Abstract
Aim:
To evaluate the effect of inhaled formoterol-budesonide on airway remodeling in adult patients with moderate asthma.
Methods:
Thirty asthmatic patients and thirty control subjects were enrolled. Asthmatic subjects used inhaled Symbicort 4.5/160 μg twice daily for one year. The effect of formoterol-budesonide on airway remodeling was assessed with comparing high-resolution computer tomography (HRCT) images of asthmatic patients and controls, as well as expression levels of cytokines and growth factors, inflammatory cell count in induced sputum, and airway hyper-responsiveness.
Results:
The differences in age and gender between the two groups were not significant. However, differences in FVC %pred, FEV1 %pred, and PC20 between the two groups were significant. After treatment with formoterol-budesonide, the asthma patients' symptoms were relieved, and their lung function was improved. The WT and WA% of HRCT images in patients with asthma was increased, whereas treatment with formoterol-budesonide caused these values to decrease. The expression of MMP-9, TIMP-1, and TGF-β1 in induced sputum samples increased in patients with asthma and decreased dramatically after treatment with formoterol-budesonide. The WT and WA% are correlated with the expression levels of cytokines and growth factors, inflammatory cell count in induced sputum, and airway hyper-responsiveness, while these same values are correlated negatively with FEV1/FVC and FEV1%.
Conclusion:
Formoterol-budesonide might interfere in chronic inflammation and airway remodeling in asthmatic patients. HRCT can be used to effectively evaluate airway remodeling in asthmatic patients.
Similar content being viewed by others
Introduction
Bronchial asthma is a chronic inflammatory disease of the airways that is characterized by respiratory symptoms associated with variable airflow obstruction, airway hyper-responsiveness, and airway remodeling1. Airway remodeling refers to airway structural alterations that likely have clinical consequences. Epithelial shedding, goblet cell and submucosal gland hyperplasia, increased accumulation of smooth muscle bundles and extracellular matrix (ECM), microvascular alterations, cartilage changes, and airway wall edema are the main histological features of asthmatic airways2. The ECM remains in a state of dynamic equilibrium of new synthesis and degradation due to the action of matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs)3 as well as growth factors such as transforming growth factor β1 (TGF-β1)4. Of the MMP family, MMP-9 is one of the major proteinases involved in airway inflammation and bronchial remodeling in asthma5, 6. TIMP-1, the major inhibitor of MMP-9, has also been postulated to act in airway remodeling. In addition, TGF-β1 induces ECM deposition and thus contributes critically to fibrosis in the airways and lungs4.
High-resolution computed tomography (HRCT) has made it possible to accurately measure airway dimensions. Quantitative analysis of bronchial wall thickness (WT), airway narrowing, and bronchodilation can be performed for patients with pulmonary diseases, such as bronchial asthma, by measuring airway dimensions7. Numerous image analysis techniques have been developed for measurement of airway dimensions8, 9, 10. These techniques make it possible to accurately measure changes in airway dimensions longitudinally or after intervention by matching CT sections of the same airways in a non-invasive way.
Corticosteroids are effective in controlling asthma. Corticosteroids reduce airway eosinophilic inflammation and expression of GM-CSF, IL-4, IL-5, IL-11, and IL-1711. The combination of inhaled corticosteroids (ICSs) with long-acting inhaled β2-agonists (LABAs) has been recommended to improve the effectiveness of asthma treatment12. Formoterol-budesonide is preferentially delivered and deposited in the distal airways. However, it is not clear whether formoterol-budesonide deposition in peripheral airways can influence airway remodeling. The present study evaluated whether formoterol-budesonide can influence airway remodeling. To this end, we examined the expression levels of MMP-9, TIMP-1, and TGFβ1 in the sputum of patients with asthma compared to those treated with formoterol-budesonide. Thin-section CT was used to evaluate the degree of airway remodeling.
Materials and methods
Study design
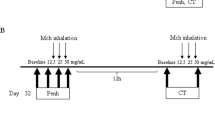
A single-center, open-label study was conducted in adult patients with moderate asthma to evaluate the effect of inhaled formoterol-budesonide on peripheral remodeling. The Ethics Committee of West China Hospital, Sichuan University, approved the study, and all subjects gave written informed consent. Patients and control subjects who met the inclusion and exclusion criteria had a baseline thin-section CT scan, an induced sputum collection, and a lung function exam. Patients were then treated with formoterol-budesonide (Symbicort, AstraZeneca, Lund, Sweden; 4.5/160 μg twice daily) for one year. After treatment for one year, another thin-section CT scan, induced sputum collection, and lung function exam were conducted. The effect of formoterol-budesonide on airway remodeling was measured by comparisons of CT images, expression levels of cytokines and growth factors in induced sputum, and airway hyper-responsiveness.
Subjects
Thirty patients were diagnosed with moderate asthma according to the Global Initiative for Asthma (GINA) 2006 [http://www.ginasthma.org], and thirty more were used as control subjects. Patients with chronic bronchitis or any major comorbid disease that might affect asthma disease activity, such as HIV, metastatic cancer, and congestive heart failure were excluded from the study. Subjects with moderate asthma had to fulfill the following criteria: daily symptoms; exacerbations that may affect activity and sleep; nocturnal symptoms more than once a week; daily use of inhaled short-acting β2-agonist; FEV1 or PEF 60% to 80% predicted; and PEF or FEV1 variability >30%. Asthmatic subjects had not used any steroids within the 180 d preceding the beginning of the study. Healthy control subjects were recruited from hospital personnel who answered in a screening questionnaire that they did not have respiratory symptoms and who had FEV1 values of more than 80% of the predicted value, PC20 methacholine of more than 10 mg/mL, and normal findings on simple chest radiograms. All subjects were nonsmokers or ex-smokers of at least 2 years with a smoking history of less than 15 pack-years. None of the subjects had respiratory tract infections in the 2 weeks preceding the two follow-ups.
Sputum collection and procession
Induced sputum was obtained according a previously described method, with slight modification13. The sputum was examined within 1 h. The entire sputum sample was inspected for salivary contamination under an inverted microscope; all portions that appeared free of salivary contamination were placed in a 15-mL polystyrene tube using forceps. Dithiothreitol (a final concentration of 1 mmol/L) was freshly diluted in distilled water equal to 4 times the sputum weight and added to the sputum sample. The mixture was vortexed for 30 s and then placed on a bench rocker and rocked for 15 min. A further 4 volumes of Dulbecco's phosphate-buffered saline was added to stop the effect of dithiothreitol and rocked for 5 min. The suspension was filtered through a 70-μm cell strainer. The resulting suspension was centrifuged at 800×g for 10 min and the supernatant was aspirated and stored in Eppendorf tubes at −70°C in the presence of aprotinin. All subjects produced an adequate specimen of sputum; a sample was considered adequate if the patient was able to expectorate at least 2 mL of sputum.
Total cell counts were performed in a hemocytometer and expressed as millions per milligram of selected induced sputum. The proportion of salivary squamous cells was noted. Differential cell counts were performed by counting 400 cells on May Grünwald Giemsa-stained slides. Results were expressed as a percentage of the total cell count. Slides were coded and cell counts were performed by an expert observer who did not know the clinical characteristics of the patients. Only samples with cell viability >70% and squamous cell contamination <20% were considered adequate.
TGF-β1, MMP-9, and TIMP-1 concentrations were measured with enzyme-linked immunosorbent assay kits (R&D Systems Inc, Minneapolis, MN, USA; Bender MedSystems GmbH, Vienna, Austria; BioSource International Inc, Camarillo, CA, USA) according to the manufacturer's guidelines. The minimum detectable levels of TGF-β1, MMP-9, and TIMP-1 in these assay systems were 1.7 pg/mL, 0.8 ng/mL, and 1 ng/mL, respectively. All results were corrected for the volume and dilution of sputum or saliva.
High-resolution computed tomography (HRCT) protocol
HRCT was performed using a multi-detector row spiral CT scanner (Sensation 16, Siemens Medical System, Erlangen, Germany) with sixteen detector arrays. Patients were scanned in the supine position during one breath hold at deep inspiration. The scans were obtained with 16×1 mm collimation at 10 mm intervals, with a table feed of 11 mm per 0.5 s scanner rotation. Scanning was performed at 120 kV and 80 mAs, regardless of patient size, using a 512×512 matrix. Images were reconstructed with a bone algorithm and a 512×512 matrix. Images were viewed at a window level of -450 HU and a width of 1500 HU. CT scans were interpreted by two radiologists who were unaware of the clinical history of the patients and control subjects.
Bronchial wall thickening was assessed as follows. All visible sections of bronchi were counted at five levels in the pulmonary fields (right and left lungs), and all circular (complete circles or at least two thirds of a circle) and longitudinal bronchi except the hilar bronchi were included. The five levels were 1 cm above the carina (Level 1), 1 cm below the carina (Level 2), the right pulmonary vein (Level 3), 3 cm below the top of the pulmonary vein (Level 4), and above the right side of the diaphragm (Level 5). The bronchial wall thickness at these five levels was measured. The following parameters were determined with semiautomatic image-processing program: luminal area (LA), total airway area (TA), short axis of lumen (LSD), and short axis of total airway (TSD). In airways in which an adjacent vessel or a branching of a small bronchus abutted the boundary of the airway, an extrapolated line was traced. Airway wall area (WA) was calculated as TA-LA and WT was calculated as (TSD-LSD)/2. Relative WA (WA% = [WA/TA]×100) was also calculated.
Statistical analysis
All data are expressed as the mean±SEM. Statistical analyses were performed using SPSS 12.0 software. Statistical significance was analyzed with one-way analysis of variance (ANOVA) followed by the Student-Newman-Keuls test to isolate significant difference. Chi-square test and Pearson correlation analysis were also used. A P value less than 0.05 (two-tailed test) was considered statistically significant.
Results
Subjects
The sixty patients were divided into an asthma group and a control group. The patients' demographic characteristics are listed in Table 1.
The differences in age and gender between the two groups were not significant. Otherwise, the differences of FVC %pred, FEV1 %pred, PC20, V75 %pred, V50 %pred, and V25 %pred were significant between the two groups. After treatment, asthma symptoms had been relieved, and the differences of lung function were significant.
Evaluations of cytokines in induced sputum
The levels of MMP-9, TIMP-1, and TGF-β1 were increased, and there was a tendency for a higher MMP-9/TIMP-1 ratio in patients with asthma. After treatment with formoterol-budesonide, the levels of cytokines decreased significantly (Table 2).
HRCT evaluation
The bronchial wall thickening based on the number of bronchi counted on HRCT scans is shown in Figure 1 and Table 3. The WT and WA% in the asthma group before treatment were significantly increased compared to data from the control group. After treatment, the WT and WA% of the patients with asthma decreased, and the differences were also significant compared to the data before treatment.
Evaluation of airway remodeling by HRCT in five levels. (A) Following parameters were determined with semiautomatic image-processing program: luminal area (LA), total airway area (TA), short axis of lumen (LSD), and short axis of total airway (TSD). In airways in which adjacent vessel or branching of small bronchus abutted boundary of airway, extrapolated line was traced by one radiologist. Airway wall area (WA) was calculated as TA-LA, and airway wall thickness (WT) was calculated as (TSD-LSD)/2. Relative WA (WA%=[WA/TA]*100%) and ratio of airway WT to total diameter (D) (WT/D=WT/TSD) were calculated. (B) The HRCT images of a 35-year-old man in control group. (C) The HRCT images of a 38-year-old man with moderate, persistent symptoms of asthma pre-treatment. (D) The HRCT images of the same 38-year-old man with moderate, persistent symptoms of asthma after treatment.
Correlation analysis
The WT and WA% of patients with asthma were well correlated with hyper-responsiveness, degree of infiltration of inflammatory cells, and concentration of chemokines involved in airway remodeling, while being negatively correlated with FEV1/FVC and FEV1%. Importantly, the WT and WA% of patients with asthma were more correlated in the proximal airway than in the distal airway (Table 4).
Discussion
We demonstrated that FEV1/FVC and FEV1% decreased, while airway hyper-responsiveness, degree of infiltration of inflammatory cells, and concentration of chemokines involved in airway remodeling increased in patients with moderate asthma compared to patients in a control group. Formoterol-budesonide can interfere in the chronic inflammation and remodeling in the airway as well as relieve asthmatic symptoms. The WT and WA% in the moderate asthma group before treatment were significantly increased compared to data in the control group. After treatment, the WT and WA% of the asthmatic patients decreased. The WT and WA% of patients with asthma were well correlated with hyper-responsiveness, degree of infiltration of inflammatory cells, and concentration of chemokines involved in airway remodeling, while being negatively correlated with data of FEV1/FVC and FEV1%. Importantly, the WT and WA% of patients with asthma were more correlated in the proximal airway than in the distal airway.
Chronic inflammation and airway remodeling is an important feature of asthma, including infiltration of eosinophils, lymphocytes, and mast cells in the airway and the structural changes of airway walls. Observing airway inflammation and airway remodeling can directly evaluate the severity of asthma and effect of treatment14. Biopsy or bronchoalveolar lavage through a bronchofibroscope is an invasive procedure that is risky and has poor tolerance and repeatability. The clinical administration of bronchofibroscope is limited, and it is only suitable for scientific research in patients with mild asthma. Therefore, evaluation of clinical severity and treatment effect are determined indirectly by clinical manifestations and lung function, methods that are flawed. When bronchodilators are used to improve airway reactivity, symptoms and lung function do not reflect the degree of airway inflammation at that time.
As a non-invasive technology that can objectively reflect the state of airway inflammation, induced sputum technique has been applied to study the pathogenesis and development of airway inflammatory disease15, 16. As a semi-quantitative technology, it is similar to biopsy of bronchial mucosa and bronchoalveolar lavage for determining the levels of inflammatory cytokines. In our study, there were increased levels of MMP-9, TIMP-1, and TGF-β1 as well as a tendency for a higher MMP-9/TIMP-1 ratio in patients with asthma. After treatment with formoterol-budesonide, the levels of the increased cytokines decreased significantly. The counts of neutrophils and eosinophils reflect the degree of chronic inflammation, while the levels of TGF-β1, MMP-9, and TIMP-1 reflect the degree of airway remodeling3, 4, 5, 6. TGF-β1 is a 25-kDa homologous molecular dimer that can promote fibroblasts to differentiate into myofibroblasts, which can then secrete interstitial collagen17. TGF-β1 can stimulate the synthesis and deposition of the ECM and inhibit enzymatic degradation of matrix proteins, thus regulating the expression of cell-surface matrix protein receptors. In asthmatic airways, in situ hybridization and immunohistochemical studies indicate that TGF-β1 is increased and associated predominantly with submucosal and inflammatory cells, including fibroblasts, smooth muscle cells, eosinophils, macrophages, and the airway ECM, with variable expression associated with epithelial cells18. Matrix metalloproteinase (MMP) is the main rate-limiting enzyme that regulates the extracellular matrix19. In the state of asthma, too much MMP is generated, leading to an imbalance of MMP/TIMP, excessive degradation of extracellular matrix, and the imbalance of degradation/synthesis, causing structural damage to lung tissue and airway remodeling. MMP-9 and TIMP-1 are the most important factors involved in this process19. In our study, we found that there were increased levels of MMP-9, TIMP-1, and TGF-β1 and a tendency for a higher MMP-9/TIMP-1 ratio in patients with asthma, as well as clinical symptoms and hyper-responsiveness in the airway. After treatment with formoterol-budesonide for one year, the increased levels of cytokines significantly decreased, as did the degree of infiltration of inflammatory cells, clinical symptoms and hyper-responsiveness in the airway.
The pathology of asthma involves both large and small airways. The traditional lung function test preferentially identifies changes in large airways, and biopsy of the small airways is very difficult to achieve. Traditional chest X-ray and CT cannot distinguish between the minute structures of the lungs. High-resolution spiral CT-ray beams go through a narrow collimator using bone algorithm image reconstruction, which can show airways 1.5 to 2 mm in diameter and identify constitutions of 100 to 200 μm8. Thus, HRCT has a higher resolution than traditional chest X-ray and CT in the imaging of airway and lung substance and can show narrower parts of the airways. Because of its non-invasive and intuitive features, it has been used to evaluate airway remodeling in chronic inflammatory diseases in recent years9, 20. Kasahara et al21 measured the thickness of the epithelial reticular basement membrane (RBM) in the bronchial biopsy specimens of 49 patients with asthma and 18 healthy controls. HRCT evaluation of airway wall thickness was performed, which showed that the percentage of the airway wall area to the total airway area (WA%) and the percentage of the thickness of the airway wall to the diameter of the airway (WT%) in the asthma group were significantly higher than in the normal group; in addition, both WA% and WT% were well correlated with the thickness of the RBM while being negatively correlated with the FEV1 of asthmatic patients. Thickening of the RBM was accompanied by airway thickening, which could lead to irreversible airflow obstruction. HRCT showed that the airway wall thickening was well correlated with thickening of the RBM as shown by bronchial biopsy, and thickening of the airway wall had a good correlation with the deterioration of pulmonary function. Gupta et al22 found that HRCT scan abnormalities were present in 80% of subjects with severe asthma and often coexisted with bronchial wall thickening (62%), bronchiectasis (40%), and emphysema (8%). HRCT scans can reliably predict important bronchial wall changes. In this study, we carried out HRCT scans to evaluate airway remodeling at five levels so that the measurements of the small airways were more representative of degree of airway remodeling. The WT and WA% in the asthma group before treatment were significantly increased compared to data in the control group. After treatment, the WT and WA% of the patients with asthma decreased. The WT and WA% of patients with asthma were well correlated with hyper-responsiveness, degree of infiltration of inflammatory cells, and concentration of chemokines involved in the process of airway remodeling and were negatively correlated with FEV1/FVC and FEV1%. The WT and WA% of patients with asthma accurately reflected the degree of airway remodeling in patients with asthma. Reversible airway obstruction by factors such as secretions in the airway, mucus plug, bronchospasm, and edema of the airway wall could lead to the overestimation of airway wall thickness23. Before examination of high-resolution spiral CT, reversible obstructive factors should be reduced to a minimum. Measurement with a HRCT scan is also affected by many factors such as the subjective judgment of radiologists, window width, and window level24. This variability indicates that the accuracy and repeatability of direct measurement of changes in the small airway lumen should be improved. In our study, these changes were more accurate in the proximal airways than in the distal airways. A number of technical factors, including the methods of reconstruction, vision and image scanning current, and voltage, also need to be further studied.
ICS in combination with LABA inhalers are recommended for the treatment of persistent asthma. Budesonide can inhibit airway eosinophilic inflammation and reduce the number of mast cells and release of inflammatory mediators. Formoterol can stabilize the mast cell membrane, relax bronchial smooth muscle, inhibit capillary leakage, and activate sensory nerve endings. Budesonide and formoterol can complement and promote each other in the treatment of asthma24. Usmani et al25 found that formoterol might promote glucocorticosteroid receptors transferred to the nucleus and thus play a role in anti-inflammatory activity. Budesonide can upregulate the expression of β2 receptors and suppress the expression of GATA-3, which plays a role in the interaction between antigen-presenting cells and effect cells in the process of asthma26. Some earlier studies have also suggested that airway structural changes are associated with airflow limitation or airway hyper-responsiveness27, 28, 29. Taken together, these findings suggest that the airway structural changes can impair respiratory function and aggravate asthmatic symptoms even in patients with mild asthma. Although inhalation of steroids can inhibit airway inflammation in asthma, it is still unclear whether it can reverse airway structural changes30. Our research found that inhalation of budesonide-ormoterol for one year could effectively alleviate asthma symptoms, improve lung function, reduce airway hyper-responsiveness, inhibit inflammatory cell infiltration, and reverse airway remodeling in patients with asthma. These results suggest that treatment with budesonide-formoterol might be started from the early stage of even mild bronchial asthma.
In conclusion, formoterol-budesonide might interfere in chronic inflammation and remodeling in the airways as well as relieve asthmatic symptoms. HRCT and induced sputum can be applied to the evaluation of airway remodeling in asthma, which needs to be further studied.
Author contribution
Ke WANG and Chun-tao LIU designed research and wrote the manuscript; Yong-hong WU performed research; Hong-li BAI and En-sen MA analyzed data; Yu-lin FENG and Fu-qiang WEN revised the manuscript.
References
Busse WW, Lemanske RF Jr . Asthma. N Engl J Med 2001; 344: 350–62.
Bergeron C, Boulet LP . Structural changes in airway diseases: characteristics, mechanisms, consequences, and pharmacologic modulation. Chest 2006; 129: 1068–87.
Araujo BB, Dolhnikoff M, Silva LF, Elliot J, Lindeman JH, Ferreira DS, et al. Extracellular matrix components and regulators in the airway smooth muscle in asthma. Eur Respir J 2008; 32: 61–9.
Makinde T, Murphy RF, Agrawal DK . The regulatory role of TGF-beta in airway remodeling in asthma. Immunol Cell Biol 2007; 85: 348–56.
Vignola AM, Riccobono L, Mirabella A, Profita M, Chanez P, Bellia V, et al. Sputum metalloproteinase-9/tissue inhibitor of metalloproteinase-1 ratio correlates with airflow obstruction in asthma and chronic bronchitis. Am J Respir Crit Care Med 1998; 158: 1945–50.
Simpson JL, Scott RJ, Boyle MJ, Gibson PG . Differential proteolytic enzyme activity in eosinophilic and neutronphilic asthma. Am J Respir Crit Care Med 2005; 172: 559–65.
Castagnaro A, Rastelli A, Chetta A, Marangio E, Tzani P, De Filippo M, et al. High-resolution computed tomograghy evaluation of airway distensibility in asthmatic and healthy subjects. Radio Med 2008; 113: 43–55.
Chooi WK, Matthews S, Bull MJ, Morcos SK . Multislice helical CT: the value of multiplannar image reconstruction in assessment of the bronchi and small airways disease. Br J Radiol 2003; 76: 536–40.
Matsuoka S, Kurihara Y, Nakajima Y, Niimi H, Ashida H, Kaneoya K . Serial change in airway lumen and wall thickness at thin-section CT in asymptomatic subjects. Radiology 2005; 234: 595–603.
Marchac V, Emond S, Mamou-Mani T, Mamou-Mani T, Le Bihan-Benjamin C, Le Bourgeois M, et al. Thoracic CT in pediatric patients with difficult-to-treat asthma. AJR Am J Roentgenol 2002; 179: 1245–52.
Stock P, Akbari O, Dekruyff RH, Umetsu DT . Respiratory tolerance is inhibited by the administration of corticosteroids. J Immunol 2005; 175: 7380–7.
Wang K, Liu CT, Wu YH, Feng YL, Bai HL . Budesonide/formoterol decreases expression of vascular endothelial growth factor (VEGF) and VEGF receptor 1 within airway remodelling in asthma. Adv Ther 2008; 25: 342–54.
Duong M, Subbarao P, Adelroth E, Obminski G, Strinich T, Inman M, et al. Sputum eosinophils and the response of exercise-induced bronchoconstriction to corticosteroid in asthma. Chest 2008; 133: 404–11.
Bartoli ML, Bacci E, Carnevali S, Cianchetti S, Dente FL, Di Franco A, et al. Clinical assessment of asthma severity partially corresponds to sputum eosinophilic airway inflammation. Respir Med 2004; 98: 184–93.
Malerba M, Ragnoli B, Radaeli A, Tantucci C . Usefulness of exhaled nitric oxide and sputum eosinophils in the long-term control of eosinophilic asthma. Chest 2008; 134: 733–9.
Reid DW, Wen Y, Johns DP, Williams TJ, Ward C, Walters EH . Bronchodilator reversibility, airway eosinophilia and anti-inflammatory effects of inhaled fluticasone in COPD are not related. Respirology 2008; 13: 199–809.
Batra V, Musani AI, Hastie AT, Khurana S, Carpenter KA, Zangrilli JG, et al. Bronchoalveolar lavage fluid concentrations of transforming growth factor (TGF)-beta1, TGF-beta2, interleukin (IL)-4 and IL-13 after segmental allergen challenge and their effects on alpha-smooth muscle actin and collagen III synthesis by primary human lung fibroblasts. Clin Exp Allergy 2004; 34: 437–44.
Bottoms SE, Howell JE, Reinhardt AK, Evans IC, McAnulty RJ . TGF-bera isoform specific regulation of airway inflammation and remodeling in a murine model of asthma. PloS One 2010; 5: e9674.
Araujo BB, Dolhnikoff M, Silva LF, Elliot J, Lindeman JH, Ferreira DS, et al. Extracellular matrix components and regulators in the airway smooth muscle in asthma. Eur Respir J 2008; 32: 61–9.
Matsuoka S, Kurihara Y, Yagihashi K, Niimi H, Nakajima Y . Peripheral solitary pulmonary nodule: CT findings in patients with pulmonary emphysema. Radiology 2005; 235: 266–73.
Kasahara K, Shiba K, Ozawa T, Okuda K, Adachi M . Correlation between the bronchial subepithelial layer and whole airway wall thickness in patients with asthma. Thorax 2002; 57: 242–6.
Gupta S, Siddiqui S, Haldar P, Raj JV, Entwisle JJ, Wardlaw A, et al. Qualitative analysisof high-resolution CT scans in severe asthma. Chest 2009; 136: 1521–8.
Franquet T, Stern EJ . Bronchiolar inflammatory diseases: high-resolution CT findings with histologic correlation. Eur Radiol 1999; 9: 1290–303.
Humbert M, Andersson TL, Buhl R . Budesonide/formoterol for maintenance and reliver therapy in the management of moderate to severe asthma. Allergy 2008; 63: 1567–80.
Usmani OS, Ito K, Maneechotesuwan K, Ito M, Johnson M, Barnes PJ, et al. Glucocorticoid receptor nuclear translocation in airway cells after inhaled combination therapy. Am J Respir Crit Care Med 2005; 172: 704–12.
Miller-Larsson A, Selroos O . Advances in asthma and COPD treatment combination therapy with inhaled corticosteroids and long-acting beta 2 agonists. Curr Pharm Des 2006; 12: 3261–79.
Bouler LP, Laviolette M, Turcotte H, Cartier A, Dugas M, Malo JL, et al. Bronchial subepithelial fibrosis correlates with airway responsiveness to methacholine. Chest 1997; 112: 45–52.
Beasley R, Roche WR, Roberts JA, Holgate ST . Cellular events in the bronchi in mild asthma and after bronchial provocation. Am Rev Respir Dis 1989; 139: 806–7.
Chetta A, Foresi A, Del Donno M, Bertorelli G, Prsci A, Olivieri D . Airways remodeling is a distinctive feature of asthma and is related to severity of disease. Chest 1997; 111: 852–7.
Leigh R, Pizzichini MM, Morris MM, Maltais F, Hargreave FE, Pizzichina E . Stable COPD: predicting benefit from high-dose inhaled corticosteroid treatment. Eur Respir J 2006; 27: 964–71.
Acknowledgements
This study was supported by a grant from Clinical Medicine Research Special Fund from Chinese Medical Association (No 08020750153).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, K., Liu, Ct., Wu, Yh. et al. Effects of formoterol-budesonide on airway remodeling in patients with moderate asthma. Acta Pharmacol Sin 32, 126–132 (2011). https://doi.org/10.1038/aps.2010.170
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2010.170
Keywords
This article is cited by
-
Prolonged Treatment with Inhaled Corticosteroids does not Normalize High Activity of Matrix Metalloproteinase-9 in Exhaled Breath Condensates of Children with Asthma
Archivum Immunologiae et Therapiae Experimentalis (2015)