Abstract
Objective:
An important area concerning morbidity among infants with congenital heart defects (CHD) is related to feeding problems. Our objectives were to characterize the evolution of feeding milestones related to transition to per oral feeding among infants with CHD, and to identify associated variables impacting the feeding abilities. Specifically, we differentiated the feeding characteristics in neonates with acyanotic vs cyanotic CHD.
Study Design:
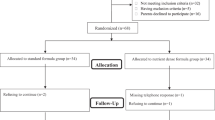
Feeding progress was tracked during the first hospitalization in a retrospective chart review study involving 76 infants (29 acyanotic, 47 cyanotic CHD). The ages at which the following milestones attained were recorded: first feeds, maximum gavage feeds, first nipple feeds and maximum nipple feeds, in addition to the length of hospital stay. Effects of perinatal factors, duration of respiratory support, vasopressor and narcotic use and use of cardiopulmonary bypass on the feeding milestones were also evaluated. ANOVA, t-test, and stepwise linear regression analysis were applied as appropriate. Data stated as mean±s.e.m., or %; P<0.05 was considered significant.
Result:
Prenatal and birth characteristics were similar (P=NS) between the neonates with acyanotic and cyanotic CHD. Cyanotic CHD required three times prolonged use of ventilation, narcotics and vasopressor use (all P<0.05, compared to the acyanotic group). In the acyanotic group, prolonged respiratory support correlated linearly with time to attain maximal gavage feeds and nippling (both, R2=0.8). In the cyanotic group, delayed initiation of gavage feeds and prolonged respiratory support both correlated linearly with time to attain maximal gavage feeds and nippling (both, R2=0.8). Age at first gavage feed correlated with maximum gavage feeds among neonates with cyanotic CHD, and first nipple feed correlated with maximum nipple feeds among all groups (P<0.01). Use of cardiopulmonary bypass in cyanotic CHD delayed the feeding milestones and prolonged the length of stay (both, P<0.05 vs non-bypass group); similar findings were not seen in the acyanotic group.
Conclusion:
In contrast to neonates with acyanotic CHD, cyanotic CHD group had significant delays with (a) feeding readiness, (b) successful gastric feeding, (c) oromotor readiness and (d) successful oromotor skills. Co-morbid factors that may directly influence the delay in feeding milestones include the (a) duration of respiratory support and (b) use of cardiopulmonary bypass. Delays in achieving maximum gavage and maximum nippling may suggest foregut dysmotility and oropharyngeal dysphagia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Varan B, Tokel K, Yilmaz G . Malnutrition and growth failure in cyanotic and acyanotic congenital heart disease with and without pulmonary hypertension. Arch Dis Child 1999; 81: 49–52.
Kliegman RM . Neonatal technology, perinatal survival, social consequences, and the perinatal paradox. Am J of Public Health 1995; 85: 909–913.
Author: American Academy of Pediatrics, Committee on Children with Disabilities. Managed care and children with special health care needs. Pediatrics 1998; 102 (3): 657–660.
American Academy of Pediatrics, Committee on Fetus and Newborn. Hospital discharge of the high risk neonate: proposed guidelines. Pediatrics 1998; 102 (2): 411–417.
Kelleher DK, Laussen P, Teixeira-Pinto A, Duggan C . Growth and correlates of nutritional status among infants with hypoplastic left heart syndrome after stage I Norwood procedure. Nutrition 2006; 22: 237–244.
Sloper P, Turner S . Risk and resistance factors in the adaptation of parents of children with severe physical disability. J Child Psychol Pyschiatry 1993; 34: 167–188.
Sadler TW . Special embryology: Respiratory system and Digestive system. In: Sadler TW (ed). Langman's medical embryology, 7th edn. Williams and Wilkins: Baltimore, MD, 1995, pp 232–271.
Bu'Lock F, Woolridge MW, Bairn JD . Development of coordination of sucking, swallowing, and breathing: ultrasound study of term and preterm infants. Dev Med Child Neurol 1990; 32: 669–678.
Einarson KD, Arthur HM . Predictors of oral feeding difficulty in cardiac surgical infants. Pediatr Nurs 2003; 29: 315–319.
Kogon BE, Ramaswamy V, Todd K, Plattner C, Kirshbom PM, Kanter KR et al. Feeding difficulty in newborns following congenital heart surgery. Congenital Heart Dis 2007; 2: 332–337.
Skinner ML, Halstead LA, Rubinstein CS, Atz AM, Andrews D, Bradley SM . Laryngopharyngeal dysfunction after Norwood procedure. J Thoracic Cardiovasc Surg 2005; 130: 1293–1301.
Armitage P, Berry G . Statistical methods in medical research. Blackwell Scientific Publications: Oxford, 1987.
Snedecor GW, Cochrann WG . Statistical methods, 7th edn. The Iowa State University Press, Ames, Iowa, 1980.
Cameron JW, Rosenthal A, Olson AD . Malnutrition in hospitalized children with congenital heart disease. Arch Pediatr Adolesc Med 1995; 149: 1098–1102.
Jeffries HE, Wells WJ, Starnes VA, Wetzel RC, Moromisato DY . Gastrointestinal morbidity after Norwood palliation for hypoplastic left heart syndrome. Ann Thorac Surg 2006; 81 (3): 982–987.
Glass P, Miller M, Short B . Morbidity for survivors of extra corporeal membrane oxygenation: neurodevelopmental outcome at 1 year of age. Pediatrics 1989; 83: 72–78.
Pillo-Blocka F, Adatia I, Sharieff W, McCrindle BW, Zlotkin S . Rapid advancement to more concentrated formula in infants after surgery for congenital heart disease reduces duration of hospital stay: a randomized clinical trial. J Pediatr 2004; 145: 761–766.
Ohri SK, Somasundaram S, Koak Y, Macpherson A, Keogh BE, Taylor KM et al. The effect of intestinal hypoperfusion on intestinal absorption and permeability during cardiopulmonary bypass. Gastroenterology 1994; 106: 318–323.
Jolley SG, McClelland KK, Mosesso-Ronssaeau M . Pharyngeal and swallowing disorders in infants. Semin Pediatr Surg 1995; 4 (3): 157–165.
Jadcherla SR, Berseth CL . Antroduodenal motility and feeding outcomes among neonatal extra corporeal membrane oxygenation survivors. J Pediatr Gastroenterol Nutr 2005; 41: 347–350.
Sachdeva R, Hussain E, Moss MM, Schmitz ML, Ray RM, Imamura M et al. Vocal cord dysfunction and feeding difficulties after pediatric cardiovascular surgery. J Pediatr 2007; 151: 312–315.
Berseth CL, McCoy HH . Birth asphyxia alters neonatal intestinal motility in term neonates. Pediatrics 1992; 90 (5): 669–673.
Hofner G, Behrens R, Koch A, Singer H, Hofbeck M . Enteral nutritional support by percutaneous endoscopic gastrostomy in children with congenital heart disease. Pediatr Cardiol 2000; 21: 341–346.
Imms C . Feeding the infant with congenital heart disease: an occupational performance challenge. Am J Occup Ther 2001; 55 (3): 277–284.
Hoffman HS, Stratton JW, Newby V . The control of feeding behavior by an imprinted stimulus. J Exp Anal Behav 1969; 12 (6): 847–860.
Barker GR, Bird F, Alexander V, Warburton EC . Recognition memory for objects, place, and temporal order: a disconnection analysis of the role of the medial prefrontal cortex and perirhinal cortex. J Neurosci 2007; 27 (11): 2948–2957.
Jadcherla SR, Gupta A, Stoner E, Fernandez S, Shaker R . Pharyngeal swallowing: defining pharyngeal and upper esophageal sphincter relationships in human neonates. J Pediatr 2007; 151: 597–603.
Jadcherla SR, Hoffmann RG, Shaker R . Effect of maturation on the magnitude of mechanosensitive and chemosensitive reflexes in the premature human esophagus. J Pediatr 2006; 141 (1): 77–82.
Jadcherla SR, Gupta A, Coley BD, Fernandez S, Shaker R . Esophago-glottal closure reflex in human infants: a novel reflex elicited with concurrent manometry and ultrasonography. Am J Gastroenterol 2007; 102: 2286–2293.
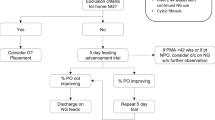
Jadcherla SR, Stoner E, Gupta A, Bates DG, Fernandez S, Di Lorenzo C et al. Evaluation and management of neonatal dysphagia: impact of pharyngo-esophageal motility studies and multidisciplinary feeding strategy. JPGN 2008 (in press).
Acknowledgements
We express our gratitude to Dr Raymond G Hoffmann, PhD, Department of Biostatistics, Medical College of Wisconsin, for advice with the statistical analysis; Dr P Sasidharan, MD, Section of Neonatology, and Dr Stu Berger, MD, Section of Cardiology, in the Department of Pediatrics, Medical College of Wisconsin, for their valuable advice, guidance and support for this initiative. Dr Jadcherla was supported in part by NIH Grant ROI DK 068158.
Author information
Authors and Affiliations
Corresponding author
Additional information
Location of work: Children's Hospital of Wisconsin, Milwaukee, WI 53226, USA.
Rights and permissions
About this article
Cite this article
Jadcherla, S., Vijayapal, A. & Leuthner, S. Feeding abilities in neonates with congenital heart disease: a retrospective study. J Perinatol 29, 112–118 (2009). https://doi.org/10.1038/jp.2008.136
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.136
Keywords
This article is cited by
-
Risk Factors for Tube Feeding at Discharge in Infants Undergoing Neonatal Surgery for Congenital Heart Disease: A Systematic Review
Pediatric Cardiology (2023)
-
Relationship Between Human Milk Feeding Patterns and Growth in the First Year of Life in Infants with Congenital Heart Defects
Pediatric Cardiology (2023)
-
Reliability and validity of the FFQ and feeding index for 7-to 24-month-old children after congenital heart disease surgery
BMC Pediatrics (2022)
-
Surgically Acquired Vocal Cord Palsy in Infants and Children with Congenital Heart Disease (CHD): Description of Feeding Outcomes
Dysphagia (2022)
-
Impact of the nutritional status of children with congenital heart diseases on the early post-operative outcome
Egyptian Pediatric Association Gazette (2021)