Abstract
Vaccines against the human papillomaviruses (HPV) that cause around 70% of cervical cancer cases worldwide are highly efficacious when administered before infection with the viruses, which occurs soon after initiation of sexual activity. Despite recommendations from key public health bodies that the primary target population for HPV vaccination should be young adolescent girls, numerous articles have suggested widening the target age group to include older adolescent girls and adult women. These articles cite evidence of efficacy and cost-effectiveness when making recommendations, and they rarely take into account the difficult resource-allocation issues faced by decision makers in low-income countries. Authors and sponsors of these articles are usually from high-income countries and sometimes include vaccine manufacturers. This review discusses the strengths and weaknesses of several types of evidence offered by these papers in support of vaccination of a broad age range of girls and women. It concludes that the greatest public health benefit and value for resources will come from vaccinating girls before sexual debut and exposure to HPV, particularly in low-resource areas.
Similar content being viewed by others
Main
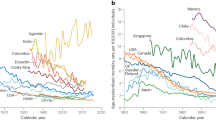
New technologies based on the discovery that cervical cancer is caused by oncogenic human papillomaviruses (HPV) have the potential to become the most effective tools for cervical cancer prevention in low-income countries. These countries shoulder the highest burden of this disease (Ferlay et al, 2010) and yet have almost no screening programmes – the key to the reductions in cervical cancer deaths in high-income countries over the past 40–50 years. The new technologies include HPV vaccines against the viral types responsible for at least 70% of cervical cancers and HPV screening tests that before long will be cheaper and easier to implement in developing countries than the Pap smears that revolutionised prevention in industrialised countries.
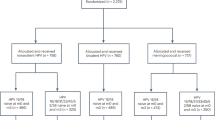
Two prophylactic vaccines have been approved by several regulatory authorities and are licensed in over 100 countries worldwide – a quadrivalent vaccine against HPV types 6, 11, 16, and 18 and a bivalent vaccine against types 16 and 18. Randomised clinical trials demonstrated at least 93% efficacy against infections and precancerous cervical lesions caused by HPV types 16 and 18, the oncogenic types targeted by the vaccines, in young women with no evidence of current infection or previous exposure to these types (The FUTURE II Study Group, 2007; Paavonen et al, 2009). Human papillomavirus types 6 and 11 are responsible for most cases of genital warts. Analyses that included all women in the trials regardless of current or past HPV exposure resulted in significantly lower efficacy, on the order of 50% or less, suggesting that vaccinating before sexual debut will provide more value for resources used.
The pivotal trials of the two vaccines did not include girls younger than 15 years, but immuno-bridging studies showed that vaccinating girls aged 9–14 years resulted in antibody titres that were not inferior to those in the efficacy trials and were usually much higher (Pedersen et al, 2007). This finding, along with safety data, was essential for approvals and subsequent recommendations for girls as young as 9 or 10 to receive the vaccines. Based on the efficacy of the vaccines, the cost of vaccinations (including programme costs), the likelihood of achieving high coverage and the resulting cost-effectiveness for various groups, key public health bodies, including the World Health Organization (WHO), (World Health Organization, 2009) have recommended that highest priority be vaccinating girls before initiation of sexual activity.
Despite this global recommendation, numerous articles have suggested widening the target age group to include older girls and adult women, raising policy questions with regard to the best use of scarce resources. We conducted a critical review of the literature to weigh the strengths and weaknesses of evidence used to support recommendations for vaccinating beyond the age of sexual debut, and to propose likely benefits and drawbacks associated with various recommendations if applied in public health programmes in low-resource settings. The analysis is intended to aid policymakers in developing countries that are deciding on populations to include for HPV vaccinations in their immunisation programmes.
Methods
We performed a systematic PubMed search of English-language literature for original papers in the 5 years preceding July 2011, and for reviews in the 3 most recent years in major scientific journals, excluding those such as nursing and family practice publications. Search terms included combinations of the following: HPV vaccination, HPV infection, cost-effectiveness, efficacy, age, recommendations, and developing country. Subsequently we looked at papers cited in those found in the PubMed search. Papers on the epidemiology of HPV infection and on vaccine clinical trials were also reviewed. Articles with the major focus on the following topics were excluded: vaccinating males, acceptability, vaccine controversy, HIV-positive women, molecular biology, immune mechanisms, screening, genotype distribution, sexual behaviour, vaccination coverage, and cancers other than cervical cancer.
Findings
Most papers that address the question of the appropriate age for HPV vaccination endorse the WHO recommendations for young adolescent girls as the primary target group, but many also advocate for vaccinating women after sexual debut, without differentiating between high- and low-resource settings. Recommendations for vaccinating after initiation of sexual activity generally are based on interpretations of two types of evidence: vaccine efficacy or cost-effectiveness. In Table 1, we present our overall conclusions from the literature assessed for this review. Vaccinating girls and women older than the primary target group could entail a 5- to 30-fold increase in the number of people to be vaccinated – depending on how many additional age groups were included – and an associated increase in burden on health personnel, cold chain, and other infrastructure, in addition to greater vaccine costs. However, catch-up efforts (up to approximately age 18) could be desirable in some low-resource countries where HPV vaccination may be lifesaving in adolescent girls whose future access to cervical screening is uncertain. Concerns that women might forego screening where it is available, because they believe vaccine is fully protective, become more important as women get older.
Our interpretation of the comparisons in Table 1 is that for resource-poor areas, drawbacks far outweigh benefits for vaccinating after sexual initiation. Why, then, do some authors still recommend vaccinating older girls and adult women? We analysed interpretations of vaccine efficacy – and the associated topic of the natural history of infection – and cost-effectiveness in the papers identified in our literature search.
Recommendations based on interpretations of vaccine efficacy
Of the 18 papers discussing the topics of vaccine efficacy and HPV infection, 5 gave unqualified support for vaccinating all ages; 5 expressed qualified support for a range of ages not exceeding 26 years; 1 indicated benefit for women up to 45 years; and 7 emphasised vaccinating before sexual debut. Only 3 papers discussed the situation in developing countries, with all recommending vaccination before sexual debut in these settings (Garland and Smith, 2010; Stanley, 2010; Elit et al, 2011) (see Table 2).
We noted four main arguments in this literature for vaccinating sexually active women; these are evaluated below. Our review provides counter-arguments to pro-vaccination arguments 1 and 2 and no support for argument 4, while recognising that argument 3 is still unsettled.
Argument number 1
Prevention of HPV infection, rather than cervical intraepithelial neoplasia grade 2 or worse (CIN2+) lesions, is equally acceptable as a vaccine efficacy endpoint for women older than age 26 years as it is for younger women.
Counter-argument number 1
The only data on the efficacy of HPV vaccine in women who are 27–45 years old derive from a randomised clinical trial of the quadrivalent vaccine (Castellsague et al, 2011) where the primary efficacy endpoint was the combined incidence of persistent infection, CIN, and external genital lesions related to HPV 6/11/16/18. Although the efficacy against the combined endpoint after 4 years of follow-up was statistically significant in both per-protocol-for-efficacy and intention-to-treat (ITT) populations, the CIN2+ outcomes in the ITT population, which more closely resembles older women who would be vaccinated in catch-up programmes, do not mirror the combined endpoint results (based primarily on infection) as they generally do among younger women in other trials. There were 21 cases of CIN2+ in the vaccine group and 27 in the placebo group (approximately 1% in each group) – a non-statistically significant difference.
The inadequacy of using HPV infection as the primary endpoint for efficacy in women over age 26 years is underscored by the refusal of the US Food and Drug Administration to grant approval for the quadrivalent vaccine for women aged 27–45 based on data from the above-mentioned trial of women up to age 45 years (Roberts, 2011).
Argument number 2
Some sexually active women will not yet have been infected by either, or at least not by both, of the oncogenic HPV types included in the vaccines (types 16 and 18), or in the case of the quadrivalent vaccine, may not have been infected by HPV types 6 or 11, which cause most genital warts (Wright et al, 2008; Adams et al, 2009; Basu et al, 2009).
Counter-argument number 2
Young sexually active women are less likely than somewhat older women to have been infected with both oncogenic vaccine virus types, but the incidence of new infections increases rapidly with age up to around age 25 years, at least in most high- and intermediate-resource areas investigated, and then declines (Franceschi et al, 2006). As the vaccines have no effect on current infections (Hildesheim and Herrero, 2007), vaccinating sexually active women runs the risk of having little benefit among these women who are young and more likely to have active infections.
In the one reported trial on vaccine efficacy in older women (Castellsague et al, 2011), the very low rates of CIN2+ or external genital lesions in HPV-naïve women in the placebo group suggest that whether older women have been infected with all vaccine types or not, they are at very low risk of incident disease at this time in their lives.
To translate recommendations for vaccinating before sexual debut into plans for vaccinating at or before a specific age, decision makers require information on the age of sexual debut in their countries or areas. Reports on sexual practices in the world indicate that very early intercourse might be occurring in adolescence, with median age of sexual debut in the mid-teens in many countries (e.g., Singh et al, 2000). This means that 50% of young women initiated sexual activity before these ages; thus, vaccination programmes aiming to protect the maximum number of young adolescents must plan to vaccinate well before the mid-teens.
Argument number 3
Natural immunity cannot protect against re-infection by the same HPV type, but vaccination can.
Counter-argument number 3
Conclusive evidence on whether natural immunity is protective is not yet available. Indirect evidence of possible natural immunity comes from an analysis of the subpopulation of seropositive women (those with evidence of previous HPV infection) in a large clinical trial of the bivalent vaccine (Szarewski et al, 2011). Although the authors highlighted vaccine efficacy in women seropositive and DNA negative, the confidence intervals for significance at the 5% level included zero (not significant) for one analysis, and were very wide in another. An interesting result not called out by the authors was the finding that among women in the placebo group, those who were seropositive and DNA negative had about half the rate of CIN2+ as those who were seronegative and DNA negative, a hint that natural immunity might be providing protection.
Evidence is also lacking on whether HPV vaccines protect against re-infection by or re-activation of vaccine viral types. In a sub-analysis of women who were seropositive and DNA negative in three clinical trials of the quadrivalent vaccine (Olsson et al, 2009), there were no cases of CIN in the vaccine groups, but seven in the placebo groups. However, statistical significance for vaccine efficacy was only reached when including cases of CIN1, which is currently considered a mere marker of HPV infection. Efficacy against CIN2+ was not shown.
Argument number 4
Older women have high risk for new infections, and those who develop a new infection are at high risk for progression (Basu et al, 2009; Poppe et al, 2010).
Counter-argument number 4
In a report from a study of more than 8000 women in Costa Rica, regardless of the woman’s age, newly detected infections were associated with very low absolute risk of persistence or CIN2+ (Rodriguez et al, 2010). On the other hand, prevalent infections in older women, especially in inadequately screened populations, are much more likely to be persistent infections (acquired years earlier) than those in younger women, and the vaccines have no effect on persistent infections (Hildesheim and Herrero, 2007), making it clear that any comparison of CIN2+ risk across women of different ages should separate incident from persistent infections.
A recent report offers indirect evidence that older women may actually be at lower risk of disease due to new HPV infection. This re-analysis that pooled data from 20 studies on cervical cancer found that the risk of cervical cancer increases as the square of time since first intercourse, using first intercourse as a reasonable proxy for first exposure to HPV (Plummer et al, 2011). According to this report, the relationship between HPV infection and cervical cancer resembles that found for other cancers caused by strong early-stage carcinogens (e.g., tobacco smoking and lung cancer), with incidence rates proportional to a power of the duration of exposure to the relevant carcinogenic agent and with a delay between infection and cancer. The multi-stage cancer model postulates that a certain number of cellular changes must occur for malignant transformation, which explains the delay and predicts that new HPV infections acquired later in life are less likely than those incurred earlier to develop into cervical cancer. In addition, epidemiological and animal data suggest that, although HPV is the cause of cervical cancer, steroid sex hormones are the fuel of HPV-driven carcinogenesis in the cervix. In populations where screening has not distorted the age distribution of the disease, cervical cancer shows a flattening in age-specific incidence rates at the time menopausal changes start (Plummer et al, 2011). Thus, vaccinating women at this time may have little benefit because the falling levels of steroid sex hormones appear to diminish the potential for malignant transformation of new HPV infections.
Authorship of papers with age recommendations for HPV vaccinations based on efficacy
In analysing the 18 papers on the efficacy of HPV vaccines as well as the literature on HPV infection, we noted that most are written by investigators in high-resource countries, where governments can afford to implement vaccination programmes and private individuals may wish to pay for vaccination even if the benefit is minimal. Some were funded by vaccine manufacturers or co-authored by company employees (Table 2). Of the 18 papers, 5 had such potential conflicts of interest, and 3 of these recommended vaccinating unlimited ages. All except 1 (Basu et al, 2009) of the 18 articles were authored by investigators in high-income countries.
Recommendations based on interpretation of cost-effectiveness
Cost-effectiveness studies use mathematical models that combine disease and natural history parameters, vaccine-efficacy findings, and estimated vaccine and health system delivery costs to compute the extra quantity and quality of life provided by an intervention. The intervention is usually considered cost-effective if the cost per quality-adjusted life year (QALY) is less than or equal to the gross domestic product per capita of a given country.
Many cost-effectiveness analyses have modelled HPV vaccination for young adolescent girls, usually 12 years of age, and have found that vaccination at this age is cost-effective in high-income countries, and a 2008 study on cost-effectiveness of vaccinating girls before the age of 12 years in 72 developing countries concluded that vaccination could be cost-effective if the price of vaccine per dose was US$2 (Goldie et al, 2008). Our search identified 13 papers that evaluated vaccinating beyond age 12 years, all modelling cost-effectiveness in high- or middle-income countries (see Table 3). Six of these found vaccination cost-effective up to ages 24–26 years, the maximum ages studied, and one that modelled to age 50 years found that vaccinating to age 25 years, but not beyond, was cost-effective. Three found that vaccinating up to ages 15, 18, or 21 could be cost-effective. Another paper, which considered women up to 35 years of age in several countries, found vaccination most cost-effective up to 15–19 years, depending on the age for the peak of HPV infection in the region under question. Two papers reported that only vaccinating girls ⩽12 years old was cost-effective. Thus, in the few studies that have modelled beyond age 26, none has found including older ages to be cost-effective.
As the papers we reviewed are mathematical modelling studies, the reasons for disparate results must be found in study assumptions. Factors that can change the results of studies include:
-
Basic model structure: static (e.g., Markov) or dynamic (e.g., population- or individual-based)
-
Duration of vaccine protection
-
Natural infection rates in population
-
Degree of natural immunity after infection
-
Definition of ‘cost-effective’
-
Price estimated for vaccine
-
Inclusion and estimate of administrative costs
-
Effect and cost of screening
-
Health outcomes included (e.g., warts, male outcomes for quadrivalent vaccine, other HPV-related cancers)
-
Impact on quality of life for cervical lesions, genital warts
Estimates of cost per QALY can increase dramatically when using less favourable assumptions for these factors; for example, reduced duration of vaccine protection, reduced vaccine efficacy, fewer health outcomes, or reduced impact of health outcomes on quality of life. Virtually all studies on the quadrivalent vaccine include outcomes on genital warts and this typically lowers the cost per QALY.
In a modelling study of mid-adult women in the United States, researchers found that HPV vaccination provided only nominal benefits in the context of current screening recommendations and practice among women aged 35–45 years (Kim et al, 2009). A review of cost-effectiveness studies included a report that less than about 5% of the total health benefits of vaccinating 12- to 44-year-olds were attributable to vaccination of women after their mid-twenties (Grant et al, 2011).
Authorship of papers with age recommendations for HPV vaccinations based on cost-effectiveness
All 13 of the papers that met our search criteria for cost-effectiveness presented analyses for middle- or high-income countries. Eight of the studies were funded by a vaccine manufacturer or had at least two authors who were employees of a vaccine company (Table 3). Of these, seven found vaccinating to ages 24–26 years to be cost-effective. The other paper reported that depending on the region, HPV vaccination could be cost-effective to age 15, 17, or 19 (Suarez et al, 2008). On the other hand, in the group of papers not directly funded by vaccine manufacturers or authored by employees, the highest age for which vaccinating was found to be cost-effective was 21 (one study), and two studies found that only vaccinating 12-year-old girls was cost-effective.
Discussion
WHO guidance
The WHO position paper on HPV vaccines states that as HPV vaccines are prophylactic, the largest impact of vaccination is expected from high coverage of young adolescent girls before first sexual activity and exposure to the viruses, and recommends that females aged 9 or 10 through 13 be the primary target population (World Health Organization, 2009). With this clear guidance, it is puzzling that many authors continue to recommend vaccinating older girls and adult women without acknowledging the implications for resources in low- and middle-income countries. Although some young women will benefit from vaccination after sexual initiation because they have not yet been infected with all vaccine HPV types, it is much more efficient and cost-effective to vaccinate earlier.
Efficacy
Vaccine efficacy against CIN2+ caused by HPV16/18 in the pivotal clinical trials for both the quadrivalent (The FUTURE II Study Group, 2007) and bivalent (Paavonen et al, 2009) vaccines was around 50% in women aged 15–26 years and 22.4% in older women (Castellsague et al, 2011) when total trial populations were analysed. But even these mixed, ITT populations do not approximate a ‘real world’ setting, because stringent trial inclusion criteria will not apply in public immunisation programmes.
Cost-effectiveness
For high-income countries with well-managed cervical cancer screening programmes, offering HPV vaccinations to sexually active women in some age groups (Jit et al, 2008; Usher et al, 2008) may lead to savings in screening programmes and may shorten the time by which a lower incidence of precancerous lesions and, eventually, a lower rate of cervical cancer are seen. Although these are the very places where screening programmes provide excellent protection against cervical cancer, such countries may be able to afford the additional benefits of vaccinating young women.
In developing countries, where screening services are not available or have only been introduced in a few areas, one might argue that vaccinations among older adolescents and young women could speed up the rate at which cervical cancer incidence and deaths decline while screening programmes get underway. However, in these countries, the notion of cost-effectiveness does not always correspond to affordability or to best use of resources compared with other cost-effective interventions; factors such as population health needs and local priorities must also be considered.
The economic challenges of increasing vaccine purchases and the logistical difficulty of achieving high coverage among older girls and young women in developing countries raise serious concerns (World Health Organization, 2009). Recently the manufacturer of the quadrivalent vaccine announced that it will be available to the GAVI Alliance (GAVI) at a price of US$5 per dose, and the GAVI Board announced that it would take the first steps towards supporting the introduction of HPV vaccines in developing countries (GAVI Alliance, 2011). If GAVI is able to subsidise the vaccine cost for eligible low-income countries, vaccinations should become affordable even in very low-income settings for girls around the age of 12 years.
Feasibility of reaching different age groups with vaccine and alternatives
Vaccinating children beyond the ages for infant immunisations (the target population for HPV vaccination) in these regions is a challenge, but reaching girls of primary school ages is a credible strategy. As a result of Goals 2 and 3 of the Millennium Development Goals, girls’ attendance in primary school has climbed dramatically in all regions of the world making school-based delivery one of the most promising systems for achieving high coverage with the HPV vaccines in low-income countries.
In a broad range of socioeconomic settings, modelling has demonstrated that screening, with treatment when necessary, is a very practical and cost-effective approach for cervical cancer prevention for sexually active women even if performed only once, around age 35 years. In principle, Pap smear (where already in place and functioning well), HPV DNA screening tests, or less costly methods such as visual inspection may be worthwhile in low-resource areas.
Conclusions
While individual women may benefit from HPV vaccination after initiating sexual activity, the number not exposed to vaccine HPV types decreases steadily with time after sexual debut. The greatest public health benefit and value for resources will come from vaccinating girls before sexual debut and exposure to HPV, particularly in low-resource areas. Most papers that are favourable to vaccinating a broad age range of sexually active women are authored by investigators in high-income countries or are funded by vaccine manufacturers. These papers rely on very weak evidence of vaccine efficacy among women aged 27 years or older and they do not take into account the difficult resource-allocation issues faced by decision makers in low-income countries. Before broadening the WHO-recommended age range for public HPV vaccination programmes in their regions, policymakers should make sure that the vaccination is firmly in place for young adolescent girls who can benefit the most from it and concentrate on screening-based approaches for cervical cancer prevention among older women.
Change history
11 October 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adams M, Jasani B, Fiander A (2009) Prophylactic HPV vaccination for women over 18 years of age. Vaccine 27 (25-26): 3391–3394
Basu P, Ngan HY, Hseon TE (2009) HPV vaccination in women over 25 years of age: Asian Cervical Cancer Prevention Advisory Board recommendations. J Obstet Gynaecol Res 35: 712–716
Castellsague X, Munoz N, Pitisuttithum P, Ferris D, Monsonego J, Ault K, Luna J, Myers E, Mallary S, Bautista OM, Bryan J, Vuocolo S, Haupt RM, Saah A (2011) End-of-study safety, immunogenicity, and efficacy of quadrivalent HPV (types 6, 11, 16, 18) recombinant vaccine in adult women 24-45 years of age. Br J Cancer 105: 28–37
Castellsague X, Schneider A, Kaufmann AM, Bosch FX (2009) HPV vaccination against cervical cancer in women above 25 years of age: key considerations and current perspectives. Gynecol Oncol 115 (3 Suppl): S15–S23
Castle PE, Fetterman B, Akhtar I, Husain M, Gold MA, Guido R, Glass AG, Kinney W (2009) Age-appropriate use of human papillomavirus vaccines in the U.S. Gynecol Oncol 114 (2): 365–369
Chesson H (2010) Cost-effectiveness of quadrivalent HPV vaccination of adult women. Available at http://www.oralcancerfoundation.org/hpv/pdf/02-4-hpv.pdf
Dasbach EJ, Insinga RP, Elbasha EH (2008a) The epidemiological and economic impact of a quadrivalent human papillomavirus vaccine (6/11/16/18) in the UK. BJOG 115 (8): 947–956
Dasbach EJ, Largeron N, Elbasha EH (2008b) Assessment of the cost-effectiveness of a quadrivalent HPV vaccine in Norway using a dynamic transmission model. Expert Rev Pharmacoecon Outcomes Res 8 (5): 491–500
Elbasha EH, Dasbach EJ, Insinga RP (2007) Model for assessing human papillomavirus vaccination strategies. Emerg Infect Dis 13 (1): 28–41
Elbasha EH, Dasbach EJ, Insinga RP, Haupt RM, Barr E (2009) Age-based programs for vaccination against HPV. Value Health 12 (5): 697–707
Elit L, Jimenez W, McAlpine J, Ghatage P, Miller D, Plante M (2011) SOGC-GOC-SCC Joint Policy Statement. No. 255, March 2011. Cervical cancer prevention in low-resource settings. J Obstet Gynaecol Can 33 (3): 272–279
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Globocan 2008 V1.2, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet]. International Agency for Research on Cancer: Lyon, France, Available at http://globocan.iarc.fr
Franceschi S, Herrero R, Clifford GM, Snijders PJ, Arslan A, Anh PT, Bosch FX, Ferreccio C, Hieu NT, Lazcano-Ponce E, Matos E, Molano M, Qiao YL, Rajkumar R, Ronco G, de SS, Shin HR, Sukvirach S, Thomas JO, Meijer CJ, Munoz N (2006) Variations in the age-specific curves of human papillomavirus prevalence in women worldwide. Int J Cancer 119: 2677–2684
Garland SM, Smith JS (2010) Human papillomavirus vaccines current status and future prospects. Drugs 70 (9): 1079–1098
GAVI Alliance (2011) GAVI takes first steps to introduce vaccines against cervical cancer and rubella. GAVI Alliance. Available at http://www.gavialliance.org/library/news/press-releases/2011/gavi-takes-first-steps-to-introduce-vaccines-against-cervical-cancer-and-rubella/
Goldie SJ, O’Shea M, Campos NG, Diaz M, Sweet S, Kim SY (2008) Health and economic outcomes of HPV 16,18 vaccination in 72 GAVI-eligible countries. Vaccine 26: 4080–4093
Grant LA, Dunne EF, Chesson H, Markowitz LE (2011) Considerations for human papillomavirus (HPV) vaccination of mid-adult women in the United States. Vaccine 29: 2365–2370
Hildesheim A, Herrero R (2007) Human papillomavirus vaccine should be given before sexual debut for maximum benefit. J Infect Dis 196 (10): 1431–1432
Insinga RP, Dasbach EJ, Elbasha EH, Puig A, Reynales-Shigematsu LM (2007) Cost-effectiveness of quadrivalent human papillomavirus (HPV) vaccination in Mexico: a transmission dynamic model-based evaluation. Vaccine 26 (1): 128–139
Jit M, Choi YH, Edmunds WJ (2008) Economic evaluation of human papillomavirus vaccination in the United Kingdom. BMJ 337: a769
Kim JJ, Goldie SJ (2008) Health and economic implications of HPV vaccination in the United States. N Engl J Med 359: 821–832
Kim JJ, Ortendahl J, Goldie SJ (2009) Cost-effectiveness of human papillomavirus vaccination and cervical cancer screening in women older than 30 years in the United States. Ann Intern Med 151: 538–545
Kulasingam S, Connelly L, Conway E, Hocking JS, Myers E, Regan DG, Roder D, Ross J, Wain G (2007) A cost-effectiveness analysis of adding a human papillomavirus vaccine to the Australian National Cervical Cancer Screening Program. Sex Health 4 (3): 165–175
Lu B, Kumar A, Castellsague X, Giuliano AR (2011) Efficacy and safety of prophylactic vaccines against cervical HPV infection and diseases among women: a systematic review & meta-analysis. BMC Infect Dis 11: 13
Markowitz LE, Sternberg M, Dunne EF, McQuillan G, Unger ER (2009) Seroprevalence of human papillomavirus types 6, 11, 16, and 18 in the United States: National Health and Nutrition Examination Survey 2003-2004. J Infect Dis 200 (7): 1059–1067
Monsonego J, Cortes J, Greppe C, Hampl M, Joura E, Singer A (2010) Benefits of vaccinating young adult women with a prophylactic quadrivalent human papillomavirus (types 6, 11, 16 and 18) vaccine. Vaccine 28 (51): 8065–8072
Olsson SE, Kjaer SK, Sigurdsson K, Iversen OE, Hernandez-Avila M, Wheeler CM, Perez G, Brown DR, Koutsky LA, Tay EH, Garcia P, Ault KA, Garland SM, Leodolter S, Tang GW, Ferris DG, Paavonen J, Lehtinen M, Steben M, Bosch FX, Dillner J, Joura EA, Majewski S, Munoz N, Myers ER, Villa LL, Taddeo FJ, Roberts C, Tadesse A, Bryan J, Maansson R, Vuocolo S, Hesley TM, Saah A, Barr E, Haupt RM (2009) Evaluation of quadrivalent HPV 6/11/16/18 vaccine efficacy against cervical and anogenital disease in subjects with serological evidence of prior vaccine type HPV infection. Hum Vaccin 5: 696–704
Paavonen J (2010) At what age should we be vaccinating for human papillomavirus? Gynecol Obstet Invest 70 (4): 233–236
Paavonen J, Naud P, Salmeron J, Wheeler CM, Chow SN, Apter D, Kitchener H, Castellsague X, Teixeira JC, Skinner SR, Hedrick J, Jaisamrarn U, Limson G, Garland S, Szarewski A, Romanowski B, Aoki FY, Schwarz TF, Poppe WA, Bosch FX, Jenkins D, Hardt K, Zahaf T, Descamps D, Struyf F, Lehtinen M, Dubin G, Greenacre M (2009) Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet 374: 301–314
Pedersen C, Petaja T, Strauss G, Rurnke HC, Poder A, Richardus JH, Spiessens B, Descamps D, Hardt K, Lehtinen M, Dubin G (2007) Immunization of early adolescent females with human papillomavirus type 16 and 18 L1 virus-like particle vaccine containing AS04 adjuvant. J Adolesc Health 40: 564–571
Plummer M, Peto J, Franceschi S (2011) Time since first sexual intercourse and the risk of cervical cancer. Int J Cancer 130 (11): 2638–2644
Poppe WA, Simon PH, De Ridder MR (2010) Why consider human papillomavirus vaccination in older women? Gynecol Obstet Invest 70 (4): 237–243
Prymula R, Anca I, André F, Bakir M, Czajka H, Lutsar I, Mészner Z, Salman N, Šimurka P, Usonis V (2009) Central European Vaccination Advisory Group (CEVAG) guidance statement on recommendations for the introduction of HPV vaccines. Eur J Pediatr 168 (9): 1031–1035
Roberts JN (2011) Clinical Review of Biologics License Application Supplement STN# 125126/773—mid-adult women indication for Gardasil. Food and Drug Administration. Available at http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm094042.htm
Rodriguez AC, Schiffman M, Herrero R, Hildesheim A, Bratti C, Sherman ME, Solomon D, Guillen D, Alfaro M, Morales J, Hutchinson M, Katki H, Cheung L, Wacholder S, Burk RD (2010) Longitudinal study of human papillomavirus persistence and cervical intraepithelial neoplasia grade 2/3: critical role of duration of infection. J Natl Cancer Inst 102: 315–324
Singh S, Wulf D, Samara R, Cuca YP (2000) Gender differences in the timing of first intercourse: data from 14 countries. Int Fam Plan Perspect 26: 21–28
Solomon D, Castle P, Hildesheim A, Katki HA, Schiffman M, Wacholder S (2009) HPV vaccination in women aged 24–45 years. Lancet 374 (9697): 1239–1240
Stanley M (2010) Prophylactic human papillomavirus vaccines: will they do their job? J Intern Med 267 (3): 251–259
Suarez E, Smith JS, Bosch FX, Nieminen P, Chen CJ, Torvinen S, Demarteau N, Standaert B (2008) Cost-effectiveness of vaccination against cervical cancer: a multi-regional analysis assessing the impact of vaccine characteristics and alternative vaccination scenarios. Vaccine 26 (Suppl 5): F29–F45
Szarewski A, Poppe WA, Skinner SR, Wheeler CM, Paavonen J, Naud P, Salmeron J, Chow SN, Apter D, Kitchener H, Castellsague X, Teixeira JC, Hedrick J, Jaisamrarn U, Limson G, Garland S, Romanowski B, Aoki FY, Schwarz TF, Bosch FX, Harper DM, Hardt K, Zahaf T, Descamps D, Struyf F, Lehtinen M, Dubin G (2011) Efficacy of the human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine in women aged 15-25 years with and without serological evidence of previous exposure to HPV-16/18. Int J Cancer 131 (1): 106–116
The FUTURE II Study Group (2007) Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med 356: 1915–1927
Usher C, Tilson L, Olsen J, Jepsen M, Walsh C, Barry M (2008) Cost-effectiveness of human papillomavirus vaccine in reducing the risk of cervical cancer in Ireland due to HPV types 16 and 18 using a transmission dynamic model. Vaccine 26: 5654–5661
Westra TA, Rozenbaum MH, Rogoza RM, Nijman HW, Daemen T, Postma MJ, Wilschut JC (2011) Until which age should women be vaccinated against HPV infection? Recommendation based on cost-effectiveness analyses. J Infect Dis 204 (3): 377–384
World Health Organization (2009) Human papillomavirus vaccines. WHO position paper. Wkly Epidemiol Rec 84: 118–131
Wright TC, Huh WK, Monk BJ, Smith JS, Ault K, Herzog TJ (2008) Age considerations when vaccinating against HPV. Gynecol Oncol 109 (2 Suppl): S40–S47
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Tsu, V., Murray, M. & Franceschi, S. Human papillomavirus vaccination in low-resource countries: lack of evidence to support vaccinating sexually active women. Br J Cancer 107, 1445–1450 (2012). https://doi.org/10.1038/bjc.2012.404
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.404