Abstract
Purpose
To determine the relationship between vision-related quality of life, metamorphopsia, and stereopsis after successful surgery to correct rhegmatogenous retinal detachment (RRD).
Patients and methods
Data were obtained from 30 patients with RRD who had scleral buckle surgery or vitrectomy. Age, gender, duration of blurred vision, the best-corrected visual acuity (BCVA), extent of detachment, and the location of retinal tears were measured before surgery. Approximately 1 year after surgery, stereopsis was measured with the Randot stereo test, visual acuity (VA) was measured using a Snell VA acuity measurement at a distance of 5 m and was presented as a linear LogMAR value, metamorphopsia was examined using an M-chart, and vision-related quality of life was determined using the 25-Item National Eye Institute Visual Function Questionnaire (VFQ-25).
Results
All of the patients achieved anatomical retinal reattachment. There was a significant difference between preoperative BCVA (0.78±0.72) and BCVA 1 year postoperatively (0.25±0.25) (P<0.05). Twenty-three patients had visual distortion postoperatively, including vertical metamorphopsia (0.53±0.52°), and horizontal metamorphopsia (0.48±0.53°). Twenty patients had no stereopsis. The composite score of VFQ-25 was 76.60 postoperatively. Significant differences in postoperative BCVA, metamorphopsia, and VFQ-25 were found between macula-on and macula-off groups (all P<0.05). There was a negative correlation between VFQ-25 composite score and metamorphopsia (P<0.005); there was no significant correlation between VFQ-25 composite score and BCVA or stereopsis.
Conclusion
Vision-related quality of life correlated with metamorphopsia, but did not correlate with VA or stereopsis.
Similar content being viewed by others
Introduction
Rhegmatogenous retinal detachment (RRD) is a common type of retinal detachment, that is, a detachment of the neurosensory retina from the underlying retinal pigment epithelium owing to a defect in the retina.1 Improvements in surgical techniques have resulted in an increased anatomical success rate; however, functional recovery is often compromised and some patients are not satisfied with the quality of life after surgery.2, 3 In macula-off RRD, visual distortion is a major complaint and postoperative metamorphopsia is a highly prevalent problem that occurs in around two-thirds of patients.4, 5 M-Chart is a convenient and reliable method to evaluate metamorphopsia, and it has been used to assess the degree of visual distortion for macular pucker and macular holes in previous studies.6, 7
Vision-related quality of life issues include walking difficulties, social distress, and inconvenience of daily living.8 The 25-Item National Eye Institute Visual Function Questionnaire (VFQ-25) was developed by the National Eye Institute and is widely used to assess patients’ perception of visual function and quality of life.8 In the present study we used VFQ-25, M-Chart, and the Randot stereo test to determine the relationships between vision-related quality of life, metamorphopsia, and stereopsis of patients who had successful surgery to correct RRD.
Patients and methods
Thirty patients (30 eyes) with RRD, who were treated from January, 2008 to November, 2009 were included in this prospective and non-randomized clinical trial. The study included patients with spontaneous, uncomplicated, recent onset RRD who underwent scleral buckling or vitrectomy surgery. Patients were excluded from the study if they had traumatic retinal detachment, recurring retinal detachment, proliferative vitreoretinopathy with a grade greater than B-level, macular disorders, vitreous hemorrhages, amblyopia, high refractive errors, severe cataracts, duration lasting longer than one month, and postoperative follow-up <1 year.
All of the patients were evaluated by at least two physicians before surgery. Stereopsis, metamorphopsia, and VFQ-25 were assessed, respectively, by masked physicians after surgery. Preoperative best-corrected visual acuity (BCVA) was measured using the Snell visual acuity (VA) measurement, which was converted into a linear logMAR value. Approximations for VA worse than 20/400 were made as follows: counter finger is 20/2000 (logMAR value=2.0), hand motion is 20/4000 (logMAR value=2.3), and light perception is 20/8000 (logMAR value=2.6).8 Examinations were made with a slit-lamp and binocular indirect ophthalmoscope with scleral depression, if necessary. The course of the disease was measured from the time that the patient noticed blurred vision. Optical coherence tomography was used to evaluate the macular structure pre- and postoperatively.
Surgeries were performed by an experienced surgeon. The postoperative follow-up period was at least 1 year. Final BCVA was measured postoperatively as described above for preoperative measurements.
In previous studies, the severity of metamorphopsia was estimated using an Amsler chart.9 However, it is difficult to achieve precise and reproducible assessments of metamorphopsia using the Amsler chart because patients have to self-describe the extent and degree of image distortion. Therefore, an M-Chart (Inami Co., Tokyo, Japan) was used to quantitate metamorphoses. An M-Chart consists of 19 dotted lines with dot intervals ranging from 0.2 degrees to 2.0 degrees of visual angle. If the straight line is substituted with a dotted line, and the dot interval is changed from fine to coarse, the distortion of the line decreases with the increasing dot interval until the dotted line appears straight. The examination was performed at 30 cm so that the refraction of the eye was exactly corrected for this distance. At first, vertical straight lines (0 degrees) were shown to the patient. If the patient recognized the straight line as straight, the metamorphopsia score was 0. If the patient recognized the straight line as irregular or curved, then subsequent pages of M-Chart, in which the dot intervals of the dotted line change from fine to coarse, were shown subsequently. When the patient recognized a dotted line as being straight, the visual angle that separated the dots was considered to represent his/her metamorphopsia score for the vertical line. The M-Chart was also rotated 90 degrees and the same test was performed using horizontal lines. The examinations were repeated three times for each subject to evaluate the reproducibility of the test, and their mean was used for data analyses.10
Stereopsis was measured with the Randot stereo test (Stereo Optical Co, Inc., Chicago, IL, USA) at 30 cm, and the refraction of the eye was exactly corrected for this distance. Vision-related quality of life was assessed by VFQ-25.11 The VFQ-25 included questions related to general health status and questions related to 11 objective and vision-related parameters, including general vision, ocular pain, near activities, distance activities, social functioning, mental health, role difficulties, dependency, driving, color vision, and peripheral vision. Patients chose from four scores, 100, 75, 50, and 25, for each VFQ-25 parameter according to the severity of the quality of life issue. A higher VFQ-25 score corresponded to a higher quality of life. Overall questionnaire scores were the average of 11-dimensional objective scores, excluding the questions on general health. The VFQ-25 was completed before other examinations. The research staff explained the questionnaire to the patients, gave instructions verbally, and provided assistance when required. The completed questionnaires were reviewed for missing data by the research staff.
Statistics
BCVA, metamorphopsia, and VFQ-25 were compared between scleral buckling and vitrectomy groups, and between macula-on and macula-off groups. Data were analyzed by a non-parametric test using SPSS Program Package 16.0 for Windows. Data were identified as significant at a level of P≤0.05. The Wilcoxon-paired comparison rank sum test was used to test the significance of preoperative and postoperative VA data. Spearman rank correlation analysis was used to test the correlation of BCVA, visual distortion degree, and overall score. The data were divided into two groups on the basis of the stereopsis, and the Mann–Whitney U-test was used to compare stereopsis to the quality of life.
Results
The results presented are for cases in which retinal reattachment was achieved. Patients with recurrent retinal detachment were excluded. The number of excluded patients was not recorded. Pre- and postoperative characteristics of RRD patients are shown in Table 1 (scleral buckling vs vitrectomy) and Table 2 (macula-on vs macula-off). There was no significant difference in BCVA, metamorphopsia, and VFQ-25 between the scleral buckling group and vitrectomy group (all P>0.05). Significant differences in postoperative BCVA, metamorphopsia, and VFQ-25 were found between the macula-on group and macula-off group (all P<0.05).
Postoperative visual function and vision-related quality of life
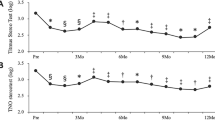
The preoperative BCVA was 0.78±0.72, and after 1 year of follow-up, the BCVA was 0.25±0.25 (P<0.001). Twenty-three patients had visual distortion (metamorphopsia), 17 of them had macula-off RRD before surgery, and submacular fluid was found by optical coherence tomography in 15 of the 23 patients 1 year after surgery. The average vertical metamorphopsia score was 0.53±0.52°, whereas the average horizontal metamorphopsia score was 0.48±0.53°. The reliability of M-chart to evaluate metamorphopsia was excellent (intraclass correlation coefficient: 0.985 in vertical metamorphopsia and 0.998 in horizontal metamorphopsia). Twenty patients had no stereopsis.
Correlation between postoperative vision-related quality of life and visual function
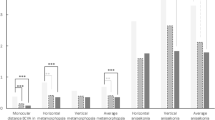
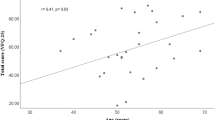
The average VFQ-25 scores postoperatively are listed in Table 3. The VFQ-25 scores and postoperative BCVA were not statistically correlated (P>0.05). In addition, there was a negative correlation between the composite VFQ-25 quality of life score and vertical metamorphopsia and horizontal metamorphopsia (P≤0.005) (Figure 1,Table 4). Patients were divided into two groups according to stereoscopic vision. However, there was no statistically significant correlation between the composite VFQ-25 score and stereoscopic vision (P>0.05).
Discussion
Postoperative VA, metamorphopsia, and stereopsis
Some studies suggested that scleral buckling and vitrectomy surgery, which anatomically corrects RRD, do not restore visual function, as measured by VA.12, 13, 14 In our study, after scleral buckling or vitrectomy to correct RRD, postoperative VA improved significantly compared with preoperative VA in agreement with previous studies.14, 15, 16 Scholars suggested that preoperative VA was the key to determine postoperative visual recovery.16 Although VA improved after surgery in this study, it was not restored to the level of the contralateral eye. Animal models of retinal detachment showed that after a half an hour of detachment, vision loss was irreversible, and photoreceptor cells underwent apoptosis after a few days.17 Apoptosis might explain why some patients did not have ideal VA even when the surgery was performed on the same day as RRD.
Metamorphopsia is a visual illusion of object size, shape, and tilt distortion.18 Patients with retinal detachment had different degrees of visual distortions.19 In one study, 67% of the patients had visual distortion after macula-off RRD surgery.5 In our study, metamorphopsia was the most common symptom in patients with submacular fluid. Although ophthalmoscope observation after RRD surgery showed a flattened retina, the optical coherence tomography scan still revealed a shallow foveal detachment and abnormally rough neural epithelium. Even after successful retinal reattachment, macular optical coherence tomography scans showed that some patients still had subretinal fluid, macular edema, macular thickening, or epiretinal membranes, which could be the reason for visual distortion after scleral buckling or vitrectomy to correct RRD.19, 20, 21, 22, 23 The present study indicated that the abnormal macular structure and subretinal fluid might influence the severity of postoperative metamorphopsia.
There has been only one study that measured binocular three-dimensional stereoscopic vision in relation to surgery to correct RRD.14 The authors suggested that following RRD surgery, subfoveal fluid, and macular edema, as well as a decline in perception, lead to a decline in binocular stereoscopic vision.14 In our study, 10 patients had stereopsis after surgery, 5 of them had macula-off RRD, and 4 of them had postoperative submacular fluid.
We found no significant difference in BCVA, metamorphopsia, and VFQ-25 between the scleral buckling group and vitrectomy group, indicating that the two techniques to treat RRD might have similar effects on the recovery of macular structure and inflammatory responses. The macula-on group had better pre- and postoperative BCVA, less-severe metamorphopsia and a higher VFQ score than the macula-off group indicating that preoperative macular status was an important factor that affects the outcome and visual function after RRD surgery.
Assessment of vision-related quality of life and the relevance of visual distortion and stereopsis
In our study, the overall average VFQ-25 score was 76.60, slightly less than previously reported (80.03).8 We found that the quality of life scores and postoperative BCVA had no correlation, which was in agreement with a previous study.8 In addition, most patients stated that their weaknesses did not affect the quality of life, possibly because of the compensation by the contralateral eye.
Visual distortion reflects visual quality and is an indicator of visual function. It can damage the patients’ feeling of well-being, and the patients may have positioning and reading difficulties after scleral buckling.24 Our results indicated that metamorphopsia had a key role in the deterioration of vision-related quality of life, which correlated with the severity of postoperative visual distortion.
It has been reported that postoperative stereo acuity declines in the majority of patients, but it does not affect the visual quality of life postoperatively.25 Stereoscopic depth is a more precise determination of space; however, there can be some monocular stereoscopic vision. Life experiences and common sense may contribute to stereopsis. Long adaptation can accommodate the patient’s monocular stereopsis. This might explain why the studies showed no correlation between stereopsis and postoperative quality of life.
There are some limitations in this study. The first one was the lack of information on the binocular state and ocular dominance of our patients before the development of RRD mainly because most Chinese never have an eye examination unless their vision is significantly impaired. Although all of the patients in this study reported that their vision was ‘normal’ prior to the retinal detachment, it would be better to have a stereopsis or binocular vision test done before this condition occurred. A second limitation was that some factors like surgery techniques, buckle designs, tear locations, and preoperative macular status could affect the severity of postoperative metamorphopsia. Future studies are needed to investigate how and if these factors influence metamorphopsia and the quality of life. The main purpose of this study was to focus on the evaluation of existing postoperative metamorphopsia and the correlation between metamorphopsia and quality of life.
In summary, RRD can cause metamorphopsia and further affect a patient’s quality of life. Patients with macula-on RRD had better pre- and postoperative BCVA, less-severe metamorphopsia and a higher VFQ-25 score than patients with macula-off RRD. No significant difference in BCVA, metamorphopsia, and VFQ-25 was found between patients with scleral buckling and vitrectomy surgeries. Improvement in postoperative VA and a decline in stereopsis did not affect the patients’ quality of life, whereas the degree of postoperative visual distortion were negatively correlated with the patients’ quality of life after surgery.

References
D’Amico DJ . Clinical practice primary retinal detachment. N Engl J Med 2008; 359 (22): 2346–2354.
Mitry D, Awan MA, Borooah S, Syrogiannis A, Lim-Fat C, Campbell H et al. Long-term visual acuity and the duration of macular detachment: findings from a prospective population-based study. Br J Ophthalmol 2013; 97 (2): 149–152.
Diederen RM, La Heij EC, Kessels AG, Goezinne F, Liem AT, Hendrikse F . Scleral buckling surgery after macula-off retinal detachment: worse visual outcome after more than 6 days. Ophthalmology 2007; 114 (4): 705–709.
Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T . Metamorphopsia and optical coherence tomography findings after rhegmatogenous retinal detachment surgery. Am J Ophthalmol 2013; 157 (1): 214–220.
Wang Y, Li SY, Zhu M, Chen SJ, Liu Y, Men XH et al. Metamorphopsia after successful retinal detachment surgery: an optical coherence tomography study. Acta Ophthalmol Scand 2005; 83 (2): 168–171.
Matsumoto C, Arimura E, Okuyama S, Takada S, Hashimoto S, Shimomura Y . Quantification of metamorphopsia in patients with epiretinal membranes. Invest Ophthalmol Vis Sci 2003; 44 (9): 4012–4016.
Arimura E, Matsumoto C, Okuyama S, Takada S, Hashimoto S, Shimomura Y . Quantification of metamorphopsia in a macular hole patient using M-CHARTS. Acta Ophthalmol Scand 2007; 85 (1): 55–59.
Okamoto F, Okamoto Y, Fukuda S, Hiraoka T, Oshika T . Vision-related quality of life and visual function following vitrectomy for proliferative diabetic retinopathy. Am J Ophthalmol 2008; 145 (6): 1031–1036.
Crossland M, Rubin G . The Amsler chart: absence of evidence is not evidence of absence. Br J Ophthalmol 2007; 91 (3): 391–393.
Okamoto F, Okamoto Y, Fukuda S, Hiraoka T, Oshika T . Vision-related quality of life and visual function after vitrectomy for various vitreoretinal disorders. Invest Ophthalmol Vis Sci 2010; 51 (2): 744–751.
Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD . Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol 2001; 119 (7): 1050–1058.
Schwartz SG, Kuhl DP, McPherson AR, Holz ER, Mieler WF . Twenty-year follow-up for scleral buckling. Arch Ophthalmol 2002; 120 (3): 325–329.
Heimann H, Zou X, Jandeck C, Kellner U, Bechrakis NE, Kreusel KM et al. Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol 2006; 244 (1): 69–78.
Ozgur S, Esgin H . Macular function of successfully repaired macula-off retinal detachments. Retina 2007; 27 (3): 358–364.
Burton TC . Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc 1982; 80: 475–497.
Lecleire-Collet A, Muraine M, Menard JF, Brasseur G . Predictive visual outcome after macula-off retinal detachment surgery using optical coherence tomography. Retina 2005; 25 (1): 44–53.
Faude F, Francke M, Makarov F, Schuck J, Gärtner U, Reichelt W et al. Experimental retinal detachment causes widespread and multilayered degeneration in rabbit retina. J Neurocytol 2001; 30 (5): 379–390.
River Y, Ben HT, Steiner I . Reversal of vision metamorphopsia: clinical and anatomical characteristics. Arch Neurol 1998; 55 (10): 1362–1368.
Wolfensberger TJ, Gonvers M . Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol 2002; 240 (2): 85–89.
Hagimura N, Iida T, Suto K, Kishi S . Persistent foveal retinal detachment after successful rhegmatogenous retinal detachment surgery. Am J Ophthalmol 2002; 133 (4): 516–520.
Gibran SK, Alwitry A, Cleary PE . Foveal detachment after successful retinal reattachment for macula on rhegmatogeneous retinal detachment: an ocular coherence tomography evaluation. Eye (Lond) 2006; 20 (11): 1284–1287.
Baba T, Hirose A, Moriyama M, Mochizuki M . Tomographic image and visual recovery of acute macula-off rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol 2004; 242 (7): 576–581.
Tranos PG, Ghazi-Nouri SM, Rubin GS, Adams ZC, Charteris DG . Visual function and subjective perception of visual ability after macular hole surgery. Am J Ophthalmol 2004; 138 (6): 995–1002.
Ugarte M, Williamson TH . Horizontal and vertical micropsia following macula-off rhegmatogenous retinal-detachment surgical repair. Graefes Arch Clin Exp Ophthalmol 2006; 244 (11): 1545–1548.
Lennerstrand G, Ahlstrom CO . Contrast sensitivity in macular degeneration and the relation to subjective visual impairment. Acta Ophthalmol (Copenh) 1989; 67 (3): 225–233.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lina, G., Xuemin, Q., Qinmei, W. et al. Vision-related quality of life, metamorphopsia, and stereopsis after successful surgery for rhegmatogenous retinal detachment. Eye 30, 40–45 (2016). https://doi.org/10.1038/eye.2015.171
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.171
This article is cited by
-
Retinal detachment
Nature Reviews Disease Primers (2024)
-
Patient-reported outcome measures in vitreoretinal surgery: a systematic review
Eye (2023)
-
Changes in metamorphopsia following intravitreal aflibercept injection for diabetic macular edema
Scientific Reports (2022)
-
Relationship between stereopsis and vision-related quality of life following intravitreal ranibizumab injections for central retinal vein occlusion
Scientific Reports (2021)
-
Stress and vision-related quality of life in acute and chronic central serous chorioretinopathy
BMC Ophthalmology (2020)