Abstract
Background: Recent expansion of the newborn screening panels has presented an interesting challenge to specialty care centers, especially the clinical genetics community. Some of the conditions in the core and secondary newborn screening panels have extremely variable clinical presentations; others are so rare that only a handful of newborns have been diagnosed with them to date (Region 4 Collaborative MS/MS project—http://region4genetics.org/msms_data_project/data_project_home.aspx). Definition of some disorders is problematic—does continued abnormality of the screening analyte constitute diagnosis or is further testing necessary?
Methods: A work group of the New York Mid-Atlantic Consortium for Genetic and Newborn Screening Services (region 2), one of seven regional collaboratives funded by the Federal Health Resources and Services Administration and administered by the Maternal and Child Health Bureau (U22MC03956), has developed guidelines for the confirmation of diagnosis of the conditions in the newborn screening panels for use by the specialty care centers.
Discussion: The diagnostic guidelines are a work in progress and are being reviewed and revised regularly as our understanding of the newborn screened disorders improves. The aim is to make it a relevant guide for specialty care physicians and other healthcare professionals in the diagnostic workup of these patients.
Similar content being viewed by others
Main
The expansion of newborn screening over the last decade has been one of largest changes to any public health program in the United States in recent history.1 By the end of 2009, every state newborn screening program had augmented their existing program to include tandem mass spectrometry testing (National Newborn Screening and Genetic Resource Center— http://genes-r-us.uthscsa.edu). Where previous screening was limited to 10 or fewer disorders, all states now screen for up to 29 analytes, leading to the diagnosis of more than 50 disorders. A huge investment has been made by states to develop the screening laboratories to include this technology. However, the implications of the massive increase in referrals of newborns to the clinical specialists for evaluation and diagnostic testing have not been addressed and fall on already overstretched services.
The Newborn Screening Standardization Work Group of New York Mid-Atlantic Consortium (NYMAC) was convened in August 2007 to review and advise on the standardization of newborn screening in the eight newborn screening programs (Delaware, District of Columbia, Maryland, New Jersey, New York, Pennsylvania, Virginia, and West Virginia). One of the first tasks was to examine how diagnoses for newborn-screened disorders were being confirmed. Concerns have been raised that some infants are carried with unconfirmed, incorrect, or unclear diagnoses, depending on what was included in the confirmatory evaluation. Some infants do not have access to adequate diagnostic services, primarily because of lack of insurance coverage for specific tests. Others may not be completely evaluated because of the lack of Clinical Laboratory Improvement Amendments or a state designated laboratory permitted laboratories to do the confirmatory analyses (GENETESTS: http://www.ncbi.nlm.nih.gov/sites/GeneTests/).
RATIONALE
In the regular process of newborn screening, an infant with one or more markedly abnormal metabolites on the initial screen is referred for follow-up testing to a newborn screening referral center. At the center, the infant usually undergoes clinical, nutritional, and laboratory evaluation. Infants must receive confirmatory testing to distinguish those with true disease who might require prompt medical attention from those for whom the confirmatory testing result is not indicative of disease. Problems may occur because an intermediate class of patients is identified through this diagnostic process with what are referred to as “metabolite diagnoses.” These patients continue to have mildly abnormal metabolites, but the appropriate confirmatory testing has not been initiated, completed, or is inconclusive. Metabolite diagnoses often occur in the “secondary target” group of disorders—those which are very rare and for which detailed understanding of the natural history is not available; in this group, even the experts disagree as to confirmation of a diagnosis. Unfortunately, metabolite diagnoses also occur in the core group of disorders. This is of greater concern. Patients with abnormal metabolites who remain clinically asymptomatic cause undue anxiety and costs for both caretakers and physicians when diagnostic status is not confirmed.
The NYMAC work group, consisting of clinical metabolic specialists throughout the United States (see list of participants), has developed guidelines that list the laboratory analyses necessary to confirm diagnoses based on current understanding of each disorder (http://www.wadsworth.org/newborn/nymac/docs/DX_Guidelines.pdf; scroll to the bottom of the page for diagnostic guidelines). For some conditions, repeating the newborn screening analyte, possibly in conjunction with related analytes, is sufficient, because a consistently abnormal level in these cases can be indicative of clinical disease. Examples of these conditions include congenital hypothyroidism, argininosuccinic lyase deficiency, homocystinuria, and maple syrup urine disease. In other cases, such as long-chain 3-hydroxyacyl-coA dehydrogenase deficiency, 3-methyl-crotonyl-coA-carboxylase deficiency, and short-chain acyl-CoA dehydrogenase (SCAD) deficiency, consistently abnormal analytes do not necessarily lead to a correct diagnosis without either enzyme or mutation analysis. Correct diagnosis is crucial to (1) help the parents and specialists appropriately manage the child's health; (2) determine the incidence of the disease in the US population; (3) track the clinical course of and best treatment for these conditions; and (4) to allow the newborn screening laboratories to set appropriate cut-off levels that minimize both false-positive and false-negative screening results. Setting guidelines that are acknowledged by the specialist community may encourage health insurance companies to cover the cost of these expensive tests and to increase the number of laboratories performing the tests. The New York State Medicaid program has endorsed the guidelines.2
THE NYMAC NEWBORN SCREENING DIAGNOSTIC GUIDELINES
The work group believed that a comprehensive evaluation that ends with a diagnosis is warranted for each infant. The NYMAC Newborn Screening Diagnostic Guidelines address the laboratory testing that is required for patients referred to a specialty care center to reach diagnostic confirmation. Correctly determining a diagnosis is important to whether the process of newborn screening for a particular disorder succeeds or fails. Newborn screening starts at the state, regional, or commercial screening laboratory, continues at the referral center, and ends with long-term follow-up (LTFU) of the diagnosed patients. The second and third steps are refined by the data collected at the steps before.
Thus, a correctly diagnosed patient will receive the appropriate treatment and follow-up for the specific diagnosis. A diagnosed patient enters LTFU, and clinical data are collected to benefit future patients. However, a patient given a “metabolite diagnosis” of, for example, SCAD deficiency without the recommended evaluation could actually have another diagnosis, such as isobutryl-coA dehydrogenase deficiency, or perhaps no disorder at all. Therefore, the data collected on him during LTFU would not be predictive for SCAD deficiency. A final diagnosis does not define the clinical variability of the disorder or even determine whether the disorder has clinical significance but only whether the criteria for a particular diagnosis have been met. Once the diagnosis is correctly assigned, then long-term outcome studies can determine whether mild phenotypes actually constitute disease, a metabolic abnormality, or a polymorphism of no clinical significance.
In addition, confirmed diagnoses, including metabolite diagnoses, help determine state newborn screening cut-off levels. Feedback from the specialty care referral centers is integral to the development and refinement of cut-off levels, and algorithms used by the newborn screening laboratories to decide whether particular infant samples need referral. In New York State, approximately 3% of screened samples, or approximately 8000 annually (http://www.wadsworth.org/newborn/annualrept/annsum.htm), must be repeated on a second bloodspot specimen, mostly for mildly elevated results. These repeat specimens are generally resolved as normal. For more significantly elevated results (actionable levels), the patient is sent to a referral center for formal evaluation. Currently, the positive predictive value for these results nationwide can be <10% (http://genes-r-us.uthscsa.edu). The positive predictive value can be increased when clinical diagnoses are reached appropriately, enabling cut-off levels and algorithms to be revised.3 Thus, correctly diagnosing disorders lowers the false-positive rate over time, while assuring extremely low false-negative rates, decreasing the number of infants getting clinical evaluation and tests, and the number of parents subjected to the anxiety of uncertainty. This is an ongoing process and has resulted in decreasing numbers of referrals for several acylcarnitine results in New York State.4
Another situation that is addressed with appropriate evaluation is identification of those conditions where most of the patients are clinically asymptomatic. They may have gene polymorphisms that cause mildly abnormal metabolites on follow-up testing. This includes SCAD deficiency, 3-methyl-crotonyl-coA-carboxylase deficiency, and very long-chain acyl-coA dehydrogenase deficiency. It is anticipated that this list of disorders will increase as biochemical individuality is better understood. Thus, expanded screening presents a unique opportunity to systematically evaluate all referred cases, to not only improve the understanding of these very rare disorders but also assure that future patients benefit from the screening process while avoiding needless diagnostic evaluations.
THE DIAGNOSTIC GUIDELINES: AN EXAMPLE
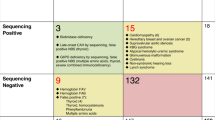
With these concerns, the members of the NYMAC Work Group developed diagnostic guidelines. For each disorder, the expected abnormal screening metabolites are listed. Then the recommended and additional tests to be done at the specialty care center are listed, followed by anticipated results that would lead to a specific diagnosis. Given the incomplete knowledge of these very rare disorders, there may be no straightforward answer as yet for what the abnormal test result should be. Hence, these are considered working guidelines to facilitate the evaluation of newborn screening referrals and to reduce the number of metabolite or “gray-zone” diagnosis. Table 1 is an example of the guidelines with an explanation of its use.
PROJECT HISTORY
To create these guidelines, a nationwide panel of metabolic experts, chosen for their body of work, was asked to collaborate on this project. Those who were available met in small groups determined by their areas of expertise and experience to debate what laboratory testing should first be required when an infant is referred with an abnormal analyte, what results would be expected for positive and negative cases, and what additional testing should be ordered to confirm the diagnosis. Depending on the disorder, the diagnosis can be confirmed by persistence of the abnormal metabolite, in the function of the gene product, identifying an enzyme defect, or finding a disease-associated mutation. These recommendations were then shared with additional experts for their concurrence.
For disorders with which there are many years of experience, a metabolite diagnosis may be acceptable for diagnostic confirmation, for example, maple syrup urine disease or propionic acidemia. However, an additional step is needed for diagnostic confirmation in most expanded newborn screening disorders. Even in phenylketonuria, the condition that has been on state screening panels for more than 45 years, biopterin synthesis defects must be ruled out.
In the table of diagnostic guidelines, additional resources are supplied, so the health provider can better understand each disorder (Mendelian Inheritance in Man—http://www.ncbi.nlm.nih.gov/sites/entrez?db=omim, and the American College of Medical Genetics (ACMG) ACTion sheets and algorithms— http://www.acmg.net/AM./Template.cfm?Section=Reference_Materials&Template=/CM/HTMLDisplay.cfm&ContentID=3669) and can find out where additional testing can be obtained (GeneTests—http://www.ncbi.nlm.nih.gov/sites/GeneTests).
The initial draft of the Guidelines were presented to the NYMAC Newborn Screening Standardization Work Group. The draft included only conditions in the core group of the ACMG panel. It quickly became apparent that it was important to expand the table to include the secondary targets because of current limited understanding of the pathophysiology of these conditions. The guidelines were initially presented nationally as a poster at the Society of Inherited Metabolic Disorders meeting in 2007. To develop consensus for diagnostic evaluations, they were distributed to metabolic specialists in the NYMAC region, followed in June 2008, by a workshop in which specialists from throughout North America discussed the specifics of each condition at the Maria Fareri Children's Hospital at Westchester Medical Center. The reviewers helped determine the efficacy of the diagnostic table and the understanding of what constitutes a confirmed diagnosis for each newborn-screened disorder. They have also been introduced to the Advisory Council of NYMAC at the 2008 Southeast NBS & Genetics Collaborative annual meeting and at the 2008 American Public Health Laboratories Newborn Screening Symposium.
FUTURE DIRECTIONS
The diagnostic guidelines are a work in progress and will be revised as the understanding of the screened disorders improves. The LTFU of the children with these disorders, including their health status and effective treatment, will guide other revisions. As more diseases are added to the newborn screening panel, guidelines will be developed for them. Similarly, LTFU data might lead to discontinuation of screening for disorders. Although the guidelines have similarities to the ACMG ACTion sheets, the goals of this endeavor are to more specifically define the diagnostic criteria for each disorder and to ensure that each infant with an abnormal newborn screen is evaluated according to expected standards. It is hoped that future activities will include review of patients diagnosed through the newborn screening process in the NYMAC region to determine whether the results satisfy the criteria outlined in the guidelines for each diagnosis.
Another future project concerns the availability of the recommended testing, especially mutation and enzyme analysis. In some cases, the appropriate analyses are not available in the US Clinical Laboratory Improvement Amendments-approved laboratories. In other cases, the patient's health insurance, whether public or private, may not cover the cost of the tests. Because these disorders are rare, confirmatory tests, when available, are done by only a few specialized laboratories that do not have contracts with the insurers. In these cases, insurance preauthorization is required and is, in many cases, denied. For many families, the laboratory charges are not affordable, and thus, without insurance coverage, the metabolite diagnosis is not confirmed. In the NYMAC region, the New York State Medicaid program is working to get the necessary laboratories into the Medicaid system, thus assuring coverage for those infants with Medicaid coverage. It has also endorsed the guidelines and will pay necessary laboratory costs for the appropriate tests.2 This could serve as a model for other state programs, and it is hoped that private insurance companies will adopt Medicaid policy, making confirmatory testing more widely available.
REFERENCES
American College of Medical Genetics: towards a uniform screening panel and system. Genet Med 2006; 8: 1s–250s.
New York State Medicaid Update, 2010. Available at: http://www.health.state.ny.us/health_care/medicaid/program/update/2010/2010-01.htm. Accessed October 22, 2010.
Schulze AS, Matern D, Hoffman GF . Newborn screening. In: Sarafogolou K, editor. Pediatric endocrinology and inborn errors of metabolism. NY: McGraw-Hill Companies, 2009: 17–32.
Change in NYS newborn screening program cut-offs, 2009. Available at: http://www.wadsworth.org/newborn/news/AMCletter.pdf. Accessed October 22, 2010.
Acknowledgements
Members of the Diagnostics Guidelines Work Group: Darius Adams, Albany Medical Center; Georgianne Arnold, University of Rochester School of Medicine; Susan Berry, University of Minnesota; Nancy Braverman, McGill University—Montreal Children's Hospital; Susan Brooks, The University of Medicine and Dentistry of New Jersey; Frank Desposito, The University of Medicine and Dentistry of New Jersey; George Diaz, Mount Sinai Medical Center; Can Ficiogliu, Children's Hospital of Philadelphia; Renata Gallagher, University of Colorado; Patricia Galvin-Parton, Stony Brook Medical Center; Cheryl Garganta, Tufts Medical Center; Micki Gartzke, Save The Babies Through Screening; Carol Greene, University of Maryland Medical Center; Katharine Harris, Wadsworth Center, NYS Department of Health; David Kronn, New York Medical College; Paul Levy, Albert Einstein School of Medicine; Jill Levy-Fisch, Save The Babies Through Screening; Uta Lichter-Konecki, Children's National Medical Center; Elizabeth Lim-Melia, New York Medical College; Nicola Longo, University of Utah Health Science Center; Madelena Martin, UMass Memorial Medical Center; Dietrich Matern, Mayo Clinic; Kate McCurdy, Barth Syndrome Foundation; Shideh Mofidi, New York Medical College; Marzia Pasquali, ARUP Laboratories; Kenneth Pass, Wadsworth Center, NYS Department of Health; Robert Rapaport, Mount Sinai School of Medicine, Rani Singh, Emory University School of Medicine; Phyllis Speiser, Schneider Children's Hospital; Valerie Stein, New York Medical College; Sharon Suchy, GeneDx; and William Wilson, University of Virginia Health System. The authors thank Harvey Levy, MD, for his critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kronn, D., Mofidi, S., Braverman, N. et al. Diagnostic guidelines for newborns who screen positive in newborn screening. Genet Med 12 (Suppl 12), S251–S255 (2010). https://doi.org/10.1097/GIM.0b013e3181fe5d8b
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181fe5d8b