Abstract
Although angiotensin receptor blockers have different receptor binding properties no comparative studies with cardiovascular disease (CVD) end points have been performed within this class of drugs. The aim of this study was to test the hypothesis that there are blood pressure independent CVD-risk differences between losartan and candesartan treatment in patients with hypertension without known CVD. Seventy-two primary care centres in Sweden were screened for patients who had been prescribed losartan or candesartan between the years 1999 and 2007. Among the 24 943 eligible patients, 14 100 patients were diagnosed with hypertension and prescribed losartan (n=6771) or candesartan (n=7329). Patients were linked to Swedish national hospitalizations and death cause register. There was no difference in blood pressure reduction when comparing the losartan and candesartan groups during follow-up. Compared with the losartan group, the candesartan group had a lower adjusted hazard ratio for total CVD (0.86, 95% confidence interval (CI) 0.77–0.96, P=0.0062), heart failure (0.64, 95% CI 0.50–0.82, P=0.0004), cardiac arrhythmias (0.80, 95% CI 0.65–0.92, P=0.0330), and peripheral artery disease (0.61, 95% CI 0.41–0.91, P=0.0140). No difference in blood pressure reduction was observed suggesting that other mechanisms related to different pharmacological properties of the drugs may explain the divergent clinical outcomes.
Similar content being viewed by others
Introduction
Hypertension is an important risk factor for the development of cardiovascular disease (CVD), and blood pressure lowering treatments have preventive effects.1 Several studies comparing antihypertensive agents have shown differences in risk reduction in CVD with a similar blood pressure lowering effect, suggesting that specific pharmacological mechanisms may be involved.2, 3, 4 The renin-angiotensin system (RAS) is targeted by some of the most widely used antihypertensive medication classes: angiotensin converting enzyme inhibitors and angiotensin receptor blockers (ARBs). ARBs are increasingly used in the treatment of hypertension because of fewer side effects than angiotensin converting enzyme inhibitors, combined with similar blood pressure lowering abilities.5, 6
The RAS provides the most powerful regulation of blood pressure and angiotensin II is the primary mediator in this system. The binding of angiotensin II to an AT1 receptor produces a number of potentially harmful effects that include increased blood pressure, progression of atherosclerosis, myocardial-, and vascular hypertrophy. Losartan was the first ARB and has been shown to reduce the risk of stroke and new onset diabetes compared to atenolol.4 A more recently developed ARB is candesartan, which has also shown a proven benefit in the treatment of heart failure and the prevention of stroke and new onset diabetes.7, 8, 9 Although they belong to the same class of drugs, losartan and candesartan have important pharmacological differences.10 The binding to the AT1 receptor is tighter and lasts longer with candesartan compared to losartan.10, 11, 12
Although losartan and candesartan have, in several large randomized clinical trials, documented effect on CVD-risk reduction, no head-to-head comparison studies have been performed. The established approach to study differences between the two drugs is a randomized controlled trial.13 Such a trial would, however, take 5–10 years and involve large resourses that are usually unavailable. In addition, it is difficult to justify from a health political perspective. The randomized controlled trials also differ from a real life clinical setting as there is a selection of both physicians and patients; the treatment alternatives depend on the study protocol and the study itself may compromise patient–doctor relationships.14 We therefore studied a real life clinical situation by electronically extracting patient data from electronic primary care journals and mandatory Swedish national registers for death and hospitalization.15, 16
The aim of this study was to test the hypothesis that losartan and candesartan have different effects on CVD-risk reduction in a real life setting with primary hypertensive treatment.
Methods
The study protocol was reviewed and approved by the regional research ethics committee in Uppsala, Sweden and registered with ClinicalTrials.gov, number NCT00620178.
Patients eligible for the study were males or females, more than 17 years of age who were prescribed candesartan (Anatomical Therapeutic Chemical (ATC) classification system: C09CA06, C09DA06) or losartan (ATC: C09CA01, C09DA01) for hypertension in the period 1 January 1999–31 December 2007. The first prescription found in the primary care journals within the study period was defined as the index prescription (treatment onset).
Exclusion criteria were a prior history of CVD and on-going malignancy (with the exception of basal cell or squamous cell carcinoma of the skin) found in primary care journals or the Swedish Hospital Discharge Register. Patients who were prescribed vitamin K antagonists, digitalis glycosides, or nitrates within 15 months prior to the index prescription were also considered to have potential CVD and were excluded. The remaining exclusion criterion was the prescription of an RAS inhibitor, other than the study medications within 1 week after index prescription.
In Sweden, blood pressure measurements are performed according to standardized methods, using the manual Korotkoff method or automatic measurements. Sweden has extensive use of well-calibrated blood pressure equipment and measurements are mostly performed by public health nurses. The patients are told to avoid coffee and tobacco 30 min before the examination. After 5 min rest in either the supine or sitting position an appropriate sized cuff is placed on the over arm. Heart rate is measured for 1 min before blood pressure measurement. Communication with the patient is normally not recommended. When several readings are performed, the calculated mean is recorded. A detailed report of blood pressure readings in the Swedish primary care concluded that public health nurses had an overall correct technique.17 When analysing the extracted data, the baseline value for blood pressure was calculated as the mean of the three last available blood pressures during the time period 15 month before index prescription until 14 days after index prescription. Blood pressure at 6 months was calculated as the mean of recorded blood pressures during the time period 2 weeks–6 months after index prescription. From 6 months and onwards, consecutive blood pressure values were calculated as the mean of recorded blood pressures from 0.5 years before and 0.5 years after the specific time point.
The primary composite end point consisted of CVD morbidity, CVD mortality, and elective coronary revascularization procedures. CVD was defined as heart failure (International Classification of Diseases (ICD): I50, ICD-9: 428), cardiac arrhythmias (ICD-10: I46–I48, ICD-9: 427), peripheral artery disease (ICD-10: I70, I71, I74, ICD-9: 440, 441, 444), chronic ischemic heart disease (ICD-10: I20.9, I25.1, ICD-9: 413–414), myocardial infarction (ICD-10: I21–I23, ICD-9: 410, 411, 429), stroke (ICD-10: I61, I63–I64, G45, ICD-9: 431–434, 435), unstable angina (ICD-10: I20.0, ICD-9: 411), and coronary revascularization. Cardiovascular mortality was defined as death due to CVD with the above diagnoses. Diabetes was registered separately (ICD-10: E10–E14, ICD-9: 250).
In Sweden, a patient has only one general practitioner who follows the patient. Both nurses and physicians in a primary care centre have access to the electronic patient journal and are responsible for documenting their examinations. The patient journal is continuously updated with external data (that are radiologic results, ultrasound examinations, hospital discharge data, and laboratory data). The selected 72 primary care centres had to use the same patient journal system to be eligible for participation.18 Generally, the use of electronic patient journals, both in private and public care, is very common in Sweden. The selected journal system was the most widely used patient journal system, having approximately 20 000 users, 57% of all primary care centres in Sweden. No formal randomization of the primary care centres was conducted. However, an effort was made in the recruitment of study sites to ensure a representative selection of primary care centres. Selection of study sites was based on the following criteria to ensure a representative sample of the Swedish population: a mix of rural and urban areas; public and private care providers; small, midsized, and large primary care centres. The use of ARBs was not considered when selecting study sites, and the centres were included by a written invitation. The final selection of centres for the study included 39 public primary care centres located in 5 of the 21 Swedish county councils and 33 private care centres located in 7 of the counties. With regards to size, 13 (18%) small clinics, 12 (17%) midsize clinics, and 47 (65%) large clinics were recruited. With rural areas defined as communities inhabiting <15 000 people, 36 of the sites were considered rural and 36 sites were defined as urban. This sample represents 4.7% of the total number of public care centres and 14.7% of the total number of private care centres in Sweden. Age or other characteristics of the physicians was not considered in the selection.
Patient data were extracted from primary care centre servers using a software system, which has also been used in earlier studies.19, 20, 21, 22 The program scanned all patient journals at the participating primary care centres and identified all patients who were prescribed losartan or candesartan. The patient's social security number was replaced with a study ID when processing the data. Data from 100 patient journals at 25 primary care centres were manually compared with the study database to ensure that the software system had extracted correct patient data. No discrepancies were found.
The date of admission and discharge diagnoses and causes of death were collected from the Swedish Hospital Discharge and Cause of Death Registers.15, 16 The merging of data from primary care and hospital registers was performed by the Swedish National Board of Health and Welfare.
Statistical methods
The data were processed and analysed at an independent statistical contract company, and the study database was managed by the Department of Public Health and Caring Sciences, Uppsala University, Uppsala, Sweden.
The included patients were only eligible for the analysis as long as they continued treatment with the losartan or candesartan. The observation period ended on the date when the patient died, started a new RAS inhibiting drug or until the last valid day of the index prescription.
All descriptive data are given as mean or proportion. The difference in continuous and categorical data was analysed with t-test and χ2 test, respectively. We used proportional hazards regression to compute hazard ratio (HR) and 95% confidence interval (CI). In the primary survival model, adjustments were made for age, gender, diabetes, and prescription index year. Additional adjustments in the primary survival model were considered as sensitivity analyses. Kaplan–Meier curves were used to illustrate risk development during follow-up. If one patient had several end points, only the first was used in the survival model. Although the maximum observation period was 108 months, the x axis for the plots was truncated at 96 months because of low number of observations after this time.
To assess the difference in discontinuation we removed x number of discontinued subjects from the losartan group, which gave a similar proportion of discontinued subjects as that in the candesartan group (that is 24.8%). When performing the sensitivity analysis, only discontinuation before a CVD event could be used. The patient numbers therefore differs slightly from the discontinuation reported for the total observation time. An HR that remains similar, compared to the primary survival models, will support the main results. By solving the equation (1880−x/6771−x=1819/7329), x was found to be 265. All statistical analyses were performed using R version 2.7.2.23
Results
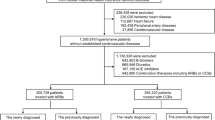
Among 24 943 eligible patients; 14 100 (56.5%) were included in the study (Figure 1). The number of discontinued patients was significantly higher in the losartan group compared to the candesartan group, 31.4% (n=2123) vs 27.5% (n=2015, P<0.0001). Patients who were initially treated with losartan were also more frequently converted to another RAS inhibitor compared with candesartan-treated patients 13.9% (n=939) vs 10.8% (n=788, P<0.0001) during the study. Other reasons for discontinuations were death (2.3% (n=155) vs 2.1% (n=156, P=0.1588), in the losartan group and the candesartan group, respectively) or cessation of study drug prescription (15.2% (n=1029] vs 14.6% (n=1071, P=0.3768), in the losartan group and the candesartan group, respectively).
To assess the effects of the difference in discontinuation, 265 discontinued subjects from the losartan group were omitted to obtain the proportion of discontinued subjects equal to the candesartan group, and the survival models were re-run. The 265 discontinued subjects were selected in three different ways: subjects with shortest exposure time, subjects with longest exposure time, and randomly in 1000 repeated analyses. None of these analyses changed the conclusions as compared with the primary survival model (data on file).
The proportion of included patients per year, from 1999 to 2007, was similar when comparing the losartan and candesartan group (data on file). All 72 primary care centres prescribed both losartan and candesartan, although in various ratios. The prescription ratio for losartan/candesartan had a linear range from 7 to 85% among the centres.
The losartan group were older (+0.7 years), had lower systolic and diastolic blood pressures (−1/−1 mm Hg), had higher blood glucose (+0.1 mmol l−1), had higher HbA1c (+0.1%), and had a higher prevalence of diabetes (+2.8%), were less frequently treated with thiazides (−2.3%) and β-blockers (−2.0%) and more frequently treated with glucose lowering drugs (+1.7%), statins (+1.3%), and antithrombotics (+0.8%) compared with the candesartan group (Table 1).
Some blood pressure recordings were absent at all time points. Figure 2 shows the similar blood pressure levels that were recorded during the follow-up, and also the number of missing values. The frequency of blood pressure recordings was equal in both groups. When calculating 95% CIs for the blood pressures values at each time point, no significant differences between the losartan and candesartan group were observed (data on file).
During the study (median follow-up 2.0 years, maximal follow-up 9.0 years, and 36 339 patient years), 676 CVD events occurred in the losartan group, and 575 in the candesartan group (Table 2). The cumulative incidence of the primary composite end point was lower in the candesartan group compared to the losartan group (Figure 3) and the adjusted HR was 0.86 (95% CI 0.77–0.96, P=0.0062) (Table 2).
Figure 4 illustrates the risk development among six separate end points. The cumulative incidence of heart failure, cardiac arrhythmias, and peripheral artery disease was lower with candesartan than losartan (Figure 4, panels a, b, and c). Compared to losartan, the adjusted HR was lower for heart failure 0.64 (95% CI 0.50–0.82, P=0.0004), cardiac arrhythmias 0.80 (95% CI 0.65–0.98, P=0.0330), and peripheral artery disease 0.61 (95% CI 0.41–0.91, P=0.0140) in the candesartan group (Table 2). Cardiac arrhythmias were mainly because of atrial fibrillation (n=193, 91.9%), which had a separate adjusted HR of 0.77 (95% CI 0.62–0.95, P=0.0170).
Chronic ischemic heart disease, myocardial infarction, and stroke showed similar cumulative incidence in both groups (Figure 4, panels d, e, and f, respectively). The losartan group showed a small non-significant, increased incidence of the following events: chronic ischemic heart disease, myocardial infarction, stroke, hospitalization for unstable angina, elective coronary revascularization, cardiovascular mortality, total mortality, and new onset diabetes compared with the candesartan group (Table 2). No differences in risk for these events were found in proportional hazards regression models. Chronic ischemic heart disease was the exception and had an unadjusted lower risk in the candesartan group (0.80 (95% CI 0.66–0.99, P=0.0350)) compared with the losartan group.
Figure 5 shows that the use of both losartan and candesartan was according to prescribing recommendations for hypertension. The losartan group generally started with 50 mg and up-titrated to fixed combination 50/12.5 mg. The candesartan group, on the other side, mainly started with 4 and 8 mg in patients with higher blood pressure at baseline, +1/+1 mm Hg. Within the first 6 months these patients were up-titrated to 16 and 16/12.5 mg. Within the first 6 months losartan was up-titrated by 6.1% and candesartan by 13.2%.
The frequency of fixed combination tablets (ARB+hydrochlorothiazide) in the losartan group rose from 24.7 to 60.5% (+35.9%) compared with an increase from 13.4 to 33.4% (+20.0%) in the candesartan group.
Figure 6 shows the use of other antihypertensive medications (thiazides, calcium channel blockers, and β-blockers) increased in both groups during follow-up. The use of thiazides (both separate and in fixed combination tablets) was more frequent in the losartan group compared to the candesartan group. Slightly more prescriptions of oral glucose lowering drugs at baseline and during follow-up were observed in the losartan group compared to the candesartan group.
Sensitivity analyses
When additionally adjusting for lipid lowering drugs, thiazides, β-blockers, and antithrombotics the risk of CVD in the candesartan group remained significantly lower (HR 0.84, 95% CI 0.75–0.94, P=0.0030). When adding systolic blood pressure to the adjustments (age, gender, diabetes, index year, lipid lowering drugs, thiazides, β-blockers, and antithrombotics), the number of patients available for a survival analysis was reduced by 20% (n=11230) because of absent blood pressure values. However, despite this loss of patients in the survival model, the risk remained similar (HR 0.87, 95% CI 0.77–0.98, P=0.0250) compared with the primary survival model.
To further evaluate potential effects of differences at baseline, patients without a history of diabetes or treated with any glucose lowering drug (n=11 596) were analysed separately. When adjusting for age, gender, and index year, the risk of CVD remained similar (HR 0.86, 95% CI 0.76–0.98, P=0.0210) in patients without diabetes.
Discussion
In this study, 14 100 patients in a primary prevention setting were treated with either losartan (n=6771) or candesartan (n=7329). They fulfilled the inclusion criteria of being hypertensive and without previously known CVD. Patients were followed for a median of 2 years with a total of 36 339 patient years, using the combination of patient journal data in 72 primary care centres and the mandatory Swedish national hospital discharge and cause of death registers. There was a substantial blood pressure reduction after treatment with both drugs, with no difference in blood pressure between the two treatment groups during the follow-up period. Our results showed that candesartan was more effective than losartan in reducing the risk of primary composite end point, HR 0.86 (95% CI 0.77–96, P=0.0062).
We used a method that uses the strengths of electronic patient registers, which cover large patient groups, making them increasingly accessible to real life observational studies. However, though this method provides large number of patients in short time and at a rather low cost, some limitations are inevitable.
One of the limitations with this method is the absence of recorded baseline data in the electronic patient primary care journal. Blood pressure recordings were only registered in 80% of all the patients at baseline, leaving 20% unaccounted for, which was similar in both groups. The candesartan group had a slightly higher baseline blood pressure compared to the losartan group. When adjusting for blood pressure we lost 20% of the patient material in the survival model, but the results remained similar. This type of large register study will always be associated with incomplete data. However, the large number of patients may compensate for this weakness.
When including patients over a longer time span, the possibility of variations in the patient handling may be a confounder. For example, an important potential confounding factor could have been variation in hypertensive treatment, favouring inclusion either in the losartan or candesartan group. The annual frequency of inclusion to the losartan or candesartan group from 1999 to 2007 was, however, similar. This suggests that there was a similar assessment of hypertensive patients with no differences between groups regarding the time point of inclusion.
Some confounders are difficult to measure and therefore not usable in a survival model. These confounders may have changed the baseline risk among the patients (that are the recording of diagnoses, new indications, reimbursement, guidelines, marketing, and shift in the ICD system or continuous updating of the software for electronic patient journal systems). Adjusting for all these potential confounders is difficult and we, therefore, made adjustments for the year of index prescription to minimize the possible effects of temporal changes with regard to the above parameters.
Registry data are to a certain degree associated with absent laboratory data (blood samples and blood pressure measurements) at specific time intervals. However, in our study the frequency of laboratory data did not differ markedly between the two groups, suggesting similar need of medical attention at baseline.
We have adjusted for differences in observed CVD risk between the two groups at inclusion. However, differences in undetected risk at inclusion may also be of concern. When excluding patients because of earlier CVD, more patients (9.9%) were excluded from the losartan group. Consequently, the risk of undetected CVD may have been higher in this group, requiring a reliable method of finding CVD before inclusion. To exclude patients with earlier CVD, patient journals in primary care were searched for CVD diagnoses on average 5.8 years before inclusion and drugs associated with CVD before inclusion. Patients were also scanned for hospitalizations caused by CVD in the Swedish Hospital Discharge Register, which has had mandatory registration since 1984.16 The combination of these two search techniques should therefore have lowered the risk of skewed CVD prevalence at baseline as all patients with documented CVD in the primary care journals, hospital records, or indicated by drug prescriptions were excluded. Thus, we feel that we have reasonable well excluded the risk of confounding by indication. The increased prescriptions of antithrombotics and statins at baseline in the losartan group could have also signalled a systematic failure in CVD detection before inclusion. However, having more diabetic patients in the losartan group may have translated into more prescriptions of drugs used in the primary prevention of CVD. Furthermore, the HR for CVD was unchanged compared to the primary survival model when additionally adjustments were made for baseline differences in lipid lowering drugs, thiazides, β-blockers, and antithrombotics.
The study had a follow-up time of median 2.0 years, and 47% of the patients were followed for 2 years. Compared to the LIFE study (93% over 2 years), this follow-up intensity may seem low and stresses the need of large patient groups when performing a register study with this method.4 The explanation for this drop in patient numbers in our study could partly be due to the lack of adherence to the primary treatment of hypertension (approximately 30%), which was also described in other real life studies.23 Randomized controlled trials have also had a similar follow-up time as those in our study. In the JUPITER trial the median follow-up time was 1.9 years and only 43% of the patients were followed for 2 years.25
Our main finding was a risk reduction in CVD mainly determined by heart failure, cardiac arrhythmias, and peripheral artery disease. The risk of heart failure was reduced by 36% in the candesartan group. Heart failure may be a result of left ventricular hypertrophy and/or myocardial infarction, and is therefore responsive to the myocardial remodelling properties of a drug. Both losartan and candesartan have beneficial remodelling effects on hypertrophic myocardium.4, 26 The risk of cardiac arrhythmias in the candesartan group was 20% lower and may be explained by the lower incidence of heart failure. Alternatively, the lower incidence of atrial fibrillation may explain the lower risk of heart failure.27 We believe that the lower risk of new heart failure and cardiac arrhythmias in the candesartan group may be due to a more potent inhibition of AT1 receptors as this occurred at the same level of blood pressure control and in patient groups with similar baseline characteristics.10
Furthermore, candesartan has reported positive effects on risk markers such as high oxidative stress and increased coagulability compared to losartan, which may explain the lower risk for CVD complications.28 Interestingly, the risk of peripheral artery disease was lower (39%) in the candesartan group compared to the losartan group. A possibility is that the peripheral circulation may be reduced in patients with heart failure leading to earlier ischemic symptoms in the lower limbs.
There was no difference between the two treatment groups in blood pressure throughout the study, with an average blood pressure of approximately 145/85 mm Hg in both groups. The blood pressures in this study are office readings and a potential difference in 24 h blood pressure has not been investigated and can therefore not be excluded. Slightly elevated baseline blood pressure in the candesartan group suggests that this group may have had a higher baseline CVD risk. However, after adjustment for baseline systolic blood pressure, only small effects in the survival analyses were seen. The similar blood pressure in both groups after inclusion may explain why we did not observe any differences in the risk of stroke. The LIFE study, which compared losartan and atenolol, did show a blood pressure independent reduction in stroke risk in favour of losartan, but atenolol may be an inferior drug for stroke prevention.4, 29 Our results suggest that candesartan and losartan have similar effects on stroke prevention.
Up-titration of the ARB dose from the index prescription was somewhat higher in the candesartan group compared to the losartan group, which may be seen in light of the different start dosage alternatives and the next dose step. The losartan group was generally started with ARB only and up-titrated by adding thiazides, without changing the ARB dose. The candesartan group, on the other side, was mainly started with lower ARB dosages in patients with significantly higher blood pressure at baseline. Within the first 6 months those patients were up-titrated by both increasing ARB dosage and adding thiazides. The initial ARB dosage was therefore relatively lower during the first 6 months in the candesartan group compared with the losartan group. The ARB use was therefore considered reasonably comparable in the two groups after up-titration.
In this study, the initial and continued use of thiazides was more frequent in the losartan group compared to the candesartan group. The increased use of thiazides in the losartan group support reports of an improved blood pressure lowering effect with candesartan compared with losartan when given as monotherapy.10, 30, 31 Recently, the LIFE study group reported that concomitant thiazide therapy was associated with reduced cardiovascular morbidity and mortality, independent of blood pressure and electrocardiographic evidence of left ventricular hypertrophy.32 Consequently, the use of more concomitant thiazide treatment in patients treated with losartan should therefore have potentially reduced CVD risk in this group. Other concomitant antihypertensive treatments (calcium channel blocker and β-blocker) did not differ during the observation period. We have therefore no reason to believe that the use of additional antihypertensive drugs could have influenced our results.
Conclusion
We believe that our study method provides a new tool that can be used to study existing treatments, providing rapid results at a low cost. However, it requires the wide use of similar electronic patient journal systems in primary care and a long tradition with nationwide hospitalization and cause of death registers. Sweden offers this combination and provides the opportunity to study differences between treatments, not feasible to assess in randomized clinical trials.
The results of this study suggest that there is a blood pressure independent risk reduction in CVD with candesartan compared to losartan in the primary treatment of hypertension. This suggests that pharmacological differences within the ARB class may translate into important clinical effects. Furthermore, the study of a real life situation may provide an additional method that can be used to assess existing and future treatments.

Conflict of interest
The study was designed by a steering committee (authors of this paper) and AstraZeneca. The steering committee had full access to all data and had full independence to interpret them. Professor David Russell, Professor Sverre E Kjeldsen, and Jan Stålhammar did not receive any financial compensation for their work in this study and do not declare any conflict of interest. Johan Bodegard and Pål Hasvold are employed by AstraZeneca and participated as non-voting members in the steering committee. Urban Olsson was responsible for database managing and is employed by an independent statistical company who were invoiced by AstraZeneca.
References
Lawes CM, Vander Hoorn S, Rodgers A . Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371 (9623): 1513–1518.
Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL et al. A comparison of outcomes with angiotensin-converting—enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003; 348 (7): 583–592.
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288 (23): 2981–2997.
Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002; 359 (9311): 995–1003.
Gavras H . Update on the clinical pharmacology of candesartan cilexetil. Am J Hypertens 2000; 13 (1 Pt 2): 25S–30S.
Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358 (15): 1547–1559.
Young JB, Dunlap ME, Pfeffer MA, Probstfield JL, Cohen-Solal A, Dietz R et al. Mortality and morbidity reduction with Candesartan in patients with chronic heart failure and left ventricular systolic dysfunction: results of the CHARM low-left ventricular ejection fraction trials. Circulation 2004; 110 (17): 2618–2626.
Lithell H, Hansson L, Skoog I, Elmfeldt D, Hofman A, Olofsson B et al. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens 2003; 21 (5): 875–886.
Lindholm LH, Persson M, Alaupovic P, Carlberg B, Svensson A, Samuelsson O . Metabolic outcome during 1 year in newly detected hypertensives: results of the Antihypertensive Treatment and Lipid Profile in a North of Sweden Efficacy Evaluation (ALPINE study). J Hypertens 2003; 21 (8): 1563–1574.
Van Liefde I, Vauquelin G . Sartan-AT1 receptor interactions: in vitro evidence for insurmountable antagonism and inverse agonism. Mol Cell Endocrinol 2009; 302 (2): 237–243.
Fabiani ME, Dinh DT, Nassis L, Casley DJ, Johnston CI . In vivo inhibition of angiotensin receptors in the rat kidney by candesartan cilexetil: a comparison with losartan. Am J Hypertens 2000; 13 (9): 1005–1013.
Ojima M, Inada Y, Shibouta Y, Wada T, Sanada T, Kubo K et al. Candesartan (CV-11974) dissociates slowly from the angiotensin AT1 receptor. Eur J Pharmacol 1997; 319 (1): 137–146.
Stanley K . Design of randomized controlled trials. Circulation 2007; 115 (9): 1164–1169.
Nallamothu BK, Hayward RA, Bates ER . Beyond the randomized clinical trial: the role of effectiveness studies in evaluating cardiovascular therapies. Circulation 2008; 118 (12): 1294–1303.
Bjørkenstam C . The Causes of Death Register. 2008 (cited; available from: http://www.socialstyrelsen.se/en/Statistics/statsbysubject/The_Cause_of_Death_Register.htm).
Edberg A, Forsberg L, Jacobsson A, Nyqvist K . The National Patient Register. 2008 (cited; available from: http://www.socialstyrelsen.se/en/Statistics/statsbysubject/The+Swedish+Hospital+Discharge+Register.htm).
Drevenhorn E, Hakansson A, Petersson K . Blood pressure measurement—an observational study of 21 public health nurses. J Clin Nurs 2001; 10 (2): 189–194.
Profdoc Software. 2008 (cited; Medical Office) Available from: http://www.profdoc.com/medical_office/software/.
Lidman B, Linder R . Working Model. 2007 (cited; available from: http://www.pygargus.se/3_en.html).
Lindgren P, Borgstrom F, Stalhammar J, Alemao E, Yin DD, Jonsson L . Association between achieving treatment goals for lipid-lowering and cardiovascular events in real clinical practice. Eur J Cardiovasc Prev Rehabil 2005; 12 (6): 530–534.
Ringborg A, Martinell M, Stalhammar J, Yin DD, Lindgren P . Resource use and costs of type 2 diabetes in Sweden—estimates from population-based register data. Int J Clin Pract 2008; 62 (5): 708–716.
Ringborg A, Lindgren P, Martinell M, Yin DD, Schon S, Stalhammar J . Prevalence and incidence of Type 2 diabetes and its complications 1996–2003—estimates from a Swedish population-based study. Diabet Med 2008; 25 (10): 1178–1186.
Team RDC. R: A Language and Environment for Statistical Computing. Fountation for Statistical Computing: Vienna Austria, 2008.
Corrao G, Zambon A, Parodi A, Poluzzi E, Baldi I, Merlino L et al. Discontinuation of and changes in drug therapy for hypertension among newly-treated patients: a population-based study in Italy. J Hypertens 2008; 26 (4): 819–824.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359 (21): 2195–2207.
McMurray JJ, Ostergren J, Swedberg K, Granger CB, Held P, Michelson EL et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-added trial. Lancet 2003; 362 (9386): 767–771.
Aksnes TA, Schmieder RE, Kjeldsen SE, Ghani S, Hua TA, Julius S . Impact of new-onset diabetes mellitus on development of atrial fibrillation and heart failure in high-risk hypertension (from the VALUE trial). Am J Cardiol 2008; 101 (5): 634–638.
Koh KK, Han SH, Chung WJ, Ahn JY, Jin DK, Kim HS et al. Comparison of effects of losartan, irbesartan, and candesartan on flow-mediated brachial artery dilation and on inflammatory and thrombolytic markers in patients with systemic hypertension. Am J Cardiol 2004; 93 (11): 1432–1435, A1410.
Lindholm LH, Carlberg B, Samuelsson O . Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet 2005; 366 (9496): 1545–1553.
Andersson OK, Neldam S . The antihypertensive effect and tolerability of candesartan cilexetil, a new generation angiotensin II antagonist, in comparison with losartan. Blood Press 1998; 7 (1): 53–59.
Lacourciere Y, Asmar R . A comparison of the efficacy and duration of action of candesartan cilexetil and losartan as assessed by clinic and ambulatory blood pressure after a missed dose, in truly hypertensive patients: a placebo-controlled, forced titration study. Candesartan/losartan study investigators. Am J Hypertens 1999; 12 (12 Pt 1–2): 1181–1187.
Okin PM, Devereux RB, Hille DA, Kjeldsen S, Lindholm LH, Edelman JM et al. Concomitant hydrochlorothiazide therapy in hypertensive patients is associated with reduced cardiovascular morbidity and mortality independent of blood pressure and electrocardiographic left ventricular hypertrophy: the LIFE study. Circulation 2008; 118 (18): 886.
Acknowledgements
We are very thankful for the ideas, encouragement, and scientific support provided by Anders Ljunggren, AstraZeneca Mölndal. We thank Bo Lidman, Pygargus AB, for his engagement in the data collection. Sven Olof Jansson was involved in designing the study, protocol writing, and preparation of the paper. The study was funded by AstraZeneca AS Norway.
Author information
Authors and Affiliations
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Licence. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kjeldsen, S., Stålhammar, J., Hasvold, P. et al. Effects of losartan vs candesartan in reducing cardiovascular events in the primary treatment of hypertension. J Hum Hypertens 24, 263–273 (2010). https://doi.org/10.1038/jhh.2009.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2009.77
Keywords
This article is cited by
-
Prediction of CYP-mediated silybin A-losartan pharmacokinetic interactions using physiological based pharmacokinetic modeling
Journal of Pharmacokinetics and Pharmacodynamics (2022)
-
Epidemiology of Pulmonary Fibrosis: A Cohort Study Using Healthcare Data in Sweden
Pulmonary Therapy (2019)
-
In Silico Investigations of Chemical Constituents of Clerodendrum colebrookianum in the Anti-Hypertensive Drug Targets: ROCK, ACE, and PDE5
Interdisciplinary Sciences: Computational Life Sciences (2018)
-
Evaluation of the use of Swedish integrated electronic health records and register health care data as support clinical trials in severe asthma: the PACEHR study
Respiratory Research (2016)
-
Diabetes and CVD risk during angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker treatment in hypertension: a study of 15 990 patients
Journal of Human Hypertension (2014)