Abstract
Purpose
Correction of upper eyelid ptosis is one of the most commonly performed oculoplastic procedures on the NHS but there is currently no data in the literature informing the surgeon of the optimal time for the first postoperative review. Our aim was to investigate how often a complication that warranted intervention occurred in the first 6 weeks after surgery and whether such a complication could have been predicted preoperatively.
Patients and methods
A retrospective review was performed of 300 operations in 239 patients over a 9-month period at Moorfields Eye Hospital, London. Electronic medical record software was used to extract data regarding the timing of first postoperative review, complications, any return to theatre, and any underlying risk factors or co-morbidities.
Results
At 1 week 44 % (133) cases were reviewed, 30% (89) at 2 weeks, 17% (50) at 3 weeks, and 9% (28) at 4 or more weeks. The overall complication rate at any time during the 6-week follow-up interval was 8%. The majority of these complications were minor (24 eyes, 8%) and 1 was major (0.3%). Of the 25 complications, an underlying risk factor was identified in 14 cases.
Conclusions
These data indicate that postoperative complications are very low in the absence of preoperative risk factors. In our institution, as the risk of overcorrection is low, most patients without risk factors for exposure (51% in this series) can safely be reviewed later than 1 week after surgery, but for those with risk factors earlier follow-up is warranted.
Similar content being viewed by others
Introduction
Correction of upper eyelid ptosis is one of the most commonly performed oculoplastic procedures on the NHS and usually involves surgery to the levator palpebrae superioris muscle or its aponeurosis.1 The operation may be performed under local anaesthesia (with or without sedation) or general anaesthesia, depending on the type of ptosis and age of the patient. An anterior (skin) or posterior (conjunctival) approach may be used and various techniques have been documented in the literature.2, 3, 4, 5
Overcorrection of the upper lid height carries a risk of subsequent corneal exposure and ulceration, with many junior surgeons erring on the side of undercorrection to reduce this risk. Other early postoperative complications include undercorrection, asymmetry, ectropion or entropion, lash loss, conjunctival prolapse, infection, and haemorrhage with or without visual sequelae. Traditionally, patients are reviewed 1 week following surgery, with some surgeons routinely assessing patients within 24 h, once the effects of local anaesthesia have worn off. If complications occur, they may be addressed with conservative measures (increased lubrication, manual traction, and antibiotics) or with surgery.6
There is no data in the literature informing the surgeon of the optimal time for the first postoperative review, the chief reason for seeing the patient being to identify those with significant over- or undercorrection. Opinions regarding the optimum time for the first postoperative review for uncomplicated aponeurosis-dehiscence-type ptosis vary, being between 24 h and 6 weeks, and is often based on other factors; for example, the need to remove sutures or convenience to the patient. We wished to identify evidence to support the optimum time for review given the variation in practice that exists.
Our unit therefore undertook a retrospective review of 300 consecutive patients undergoing upper lid ptosis correction to answer the following specific questions:
-
1
How often did a complication that warranted intervention occur in the first 6 weeks after surgery?
-
2
Could such complication(s) have been predicted preoperatively?
-
3
Did any patients with a functional and potentially correctable complication miss a window of opportunity for treatment by having a review later than 1 week (this often considered the optimum interval until first review)?
The purpose of this study was primarily to help inform patients regarding early complication rates specific to our institution but also to provide evidence-based rationale to guide clinicians and services organising follow-up for patients undergoing ptosis surgery.
Materials and methods
A retrospective review using the Galaxy theatre management software (iSOFT, Banbury, Oxfordshire, UK) identified 452 consecutive operations, over a 9-month period, performed in adult patients (18 years or over) at Moorfields Eye Hospital, City Road, where ‘ptosis’ was included in the description. Upper lid ptosis procedures under any form of anaesthesia (mostly local anaesthetic) were included. Any operation that was not surgery to the levator muscle or aponeurosis±blepharoplasty (for example, brow lift or lid lowering) was excluded. In all, 13 patients who did not attend their first postoperative appointment were also excluded. None of these patients attended the Moorfields Eye Casualty following their surgery, confirmed through cross-checking with the eye casualty attendances recorded in the Patient Administration System. This left 300 eyes (239 patients) for analysis.
Using the Openeyes electronic medical record software (London, UK) we extracted the following data: demographic details; operation date; grade of surgeon; type of surgery; date of first postoperative review; intraoperative and postoperative complications; postoperative management; any return to theatre; and any underlying risk factors or co-morbidities. In addition to all complications we specifically looked at major and minor exposure or height-related complications. We defined a major exposure or height-related complication as one that required immediate surgical intervention. Minor exposure or height-related complications were defined as those where conservative management was judged to be appropriate initially (for example, topical drop therapy, lid traction, and early suture removal).
Results
In all, 300 ptosis operations were performed in 239 patients with a median age of 61 years (range 18−88). A total of 286 (95%) had anterior approach and 14 (5%) had posterior approach ptosis surgery. In all, 146 eyes (49%) had a potential underlying risk factor or co-morbid condition that could have affected the postoperative outcome (Figure 1). We recorded four main risk factors: previous upper lid surgery; congenital ptosis; underlying myopathy; and previous lid injury. We also recorded a fifth group of patients with particular co-morbid conditions that could have influenced the surgical technique or intended height (Table 1).
A total of 161 (54%) operations were performed by a fellow (that is, trainees engaged in oculoplastic subspecialty training after basic training in ophthalmology), 98 (33%) were performed by a consultant, and 10 (3%) were performed by a trainee (registrar). In 31 (10%) cases, the grade of surgeon was not recorded electronically.
The immediate postoperative management in almost all cases was the application of a pressure dressing (usually two eye pads with a non-adherent dressing underneath) having instilled chloramphenicol ointment into the conjunctival sac with instructions to the patient to remove this the following day and return earlier than the planned review if any problems. One patient was reviewed within 24 h (before discharge and routine practice for that surgical team) but no change in management or surgical adjustment was recorded. Prophylactic chloramphenicol ointment (7–14 days) with or without topical lubricants (1 month) was the usual postoperative regime.
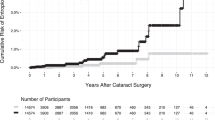
This retrospective review of follow-up data across a number of different surgical ‘firms’ identified that for the first postoperative review in clinic, 44% (133) of cases were reviewed at 1 week, 30% (89) at 2 weeks, 17% (50) at 3 weeks, and 9% (28) at 4 or more weeks (Figure 2).
Of 300 cases the overall complication rate at any time during the 6-week follow-up interval was 8%. The majority of these complications were minor (24 eyes, 8%) and 1 was major (0.3%). The minor complications were either self-limiting or resolved with simple treatments (Table 2).
Specifically looking at exposure-/height-related complications, only 1 case (0.3%) had a major complication and 15 eyes (5%) had a minor complication. The patient with the major complication had an underlying congenital levator dystrophy (with planned maximal levator resection surgery performed under general anaesthesia) and presented to eye casualty 5 days postoperatively with symptoms and signs of severe corneal exposure related to overcorrection, which required surgical intervention. In all, 15 eyes (5%) had minor complications requiring a change to medication or a change in management (Table 2). Of the three patients with mild exposure keratopathy only one case was related to overcorrection requiring lid traction.
Of the 25 complications, an underlying risk factor was identified in 14 cases: 9 eyes had had previous lid surgery; 5 were known to have an underlying myopathy; 2 had a history of prior lid injury; and 2 had congenital levator dystrophy. Thirteen of the 25 operations were performed by a consultant, 9 by a fellow, and 3 by a trainee.
Of the 15 eyes that had a minor complication related to exposure or lid height, 8 had risk factors and 7 did not. In the ‘risk factor’ group the exposure resolved with conservative treatment in 7 patients and 1 patient eventually needed lid lowering 6 months later. Of these 8 patients, 5 were seen at 1 week, 1 at 2 weeks, 1 at 3 weeks, and 1 at 4 weeks. One required punctal plugs, 7 were managed with lid traction and increased frequency of topical lubricants, and 1 patient eventually needed lid lowering. In the ‘no risk factor’ group, 6 were managed conservatively and 1 patient underwent lid lowering at 4 weeks postoperatively. Of these 7 patients, 1 was seen at 1 week, 3 at 2 weeks (including the 1 patient who went on to have lid lowering 2 weeks later), and 3 at 3 weeks (Table 3).
Discussion
The risk of (i) overcorrection and (ii) corneal exposure following ptosis surgery depends on the degree of effective retractor advancement and the underlying risk factors for corneal exposure (such as pre-existing ocular surface disease). A retrospective case series review of 272 surgeries comparing external levator advancement and Muller’s muscle-conjunctival resection for upper lid involutional ptosis had complication rates of overcorrection in 1.4%, lagophthalmos of 1 mm in 3.6%, and pyogenic granuloma in <1%. 7 It is important to point out that the aforementioned study specifically looked at involutional ptosis and therefore excluded any alternative causes of ptosis that may have led to a higher risk of complications or overcorrection. Mehta and Perry8 reported complication rates in 18% of 170 patients undergoing ptosis correction, with reoperation considered necessary in 4% of patients. This retrospective case note review examined the outcome among 170 patients undergoing 248 surgeries, whose only exclusion criteria were those with incomplete records. Data were pooled for both conjunctival mullerectomy (with or without tarsectomy) and levator advancement, and included all grades of surgeon. Peter and Khooshabeh9 conducted a retrospective case review of 300 cases of open-sky isolated Muller’s muscle resection for upper lid ptosis. This study excluded those with poor levator function and previous ptosis surgery and had a complication rate of 4% that included five corneal abrasions, two suture abscesses, four prolonged postoperative pain, and one blood cyst.
In our series, the incidence of major height-related complications was <0.5% and occurred in a patient known to be at risk. Thus, the actual likelihood of significant ocular surface complications in patients with no pre-existing risk factors is likely to be even less. Interestingly, this patient self-presented earlier than the planned 1 week review, which suggests that it is probably more important to either review such a patient within a day of surgery, or at the very least to provide readily available out of hours emergency access. The risk of a minor height-related complication in our series was 5% but the risk of an unexpected minor complication (those patients without an obvious risk factor) was 2%.
It is more difficult to determine whether patients reviewed later than 1 week (66% in this cohort) may have required temporary intervention in the first few week(s) after surgery. However, given that none attended the large and readily available Moorfields Eye Casualty before their first scheduled appointment, any undetected complications were presumably either asymptomatic or treated by the GP. A larger, comparative, prospective study looking at early vs late postoperative review would be more informative. However, of the patients in our series who developed complications, we could only identify one (with no obvious risk factor, seen at 2 weeks, and requiring lid lowering at 4 weeks) to whom this might have been relevant. One could argue that early manual lid traction or removal of sutures may have averted the need for surgery later. Even if this were the case, this remains a very minor proportion of the total series.
There are particular limitations to this study, and where conclusions are drawn, the context of this series (patient cohort and type of institution) should be borne carefully in mind. The data were collected retrospectively and the study was conducted at only one institution. Moorfields Eye Hospital is an NHS training institution with a high number of tertiary referrals, and these complex patients, with a wide range of underlying risk factors, were not excluded from the series. Thus, in this cohort, some patients may have been undercorrected, particularly given the high number of surgeries undertaken by ophthalmic trainees. However, the purpose of the study was not to determine the frequency of surgical under- or overcorrection (that is, surgical success or degree of lift was not a measured parameter) but the incidence of ocular complications and when these occur. In all cases a lift of the upper lid to within 1 mm of the corneal limbus (aiming for an effective marginal reflex distance of 4 mm) was the surgical objective. Half of our patients had underlying risk factors and it is therefore difficult to extrapolate these results to those institutions and practices where the surgical caseload is of differing complexity (ie, more or less complex). It is also not possible to extrapolate these results to those surgeons who routinely undertake posterior approach ptosis surgery, as 95% of our operations were performed using an anterior approach.
Despite the limitations described, we were able to make the following helpful observations from this study:
-
1
The risk of a major complication requiring intervention was low (<0.5%).
-
2
Within the follow-up period of 6 weeks, no major complications occurred in those without identifiable risk factors.
-
3
The risk of a minor complication was also low (5%) and was lower still (2%) in the absence of an underlying risk factor.
The timing of the first postoperative review following ptosis surgery is influenced by many factors, including patient and surgeon preferences, the need for suture removal, outpatient availability, and pre-existing risk factors for ocular surface exposure. However, with regards to the risk of exposure alone, these data indicate that postoperative complications are very low in the absence of preoperative risk factors. In a high-volume NHS training department such as ours, as the risk of overcorrection is low, this study indicates that most patients without risk factors for exposure (51% in this series) can safely be reviewed later than 1 week after surgery. For those with risk factors, earlier follow-up is warranted. In addition, for those highly experienced surgeons with a lower rate of undercorrection and a higher rate of overcorrection, early follow-up may be indicated, this depending on the audited results for a given surgeon.

References
Scoppettulol E, Chadha V, Bunce C, Olver JM, Wright M . British Oculoplastic Surgery Society (BOPSS) National Ptosis Survey. Br J Ophthalmol 2008; 92: 1134–1138.
Wobiq JL . Surgical technique for ptosis repair. Aust N Z J Ophthalmol 1989; 17 (2): 125–128.
Berlin A, Vestal K . Levator aponeurosis surgery: a retrospective review. Ophthalmology 1989; 96: 1033–1037.
Liu D . Ptosis repair by single suture aponeurotic tuck. Surgical technique and long-term results. Ophthalmology 1993; 100 (2): 251–259.
Dortzbach RK . Superior tarsal muscle resection to correct blepharoptosis. Ophthalmology 1979; 86 (10): 1883–1891.
Collin JRO . Complications of ptosis surgery and their management: a review. J R Soc Med 1979; 72: 25–26.
Ben Simon GJ, Lee S, Schwarcz RM, McCann JD, Goldberg RA . External levator advancement vs Muller’s muscle-conjunctival resection for correction of upper eyelid involutional ptosis. Am J Ophthalmol 2005; 140: 426–432.
Mehta VJ, Perry JD . Blepharoptosis repair outcomes from trainee versus experienced staff as the primary surgeon. Am J Ophthalmol 2013; 155: 397–403.
Peter NM, Khooshabeh R . Open-sky isolated subtotal Muller’s muscle resection for ptosis surgery: a review of over 300 cases and assessment of long-term outcome. Eye 2013; 27: 519–524.
Acknowledgements
We acknowledge Mr Daniel Ezra, Miss Michele Beaconsfield, Mr Jimmy Uddin, Miss Claire Daniel, Professor Geoffrey Rose, and Mr Raj Das-Bhaumik.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Porteous, A., Haridas, A., Collin, J. et al. Upper lid ptosis surgery: what is the optimal interval for the postoperative review? A retrospective review of 300 cases. Eye 32, 757–762 (2018). https://doi.org/10.1038/eye.2017.294
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.294