Abstract
Purpose
Preoperative counselling for penetrating keratoplasty should include awareness of symptoms and signs of possible complications as early presentation can enhance long-term success. In our corneal transplantation service, all patients are routinely instructed to arrange a same day emergency visit through a dedicated telephone line if they experience any symptoms in eyes that have undergone keratoplasty. This study was designed to evaluate the reason for presentation, management outcome of each visit and the efficiency of the system in management of postkeratoplasty complications.
Methods
A review of 100 consecutive emergency visits by postpenetrating keratoplasty (PKP) patients in a tertiary eye care centre was included.
Results
Sixty-two patients with varied preoperative diagnoses presented during the review period. Sixteen visits were within the first month after surgery and 40 visits within the first year. Ten patients (16%) sought consultation more than twice during the study period with one patient presenting five times. Pain and grittiness were the main presenting symptoms (68%). Loose corneal suture (25%) necessitating removal was the most common diagnosis. Sixteen visits resulted in hospital admission for treatment. The graft survived in all patients and the visual acuity was preserved in 95% of our patients.
Conclusion
Most corneal surgeons educate their patients to seek prompt treatment for symptoms such as redness, sensitivity to light, loss of vision, pain, or any other symptoms in eyes that have undergone keratoplasty. Early intervention of sight threatening complications increases the chance of graft survival and best-obtained vision. This review shows a simple open access system facilitates early presentation and successful management of postgraft complications.
Similar content being viewed by others
Introduction
Corneal grafting is the most common and successful human tissue transplantation procedure.1, 2 The chance of graft survival and improvement of vision is in part attributed to improved surgical technique, better donor tissue management, early recognition and prompt intervention of postoperative sight threatening complications.3 Of the potential complications, graft rejection remains the leading cause of corneal transplantation failure but other problems that arise in the postoperative period can affect the graft survival and thus the visual outcome.4, 5, 6, 7
The outcome following successful corneal transplantation not only depends on the underlying diagnosis and surgical technique but also on careful postoperative management and patient compliance with treatment. Preoperative education of patients to recognise symptoms/signs of potential complications and seek treatment immediately can improve graft survival.5, 6 Centres performing corneal graft surgery should have the appropriate back-up facilities for assessment of patients who present with acute problems.5
We report the results of 100 consecutive emergency visits by postpenetrating keratoplasty (PKP) patients using an open-access telephone system.
Methods
In our corneal transplantation service, all patients are instructed to arrange a same day emergency visit via a dedicated telephone line, day or night, if they experience any complaints in eyes that have undergone keratoplasty. These patients are evaluated on the same day if possible and prompt treatment is commenced as necessary. Preoperative information was retrieved from the patient's medical record and a corneal graft database.
The specialist registrar on-call performed clinical assessment and the entire patient's management plan was often discussed with the corneal surgeon directly responsible for the patient's long-term care. Each consultation included a history of symptoms, best-corrected vision, slit lamp examination and management as indicated by the presenting condition. The data collected prospectively included time from surgery, reason for presentation, duration of symptoms, number of visits by a single patient, clinical management and outcome of each visit, and the overall efficiency of the system.
Statistical analysis was carried out using SPSS Version 14.0 and StatXact version 7.0. Dichotomised data were analysed via the χ2 test together with odds ratios and, where appropriate, confidence intervals. After verifying the normality of distributions, associations between variables were investigated via Pearson's correlation coefficient. A logistic regression model using backward selection was constructed to identify whether any of the variables were prognostic for serious complication necessitating in-patient treatment.
Results
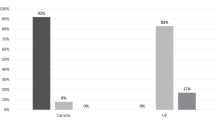
One hundred consecutive emergency visits by post-PKP patients presented between May 2001 and July 2002 were reviewed. There were 62 corneal graft patients from a cohort of 350 grafts patients, with a mean age of 62.8 years (range 18–92) and 68% males. The preoperative diagnosis was varied (Table 1), with keratoconus (37%) the most common indication for PKP. In all, 59% of the presentations were more than a year after their PKP and only 16% presented within a month of surgery (Figure 1). In all, 92% of the emergency visits were arranged after a telephone consultation and the remaining presented directly to the eye emergency service. All patients were seen on the same day.
There was considerable variation in the main presenting complaint (Figure 2). The duration of symptoms were <3 days in 67% of visits and it was less than a week in 91%. In 64 visits (64%) the presenting complaint was primarily pain (95% confidence interval from 54 to 73%). The most common reason to seek emergency consultation was gritty eyes due to a loose suture requiring removal (25%). In this group, one patient's best-corrected visual acuity worsened by two lines due to postsuture removal astigmatism (Figure 3). Sixteen of the emergency visits (14 patients) needed admission and intensive treatment (Table 2).
Three patients were admitted twice for the same problem (two patients for rejection, 6 months apart and one patient for significantly raised intraocular pressure (IOP) not responding to conventional treatment, a month apart). Visual blurring of <3 days duration was the presenting complaint in all patients who were diagnosed to have endothelial rejection. The mean interval between surgery and the rejection episode was 14 months (range 4–35). Following our standard protocol all patients with rejection episode were admitted and treated successfully with intensive topical steroids. Their vision remained stable or improved when compared to their pre-event record.
Painful loss of vision was the presenting complaint in all five patients with a diagnosis of graft infection, which was suture-related. All were successfully treated with intensive topical antibiotics. The final visual acuity worsened in two patients due to corneal scar-induced astigmatism (Figure 3).
Two patients seen with contact lens related epithelial problems were managed successfully. Herpes simplex recurrence was observed in six visits (four patients), which included new dendrites and disciform changes. The patient with macula-on retinal detachment presented with visual blurring and a nasal field defect of two days duration. He underwent vitreo-retinal surgery on the same day and his vision remained stable, with the retina still flat and corneal graft clear 2 years later.
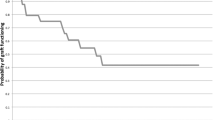
There were nine visits from nine patients, where the clinical examination was normal. Four of these patients were subsequently admitted for a serious complication including rejection and infection in the last 6 months of this study. This group was younger in age (mean 37.6 years). Forty patients (64%) presented only once. Eleven patients (18%) presented on more than three visits and only one patient presented five times (Figure 4).
The patient who sought emergency consultation five times was a 27-year-old male who had undergone PKP for a herpetic corneal scar. A diagnosis of herpetic recurrence was made three times and treated successfully. He was noted to have subconjunctival haemorrhage twice.
There was no association between the number of attendances and age (r=−0.15, P=0.23), presenting vision (r=−0.07, P=0.55), and duration of symptoms (r=−0.12, P=0.36). We investigated the probability of complications necessitating admission in relation to presenting visual acuity (Table 3) and presenting complaints.
There was a significant difference between the proportions of admissions for those patients with visual acuity ≤6/60. The odds ratio for visual acuity ≤6/60 vs ≥6/36 and probability of admission was 5.0 (95% confidence interval from 1.6 to 15.6, P=0.003). Similarly, patients presenting with visual loss were also more likely to be admitted to hospital (χ2=11.3, P=0.01).
A logistic regression model was constructed with a view to finding out whether certain variables were prognostic for a patient being admitted to hospital. The model resulted in two variables being retained, visual acuity ≤6/60 and a presenting complaint of visual loss. This supports the results of the previous bivariate models.
Discussion
The outcome following a successful corneal transplantation not only depends on the underlying diagnosis and surgical technique but also on careful postoperative management and patient compliance.5, 6
Despite improved donor tissue management, better understanding of tissue rejection and updated medical treatment, corneal graft rejection remains the major cause of graft failure.8, 9 Early recognition and prevention are still the best therapeutic options to date.5, 6 This is true not just for graft rejection but also for all other causes of complications that can result in graft failure.10, 11, 12, 13, 14, 15 Unless the patient is aware of the consequences, they may not seek medical attention until graft damage has progressed. ‘R.S.V.P’ is a good mnemonic by which patients can remember the signs and symptoms of graft rejection: R for redness, S for sensitivity of light, V for visual symptoms and P for pain.1
In our review of 100 visits, loose suture necessitating removal closely followed by epithelial defect and dry eyes were the most common presenting diagnoses. These clinical conditions should not be ignored as delay in management may result in sight threatening complications such as graft infection and/or rejection.
Sixteen visits resulted in admission for the management of sight threatening complications of which eight patients had signs of endothelial rejection. Early presentation, diagnosis, and management resulted in graft survival in all and preservation of visual acuity in 95% of our patients. This compares well with a previously published study by Morris and Kirkness in 1988 of emergency presentations of 205 consecutive corneal graft patients attending the accident and emergency department in a tertiary care eye hospital.5 Over 90% had demonstrable pathology and over 50% had conditions directly related to their corneal transplant. In 30%, there was an acute rejection episode and patients who presented early responded more rapidly to treatment. In their study, 57% of the rejection cases occurred within 2 years and 27% occurred at least 5 years after surgery. Alldredge, in his retrospective study found over 90% of rejection episodes occurred within 2 years of surgery.7 In our study, six patients (eight visits) managed for endothelial rejection presented within 3 years of their corneal transplant and in one patient the surgery was 15 years prior to the rejection episode. This illustrates the need for long-term follow-up in this group of patients.
Kamp et al6 found that in a group of high-risk patients, nearly 70% of graft rejection episodes were preceded by patient symptoms and only 30% of graft rejections were identified on routine clinical examination. However, the sensitivity and specificity of the patient's symptom as an indicator of graft rejection was poor. Despite this, patient symptoms cannot be ignored and the patient must be evaluated to exclude complications including rejection. In our series, all eight patients diagnosed with graft rejection during the study period presented with a short duration of symptoms (mean of 2.7 days).
In a corneal graft patient with previous history of herpes simplex keratitis the possibility of recurrence should always be considered.9, 16 However, recurrence of herpes simplex keratouveitis is the most difficult condition to differentiate from corneal graft rejection. It is important to bear in mind that Herpes Simplex Virus reactivation can precipitate graft rejection and therefore both conditions can be present simultaneously.
An open access system could theoretically be abused, however there were only nine visits in our series diagnosed to be clinically normal. This compares well with a previous study that reported absence of any abnormality in 10% of emergency visits.5
Post-PKP patients are normally very anxious and reassurance is a very important mode of treatment. It is also important not to discourage such patients from attending on future occasions.
The need for early recognition of graft rejection and other serious complications is very important for both the physician and the patient. It is also important to educate health staff regarding the importance of recognising corneal transplant patients' symptoms with view to early assessment and appropriate management.
Conclusion
Preoperative counseling for penetrating keratoplasty should include awareness of symptoms and signs of possible postoperative complications and the consequences of delayed medical treatment. Early recognition and intervention of any sight threatening complications increases the chance of graft survival and improvement of vision. A simple open access emergency system can help early presentation and successful management of postgraft complications.
References
Tham VM, Abbott RL . Corneal graft rejection: recent updates. Int Ophthalmol Clin 2002; 42 (1): 105–113.
Williams KA, Muehlberg SM, Wing SJ . The Australian corneal graft registry, 1990–1992 report. Aust NZ J Ophthalmol 1993; 21 (suppl): 1–48.
Rinne JR, Stulting RD . Current practises in the prevention and treatment of corneal rejection. Cornea 1992; 11: 326–328.
Ing JJ, Ing HH, Nelson LR, Hodge DO, Bourne WM . Ten-year post-operative results of penetrating keratoplasty. Ophthalmology 1998; 105: 1855–1865.
Morris RJ, Kirkness CM . Emergency presentation of corneal graft patients. Eye 1988; 2): 71–76.
Kamp MT, Fink NE, Enger C, Maguire MG, Stark WJ, Stulting RD . Patient-reported symptoms associated with graft reactions in high-risk patients in the collaborative corneal transplantation studies. Cornea 1995; 14: 43–48.
Allredge OC, Krachmer JH . Clinical types of corneal transplant rejection. Their manifestations, frequency, pre-operative correlates, and treatment. Arch Ophthalmol 1981; 99 (4): 599–604.
Arentsen JJ . Corneal transplant allograft rejection: possible predisposing factors. Trans Am Ophthalmol Soc 1983; 81: 361–402.
Larkin DFP . Corneal transplantation for herpes simplex keratitis. Br J Ophthalmol 1998; 82: 107–108.
The Collaborative Corneal Transplantation Studies Research Group. The collaborative corneal transplantation studies. Arch Ophthalmol 1992; 110: 1392–1403.
Boisjoly HM, Tourigny R, Bazin R, Laughrea PA, Dube I, Chamberland G et al. Risk factors of corneal graft failure. Ophthalmology 1993; 100: 1728–1735.
Yamagami S, Suzuki Y, Tsuru T . Risk factors for graft failure in penetrating keratoplasty. Acta Ophthalmol Scand 1996; 74: 584–588.
Volker-Dieben HJM, D'Amaro J, Kok-Alphen CC . Hierarchy of prognostic factors for corneal allograft survival. Aust NZJ Ophthalmol 1987; 15 (1): 11–18.
Maguire MG, Stark WJ, Gottsch JD, Stulting RD, Sugar A, Fink NE et al. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative corneal transplantation studies. Ophthalmology 1994; 10: 1536–1547.
Williams KA . Factors predictive of corneal graft survival. Ophthalmology 1992; 99: 403–414.
Foulks GN . Clinical aspects of corneal allograft rejection. In: Krachmer JH, Mannis MJ, Holland EJ (eds). Cornea: Surgery of the Cornea and Conjunctiva. Mosby: St. Louis, 19: pp 1687–1696.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part as a poster at the ARVO meeting, Fort Lauderdale, Florida, May 2003 and Bowman Club meeting, London March 2004
The authors have no proprietary or financial interest in any of the materials used in this study
Rights and permissions
About this article
Cite this article
Gnanaraj, L., Sandhu, S., Hildreth, A. et al. Postkeratoplasty emergency visits—a review of 100 consecutive visits. Eye 21, 1028–1032 (2007). https://doi.org/10.1038/sj.eye.6702546
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702546
Keywords
This article is cited by
-
Outcomes of N-butyl-2-Cyanoacrylate Tissue Adhesive Application in Corneal Perforation Disorders: Consecutive Case Series
Ophthalmology and Therapy (2023)
-
Ocular emergencies visits after corneal transplantation at a tertiary eye care hospital in Saudi Arabia
International Ophthalmology (2022)