Abstract
Background:
Coffee and other sources of methylxanthines and risk of Type I vs Type II endometrial cancer (EC) have not been evaluated previously.
Methods:
Prospective cohort of 23 356 postmenopausal women with 471 Type I and 71 Type II EC cases.
Results:
Type I EC was statistically significantly associated with caffeinated (relative risk (RR)=0.65 for 4+ cups per day vs ⩽1 cup per month: 95% confidence interval (CI): 0.47–0.89) but not decaffeinated (RR=0.76; 95% CI: 0.50–1.15) coffee intake; there were no associations with tea, cola or chocolate, or for Type II EC. The inverse association with caffeinated coffee intake was specific to women with a body mass index 30+ kg m−2 (RR=0.56; 95% CI: 0.36–0.89).
Conclusion:
Coffee may protect against Type I EC in obese postmenopausal women.
Similar content being viewed by others
Main
Following water and tea, coffee is the third most consumed beverage in the world (Bushman, 1998; La Vecchia and Tavani, 2007). A recent meta-analysis reported an inverse association of coffee intake with endometrial cancer (EC) risk (Je and Giovannucci, 2011). The presence of antioxidants and other chemopreventive compounds in coffee may explain its anticarcinogenic effect (Vivani, 1993; Cavin et al, 2002). However, it is not clear whether coffee per se, caffeine or other methylxanthines (e.g., theophylline and theobromine) are most relevant. Also unexplored is whether there is heterogeneity by Type I vs Type II EC, which may have different aetiologies (Bokhman, 1983; Doll et al, 2008; Mendivil et al, 2009). The aim of the present study was to evaluate the association of coffee consumption (with and without caffeine) and other sources of methylxanthines with risk of Type I vs Type II EC, overall and stratified on body mass index (BMI), smoking history and hormone therapy (HT) use.
Materials and methods
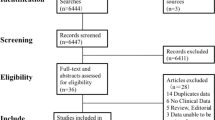
Details regarding the Iowa Women’s Health Study (IWHS) have been published (Folsom et al, 1990). In brief, 41 836 women aged 55–69 years completed a self-administered survey at enrolment in 1986. The baseline survey included a 126-item semiquantitative food-frequency questionnaire (FFQ) (Willett et al, 1988), which included the average intake in the past year of the following items: caffeinated coffee; decaffeinated coffee; tea (excluding herbal teas); regular and sugar-free carbonated beverages with caffeine; chocolate; chocolate bars; and brownies. The FFQ was reliable and valid in this population (Munger et al, 1992).
Incident EC cases were identified through 2005 via annual linkage with the Iowa Cancer Registry. Cancer data were coded according to the International Classification of Diseases for Oncology (Fritz et al, 2000). Type I or Type II were classified based on registry codes (see Table 1 footnote) as described previously (Uccella et al, 2011); there was no central pathology review. Deaths were ascertained by follow-up surveys, annual linkage with Iowa death certificates and linkage to the National Death Index.
Women with history of cancer before baseline, except non-melanoma skin cancer (n=3830); hysterectomy before baseline (n=14 350); extreme dietary intake (<600 or >5000 kcal per day) or incomplete FFQ questionnaires (⩾30 blank food items) (n=3096); or who were not postmenopausal at baseline (n=569) were excluded from the present analysis (not mutually exclusive), yielding a final sample size of 23 356 study participants.
Each woman accumulated person-years of follow-up from baseline to date of EC diagnosis, move from Iowa, death or administrative censoring on 31 December 2005. Relative risks (RR) and 95% confidence intervals (95% CIs) were estimated using Cox proportional hazards regression, and modelling age was used as the time variable (Korn et al, 1997). All Cox model attributes included as covariates are listed in corresponding table footnotes, and were selected a priori based on their suspected or known associations with endometrial cancer. Separate analyses were carried out for Type I and Type II EC. Tests for trend were carried out by ordering the intake quartiles from lowest to highest and including the resulting variable as a 1 d.f. linear term in the Cox regression models.
We formally determined if risk ratios for the exposure variables differed by type of EC using a competing risk form of Cox proportional hazards regression (Lunn and McNeil, 1995). We also examined associations between exposure variables and subtype-specific EC risk within strata defined by BMI, smoking status and use of HT. All statistical tests were two-sided, and analyses were carried out using SAS (SAS Institute Inc., Cary, NC, USA) and R software systems.
Results
At study baseline, there were 23 356 women in the at-risk cohort, of whom 5218 (22.3%) were obese (BMI ⩾30 kg m−2) and 6843 (29.3%) drank 4+ cups per day of coffee (caffeinated or decaffeinated). The correlation of coffee intake with EC risk factors is shown in Table 2.
During the 20-year follow-up period, we identified a total of 542 incident cases of EC, 471 Type I and 71 Type II. The mean age at diagnosis of Type I EC was 71.8 years (range, 57.2–89.5 years) and Type II EC was 72.8 years (range, 60.2–89.3 years).
There was an inverse association of caffeinated coffee consumption with risk of Type I EC after multivariate adjustment (RR=0.65 for 4+ cups per day compared with ⩽1 cup per month; P-trend=0.033), but there were no statistically significant trends with intake of total coffee, decaffeinated coffee, tea, colas or other sources of methylxanthines, although the highest intake of total coffee and decaffeinated coffee did have RRs <0.8 (Table 1). Compared with women who did not drink either caffeinated or decaffeinated coffee, those who drank 4+ cups per day of caffeinated coffee only (RR=0.73; 95% CI: 0.52–1.02) or 1+ cups per day of both types of coffee (RR=0.69; 95% CI: 0.47–1.01) had lower EC risk, whereas the association was weaker and not statistically significant for women who drank 4+ cups per day of decaffeinated coffee only (RR=0.81; 95% CI: 0.52–1.27). Caffeine intake showed a suggestive inverse associated with risk (RR=0.80 for >385 mg per day compared with <29.7 mg per day; P-trend=0.059). In contrast, coffee and other sources of methylxanthines were not associated with risk of Type II EC.
We next examined coffee intake with risk of Type I EC within strata defined by BMI (30+ vs <30 kg m−2), smoking history (ever/never) and HT use (ever/never); the sample size was too small to conduct these analyses for risk of Type II EC. As shown in Table 3, the inverse associations for total and caffeinated coffee, caffeine and perhaps decaffeinated coffee were only observed among obese women and not among women with a BMI <30 kg m−2. There was no striking or consistent heterogeneity in the associations for coffee or caffeine intake when stratified on smoking status (Supplementary Table 1) or HT use (Supplementary Table 2).
Discussion
Coffee consumption was most strongly associated with a lower risk of Type I EC among obese postmenopausal women, and these associations were generally stronger and statistically significant for caffeinated relative to decaffeinated coffee intake. There were no statistically significant associations of coffee consumption with Type I EC among non-obese women or for Type II EC. Tea, cola and chocolate intake were not associated with risk of Type I or Type II EC.
A recently updated meta-analysis of 6 cohort and 10 case–control studies (Je and Giovannucci, 2011) reported a pooled RR of 0.71 (95% CI: 0.62–0.81) for the risk of EC for the highest vs lowest categories of coffee intake, with the strongest inverse association observed in Japanese studies (RR=0.40; 95% CI: 0.25–0.63), intermediate for North American studies (RR=0.69; 95% CI: 0.60–0.79) and weakest but still evident for European studies (RR=0.79; 95% CI: 0.63–0.99). Consistent with our results, four recent studies found an inverse association of coffee with EC, particularly among women with BMI ⩾30 kg m−2 (Friberg et al, 2009; Giri et al, 2011; Gunter et al, 2011; Je et al, 2011). For the first time, we extend this association specifically to Type I EC and to coffee but not other common sources of methylxanthines, which were not addressed by these prior studies.
The exact mechanisms involved in any putative beneficial effect of coffee on EC remain largely unknown. Coffee is a major source of caffeine, and this methylxanthine may increase levels of circulating sex-hormone-binding globulin, thus reducing the concentrations of bioavailable sex-steroid hormones, in particular free oestradiol, and consequently modifying the hormonal milieu leading to downregulation of endometrial hyperproliferation (Ferrini and Barrett-Connor, 1996; Nagata et al, 1998). However, coffee, irrespective of caffeine content, also contains additional compounds with antioxidant activities. These compounds vary widely depending on the type of coffee, roasting and preparation, and many have been found to inhibit the proliferation of tumour cells in vitro (Vivani, 1993; Cavin et al, 2002).
An intriguing hypothesis suggests that coffee may be an insulin sensitiser (Wu et al, 2005; Huxley et al, 2009; Loopstra-Masters et al, 2011). Coffee (both caffeinated and decaffeinated) and caffeine intake were inversely associated with levels of circulating C-peptide, a marker of insulin secretion and resistance, and this association was much stronger in overweight and obese women (Wu et al, 2005).
An inverse association with coffee was not observed for Type II EC, although our analysis was limited by the relatively small number of Type II cases and by the absence of central pathology review. Type I and Type II EC may have different aetiologic pathways and distinct risk factors (Uccella et al, 2011). From a molecular point of view, Type II EC is often associated with p53 mutations, which commonly lead to DNA derangements, chromosomal instability and a more aggressive clinical behaviour (Doll et al, 2008). Conversely, alterations of p53 have been reported in only a small proportion of Type I tumours and, when they occur, they are usually a late event (Doll et al, 2008). Apoptosis of rapidly growing cells induced by caffeine in vitro is dependent on the presence of a functional p53 product, so when p53 is mutated cellular growth is not inhibited by caffeine (He et al, 2003).
In conclusion, our results suggest that coffee consumption, perhaps in part related to caffeine, may be relevant for chemoprevention of Type I EC, particularly among obese women.
Change history
01 October 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bokhman JV (1983) Two pathogenetic types of endometrial carcinoma. Gynecol Oncol 15 (1): 10–17.
Bushman JL (1998) Green tea and cancer in humans: a review of the literature. Nutr Cancer 31 (3): 151–159.
Cavin C, Holzhaeuser D, Scharf G, Constable A, Huber WW, Schilter B (2002) Cafestol and kahweol, two coffee specific diterpenes with anticarcinogenic activity. Food Chem Toxicol 40 (8): 1155–1163.
Doll A, Abal M, Rigau M, Monge M, Gonzalez M, Demajo S, Colas E, Llaurado M, Alazzouzi H, Planaguma J, Lohmann MA, Garcia J, Castellvi S, Ramon y Cajal J, Gil-Moreno A, Xercavins J, Alameda F, Reventos J (2008) Novel molecular profiles of endometrial cancer − new light through old windows. J Steroid Biochem Mol Biol 108 (3–5): 221–229.
Ferrini RL, Barrett-Connor E (1996) Caffeine intake and endogenous sex steroid levels in postmenopausal women. The Rancho Bernardo Study. Am J Epidemiol 144 (7): 642–644.
Folsom AR, Kaye SA, Prineas RJ, Potter JD, Gapstur SM, Wallace RB (1990) Increased incidence of carcinoma of the breast associated with abdominal adiposity in postmenopausal women. Am J Epidemiol 131 (5): 794–803.
Friberg E, Orsini N, Mantzoros CS, Wolk A (2009) Coffee drinking and risk of endometrial cancer – a population-based cohort study. Int J Cancer 125 (10): 2413–2417.
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S (2000) International Classification of Diseases for Oncology 3rd edn. World Health Organization: Geneva, Switzerland.
Giri A, Sturgeon SR, Luisi N, Bertone-Johnson E, Balasubramanian R, Reeves KW (2011) Caffeinated coffee, decaffeinated coffee and endometrial cancer risk: a prospective cohort study among US postmenopausal women. Nutrients 3 (11): 937–950.
Gunter MJ, Schaub JA, Xue X, Freedman ND, Gaudet MM, Rohan TE, Hollenbeck AR, Sinha R (2011) A prospective investigation of coffee drinking and endometrial cancer incidence. Int J Cancer 131: E530–E536.
He Z, Ma WY, Hashimoto T, Bode AM, Yang CS, Dong Z (2003) Induction of apoptosis by caffeine is mediated by the p53, Bax, and caspase 3 pathways. Cancer Res 63 (15): 4396–4401.
Huxley R, Lee CM, Barzi F, Timmermeister L, Czernichow S, Perkovic V, Grobbee DE, Batty D, Woodward M (2009) Coffee, decaffeinated coffee, and tea consumption in relation to incident type 2 diabetes mellitus: a systematic review with meta-analysis. Arch Intern Med 169 (22): 2053–2063.
Je Y, Giovannucci E (2011) Coffee consumption and risk of endometrial cancer: findings from a large up-to-date meta-analysis. Int J Cancer 131 (7): 1700–1710.
Je Y, Hankinson SE, Tworoger SS, DeVivo I, Giovannucci E (2011) A prospective cohort study of coffee consumption and risk of endometrial cancer over a 26-year follow-up. Cancer Epidemiol Biomarkers Prev 20: 2487–2495.
Korn EL, Graubard BI, Midthune D (1997) Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 145 (1): 72–80.
La Vecchia C, Tavani A (2007) Coffee and cancer risk: an update. Eur J Cancer Prev 16 (5): 385–389.
Loopstra-Masters RC, Liese AD, Haffner SM, Wagenknecht LE, Hanley AJ (2011) Associations between the intake of caffeinated and decaffeinated coffee and measures of insulin sensitivity and beta cell function. Diabetologia 54 (2): 320–328.
Lunn M, McNeil D (1995) Applying Cox regression to competing risks. Biometrics 51 (2): 524–532.
Mendivil A, Schuler KM, Gehrig PA (2009) Non-endometrioid adenocarcinoma of the uterine corpus: a review of selected histological subtypes. Cancer Control 16 (1): 46–52.
Munger RG, Folsom AR, Kushi LH, Kaye SA, Sellers TA (1992) Dietary assessment of older Iowa women with a food frequency questionnaire: nutrient intake, reproducibility, and comparison with 24-hour dietary recall interviews. Am J Epidemiol 136 (2): 192–200.
Nagata C, Kabuto M, Shimizu H (1998) Association of coffee, green tea, and caffeine intakes with serum concentrations of estradiol and sex hormone-binding globulin in premenopausal Japanese women. Nutr Cancer 30 (1): 21–24.
Uccella S, Mariani A, Wang AH, Vierkant RA, Robien K, Anderson KE, Cerhan JR (2011) Dietary and supplemental intake of one-carbon nutrients and the risk of type I and type II endometrial cancer: a prospective cohort study. Ann Oncol 22 (9): 2129–2136.
Vivani R (1993) The composition of coffee. In Caffeine, Coffee and Health Garattini S (ed). pp 17–41. Rave Press Ltd: New York, NY, USA.
Willett WC, Sampson L, Browne ML, Stampfer MJ, Rosner B, Hennekens CH, Speizer FE (1988) The use of a self-administered questionnaire to assess diet four years in the past. Am J Epidemiol 127: 188–199.
Wu T, Willett WC, Hankinson SE, Giovannucci E (2005) Caffeinated coffee, decaffeinated coffee, and caffeine in relation to plasma C-peptide levels, a marker of insulin secretion, in U.S. women. Diabetes Care 28 (6): 1390–1396.
Acknowledgements
This study was supported by the National Institutes of Health (NIH) Grant R01 CA39742, and was approved by the IRB of the University of Minnesota.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Uccella, S., Mariani, A., Wang, A. et al. Intake of coffee, caffeine and other methylxanthines and risk of Type I vs Type II endometrial cancer. Br J Cancer 109, 1908–1913 (2013). https://doi.org/10.1038/bjc.2013.540
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.540
Keywords
This article is cited by
-
The Association Between Nutrition, Obesity, Inflammation, and Endometrial Cancer: A Scoping Review
Current Nutrition Reports (2022)
-
Endometriosis and risk of ovarian and endometrial cancers in a large prospective cohort of U.S. nurses
Cancer Causes & Control (2017)
-
Coffee and cancer risk: A meta-analysis of prospective observational studies
Scientific Reports (2016)
-
Green tea, black tea consumption and risk of endometrial cancer: a systematic review and meta-analysis
Archives of Gynecology and Obstetrics (2016)
-
Coffee consumption and risk of endometrial cancer: a dose-response meta-analysis of prospective cohort studies
Scientific Reports (2015)