Abstract
Purpose
To evaluate the effect of verteporfin therapy (Visudyne) on age-related macular degeneration (AMD) in Chinese patients. The baseline characteristic and the visual outcome will be compared with the treatment of AMD with photodynamic therapy study (TAP) and verteporfin in photodynamic therapy study (VIP).
Design
Retrospective comparative case series.
Method
We recruited patients >50 years old, with best-corrected visual acuity >20/200 and fluorescein angiography documenting subfoveal either predominantly classic with greatest linear dimension <5400 μm or pure occult choroidal neovascularization (CNV) secondary to AMD. We applied non-thermal laser to the lesion 15 min after visudyne infusion as described in TAP study. Patients were followed up with fluorescein angiography every 3 months. Additional treatment would be offered if there was evidence of recurrence of CNV.
Outcome measure
Baseline characteristic and visual outcome.
Result
In all, 46 eyes of 42 patients were enrolled at our centre from July 2002 to June 2003. They comprised 11 eyes with predominantly classic lesions and 35 eyes with pure occult lesion. The mean number of treatment sessions given was 2.9 in the first year. At the 12-month examination, there were 63 and 29% of patients showing visual improvement in predominantly classic and occult groups, respectively, while there were only 16% of patients in the TAP study and 12% of patients in the VIP study showing visual improvement in the same period.
Conclusion
Verteporfin therapy for subfoveal CNV is beneficial to Chinese patients with AMD at first year. The visual result seems to be better than that observed in Caucasian patients.
Similar content being viewed by others
Background
Age-related macular degeneration (AMD) is the leading cause of irreversible central vision loss in Caucasians 50 years and older in the United States. The prevalence increases with age1 and AMD can either be dry or wet (neovascular). In neovascular AMD, there is ingrowth of new blood vessels choroidal neovascularization (CNV) from the choriocapillaris through Bruchs membrane and retinal pigmented epithelium into the subretinal spaces.2 Central vision loss usually occurs because of fibrous tissue that accompanies the ingrowth of new vessels in addition to the disruption of the retinal pigment epithelium—photoreceptor complex owing to leakage of serum and blood.3, 4
The results of photodynamic therapy study (TAP) and verteporfin in photodynamic therapy (VIP) studies showed that there was beneficial effect in terms of stabilization of vision treated with verteporfin therapy. In subgroup analysis of patients with predominantly classic and pure occult subfoveal CNV, there could be improvement of vision.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 However, these studies were carried out in North America and Europe where the main target population was Caucasian.16 Therefore, the effect of photodynamic therapy (PDT) by verteporin in Asian Chinese eyes is still unknown.17, 18 We reported our experience of treating patients with subfoveal CNV due to AMD in the Chinese population and compared the first year result with those of TAP/VIP studies.
Design
Retrospective case series from a single centre.
Methods
We reviewed all clinical records of patients who had PDT performed in our centre in Tuen Mun Hospital, Hong Kong, with clinical evidence of subfoveal CNV secondary to AMD, from July 2002 to June 2003. The study population consisted of patients older than 50 years of either gender and with visual acuity >20/200. All patients were examined by a single ophthalmologist (CM Fan) and assessed for suitability of performing PDT. Fluorescein angiogram was performed and interpreted by the same ophthalmologist based on the definition used in previous trial.6, 10, 19 Patients had to have fluorescein angiographic evidence of CNV due to AMD extending within the geographic centre of the foveal avascular zone in order to participate in our study. Lesions were divided into predominantly classic, minimally classic and pure occult according to their angiographic findings. We only recruited predominantly classic and pure occult lessions into our study. The predominantly classic lesion was defined as any subfoveal lesion in which the area of the classic component on FA occupied at least 50% of the area of the entire lesion at baseline, while the pure occult lesion was defined as any subfoveal lesion with pure occult component and no classic component on FA. Moreover, the greatest linear dimension of the entire lesion could not, exceed 5400 μm on the retina.
Patients were excluded from the study if any of the following conditions were noted: features other than AMD; a tear (rip) of retinal pigment epithelium; any significant ocular disease compromising their vision; inability to obtain any photograph for documentation; history of laser treatment for AMD before; previous verteporfin therapy for AMD; history of intraocular surgery or Nd : YAG capsulotomy in the last few months; active liver disease, history of porphyria or related hypersensitivity reaction.
Further courses of PDT for eligible patients were recommended as often as every 3 months until month 12 provided that fluorescein angiographic evidence of recurrent CNV was observed.
Descriptive analysis of patient's demographic, baseline characteristic, and visual outcome were recorded and compared with TAP/VIP reports at first year.
Results
In all, 46 eyes of 42 patients were recruited into our study, which included, 38 patients with either eye involved and four patients with both eyes involved. Of the patients, 30 were male while 12 were female. The mean age was 72 years (ranged from 50 to 80 years). On fluorescein angiogram, 11 eyes were classified as predominantly classic type of CNV and 35 eyes were classified as pure occult type of CNV. The size of the lesion ranged from 1.03 to 5.4 mm. The mean lesion size for predominantly classic and pure occult CNV was 2.9 and 3.9 mm, respectively. The mean number of PDT performed for each patient was 2.9 (ranged from 1 to 4) at the first year.
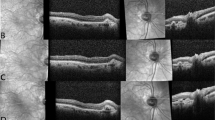
The changes in visual acuity throughout the study are summarized in Figures 1 and 2 as well as in Tables 1 and 2. Of the 11 patients with predominantly classic CNV, seven patients (64%) showed visual improvement of which five improved from one to three lines and two improved from three to six lines. On the contrary, four patients (36%) showed loss in vision that included one loss from one to three lines and three loss from three to six lines. As for the 35 patients with pure occult CNV, 10 patients (29%) showed visual improvement that included eight improved from one to three lines and two improved from three to six lines. Of the 14 patients (40%) had the same vision as before, while 11 patients (31%) lost their vision that included eight deteriorating from one to three lines and three deteriorating from three to six lines.
Discussion
The baseline demographic characteristics of our patients including mean age and lesion size are similar to that of TAP/VIP studies. The average treatment session is also comparable to the recommendation from TAP/VIP studies19 (2.9 vs 3.4/1st year).
Of the 11 predominantly classic CNV in our study, three (27%) suffered a loss more than three lines and seven (64%) had visual improvement after treatment at 12 months. The TAP 1 randomized clinical trials in 1999 revealed that at 12 months in the verteporfin-treated group, 246 of 402 eyes (61%) had a loss of less than three lines.3 In further subgroup analysis, when looking at patients with predominantly classic CNV, there was a statistically significant benefit in the prevention of visual acuity loss in the verteporfin-treated group as compared with the placebo group (67 vs 39%). When we compared our result with that of TAP report 1 for predominantly classic lesion, a smaller number of our patients had visual deterioration in terms of visual acuity loss of more than three lines than that of TAP report 1 subgroup analysis (27 vs 33%). As for the pure occult CNV group, three (9%) out of 35 patients had visual acuity loss of more than three lines while 10 (29%) had visual improvement after the treatment at 12 months. The VIP report 2 showed that the primary outcome of pure occult CNV of the verteporfin and placebo groups had similar results at the 12 month examination (51 vs 54% losts of at least three lines), although secondary outcome measures, such as angiographic outcomes, significantly favoured the verteporfin-treated group.9 When we compared our results with that of VIP report 2, a smaller number of our patients had visual deterioration in terms of visual acuity loss of more than three lines than that of VIP report 2 (9 vs 51%).
Although evidence suggests that the Chinese population with neovascular AMD have a natural history similar to that of the Caucasian population with neovascular AMD,17 our study showed that the visual outcome in Chinese AMD patients was better than in Caucasian patients after PDT at 1 year, even though our study and TAP/VIP investigations may not be directly comparable.
There are a number of limitations in our study. Firstly, our study is retrospective while TAP/VIP studies are prospective in nature. Secondly, our sample size is small when compared with either TAP or VIP study. Thirdly, there is no control group in this study.
Conclusion
The 1-year result of PDT for AMD patients with predominantly classic and pure occult CNV in Chinese eyes seems to be better than that of TAP and VIP studies. Further observation and follow-up will be necessary for documentation.
References
Schmidt-Erfurth U, Miller JW, Sickenberg M, Laqua H, Barbazetto I, Gragoudas ES et al. Photodynamic therapy with verteporfin for CNV caused by aged-related macular degeneration. Results of retreatments in a phase 1 and 2 study. Arch Ophthalmol 1999; 117: 1177–1187.
Miller JW, Schmidt-Erfurth U, Sickenberg M, Pournaras CJ, Laqua H, Barbazetto I et al. Photodynamic therapy with verteporfin for CNV caused by aged- related macular degeneration. Results of a single treatment in a phase 1 and 2 study. Arch Ophthalmol 1999; 117: 1161–1173.
Treatment of Age-Related Macular Degeneration With Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal CNV in age-related macular degeneration with verteporfin. One-year results of 2 randomized clinical trial—TAP report 1. Arch Ophthalmol 1999; 117: 1329–1345.
Treatment of Age-Related Macular Degeneration With Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal CNV in age-related macular degeneration with verteporfin. Two-year results of 2 randomized clinical trial—TAP report 2. Arch Ophthalmol 2001; 119: 198–207.
Macular Photocoagulation Study Group. Laser photocoagulation of subfoveal neovascular lesions of aged related macular degeneration. Updated findings from two clinical trials. Arch Ophthalmol 1993; 111: 1200–1209.
Macular Photocoagulation Study Group. Laser photocoagulation of subfoveal neovascular lesions of aged related macular degeneration. Arch Ophthalmol 1991; 109: 1220–1231.
Brown GC, Brown MM, Sharma S . Incremental cost-effectiveness of laser therapy for subfoveal choroidal neovascularization. Ophthalmology 2000; 107: 1374–1380.
Verteporfin in Photodynamic Therapy (VIP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in pathologic myopia with verteporfin. 1-year results of a randomized clinical trial—VIP report no. 1. Ophthalmology 2001; 108: 841–852.
Verteporfin in Photodynamic Therapy (VIP) Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization—Verteporfin in photodynamic therapy report 2. Am J Ophthalmol 2001; 131: 541–560.
Treatment of Age-Related Macular Degeneration With Photodynamic Therapy (TAP) Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: three-year results of an open-label extension of 2 randomized clinical trials—TAP Report No. 5. Arch Ophthalmol 2003; 120: 1307–1314.
Fine S . Photodynamic therapy with verteporfin is effective for selective patients with neovascular age-related macular degeneration. Arch Ophthalmol 1999; 177: 1400–1402.
Wu L, Murphy RP . Photodynamic therapy: a new approach to the treatment of choroidal neovascularization secondary to age-related macular degeneration. Curr Opin Ophthalmol 1999; 10: 217–220.
American Academy of Ophthalmology. Photodynamic therapy with verteporfin for age-related macular degeneration. Ophthalmology 2000; 107: 2314–2317.
Soubrane G, Bressler N . Treatment of subfoveal choroidal neovascularization in age-related macular degeneration: focus on clinical application of verteporfin photodynamic therapy. Br J Ophthalmol 2001; 85: 483–495.
Husain D, Kramer M, Kenny A . Effects of photodynamic therapy using verteporfin on experimental choroidal neovascularization and normal retina and choroids up to 7 weeks after treatment. Invest Ophthalmol Vis Sci 1999; 40: 2322–2331.
Sickenberg M, Schmidt-Erfurth U, Miller JW, Pournaras CJ, Zografos L et al. A preliminary study of photodynamic therapy using verteporfin for choroidal neovascularization in pathologic myopia, ocular histoplasmosis syndrome, angioid streak, and idiopathic causes. Arch Ophthalmol 2000; 117: 327–336.
Lim J, Kwok A, Wilson D . Symptomatic age-related macular degeneration in Asian patients. Retina 1998; 18: 435–438.
Pieramici D, Bressler N, Bressler S . Choroidal neovascularization in black patients. Arch Ophthalmol 1994; 112: 1043–1046.
Verteporfin Roundtable 2000 and 2001. Guidelines for using verteporfin (Visudyne) in photodynamic therapy to treat choroidal neovascularization due to age-related macular degeneration and other causes. Retina 2002; 22: 6–18.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, N., Fan, C. & Ho, C. Review of first year result of photodynamic therapy on age-related macular degeneration in chinese population. Eye 20, 523–526 (2006). https://doi.org/10.1038/sj.eye.6701991
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701991
This article is cited by
-
Genetic Predictors of Response to Photodynamic Therapy
Molecular Diagnosis & Therapy (2011)