Abstract
Hereditary motor and sensory neuropathy-type Lom (HMSNL), also known as CMT4D, a demyelinating neuropathy with late-onset deafness is an autosomal recessive disorder threatening Roma population worldwide. The clinical phenotype was reported in several case reports before the gene discovery. HMSNL is caused by a homozygous founder mutation p.Arg148* in the N-Myc downstream-regulated gene 1. Here, we report findings from the Czech Republic, where HMSNL was found in 12 Czech patients from eight families. In these 12 patients, 11 of the causes were due to p.Arg148* mutation inherited from both parents by the autosomal recessive mechanism. But in one case, the recessive mutation was inherited only from one parent (father) and unmasked owing to an uniparental isodisomy of the entire chromosome eight. The inherited peripheral neuropathy owing to an isodisomy of the whole chromosome pointed to an interesting, less frequent possibility of recessive disease and complications with genetic counseling.
Similar content being viewed by others
Introduction
Hereditary motor and sensory neuropathies (HMSN), also known as Charcot–Marie–Tooth diseases (CMT), are a heterogeneous group of inherited peripheral neuropathies (IPN), with the main clinical features being progressive distal muscle weakness and atrophy, foot deformities and distal sensory loss.1
HMSN-type Lom (HMSNL, CMT4D, OMIM 601455) is an autosomal recessive demyelinating neuropathy affecting patients of Roma origin, for which late-onset deafness was described.2 In addition to HMSN Lom, HMSN-type Russe (HMSNR, CMT4G, OMIM 605285) is another, later described, but probably more frequent nonsyndromic neuropathy among Roma. Both these IPNs typically affect only the Roma population, and only a few exceptional cases have been described with no known Roma ancestors.3, 4 HMSNL patients have been reported from throughout Europe with the exception of Bulgaria and Spain only in single patients or families.4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 No patients with HMSNL were reported from the Czech Republic yet.
HMSNL is typically caused by a single ancestral mutation p.Arg148* in the N-Myc downstream-regulated gene 1 (NDRG1). Only two other disease-causing mutations were reported in NDRG1 yet. The c.538-1G>A has been recently reported in one patient,12 and the copy-number variation—exonic duplication has recently been reported in a family with a similar phenotype as HMSNL.17
Uniparental disomy (UPD) is a term for inheritance of both chromosomes or parts of the chromosomes from only one parent. In case, the chromosomes are identical, two copies of one homolog, than the term uniparental isodisomy is used.18 So far, only two papers about the UPD causing the IPN were published. Benko et al.19 described an isodisomy of chromosome 1 causing Gaucher disease and worsening CMT, which was already present in the patient’s father and his father owing to a dominant mutation in the MPZ gene. Last year, a segmental UPD of part of the chromosome 16 was reported to cause a giant axonal neuropathy.20 By the whole-chromosome UPD and by the sporadic occurrence of CMT in the family, our patient seems to be unique.
Here, we address the clinical and genetic findings of 12 patients from eight Czech families and show that HMSNL is an important cause of neuropathy in the Czech Republic. Inherited neuropathy owing to an isodisomy of a whole chromosome points21 to an intriguing problem with genetic counseling of the risk of recurrence of the disease. We present the clinical and electrophysiological findings from a large group of HMNSL patients, children and adults, and provide evidence for the prevalence of HMSNL in the Czech Republic.
Materials and methods
Patients
Patients were recruited from the database of DNA laboratory, which is the only center for DNA diagnostics of inherited neuropathies in the Czech Republic. All Roma patients were originally tested for CMT1A/HNPP (hereditary neuropathy with liability to pressure palsies), HMSNL and HMSNR during the period 2007–2016. Overall, 71 patients were tested for HMSNL, including the family members for possible carriership of the founder mutation p.Arg148*. Patient 10 was brought to our attention by the results from massively parallel sequencing with the panel of all IPN genes as the family was not aware of their Roma ancestor (this patient is briefly mentioned among 51 patients who received a genetic diagnosis by gene panel testing in our paper by Laššuthová et al.21). All tested patients signed the informed consent for DNA diagnostics of hereditary neuropathy and the study was approved by the local ethical committee.
Methods
Exon 7 of NDRG1 (NM_006096.3) containing the ancestral founder mutation p.Arg148* (c.442 C>T) was amplified from genomic DNA. The PCR fragment was Sanger sequenced on an ABI 3130 Genetic Analyzer (Applied Biosystems, Foster City, CA, USA) and analyzed with Mutation Surveyor program (Softgenetics, State College, PA, USA).
Massively parallel sequencing of a panel of all IPN-associated genes was carried out with HaloPlex method (Agilent Technologies, Santa Clara, CA, USA). Custom design for 64 IPN genes was used and prepared library was sequenced on Miseq (Illumina, San Diego, CA, USA) as described by Laššuthová et al.21
Four dinucleotide microsatellite markers (STRs) from chromosome 8 (D8S1829, D8S286, D8S1474 and D8S551) were used for haplotype analysis. PCR products were amplified with fluorescently labeled primers and products were analyzed on ABI 3130 Genetic Analyzer (Applied Biosystems).
Whole-genome single-nucleotide polymorphism (SNP) array from peripheral blood using the HumanCyto SNP-12v2.1 (Illumina) was performed to examine all chromosomes to confirm the isodisomy of the entire chromosome 8. The evaluation was carried out with Illumina KaryoStudio 1.4 and GenomeStudio V2011.1.
Results
We found the NDRG1 p.Arg148* mutation in a homozygous state in 12 patients from eight families. The clinical features of HMSNL patients are compiled in Table 1. Photos of available patients are in Figure 1. All patients except one (patient 10) were of Roma origin (both parents Roma). In three families, additional family members were affected. Delayed motor milestones were described in six patients. Age of onset in eight patients was between 0 and 5, in two patients between 5 and 10, in one patient between 10 and 20, and is not known in one patient. The first symptoms were usually gait problems. In one patient, atypical postural tremor was present. In clinical neurological examination, distal lower limb weakness was present in all patients, distal upper limb weakness in three patients and only one patient was classified with cerebellar syndrome at the beginning of the disease. Foot deformities or orthopedic corrections were present in five patients. Orthopedic correction can rapidly improve the walking abilities in patients with severe feet deformities (comparison of patient 6/C in 11 and 22 years of age—Figure 1). The question about hearing loss has recently been evaluated by the attending physicians. Hearing loss in four patients older than 27 years was detected. Nerve conduction studies described primary clearly demyelinating neuropathy in all patients. Nerve conduction studies (Table 2) showed motor nerve conduction velocities decreased to 13–21 m s−1, and sensory nerve action potentials (SNAPs) usually absent even in very young patients (2.5–8 years) and even longer before the weakness is detectable. Nerve biopsy performed before the DNA testing availability was carried out in two patients and showed demyelinating neuropathy. In one patient, atypical pupillary reaction was found.
Pictures of selected patients with HMSNL. Patient 6/C (22 years) and 7/C suffer severe muscle wasting of the legs extending up the thigh. On the upper limbs, the reduction of the thenar and hypothenar muscles is present. The comparison of patient 6/C at the age of 11 and 22 years of age clearly show the feet deformities that did not allow walking. Corrective surgery allow almost normal walking again. In Patient 10, only feet deformities are present, at the age of 6. HMSNL, HMSN Lom.
After CMT1 neuropathy was clinically diagnosed in patient 10, the most frequent causes of IPN were tested with negative results (CMT1A/HNPP, GJB1 and MPZ). Subsequent massively parallel sequencing of a gene panel for IPN, tested only in patient 10, revealed two possible causal mutations. One was surprisingly homozygous p.Arg148* in NDRG1, causing HMSNL neuropathy in Roma, and the second was heterozygous p.Arg113* (c.337 C>T) in REEP1, previously reported as pathogenic in one family with severe complicated hereditary spastic paraparesis.22 Interestingly, examination of both parents for segregation showed both variants in heterozygous state only in the healthy father (Figure 2). The same results were gained from the repeated sampling DNA to exclude sample exchange. All SNPs from chromosome 8 included in the IPN panel were homozygous; namely in ARHGEF10, NEFL, GDAP1 and NDRG1, this raised the hypothesis of UPD. Subsequent haplotype analysis with STR markers revealed only alleles from the father (Figure 2). UPD, in this case, the complete isodisomy of chromosome 8, was confirmed by a whole-genome SNP array. There was only homozygous signal in the entire length of chromosome 8, despite the presence of two copies of the chromosome (Figure 2). For other chromosomes, the signal was combination of homozygous and heterozygous SNPs, except for the sex chromosomes. Patient 10 is a man with one copy of X and Y chromosome. A variant in REEP1 was detected also in the father and paternal grandfather, but neurological examination did not reveal any IPN or spastic paraparesis in these two adult men, therefore, we concluded this variant is probably not pathogenic.
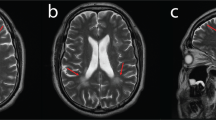
The isodisomy of chromosome 8. (a) A pedigree of patient 10; the occurrence of NDRG1 (p.Arg148*) and REEP1 (p.Arg113*) mutations is indicated; haplotype analysis with the use of microsatellite markers—first two markers are clearly only from the father, patient 10 is homozygous for all the four markers. (b) The chromatogram of p.Arg148* sequence (c.442 C>T), unlike expectations, the mother is only wildtype for the mutation and not a heterozygous carrier. (c) Results of whole-genome genotyping using the SNP array. The results for chromosome 8 are shown in the first two boxes—the loss of heterozygosity for the whole chromosome 8 is present—no heterozygous signal for 0.5 B allele frequency is present in the first box, only 0.0 and 1.0 values represent only homozygous SNPs for whole chromosome 8 are present. Normal two copies of chromosome 8 were detected in box two (log R ratio is 0—no deletion or duplication). For comparison, the normal finding for chromosome 9 is shown (last two boxes). In the third box, the signals for B Allele frequency for whole chromosome are in all three positions—0.0, 0.5 and 1.0—showing normal mix of homozygous and heterozygous SNPs. A full color version of this figure is available at the Journal of Human Genetics journal online.
Discussion
In our cohort, the causative mutation p.Arg148* in homozygous state was identified in 12 Czech HMSNL patients from eight families, comprising 0.66% from all genetically clarified IPN patients (12 out of 1818), and 24% from all IPN Roma patients (12 out of 50). HMSNL is a rare cause of IPN among Czech patients, but is the second most frequent cause in Roma; only HMSNR is more frequent, found to be mutated in 45% of Roma IPN patients, as we reported recently.23 In the majority of publications, there are only sporadic patients reported, but here we report the disease frequency and importance of HMSNL for the entire Czech Republic.
Only one similar paper about the frequencies in other countries has been reported so far. Sevilla et al.16 reported CMT4C as the most frequent form (57.14%) in the Spanish Roma population, followed by HMSNR (25%) and HMSNL (17.86%). In contrast to Sevilla’s findings, no CMT4C Roma patients have been found in the Czech Republic.24 HMSNL and HMSNR are relatively much more frequent in Czech Roma compared with Spanish Roma.
The characteristics of different Roma groups can vary between different regions in Europe, therefore, it is important to explore the frequency in particular populations for effective guidelines for genetic analysis in individual countries. HMSNL and HMSNR are however well distinguishable by a nerve conduction study. Our results clearly support the following procedure for testing in Roma with IPN; firstly the HMSNR founder mutation (g.9712G>C) and secondly HMSNL founder mutation (p.Arg148*). These tests clarified up to 70% of IPN among Czech Roma. Both tests comprise a simple examination of only one short DNA fragment each, but information about the Roma ethnicity is crucial for accurate and immediate DNA diagnosis. There is high probability that non-Roma patients with HMSNL have a distant relative of Roma origin, and therefore the ancestral mutation was inherited and did not arise de novo in non-Roma patients.3, 4 Similar will apply to patient 10 where mutation is inherited only from the father, and searching in family history appeared the possibility of distant Roma ancestor.
Clinically, HMSNL is a severe type of IPN, with progressive course. First symptoms usually appear in the first decade of life. Severely decreased nerve conduction velocities are detectable in the patients even several years before clinical manifestation, before the weakness and foot deformities manifest, as we have seen in the younger brother of patient 6/C (patient 7/C; Table 2). Corrective orthopedic surgery of feet deformities can significantly improve the quality of life in patients, but often later in life the use of a wheelchair is needed. In two of our patients (6/C, 7/C), audiological assessment revealed normal hearing at the age of 22 and 8 years. But according to new information, patient 6/C already has bilateral hearing loss; he is now 31 years old. Similar hearing loss can be expected in other patients in the fourth decade of life. Four older patients already have hearing loss (2/A, 6/C, 9, 12), but the rest have normal hearing, which is probably owing to their very young age (Table 1). Hearing loss is typical for HMSNL, but according to our results, it is not helpful for diagnosis because it occurs later in life.5
The incidence of UPD of any chromosome is estimated to be about 1:3500 live births.25 Modern technologies, such as whole-genome SNP genotyping, enable the detection of UPD in many cases. UPD for chromosomes where no recessive mutations are present do not cause any clinical manifestation. For others, where the parent is a carrier of a recessive mutation or where it causes an alteration of genomic imprinting depending on the parent origin of chromosome, it results in the specific disease phenotype.25 UPD is a rare but important cause of homozygosity in non-consanguineous families. Some 40 examples were described with recessive disorder owing to an whole-chromosome isodisomy, but no IPN was in the list.26 To our knowledge, this is the report of an unique IPN patient owing to an whole-chromosome isodisomy in a recessive type of IPN. This example illustrates the complexity of the genetic counseling, and without any detailed examinations of parents, the risk of birth of similarly affected child would be 25% as for autosomal recessive inheritance. But detailed results showed the risk for recurrence of the disease in further children of these parents is probably not increased. Patient with isodisomy is at risk for possible additional recessive mutation that maybe present on the affected chromosome.
References
Reilly, M. M., Murphy, S. M. & Laura, M. Charcot-Marie-Tooth disease. J. Peripher. Nerv. Syst. 16, 1–14 (2011).
Kalaydjieva, L., Hallmayer, J., Chandler, D., Savov, A., Nikolova, A., Angelicheva, D. et al. Gene mapping in gypsies identifies a novel demyelinating neuropathy on chromosome 8q24. Nat. Genet. 14, 214–217 (1996).
Echaniz-Laguna, A., Degos, B., Bonnet, C., Latour, P., Hamadouche, T., Levy, N. et al. NDRG1-linked Charcot-Marie-Tooth disease (CMT4D) with central nervous system involvement. Neuromuscul. Disord. 17, 163–168 (2007).
Baethmann, M., Gohlich-Ratmann, G., Schroder, J. M., Kalaydjieva, L. & Voit, T. HMSNL in a 13-year-old Bulgarian girl. Neuromuscul. Disord. 8, 90–94 (1998).
Kalaydjieva, L., Nikolova, A., Turnev, I., Petrova, J., Hristova, A., Ishpekova, B. et al. Hereditary motor and sensory neuropathy—Lom, a novel demyelinating neuropathy associated with deafness in gypsies. Clinical, electrophysiological and nerve biopsy findings. Brain 121 (Pt 3), 399–408 (1998).
Chandler, D., Angelicheva, D., Heather, L., Gooding, R., Gresham, D., Yanakiev, P. et al. Hereditary motor and sensory neuropathy—Lom (HMSNL): refined genetic mapping in Romani (Gypsy) families from several European countries. Neuromuscul. Disord. 10, 584–591 (2000).
Kalaydjieva, L., Gresham, D., Gooding, R., Heather, L., Baas, F., de Jonge, R. et al. N-myc downstream-regulated gene 1 is mutated in hereditary motor and sensory neuropathy-Lom. Am. J. Hum. Genet. 67, 47–58 (2000).
Merlini, L., Villanova, M., Sabatelli, P., Trogu, A., Malandrini, A., Yanakiev, P. et al. Hereditary motor and sensory neuropathy Lom type in an Italian Gypsy family. Neuromuscul. Disord. 8, 182–185 (1998).
Colomer, J., Iturriaga, C., Kalaydjieva, L., Angelicheva, D., King, R. H. & Thomas, P. K. Hereditary motor and sensory neuropathy-Lom (HMSNL) in a Spanish family: clinical, electrophysiological, pathological and genetic studies. Neuromuscul. Disord. 10, 578–583 (2000).
Butinar, D., Zidar, J., Leonardis, L., Popovic, M., Kalaydjieva, L., Angelicheva, D. et al. Hereditary auditory, vestibular, motor, and sensory neuropathy in a Slovenian Roma (Gypsy) kindred. Ann. Neurol. 46, 36–44 (1999).
Leonardis, L., Zidar, J., Popovic, M., Timmerman, V., Lofgren, A., Van Broeckhoven, C. et al. Hereditary motor and sensory neuropathy associated with auditory neuropathy in a Gypsy family. Pflugers Arch. 439, R208–R210 (2000).
Hunter, M., Bernard, R., Freitas, E., Boyer, A., Morar, B., Martins, I. J. et al. Mutation screening of the N-myc downstream-regulated gene 1 (NDRG1) in patients with Charcot-Marie-Tooth disease. Hum. Mutat. 22, 129–135 (2003).
Dackovic, J., Keckarevic-Markovic, M., Komazec, Z., Rakocevic-Stojanovic, V., Lavrnic, D., Stevic, Z. et al. Hereditary motor and sensory neuropathy Lom type in a Serbian family. Acta Myol. 27, 59–62 (2008).
Ricard, E., Mathis, S., Magdelaine, C., Delisle, M. B., Magy, L., Funalot, B. et al. CMT4D (NDRG1 mutation): genotype-phenotype correlations. J. Peripher. Nerv. Syst. 18, 261–265 (2013).
Gabrikova, D., Mistrik, M., Bernasovska, J., Bozikova, A., Behulova, R., Tothova, I. et al. Founder mutations in NDRG1 and HK1 genes are common causes of inherited neuropathies among Roma/Gypsies in Slovakia. J. Appl. Genet. 54, 455–460 (2013).
Sevilla, T., Martinez-Rubio, D., Marquez, C., Paradas, C., Colomer, J., Jaijo, T. et al. Genetics of the Charcot-Marie-Tooth disease in the Spanish Gypsy population: the hereditary motor and sensory neuropathy-Russe in depth. Clin. Genet. 83, 565–570 (2013).
Okamoto, Y., Goksungur, M. T., Pehlivan, D., Beck, C. R., Gonzaga-Jauregui, C., Muzny, D. M. et al. Exonic duplication CNV of NDRG1 associated with autosomal-recessive HMSN-Lom/CMT4D. Genet. Med. 16, 386–394 (2014).
Kotzot, D. & Utermann, G. Uniparental disomy (UPD) other than 15: phenotypes and bibliography updated. Am. J. Med. Genet. A 136, 287–305 (2005).
Benko, W. S., Hruska, K. S., Nagan, N., Goker-Alpan, O., Hart, P. S., Schiffmann, R. et al. Uniparental disomy of chromosome 1 causing concurrent Charcot-Marie-Tooth and Gaucher disease type 3. Neurology 70, 976–978 (2008).
Miyatake, S., Tada, H., Moriya, S., Takanashi, J., Hirano, Y., Hayashi, M. et al. Atypical giant axonal neuropathy arising from a homozygous mutation by uniparental isodisomy. Clin. Genet. 87, 395–397 (2015).
Laššuthová, P., Safka Brozkova, D., Krutova, M., Neupauerova, J., Haberlova, J., Mazanec, R. et al. Improving diagnosis of inherited peripheral neuropathies through gene panel analysis. Orphanet. J. Rare. Dis. 11, 118 (2016).
Hewamadduma, C., McDermott, C., Kirby, J., Grierson, A., Panayi, M., Dalton, A. et al. New pedigrees and novel mutation expand the phenotype of REEP1-associated hereditary spastic paraplegia (HSP). Neurogenetics 10, 105–110 (2009).
Šafka Brožková, D., Haberlova, J., Mazanec, R., Lastuvkova, J. & Seeman, P. HSMNR belongs to the most frequent types of hereditary neuropathy in the Czech Republic and is twice more frequent than HMSNL. Clin. Genet. 90, 161–165 (2016).
Laššuthová, P., Mazanec, R., Vondracek, P., Siskova, D., Haberlova, J., Sabova, J. et al. High frequency of SH3TC2 mutations in Czech HMSN I patients. Clin. Genet. 80, 334–345 (2011).
Yamazawa, K., Ogata, T. & Ferguson-Smith, A. C. Uniparental disomy and human disease: an overview. Am. J. Med. Genet. C Semin. Med. Genet. 154C, 329–334 (2010).
Engel, E. A fascination with chromosome rescue in uniparental disomy: Mendelian recessive outlaws and imprinting copyrights infringements. Eur. J. Hum. Genet. 14, 1158–1169 (2006).
Acknowledgements
We thank the clinicians for their cooperation and examination of patients. Special thanks belong to the patients and their families for participating in this study. Supported by Ministry of Health of the Czech Republic, grant nr. 15-31899A. All rights reserved. Study was also supported by GACR 16-2179S.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Šafka Brožková, D., Paulasová Schwabová, J., Neupauerová, J. et al. HMSN Lom in 12 Czech patients, with one unusual case due to uniparental isodisomy of chromosome 8. J Hum Genet 62, 431–435 (2017). https://doi.org/10.1038/jhg.2016.148
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2016.148
This article is cited by
-
Prenatal diagnosis and genetic counseling of a uniparental isodisomy of chromosome 8 with no phenotypic abnormalities
Molecular Cytogenetics (2022)
-
Biallelic variants in the SORD gene are one of the most common causes of hereditary neuropathy among Czech patients
Scientific Reports (2021)
-
Variant c.2158-2A>G in MANBA is an important and frequent cause of hereditary hearing loss and beta-mannosidosis among the Czech and Slovak Roma population- evidence for a new ethnic-specific variant
Orphanet Journal of Rare Diseases (2020)