Gross O, Kulkarni O et al. Ccl2/Mcp-1 blockade reduces glomerular and interstitial macrophages but does not ameliorate renal pathology in collagen4A3-deficient mice with autosomal recessive Alport nephropathy. J Pathol 2009;218:40–47.
Liu L, Kou P, Zeng Q et al. CD4+ T Lymphocytes, especially Th2 cells, contribute to the progress of renal fibrosis. Am J Nephrol 2012;36:386–396.
Lee S, Huen S, Nishio H et al. Distinct macrophage phenotypes contribute to kidney injury and repair. J Am Soc Nephrol 2011;22:317–326.
Braga TT, Correa-Costa M, Guise YF et al. MyD88 signaling pathway is involved in renal fibrosis by favoring a TH2 immune response and activating alternative M2 macrophages. Mol Med 2012;18:1231–1239.
Chen G, Chen H, Wang C et al. Rapamycin ameliorates kidney fibrosis by inhibiting the activation of mTOR signaling in interstitial macrophages and myofibroblasts. PLoS One 2012;7:e33626.
Cao Q, Harris DC, Wang Y . Macrophages in kidney injury, inflammation, and fibrosis. Physiology (Bethesda) 2015;30:183–194.
Sakai N, Wada T, Yokoyama H et al. Secondary lymphoid tissue chemokine (SLC/CCL21)/CCR7 signaling regulates fibrocytes in renal fibrosis. Proc Natl Acad Sci USA 2006;103:14098–14103.
Reich B, Schmidbauer K, Rodriguez Gomez M et al. Fibrocytes develop outside the kidney but contribute to renal fibrosis in a mouse model. Kidney Int 2013;84:78–89.
Kramann R, Humphreys BD . Kidney pericytes: roles in regeneration and fibrosis. Semin Nephrol 2014;34:374–383.
Migliorini A, Ebid R, Scherbaum CR et al. The danger control concept in kidney disease: mesangial cells. J Nephrol 2013;26:437–449.
Bomback AS, Appel GB . Pathogenesis of the C3 glomerulopathies and reclassification of MPGN. Nat Rev Nephrol 2012;8:634–642.
Stout LC, Kumar S, Whorton EB . Focal mesangiolysis and the pathogenesis of the Kimmelstiel-Wilson nodule. Hum Pathol 1993;24:77–89.
Ninichuk V, Gross O, Segerer S et al. Multipotent mesenchymal stem cells reduce interstitial fibrosis but do not delay progression of chronic kidney disease in collagen4A3-deficient mice. Kidney Int 2006;70:121–129.
Kaissling B, Lehir M, Kriz W . Renal epithelial injury and fibrosis. Biochim Biophys Acta 2013;1832:931–939.
Venkatachalam MA, Weinberg JM, Kriz W et al. Failed tubule recovery, AKI-CKD transition, and kidney disease progression. J Am Soc Nephrol 2015;26:1765–1776.
Jia Z, Johnson AC, Wang X et al. Allelic variants in Arhgef11 via the Rho-Rock pathway are linked to epithelial-mesenchymal transition and contributes to kidney injury in the Dahl salt-sensitive rat. PLoS One 2015;10:e0132553.
Chen Y, Rao F, Wen G et al. Naturally occurring genetic variants in human chromogranin A (CHGA) associated with hypertension as well as hypertensive renal disease. Cell Mol Neurobiol 2010;30:1395–1400.
Acknowledgements
H-JA is supported by the Deutsche Forschungsgemeinschaft (AN372/11-2 and AN372/17-1). BS-A is supported by a Sara-Borrell contract from Spanish Government, Institute of Health Carlos III, ISCIII.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Renal pathology is characterized by a mix of intrinsic injurious pathological mechanisms. In this review, the authors focus on the four major danger response programs: coagulation, inflammation, re-epithelialization and mesenchymal repair; and explain how each one contributes to the heterogeneity of kidney diseases. The characterization of these mechanisms will allow modulation of kidney diseases for better patient outcomes.
Rights and permissions
About this article
Cite this article
Suárez-Álvarez, B., Liapis, H. & Anders, HJ. Links between coagulation, inflammation, regeneration, and fibrosis in kidney pathology. Lab Invest 96, 378–390 (2016). https://doi.org/10.1038/labinvest.2015.164
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2015.164
This article is cited by
-
Coagulation parameters are associated with the prognosis of immunoglobulin a nephropathy: a retrospective study
BMC Nephrology (2020)
-
Novel plasma peptide markers involved in the pathology of CKD identified using mass spectrometric approach
Journal of Molecular Medicine (2019)
-
Recent advances in the pathogenetic mechanisms of sepsis-associated acute kidney injury
Journal of Nephrology (2018)