Abstract
Background
Conjunctival intra-epithelial neoplasia (CIN) typically occurs in elderly individuals. A number of aetiological factors are implicated in CIN, including life-long exposure to ultra-violet light and immunodeficiency states, particularly HIV infection. Asthma is a common condition affecting more than 3.5 million individuals in the UK, and is associated with atopy in approximately 70% of cases. In this paper we describe CIN occurring in young patients with asthma.
Methods
Retrospective case series: A review of our ocular oncology database helped to identify 11 patients <55 years of age and presenting with CIN. Of these, seven (64%) were noted to have co-existent asthma.
Results
Seven patients were included in the study (six male and one female). Mean age at presentation was 44 years (range 36–54 years). Five patients showed unilateral disease, whereas two showed bilateral. Five patients showed local recurrence; however, there were no cases of metastasis.
Conclusion
The occurrence of CIN, particularly bilateral CIN, in younger immunocompetent individuals is very unusual, and the presence of asthma in 64% of our patient cohort suggests that atopic asthma may be a further aetiological factor involved in the development of this rare neoplasm.
Similar content being viewed by others
Introduction
The term conjunctival intra-epithelial neoplasia (CIN) encompasses a range of squamous dysplasias of the conjunctival epithelium with no invasion of the basement membrane. It may be graded in severity from mild to severe or carcinoma in situ. The term ocular surface squamous neoplasia (OSSN) includes both pre-invasive disease (CIN) and invasive disease (squamous carcinoma). OSSN is rare in temperate climates,1 but increases in frequency at places closer to the equator.2 Lifelong exposure to ultraviolet light is therefore considered to be the major aetiological factor in the development of OSSN. However, a number of other factors have also been implicated, including immunodeficiency states such as HIV3 and iatrogenic immunosuppression post-organ transplantation,4 human papilloma virus (HPV) infection,5 as well as atopic eczema.6 OSSN typically affects elderly individuals with a mean age in excess of 60 years.7 In this paper, we describe an apparent association between asthma and CIN occurring in young and middle-aged adults.
Materials and methods
Between 1998 and 2008, 11 patients aged <55 years were seen at the ocular oncology clinic in Sheffield with a diagnosis of CIN. Of these, three were from sub-Saharan Africa, one was HIV positive and a further seven patients suffered from asthma. We retrospectively reviewed the records of this cohort of asthmatic patients, documenting their age, gender, laterality, treatments, and clinical outcomes.
Results
Seven patients were included in the study, six male and one female. Mean age at presentation was 43 years (range 36–54 years). Mean follow-up was for 38 months (range 6–120 months). Five patients exhibited unilateral disease, whereas two were bilateral cases. None of the patients gave a history of excessive UV exposure; however, two patients (patients 6 and 7) had co-existent eczema. Further clinical details are described in Table 1. The case of one patient (patient 5) is described in detail.
Patient 5
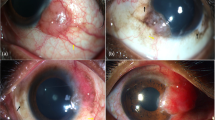
A 39-year-old man was referred in January 2008 with a leukoplakic lesion of the inferior bulbar conjunctiva of the right eye (Figure 1a). Excision biopsy with adjuvant cryotherapy revealed CIN amounting to in-situ squamous carcinoma (Figure 1b) with areas of conjunctival eosinophilia (Figure 1c). He was subsequently treated with four 1-week cycles of topical mitomycin C (MMC) 0.02% q.i.d. Further conjunctival map biopsies in September 2008 showed no residual disease in the right eye; however, a new lesion was noted in the left eye and excision biopsy (with adjuvant cryotherapy) confirmed CIN. He therefore received a further four cycles of MMC 0.02% in the left eye. Following this treatment, further conjunctival map biopsies demonstrated no residual disease; however, in March 2009 he developed a recurrence in the right eye, which was treated with topical interferon.
(a) Slit-lamp photograph of the right eye of patient 5 showing a leukoplakic lesion of the bulbar conjunctiva. (b) Haematoxylin and eosin-stained section of conjunctiva showing full-thickness squamous epithelial dysplasia, amounting to in-situ squamous carcinoma. The arrow points to a highly atypical squamous epithelial cell in the epithelium. (c) Haematoxylin and eosin-stained section of the dysplastic epithelium shown in (b), but at a higher power. The arrows indicate eosinophils within the dysplastic epithelium, which is indicative of atopic status.
Conclusion
CIN is a rare condition, which in temperate climates shows an incidence of 0.03 per 100 000 population,1 increasing towards the equator, such that the incidence in Australia has been reported at 19 per 100 000.2 Life-long exposure to ultraviolet light therefore appears to be the major risk factor in the development of CIN. The disease typically affects elderly individuals (mean age of presentation >60 years),7 although the incidence in younger patients appears to be increasing in association with immunodeficiency states, particularly HIV infection3 and iatrogenic immunosuppression following solid organ transplantation.4 The role of HPV in the development of CIN is debatable,5 with some authors suggesting that HPV alone, in the absence of other aetiological factors, may be incapable of causing CIN. A single study has reported CIN in association with atopic eczema,6 and two of our seven patients also suffered from eczema. CIN is generally a unilateral condition, although bilateral cases have rarely been described.8 Various treatment options are available, including local excision with or without adjuvant cryotherapy, topical chemotherapy with a number of agents, mainly MMC, Interferon, or 5-fluorouracil, and radiotherapy techniques such as plaque brachytherapy.5 Although local recurrence is relatively common, metastasis should not occur in the absence of invasive disease.9 The patients described in this study are very unusual in that not only were they relatively young and immunocompetent, they also presented with aggressive disease that was bilateral in two cases and recurrent in five.
Asthma is a common condition affecting more than 3.5 million adults and children in the United Kingdom,10 and is associated with atopy in approximately 70% of cases,11 which is characterised by elevated IgE levels in response to allergen presentation. The production of IgE is partly mediated by type-2 helper T lymphocytes (Th2 cells), and asthmatics (and other atopes) tend to show an exaggerated type-2 response following antigen exposure. Whereas type-2 responses predominate in neonates, they tend to decline in normal adults in favour of type-1 responses, supporting cell-mediated immunity that is particularly active against virus-infected and neoplastic cells.12 This immune switch does not occur in atopes. In this series, 60% (three out of five) of the patients tested for HPV infection were found to be positive. Two of the patients so tested were found not to express HPV; however, this does not exclude HPV infection, as it can be difficult to detect HPV following incorporation of the viral DNA into the host genome. Could it be that the relative deficiency of type-1 responses in asthmatics allows conjunctival neoplasia to develop, possibly mediated through HPV expression (as detected in 60% of our patients whom we were able to test for HPV infection)?
In conclusion, we report an apparent association between asthma and CIN arising in young and middle-aged adults. Of course it may be that with such a small cohort of patients this apparent association is merely coincidental; however, the severity of disease in our patients leads us to believe otherwise. We feel that this study supports the role of atopy in the development of CIN and that clinicians should be aware that CIN occurring in association with asthma may occur at a younger age than normally expected and be more aggressive in nature.

References
Sun EC, Fears TR, Goedert JJ . Epidemiology of squamous cell conjunctival cancer. Cancer Epidemiol Biomarkers Prev 1997; 6 (2): 73–77.
Lee GA, Hirst LW . Incidence of ocular surface epithelial dysplasia in metropolitan Brisbane: a 10-year survey. Arch Ophthalmol 1992; 110 (4): 525–527.
Ateenyi-Agaba C . Conjunctival squamous cell carcinoma associated with HIV infection in Kampala, Uganda. Lancet 1995; 345 (8951): 695–696.
Shelil AE, Shields CL, Shields JA, Eagle RC . Aggressive conjunctival squamous cell carcinoma in a patient following liver transplantation. Arch Ophthalmol 2003; 121 (2): 280–282.
Pe'er J . Ocular surface squamous neoplasia. In: Singh AD, Damato BE, Pe'er J, Linn Murphree A, Perry JD (eds). Clinical Ophthalmic Oncology. Saunders Elsevier: Philadelphia, 2007 pp 139–140.
Heinz C, Fanihagh F, Steuhl K-P . Squamous cell carcinoma of the conjunctiva in patients with atopic eczema. Cornea 2003; 22 (2): 135–137.
Lee GA, Hirst LW . Retrospective study of ocular surface squamous neoplasia. Aust NZJ Ophthalmol 1997; 25 (4): 269–276.
Cervantes G, Rodriguez Jr AA, Leal AG . Squamous cell carcinoma of the conjunctiva: clinicopathological features in 287 cases. Can J Ophthalmol 2002; 37: 14–19.
Erie JC, Campbell RJ, Liesegang TJ . Conjunctival and corneal intraepithelial and invasive neoplasia. Ophthalmology 1986; 93 (2): 176–183.
Ying S, Zhang G, Gu S, Zhao J . How much do we know about atopic asthma: where are we now? Cell Mol Immunol 2006; 3 (5): 321–332.
Humbert M, Menz G, Ying S, Corrigan CJ, Robinson DS, Durham SR et al. The immunopathology of extrinsic (atopic) and intrinsic (non-atopic) asthma: more similarities than differences. Immunol Today 1999; 20: 528–533.
Donovan CE, Finn PW . Immune mechanisms of childhood asthma. Thorax 1999; 54: 938–946.
Acknowledgements
We thank Mr Andrew Bailey at the Manchester Medical Microbiology Partnership for assessing HPV status in our patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rundle, P., Mudhar, H. & Rennie, I. Conjunctival intra-epithelial neoplasia occurring in young patients with asthma. Eye 24, 1182–1185 (2010). https://doi.org/10.1038/eye.2009.296
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.296
Keywords
This article is cited by
-
Human papillomavirus type 16 causes a defined subset of conjunctival in situ squamous cell carcinomas
Modern Pathology (2020)
-
A prospective study of the incidence, associations and outcomes of ocular surface squamous neoplasia in the United Kingdom
Eye (2019)
-
Clinical Management of Ocular Surface Squamous Neoplasia: A Review of the Current Evidence
Ophthalmology and Therapy (2018)
-
Ocular surface squamous neoplasia in an immunosuppressed patient with atopic keratoconjunctivitis
International Ophthalmology (2012)