Abstract
To test the feasibility of using the survivin promoter to induce specific expression of sodium/iodide symporter (NIS) in cancer cell lines and tumors for targeted use of radionuclide therapy, a recombinant adenovirus, Ad-SUR-NIS, that expressed the NIS gene under control of the survivin promoter was constructed. Ad-SUR-NIS mediating iodide uptake and cytotoxicity was performed in vitro. Scintigraphic, biodistribution and radioiodine therapy studies were performed in vivo. PC-3 (prostate); HepG2 (hepatoma) and A375 (melanoma) cancer cells all exhibited perchlorate-sensitive iodide uptake after infection with Ad-SUR-NIS, ∼50 times higher than that of negative control Ad-CMV-GFP-infected cells. No significant iodide uptake was observed in normal human dental pulp fibroblast (DPF) cells after infection with Ad-SUR-NIS. Clonogenic assays demonstrated that Ad-SUR-NIS-infected cancer cells were selectively killed by exposure to 131I. Ad-SUR-NIS-infected tumors show significant radioiodine accumulation (13.3±2.85% ID per g at 2 h post-injection), and the effective half-life was 3.1 h. Moreover, infection with Ad-SUR-NIS in combination with 131I suppressed tumor growth. These results indicate that expression of NIS under control of the survivin promoter can likely be used to achieve cancer-specific expression of NIS in many types of cancers. In combination with radioiodine therapy, this strategy is a possible method of cancer gene therapy.
Similar content being viewed by others
Introduction
The sodium/iodide symporter (NIS), an intrinsic membrane glycoprotein with 13 putative transmembrane domains, has an important role in the biosynthesis of thyroid hormones by mediating the active transport of iodide into thyrocytes.1, 2, 3 NIS is critical for the diagnosis and therapeutic management of thyroid diseases, including thyroid carcinoma. Cloning of the rat and human NIS genes in 1996 and extensive characterization of these genes have paved the way to novel radionuclide gene therapy strategies.1, 4 Through targeted transfer and expression of the NIS gene, radioiodine treatment could be used to treat non-thyroid malignant disease in addition to thyroid carcinoma.
Tumor-specific expression of the NIS gene has been performed with promising results in a variety of tumors, including prostate carcinoma,5, 6, 7, 8, 9 hepatocellular carcinoma,9, 10, 11, 12 medullary thyroid carcinoma,13 colon cancer,14 breast cancer15 and neuroendocrine tumors.16 For example, prostate tumors were successfully treated in vivo with systemic administration of 131I, 188Re and 211At following selective expression of NIS under control of the prostate specific antigen promoter. Although previous studies have been promising, the use of such tissue-specific promoters has a limited scope. Therefore, the identification of a more general tumor-specific promoter to regulate NIS expression could be useful for expanding this strategy for treatment of a wide variety of tumors.
Survivin, a member of the inhibitor of apoptosis gene family, is usually expressed in the embryonic lung and fetal organs in the developmental stages but undetectable in normal adult tissues other than the thymus, placenta, CD34+ stem cells and basal colonic epithelial cells.17, 18, 19, 20, 21 However, survivin seems to be selectively expressed in transformed cells and in most human cancers, including lung, breast, pancreatic and colon carcinomas, soft tissue sarcomas, brain tumors, melanoma, neuroblastoma and hematologic malignancies.22 Clinical studies have indicated a positive correlation between high survivin expression levels and poor prognosis, accelerated rate of recurrence and increased resistance to therapy in many cancer patients.23 Previous studies have identified a putative region of the survivin promoter that is likely responsible for the induction of specific, high-level expression in tumors.24, 25 The survivin promoter contains multiple cell cycle-dependent elements and a cell cycle gene homology region. This region has been suggested to control expression of various G2-M-regulated genes, including the survivin gene, in a manner correlating with G2-M cell cycle periodicity.24
In this study, we have developed a tumor-targeting adenovirus that expresses the NIS gene under control of the survivin promoter. We investigated the utility of this system for molecular imaging and radioiodine gene therapy. The results reported herein demonstrate the potential efficacy and selectivity of a combination of radioiodine therapy and adenovirus-mediated expression of the NIS gene under the control of the survivin promoter for cancer therapy.
Materials and methods
Cell lines
The human prostate cancer cell line, PC-3; the human hepatocellular carcinoma cell line, HepG2; the human melanoma cell line, A375 and the adenoviral transformed human embryonic kidney cell line, 293, were purchased from the American Type Culture Collection (ATCC, Rockville, MD). All cancer cell lines were cultured in RPMI 1640 medium supplemented with 10% calf serum (Gibco, Carlsbad, CA), 2 mM glutamine, 100 IU ml–1 penicillin and 100 ng ml–1 streptomycin. Cells were maintained at 37 °C in a humidified atmosphere containing 5% CO2. Both 293 cells and a control human dental pulp fibroblast cell line (DPF; a kind gift from Dr Peng Li, West China College of Stomatology, Sichuan University) were cultured in Dulbecco's Modified Eagle Medium (high glucose) medium supplemented with 10% FBS and 100 IU ml–1 penicillin/streptomycin (100 ng ml–1).
Construction of plasmids and recombinant adenovirus
In order to generate the luciferase expression plasmid under the control of the survivin promoter (pSUR-LUC), an ∼260 bp fragment of the human survivin gene promoter (∼222 to +39, GeneBank Accession Number AY795969) was amplified from PC-3 genomic DNA by PCR. This region contains two cell cycle-dependent elements and one cell cycle gene homology region. The sequences of the oligonucleotide primers were as follows: forward primer, 5′-AGATCTGCACGCGTTCTTTGAAAGC-3′, and reverse primer, 5′-AAGCTTCCACCTCTGCCAACGGGTC-3, which allowed for the introduction of BglII and HindIII sites (underlined in the respective sequences). The survivin promoter was T/A cloned into the PMD-T18 vector for sequencing, and then subcloned using the BglII and HindIII sites into the luciferase vector pGL3-basic (Promega, Madison, WI) to generate pSUR-Luc (Figure 1a).
Structures of plasmids used in this study. (a) Diagram represents the structure of the luciferase reporter plasmid. The survivin promoter (−222 to 39 bp) was cloned upstream of the luciferase gene using the restriction sites indicated. (b) Diagram represents the structure of the adenovirus shuttle plasmid pS-SUR-NIS. The plasmid was constructed by inserting a DNA fragment into the E1-deleted region using the KpnI/SalI restriction sites. This DNA fragment contained the survivin promoter, the full length NIS cDNA, and the Simian Virus 40 polyadenylation signal.
In order to generate the NIS constructs, the coding region of NIS was amplified from normal human thyroid tissue by RT–PCR (nucleotides 348 to 2280, GeneBank Accession Number, NM_000453), followed by T/A cloning into the PMD-T18 vector for sequencing. The sequences of the oligonucleotide primers were as follows: forward primer, 5′-CCCAAGCTTATGGAGGCCGTGGAGACCGGGGAAC-3′, and reverse primer, 5′-GCGTCTAGATCAGAGGTTTGTCTCCTGCTG-3′, which allowed for the introduction of HindIII and XbaI sites (underlined in the respective sequences). The luciferase gene of pSUR-Luc was replaced with hNIS by subcloning into the HindIII and XbaI sites. The survivin promoter-hNIS-SV40 polyA cassette was then isolated by digestion with KpnI and SalI and cloned into the pShuttle-1 vector (Stratagene, Cedar Creek, MD) to generate pS-SUR-NIS (Figure 1b). Subsequently, homologous recombination was performed using the Adeasier system (Stratagene) in BJ5183 Escherichia coli to generate pAd-SUR-NIS. The Ad-SUR-NIS virus was packaged by transfecting 4 μg of PacI-digested pAd-SUR-NIS DNA into 293 cells using Lipofectamine2000 (Invitrogen, Carlsbad, CA) and propagating in 293 cells according to the standard procedure. After two-step purification on CsCl gradients, viral stocks were desalted using Pharmacia G50 columns (Orsay, France) and frozen at −80 °C in 10 mM Tris-HCl (pH 7.5) containing 2.5% glycerol. Viral titers were calculated by a dilution plaque assay in 293 cells and expressed as PFU per ml. Purification and plaque assays were performed by SinoGenoMax, Beijing, China. The recombinant adenovirus, Ad-CMV-NIS, which uses the CMV promoter to drive NIS expression (previously described26), was used as a positive control. The recombinant adenovirus, Ad-CMV-GFP, which provided by SinoGenoMax, was used as a negative control.
Analysis of the survivin promoter activity in vitro
In order to determine the transcriptional activation activity of the survivin promoter, we utilized the Dual-Luciferase reporter assay system (Promega). The plasmid pRL-TK, which contains the Renilla luciferase gene under the control of the thymidine kinase promoter, was used as an internal control. In all, 1 × 106 cells of each cancer cell line and normal control were plated in six-well tissue culture plates and 24 h later, the cells were transfected with 4 μg of the indicated plasmid DNA and 0.1 μg of pRL-TK using Lipofectamine2000 (Invitrogen) according to the manufacturer's protocol. At 48 h post-transfection, luciferase activity was determined using the Reporter Lysis Buffer and Luciferase Assay System according to the manufacturer's protocol (Promega). The dual luciferase ratio was defined as the luciferase activity of the indicated plasmid divided by the luciferase activity of pRL-TK. The pSV40-LUC vector (Promega) that contains Simian Virus 40 (SV40) promoter was used as a positive control. All experiments were performed in triplicate.
In vitro 125I and 99mTc pertechnetate uptake experiments
In all, 1 × 106 cells of each cancer cell line and control DPF cells were plated in six-well tissue culture plates and allowed to reach exponential growth for 24 h and infected with Ad-SUR-NIS, Ad-CMV-NIS (positive control) or Ad-CMV-GFP (negative control) viruses at MOI=100 in 1 ml of medium without serum. After 2 h, the media was changed to complete medium. For each cell line, the medium used for infection was the same as the culture medium. Approximately 28–30 h after viral infection, cells were washed once with 1 ml of phosphate-buffered saline (PBS). Iodide uptake was then initiated by adding 1 ml of medium without serum containing 3.7 KBq of 125I or 99mTc pertechnetate per well. Following 30 min incubation with radionuclide, cells were washed twice with ice-cold PBS and incubated for 20 min in 1 ml of ice-cold ethanol. The ethanol was then recovered, and radioactivity was quantified (c.p.m.) using a γ-counter (No. 262 Factory, Xi’an, China). For inhibition experiments, cells were incubated with both 300 μM NaClO4 and 125I for 30 min, followed by quantification of 125I uptake as described above.
In vitro cell killing with 131I and clonogenic assay
Cell killing with 131I was performed according to the method of Boland et al.27 described as following: cells were seeded in 24-well tissue culture plates and divided into three groups. The first two groups were infected with the Ad-SUR-NIS adenovirus and the Ad-CMV-GFP virus, respectively. Thirty hours after infection, cells were washed once with PBS and incubated with 1 ml of serum-free medium containing 370 KBq 131I. The third group was not infected and was incubated in serum-free medium. After 7 h, cells from all three conditions were washed twice with PBS, trypsinized, and counted. For each condition, cells were plated in triplicate in six-well tissue culture plates (1000 cells per well) and incubated for 1 week at 37 °C. Cells were then washed once with PBS and stained with crystal violet solution (2 g l–1 crystal violet, 4% formaldehyde, 20% ethanol). Colonies of >30 cells were counted, and the mean and s.d. of the number of colonies were determined for each condition. Results were expressed as the percentage of surviving cells, defined as the percentage of colonies obtained after treatment with 131I compared with no intervention, and are representative of two independent experiments.
Biodistribution of 125I in tumor-bearing mice
Approximately 2 × 107 PC-3 cells were subcutaneously transplanted into the left or right flank of 6-week-old Balb/c nude mice and allowed to proliferate until the tumor reached a diameter of 8–10 mm. At this point, the Ad-SUR-NIS virus or the Ad-CMV-GFP virus (negative control) was injected into the tumors (both 1 × 109 PFU). Radionuclide uptake was assessed 2 days later by intravenous injection with 370 KBq of 125I. At 2, 4, 6 and 12 h post-injection, animals were killed, and selected organs (bone, muscle, heart, lung, liver, spleen, stomach, intestine, kidney, brain and tumors) were dissected, weighed and counted for radioactivity.
Scintigraphic imaging of tumor-bearing mice in vivo
Forty-eight hours after intratumoral injection of 1 × 109 PFU Ad-SUR-NIS or Ad-CMV-GFP (negative control), PC-3 tumor-bearing mice were injected with 18.5 MBq of 99mTc pertechnetate via the tail vein. After 2 h, mice were anesthetized with ketamine and xylazine and scanned with a γ-camera equipped with a pinhole collimator (Philips Medical Systems, Milpitas, CA).
Effects of NIS expression on 131I therapy in vivo
Accordingly, the PC-3 tumors were induced in Balb/c nude mice as described above. When the tumors reached 8–10 mm in diameter, the mice were given thyroxine (Sigma-Aldrich, St Louis, MO) at a concentration of 5 mg l–1 in the drinking water for 7 days before treatment. Two days before treatment, the animals were divided into two groups of three animals each. One group received an intratumoral injection of 1 × 109 PFU Ad-SUR-NIS. The other group received an intratumoral injection of 1 × 109 PFU Ad-CMV-GFP. Forty-eight hours later, both groups were given an intraperitoneal dose of 111 MBq of 131I (the dose same with Schipper et al.16 at their NIS mediate-131I therapy experiment). The length and width of the tumors were measured with a caliper at 5-day intervals after treatment. Tumor size was calculated using the formula: length × width2/2. All mice were followed for a total of 30 days and then euthanized.
Tumor samples and immunohistochemical staining
In order to detect NIS expression, resected tumors from nude mice were fixed in 4% paraformaldehyde for 24 h. Samples were immunostained using a standard streptavidin-biotin labeling protocol. Briefly, after deparaffinization and antigen retrieval, 5 μm tissue sections were incubated with NIS antibody (mouse monoclonal, 1:100, Chemicon, Temecula, CA) at 37 °C for 1 h then at 4 °C overnight. The sections were then incubated with biotinylated goat anti-mouse immunoglobulin G (1:200, Zymed Laboratories, San Francisco, CA) and subsequently incubated with horseradish peroxidase-labeled streptavidin (1:200, Zymed Laboratories). The cells were then counterstained with 3,3′-diaminobenzidine for analysis.
Statistical analysis
All data are expressed as mean±s.d. Significance was determined by the Student's t-test. P<0.05 was considered to be statistically significant.
Results
Cancer-specific activation of the survivin promoter in vitro
To assess whether the activation of the survivin promoter is cancer specific and to compare the transcriptional activation activity between the survivin promoter and the SV40 promoter, we transfected both cancer (PC-3, HepG2, A375) and normal (DPF) cells with plasmids containing the luciferase gene under control of either the survivin promoter (pSUR-Luc) or the SV40 promgfeoter (pSV40-Luc). Survivin promoter activity was generally very high in cancer cell lines and very low in normal cells. The mean dual reporter ratio for cancer and normal cell lines was 6.76±0.83 and 0.33±0.23, respectively (Figure 2). However, the activity of the SV40 promoter was similar in both cancer cell lines and normal cells, with a mean dual reporter ratio of 2.23±0.08 and 2.23±0.19, respectively (Figure 2). These data suggest that the survivin promoter is selectively active in cancer cells compared with normal cells.
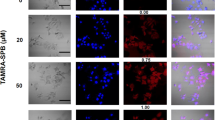
Ad-SUR-NIS is functional in various human cancer cell lines
An adenovirus that expresses NIS under control of the survivin promoter (Ad-SUR-NIS) or the CMV promoter (Ad-CMV-NIS) and a control virus expressing GFP under control of the CMV promoter (Ad-CMV-GFP) were generated and used to infect cancer cell lines (PC-3, HepG2, A375) and non-malignant control cells (DPF). In order to test the expression of NIS in these cell lines, functional assays quantifying radioiodine uptake were performed. Thirty hours after adenovirus infection, iodide uptake was measured by incubating the cells for 30 min with 3.7 KBq of 125I. As shown in Figure 3, all cancer cell lines infected with Ad-SUR-NIS exhibited significant iodide uptake, with a mean value of 12092±977 c.p.m. This value represented a 45–56-fold increase over control Ad-CMV-GFP-infected cells (237±36 c.p.m., P=0.000). No significant iodide uptake was evident in DPF cells infected with Ad-SUR-NIS (300±42 c.p.m.), consistent with luciferase reporter assays indicating the specificity of the survivin promoter for cancer cells (Figure 3). Both cancer and normal cell lines infected with the general NIS expression virus Ad-CMV-NIS exhibited significant iodide uptake. The mean amount of iodide uptake for all Ad-CMV-NIS-infected cells was 23 256±3806 c.p.m., ∼85–120 times higher than Ad-CMV-GFP-infected cells, indicating the efficacy of NIS expression for induction of radioiodine uptake (Figure 3). In addition to 125I uptake, cancer cell lines infected with Ad-SUR-NIS also exhibited selective and increased 99mTc pertechnetate uptake. The mean amount of 99mTc pertechnetate uptake was 11 906±1424 c.p.m. for cancer cells (Figure 3). In order to further demonstrate that uptake of 125I was dependent upon NIS expression in Ad-SUR-NIS-infected cells, cells were treated with the specific NIS inhibitor, sodium perchlorate during iodide uptake. Figure 3 shows that sodium perchlorate treatment inhibited iodide accumulation by 92.5±1.2% (P=0.000).
In vitro radioiodine and 99mTc pertechnetate uptake. PC-3, HepG2 and A375 cancer cell lines and the control DPF cell line were infected with Ad-SUR-NIS, Ad-CMV-NIS or Ad-CMV-GFP viruses and subjected to either 125I or 99mTc pertechnetate uptake. Ad-SUR-NIS-infected PC-3, HepG2 and A375 cancer cell lines all show significant 125I and 99mTc pertechnetate uptake ability compared with Ad-CMV-GFP-infected controls. No significant uptake was observed in Ad-SUR-NIS-infected DPF cells. Ad-CMV-NIS infection resulted in increased 125I uptake in all cell lines. Cotreatment with NaClO4 completely inhibited 125I uptake in Ad-SUR-NIS-infected cancer cells.
Ad-SUR-NIS-infected human cancer cells are efficiently killed by 131I in vitro
In order to demonstrate selective killing of cancer cells that could be obtained using Ad-SUR-NIS infection in combination with radioactive iodide treatment, 131I uptake experiments were performed on Ad-SUR-NIS-infected PC-3, A375, HepG2 and DPF cells. Ad-CMV-GFP-infected cells treated with 131I were used as controls. After 131I treatment, clonogenic assays were performed, and results were expressed as the percentage of surviving cells compared with untreated controls. Following exposure to 131I, <10% of Ad-CMV-GFP-infected cells were killed compared with untreated controls. However, 86±3.5%, 92±3.0% and 89±4.5% of PC-3, A375 and HepG2 cells, respectively, were killed by 131I following infection with Ad-SUR-NIS. No significant cell death was observed in Ad-SUR-NIS-infected DPF cells treated with 131I, as 91±2.3% of cells were recovered. These results demonstrate that coupling Ad-SUR-NIS infection and 131I treatment efficiently and specifically leads to cancer cell killing in vitro.
125I biodistribution studies in tumor-bearing mice
In order to extend our in vitro results using the Ad-SUR-NIS virus to an in vivo model, we used nude mice bearing tumors generated by subcutaneous transplantation of PC-3 cells as a model. Tumors were injected with either the Ad-SUR-NIS virus or the control Ad-CMV-GFP virus, and mice were subjected to 125I treatment 48 h later. Quantitation of the uptake of 125I (% ID per g) in tumors and various organs was evaluated at 2, 4, 6 and 12 h after 125I administration (Table 1). PC-3 tumors infected with Ad-SUR-NIS accumulated 13.3±2.85% ID per g at 2 h, 5.61±1.38% ID per g at 4 h, 2.74±0.21% ID per g at 6 h and 0.68±0.05% ID per g at 12 h, with a mean effective half-life of 3.1±0.6 h. All other organs accumulated negligible amounts of isotope (below 2.5% ID per g at all times) except stomach. The biodistribution data are summarized in Table 1. Compared with Ad-SUR-NIS-infected tumors, negative control tumors infected with Ad-CMV-GFP accumulated 0.66±0.24% ID per g 125I at 2 h after administration (P=0.000). At 4, 6 and 12 h, they accumulated 0.42±0.44% ID per g (P=0.001), 0.34±0.04% ID per g (P=0.000) and 0.06±0.01% ID per g (P=0.014), respectively. These data indicate that infection of tumors with the Ad-SUR-NIS virus leads to selective uptake of 125I in vivo.
Visualization of Ad-SUR-NIS-infected tumors by 99mTc pertechnetate scintigraphy
In order to test whether Ad-SUR-NIS-infected tumors could be visualized in vivo, scintigraphy was performed on tumor-bearing mice using 99mTc pertechnetate, allowing imaging with a pinhole collimator. 99mTc pertechnetate (18.5 MBq) was injected intraperitoneally, and images were taken after 2 h (Figure 4). As expected, tissues naturally expressing NIS (stomach and thyroid) or involved in iodide elimination (bladder) were visualized. The Ad-SUR-NIS-infected tumor was clearly visible, with intensity comparable to that of the thyroid or the bladder. However, the Ad-CMV-GFP-infected PC-3 tumor was not visible.
99mTc pertechnetate scintigraphic images of PC-3 xenografts infected with either Ad-CMV-GFP or Ad-SUR-NIS. Mice harboring PC-3 xenograft tumors infected with either Ad-CMV-GFP (a) or Ad-SUR-NIS (b) were imaged with a pinhole collimator 2 h after injection of 18.5 MBq 99mTc pertechnetate. (a) The Ad-CMV-GFP-infected tumor is not visible using 99mTc pertechnetate imaging. (b) The Ad-SUR-NIS-infected tumor is clearly visible, with an intensity comparable to that of the thyroid or the bladder.
Decreased tumor growth induced by Ad-SUR-NIS infection in combination with 131I treatment
In vitro studies suggested that Ad-SUR-NIS infection combined with radioiodine treatment can inhibit growth of cancer cells. In order to extend these results to an in vivo model, tumors were generated in Balb/c nude mice and infected with either Ad-SUR-NIS or Ad-CMV-GFP. After 48 h, mice were treated with 131I as described in the Materials and methods. As shown in Figure 5, tumors in animals that received 131I and Ad-CMV-GFP continued to grow until the end of the experiment. In contrast, tumors in animals that received injections of both Ad-SUR-NIS intratumorally and 131I intraperitoneally began to show a slight reduction in growth on day 10 and day 15, and from day 20 to day 30, tumor volumes in this group were statistically different from Ad-CMV-GFP-infected controls. The volume reduction rates at days 20, 25 and 30 were 32.9±11.3% (P=0.029), 46.2±4.4% (P=0.001) and 51.4±15.9% (P=0.012), respectively. These results suggest that expression of NIS in combination with 131I treatment may prove to be a possible strategy for reduction of tumor growth in vivo.
Therapeutic effects of Ad-SUR-NIS infection in combination with 131I treatment in PC-3 xenografts. Tumor size was assayed after 131I treatment in nude mice bearing tumors infected with either Ad-SUR-NIS or Ad-CMV-GFP. Growth of Ad-SUR-NIS-infected PC-3 tumors was significantly retarded (*,**,***P<0.05) at days 20, 25 and 30 after injection of 111 MBq 131I.
Membrane expression of NIS in tumors injected with Ad-SUR-NIS
For in vivo experiments, expression of the NIS protein in the tumor was characterized by immunohistochemical staining. Tumors injected with Ad-SUR-NIS were specifically labeled with anti-NIS antibodies. Labeling was clearly confined to cell membranes, indicating that expression of NIS driven by the Ad-SUR-NIS virus leads to correct localization of the NIS protein in vivo. Representative tumor sections are shown in Figure 6.
Discussion
Consistent with the role of NIS in the success of radioiodine therapy for thyroid cancer, targeted expression of NIS provides the possibility of NIS-targeted radionuclide therapy for treatment of non-thyroidal tumors.27, 28, 29 In contrast to other potential therapeutic genes, therapeutic use of NIS has several advantages. The potential function of NIS as a diagnostic gene allows non-invasive radioiodine imaging to confirm and localize functional NIS expression before proceeding to the application of a therapeutic 131I dose. NIS gene therapy may also be more effective due to a substantial bystander effect caused by treatment with the β-emitter 131I, which has a path length of up to 2–4 mm, and can cause the death of NIS-expressing cells as well as neighboring non-transfected cells.30
The ultimate goal of cancer therapy is to maximize cancer cell-specific cytotoxicity and minimize toxic side effects in non-malignant cells. Gene therapy using tissue-specific promoters provides a means of selectively targeting therapeutic genes to malignant cells.31 Several cancer-specific targeting promoters are available for targeting of individual cancers, including the prostate specific antigen promoter (prostate cancer), the albumin enhancer and promoter (hepatocellular cancer), the CEA promoter (medullary thyroid cancer, colorectal cancer), the MUC-1 promoter (breast cancer, pancreatic cancer) and the chromogranin A promoter (neuroendocrine tumors). These promoters are cancer-type specific, but are limited in scope.
The expression of survivin is noted in common human cancers but not in normal adult tissues. As the increased survivin activity is controlled transcriptionally, it has been suggested that the survivin promoter might control the transgene expression in a cancer-specific manner.32, 33 Previous in vivo studies indicated that the activities of survivin promoter were extremely low in the major mouse organs, and therefore, it may prove to be a good candidate for transcriptional targeting of cancer gene therapy in a wide variety of tumors.34 So in this study, we used the survivin promoter as a candidate promoter to test the feasibility of using a multicancer-specific promoter to extend the scope of a gene-based therapy. The survivin promoter was used to target hNIS expression and induce radionuclide accumulation in three representative cancers: prostate cancer, hepatocarcinoma and melanoma, all of them have relatively high incidence and mortality in China.
Our data indicated that the survivin promoter could drive luciferase expression specifically in cancer cells. The survivin promoter was 2–3 times more active than the SV40 promoter, consistent with the previous reports.32, 34 This observation suggests that the survivin promoter could induce high transgene expression in cancer cells.
In in vitro functional studies, the survivin promoter was shown to be capable of driving functional NIS expression in three different cancer cell lines. Expression of NIS via the Ad-SUR-NIS virus increased perchlorate-sensitive iodide uptake to 50-fold over that of Ad-CMV-GFP-infected cancer cells. Furthermore, no significant iodide uptake was observed in Ad-SUR-NIS-infected DPF cells, indicating that the virus was selective for cancer cells. Scintigraphy and biodistribution studies confirmed that specific accumulation of radionuclide also occurred in Ad-SUR-NIS-infected PC-3 tumors in vivo.
For effective treatment using radioisotopes, it is important that the tumor receives a high radiation dose. The dose is determined by the level of uptake, which in this case was controlled by the level of NIS expression and the available amount of iodide, and the effective half-life of the isotope in the tumor, which is a product of the physical half-life (8.021 days for 131I) and the biological half-life of the isotope. The biological half-life depends on several factors, including the rates of internalization and externalization and whether the isotope is organified in the cell. A controversy exists regarding the feasibility of NIS gene therapy for extrathyroidal tumors that cannot organify trapped iodide, which is thought to be a crucial prerequisite for effective radioiodine therapy. However, data from several groups working in non-organifying extrathyroidal tumor models, including prostate cancer, hepatocarcinoma and myeloma, clearly demonstrate that a significant therapeutic effect of 131I can be achieved after NIS gene transfer in the absence of organification.5, 9, 35 In these studies, either a long effective half-life or sufficient residual radioactivity led to effects in tumor cells.
We investigated the possibility of combining Ad-SUR-NIS infection with 131I radionuclide therapy for treatment of cancer. An in vitro clonogenic study showed that coupling Ad-SUR-NIS and 131I treatments efficiently and specifically killed multiple types of cancer cells. Similar treatments in an in vivo tumor model showed that combining Ad-SUR-NIS infection with 131I treatment retarded the tumor growth compared to controls. This result is not as significant as the studies discussed above, due to the mean effective half-life of 131I in Ad-SUR-NIS-infected PC-3 tumors is less than them, so some additional considerations should be used to improve the therapeutic efficacy of the combinatorial treatment.
One approach involves the cotransfection of thyroid peroxidase and NIS.36 Another practical approach involves the use of more powerful therapeutic radionuclides such as 211At or 188Re.6, 8, 37 These radionuclides have similar chemical properties to iodine and more favorable physical properties, including a higher linear energy transfer and shorter physical half-life. Therefore, treatments using these radionuclides should result in an increased radiation dose and, thus, enhanced efficacy. A recent study by Willhauck et al.8 demonstrated the therapeutic efficacy of 211At in LNCaP cells stably expressing NIS under the control of the prostate specific antigen promoter (NP-1) in vivo. 211At was found to have an effective half-life of 4.6 h, and treatment caused a significant reduction in tumor volume of up to 82%.8 This and other similar studies provide information that can help to develop optimized therapeutic regimens for use with the Ad-SUR-NIS system. Regarding the use of the adenoviral transport system, a regime that includes multiple injections of adenovirus/radioiodine is likely to enhance reduction in tumor volume. Use of a conditionally replicating adenovirus as a platform for delivery of NIS may represent another potential alternative. This type of virus would be able to replicate and spread within the tumor, thus increasing the rate of tumor-cell clearance due to radioiodide uptake.
An important potential complication of this therapeutic regimen must also be considered. Special care must be taken to protect the thyroid gland from damage. Generally, we utilize thyroid hormone pretreatment, which suppresses thyroidal 131I uptake, which is known to be selectively regulated by the thyroid-stimulating hormone. However, if thyroidal radioiodine uptake did cause damage to the thyroid gland, effects on patients could easily and inexpensively be managed by routine thyroid hormone replacement therapy.28 Due to the local accumulation of 131I, the stomach, salivary glands, bladder and colon lumen also receive the high radiation doses. Although no significantly increased risk of stomach and bladder was observed in thyroid cancer patients treated with radioactive iodine, the increased risks of colorectal and salivary gland cancers were found with higher cumulative amount of 131I, which should be minimized by a simple routine of having patients drink large quantities of fluids and lemon juice, and by the use of laxatives.38, 39, 40
In conclusion, the therapeutic effect of combining survivin promoter-driven expression of NIS and 131I treatment has been demonstrated in three different cancer cell types in vitro. Furthermore, survivin promoter-driven expression of NIS also induced tumor-specific iodide accumulation and a reduction in tumor growth in an in vivo PC-3 xenotransplant model in nude mice. Future studies will focus on enhancing the therapeutic effects of this treatment through the use of more powerful therapeutic radionuclides, such as 211At or 188Re, and through revision of the adenoviral delivery system.
References
Dai G, Levy O, Carrasco N . Cloning and characterization of the thyroid iodide transporter. Nature 1996; 379: 458–460.
De La Vieja A, Dohan O, Levy O, Carrasco N . Molecular analysis of the sodium/iodide symporter: impact on thyroid and extrathyroid pathophysiology. Physiol Rev 2000; 80: 1083–1105.
Spitzweg C, Heufelder AE, Morris JC . Thyroid iodine transport. Thyroid 2000; 10: 321–330.
Smanik PA, Liu Q, Furminger TL, Ryu K, Xing S, Mazzaferri EL et al. Cloning of the human sodium lodide symporter. Biochem Biophys Res Commun 1996; 226: 339–345.
Spitzweg C, O’Connor MK, Bergert ER, Tindall DJ, Young CY, Morris JC . Treatment of prostate cancer by radioiodine therapy after tissue-specific expression of the sodium iodide symporter. Cancer Res 2000; 60: 6526–6530.
Willhauck MJ, Sharif Samani BR, Gildehaus FJ, Wolf I, Senekowitsch-Schmidtke R, Stark HJ et al. Application of 188rhenium as an alternative radionuclide for treatment of prostate cancer after tumor-specific sodium iodide symporter gene expression. J Clin Endocrinol Metab 2007; 92: 4451–4458.
Kakinuma H, Bergert ER, Spitzweg C, Cheville JC, Lieber MM, Morris JC . Probasin promoter (ARR(2)PB)-driven, prostate-specific expression of the human sodium iodide symporter (h-NIS) for targeted radioiodine therapy of prostate cancer. Cancer Res 2003; 63: 7840–7844.
Willhauck MJ, Samani BR, Wolf I, Senekowitsch-Schmidtke R, Stark HJ, Meyer GJ et al. The potential of 211Astatine for NIS-mediated radionuclide therapy in prostate cancer. Eur J Nucl Med Mol Imaging 2008; 35: 1272–1281.
Willhauck MJ, Sharif Samani BR, Klutz K, Cengic N, Wolf I, Mohr L et al. Alpha-fetoprotein promoter-targeted sodium iodide symporter gene therapy of hepatocellular carcinoma. Gene Ther 2008; 15: 214–223.
Chen L, Altmann A, Mier W, Eskerski H, Leotta K, Guo L et al. Radioiodine therapy of hepatoma using targeted transfer of the human sodium/iodide symporter gene. J Nucl Med 2006; 47: 854–862.
Kim SH, Chung HK, Kang JH, Kim KI, Jeon YH, Jin YN et al. Tumor-targeted radionuclide imaging and therapy based on human sodium iodide symporter gene driven by a modified telomerase reverse transcriptase promoter. Hum Gene Ther 2008; 19: 951–957.
Ma XJ, Huang R, Kuang AR . AFP promoter enhancer increased specific expression of the human sodium iodide symporter (hNIS) for targeted radioiodine therapy of hepatocellular carcinoma. Cancer Invest 2009; 27: 673–681.
Cengic N, Baker CH, Schutz M, Goke B, Morris JC, Spitzweg C . A novel therapeutic strategy for medullary thyroid cancer based on radioiodine therapy following tissue-specific sodium iodide symporter gene expression. J Clin Endocrinol Metab 2005; 90: 4457–4464.
Scholz IV, Cengic N, Baker CH, Harrington KJ, Maletz K, Bergert ER et al. Radioiodine therapy of colon cancer following tissue-specific sodium iodide symporter gene transfer. Gene Ther 2005; 12: 272–280.
Dwyer RM, Bergert ER, O’Connor MK, Gendler SJ, Morris JC . In vivo radioiodide imaging and treatment of breast cancer xenografts after MUC1-driven expression of the sodium iodide symporter. Clin Cancer Res 2005; 11: 1483–1489.
Schipper ML, Riese CG, Seitz S, Weber A, Behe M, Schurrat T et al. Efficacy of 99mTc pertechnetate and 131I radioisotope therapy in sodium/iodide symporter (NIS)-expressing neuroendocrine tumors in vivo. Eur J Nucl Med Mol Imaging 2007; 34: 638–650.
Ambrosini G, Adida C, Altieri DC . A novel anti-apoptosis gene, survivin, expressed in cancer and lymphoma. Nat Med 1997; 3: 917–921.
Adida C, Berrebi D, Peuchmaur M, Reyes-Mugica M, Altieri DC . Anti-apoptosis gene, survivin, and prognosis of neuroblastoma. Lancet 1998; 351: 882–883.
Zhang T, Otevrel T, Gao Z, Gao Z, Ehrlich SM, Fields JZ et al. Evidence that APC regulates survivin expression: a possible mechanism contributing to the stem cell origin of colon cancer. Cancer Res 2001; 61: 8664–8667.
Fukuda S, Pelus LM . Regulation of the inhibitor-of-apoptosis family member survivin in normal cord blood and bone marrow CD34(+) cells by hematopoietic growth factors: implication of survivin expression in normal hematopoiesis. Blood 2001; 98: 2091–2100.
Gianani R, Jarboe E, Orlicky D, Frost M, Bobak J, Lehner R et al. Expression of survivin in normal, hyperplastic, and neoplastic colonic mucosa. Hum Pathol 2001; 32: 119–125.
Mita AC, Mita MM, Nawrocki ST, Giles FJ . Survivin: key regulator of mitosis and apoptosis and novel target for cancer therapeutics. Clin Cancer Res 2008; 14: 5000–5005.
Altieri DC . The molecular basis and potential role of survivin in cancer diagnosis and therapy. Trends Mol Med 2001; 7: 542–547.
Li F, Altieri DC . The cancer antiapoptosis mouse survivin gene: characterization of locus and transcriptional requirements of basal and cell cycle-dependent expression. Cancer Res 1999; 59: 3143–3151.
Li F, Altieri DC . Transcriptional analysis of human survivin gene expression. Biochem J 1999; 344 (Part 2): 305–311.
Huang R, Kuang A, Yu H, Ma C, Tang G . Construction of the recombinant adenovirus carrying sodium/iodide symporter gene. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 2005; 22: 765–768.
Boland A, Ricard M, Opolon P, Bidart JM, Yeh P, Filetti S et al. Adenovirus-mediated transfer of the thyroid sodium/iodide symporter gene into tumors for a targeted radiotherapy. Cancer Res 2000; 60: 3484–3492.
Spitzweg C, Morris JC . The sodium iodide symporter: its pathophysiological and therapeutic implications. Clin Endocrinol (Oxf) 2002; 57: 559–574.
Mandell RB, Mandell LZ, Link Jr CJ . Radioisotope concentrator gene therapy using the sodium/iodide symporter gene. Cancer Res 1999; 59: 661–668.
Carlin S, Cunningham SH, Boyd M, McCluskey AG, Mairs RJ . Experimental targeted radioiodide therapy following transfection of the sodium iodide symporter gene: effect on clonogenicity in both two- and three-dimensional models. Cancer Gene Ther 2000; 7: 1529–1536.
Hart IR . Tissue specific promoters in targeting systemically delivered gene therapy. Semin Oncol 1996; 23: 154–158.
Bao R, Connolly DC, Murphy M, Green J, Weinstein JK, Pisarcik DA et al. Activation of cancer-specific gene expression by the survivin promoter. J Natl Cancer Inst 2002; 94: 522–528.
Chen JS, Liu JC, Shen L, Rau KM, Kuo HP, Li YM et al. Cancer-specific activation of the survivin promoter and its potential use in gene therapy. Cancer Gene Ther 2004; 11: 740–747.
Zhu ZB, Makhija SK, Lu B, Wang M, Kaliberova L, Liu B et al. Transcriptional targeting of tumors with a novel tumor-specific survivin promoter. Cancer Gene Ther 2004; 11: 256–262.
Dingli D, Peng KW, Harvey ME, Greipp PR, O’Connor MK, Cattaneo R et al. Image-guided radiovirotherapy for multiple myeloma using a recombinant measles virus expressing the thyroidal sodium iodide symporter. Blood 2004; 103: 1641–1646.
Huang M, Batra RK, Kogai T, Lin YQ, Hershman JM, Lichtenstein A et al. Ectopic expression of the thyroperoxidase gene augments radioiodide uptake and retention mediated by the sodium iodide symporter in non-small cell lung cancer. Cancer Gene Ther 2001; 8: 612–618.
Petrich T, Quintanilla-Martinez L, Korkmaz Z, Samson E, Helmeke HJ, Meyer GJ et al. Effective cancer therapy with the alpha-particle emitter astatine in a mouse model of genetically modified sodium/iodide symporter-expressing tumors. Clin Cancer Res 2006; 12: 1342–1348.
Rubino C, de Vathaire F, Dottorini ME, Hall P, Schvartz C, Couette JE et al. Second primary malignancies in thyroid cancer patients. Br J Cancer 2003; 89: 1638–1644.
Brown AP, Chen J, Hitchcock YJ, Szabo A, Shrieve DC, Tward JD . The risk of second primary malignancies up to three decades after the treatment of differentiated thyroid cancer. J Clin Endocrinol Metab 2008; 93: 504–515.
Chuang SC, Hashibe M, Yu GP, Le AD, Cao W, Hurwitz EL et al. Radiotherapy for primary thyroid cancer as a risk factor for second primary cancers. Cancer Lett 2006; 238: 42–52.
Acknowledgements
We thank Mr X Yang, Ms Q Fan and Ms L Zhou for technical assistance. This work was supported by grants to Kuang AnRen and HR from the National Natural Science Foundation of China (NSFC 30670585, 30870724 and 30600153).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Huang, R., Zhao, Z., Ma, X. et al. Targeting of tumor radioiodine therapy by expression of the sodium iodide symporter under control of the survivin promoter. Cancer Gene Ther 18, 144–152 (2011). https://doi.org/10.1038/cgt.2010.66
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cgt.2010.66
Keywords
This article is cited by
-
Analysis of drug sensitivity of Escherichia Coli O157H7
Biomedical Microdevices (2021)
-
Current outlook on radionuclide delivery systems: from design consideration to translation into clinics
Journal of Nanobiotechnology (2019)
-
Sodium iodide symporter (NIS) in extrathyroidal malignancies: focus on breast and urological cancer
BMC Cancer (2014)
-
Combining transfer of TTF-1 and Pax-8 gene: a potential strategy to promote radioiodine therapy of thyroid carcinoma
Cancer Gene Therapy (2012)