Abstract
Glaucoma is the leading cause of irreversible blindness worldwide. East Asians account for approximately half of all glaucoma sufferers. It is likely that trabeculectomy will be needed for many of these people as the intraocular pressure is to be maintained at a satisfactorily low level. The eyes of East Asian people differ in some aspects from those of other races. This review describes the natural history of the eye after trabeculectomy in East Asians.
Similar content being viewed by others
Introduction
Glaucoma affects around 70 million people and is the second most common cause of blindness worldwide. Furthermore, it is the leading cause of irreversible blindness with estimates of blindness in around 10% of those affected. East Asians account for approximately half of all glaucoma sufferers.1 The World Health Organisation estimates that Asia is home to 3585 million people and that this is set to rise to 5268 million by 2050. In order to avoid blindness in over 3 million people, the management of glaucoma in East Asia has become a pressing issue.
The publication of large prospective surveys such as the Ocular Hypertension Treatment Study (OHTS),2 Collaborative Normal Tension Glaucoma Study (CNTGS),3 and the Early Manifest Glaucoma Treatment Study (EMGTS)4 have emphasized once more the important role that lowering intraocular pressure (IOP) plays in preventing the progression of glaucoma. Trabeculectomy remains the most effective weapon in the ophthalmologist's armoury with which we can achieve a satisfactory low IOP. Despite the introduction in recent years of new powerful medications, trabeculectomy has usually outperformed both medical and laser treatment in this regard.5, 6 This has led to a renewed interest in the natural history of the eye after trabeculectomy and how we can modify the operation to produce the most desirable result.
Cairns was the first to describe the partial thickness trabeculectomy that we know today, and the procedure remains much the same now as when he described it in 1967.7 Modifications introduced since then such as the introduction of antimetabolites have improved success rates.8, 9, 10, 11, 12, 13, 14, 15 This has been of particular benefit to those patients who were identified as having a higher risk for failure such as those who had had previous surgery, secondary glaucomas, young people, and non-Caucasian populations. It was established early on in its history that trabeculectomy in black subjects failed earlier compared to white subjects, presumably due to a more vigorous fibrotic response in the subconjunctival space.16, 17, 18, 19, 20, 21, 22 The reason black populations were studied in preference to the East Asian populations, for example, was probably because comparatively large communities of African-American blacks in the USA and Afro-Caribbean blacks in the UK provided a ready population to study in the countries where most of the academic literature was arising from.
Quigley's estimation that half of all the world's glaucoma sufferers are of East Asian origin has put this into perspective and, as a result, there has been a growing emphasis in the medical literature on this population. East Asian eyes have been shown to differ in many ways from the eyes of other racial groups and the assumption that these eyes will respond to trabeculectomy in the same manner as others cannot be taken as granted. An understanding of the natural history of the eyes both in terms of the glaucomatous progression and the response to standard treatments has become of prime importance in order for the burden of world preventable blindness to be lessened. Much of the populace in this region have inadequate access to health care services and this raises problems with screening and identifying at risk or affected individuals, before the treatment stage even begins. ‘One stop’ eye camps whereby trabeculectomies are performed have been proposed in those areas where follow-up would prove very difficult or access to medication is not available.23 The dictum of ‘primum non nocere’, that is, first do no harm means that the natural history of trabeculectomy in this distinct population needs to be addressed as the impact in terms of number of people treated is likely to be huge.
For the purposes of this review, East Asian is taken as meaning those peoples from China, Japan, and South-east Asia, excluding the Indian subcontinent. East Asian peoples in this context share a common racial heritage (ie Mongoloid), although heterogeneity within this group itself undoubtedly exists. Generally, as migration, genetic, and linguistics studies have shown, Northern Chinese, Korean, and Japanese form one subgroup, Southern Chinese (including Chinese Singaporeans) form another, and Malays, Indonesians, Thais, and Philippinos form yet another subgroup.24
Trabeculectomy in Whites, Hispanics, Blacks, and Indians
The natural history of trabeculectomy in white Caucasians has been studied in great detail. A national survey of the current practice of UK Ophthalmologists provided data for the first time on how individual surgeons in the UK differ in their surgical technique and subsequent management.25, 26, 27 Despite a wide variation in surgical technique, the success rate in this group of mainly unaugmented trabeculectomies was an impressive 84% at 1 year. The complication rate, however, was between 42 and 47% and more emphasis is now being placed on how best to modify Cairn's technique further to reduce this rate to acceptable levels, resulting a ‘tailor-made’ approach to patients, particularly with regard to augmentation with antimetabolite.
There have been a number of long-term studies. In a study of 150 eyes which had undergone unaugmented trabeculectomy with 9-year follow-up (predominantly white patients), 90% were controlled (IOP<20 mmHg no medication) at the last visit.28 Chen et al29 retrospectively reported a series of patients with various glaucoma diagnoses from a mixed white and black population, who underwent unaugmented primary trabeculectomies. In all, 40 patients were identified who had successful IOP control at 1 year (IOP<21 mmHg or 33% reduction). After 10 years follow-up, 27 subjects (67%) were able to maintain successful IOP control, although many of these required topical medications. Separate analysis by race was not performed. Suzuki et al30 performed a similar study of 87 eyes looking at trabeculectomies augmented with postoperative 5-fluorouracil (5-FU) injections and which were successful (IOP<21 mmHg or 33% reduction) at 1 year, but by year 10 the success rate had dropped to 44%. This poor rate could be attributed to the fact that the patients were deemed at ‘high risk’ for failure. Comparisons between studies are notoriously difficult due to differences in surgical technique, postoperative management, and patient demographics.
There are few prospective data from large studies. However, one such landmark study from the Fluorouracil Filtering Surgery Study Group (FFSSG) found that there was no significant difference in time to failure (IOP criteria) between blacks and whites. This was evident in both the treatment group (postoperative subconjunctival 5-FU injections) and the control group. There was, however, a significant difference between time to failure between Hispanics and whites, with Hispanics failing much earlier. Interestingly, the time to failure for Hispanics was much the same whether they received 5-FU or not, in marked contrast to the non-Hispanics, suggesting that the benefits of 5-FU to the white population may not be reflected in the Hispanic population.9
The FFSSG based its criteria for failure on IOP levels. The Advanced Glaucoma Intervention Study (AGIS) investigators found that although initial (mainly unaugmented) trabeculectomy lowered IOP significantly in blacks, if outcome criteria based on visual acuity and visual fields were utilised, initial treatment with argon laser trabeculoplasty (ALT) was preferable in blacks as opposed to whites.31 Longer term follow-up is required since these trends appear to be decreasing, but these differences have led some to suggest that primary open-angle glaucoma (POAG) in blacks may be a different disease than that in whites,32, 33 with more non-pressure-related factors being involved. The fact that glaucoma is more prevalent and occurs at a younger age in blacks lends some credence to this theory.34, 35, 36, 37 The AGIS investigators conclusions were that ‘planning and analysis of further studies of glaucoma treatment should take race into account’.38 The assumption that blacks from the Caribbean, Europe, America, and Africa all have the same disease process and reaction to surgery because of a shared ancestry is likely to be incorrect. Heterogeneity in these populations is marked and, even within Africa, different glaucoma epidemiological data are evident.21 It should be noted that almost all studies of trabeculectomy in black Africans have used IOP as an outcome measure of success—the AGIS results have highlighted the need for a broader definition of outcome.
The mounting evidence that blacks produce more conjunctival scarring after trabeculectomy leading to tbfnote620, 22, 39 led some to promote the use of antimetabolites in this group. Indeed many studies did show benefits of this in terms of lowered IOP,17, 40, 41, 42 although there was some evidence to the contrary.43 However, the consensus of opinion is that use of antimetabolites in blacks has now become the norm, particularly as complications such as hypotony seem to be lower in blacks than in whites.44, 45 Intraoperative antimetabolites are now used by the majority of practitioners in the American and Japanese glaucoma societies.46 Their use has improved the success rate, with 92.6 and 98.1% achieving IOP<22 mmHg for 5-FU and mitomycin-C (MMC), respectively, at 1 year in a recent randomised control trial of a racially mixed group.47 Results with long-term follow-up (>10 years) are yet to be published, as the routine use of intraoperative antimetabolites only became popular in the early 1990s.48
The Indian subcontinent consists of a heterogeneous group of people with the north consisting of predominantly Caucasian race and the south Dravidian. However, intermarrying and migration has meant that divisions along these lines have become impossible for a large portion of the population.
In a study from New Delhi, 33 patients were randomly assigned to undergo unaugmented trabeculectomy, trabeculectomy with intraoperative 5-FU or trabeculectomy with post-operative 5-FU injections.49 The success rates (IOP<22 mmHg, no medications) at 3 months were 67%, 90%, and 80%, respectively. There was a significant difference in the IOP between the groups receiving 5-FU and the control, although the former groups also had higher complication rates. Another study from Southern India examined trabeculectomy in 76 patients augmented with 0.4 mg/ml of MMC and found 93.4% success rate (IOP<21 mmHg, no medication) at 18 weeks.50 The main complications were choroidal detachment in 14% and cataract formation in 13%. These data seem to suggest that MMC-augmented trabeculectomy is the preferred option in this group of patients although larger comparative studies with longer follow-up are required.
Trabeculectomies in an East Asian population
The idea that fibrosis of the conjunctival space occurs more in darker skinned people may suggest that people of East Asian origin would be expected to have a fibrotic response similar to whites or perhaps in between whites and Indians.
However, a study from Singapore in 1996 reported that in a series of 51 eyes of mainly ethnic Chinese (76.5%) who underwent unaugmented trabeculectomy, success rate (IOP<21 mmHg) was achieved in only 48.7% of primary glaucomas at 2 years.51 This was a poorer success rate than any of the studies performed on black patients. Poor success rates were also reported in Malaysia where a study performed on 61 eyes of adult patients, mainly Chinese and Malay ethnicity, examined the results of unaugmented trabeculectomy at 2-year follow-up.52 They found 62% success (IOP<21 mmHg, no medications) for POAG and around 45% for primary angle closure glaucoma (PACG). Serious complications were low with only one eye having choroidal detachment.
Augmentation with intraoperative 5-FU has produced conflicting results in a similar population. In 1998, two studies were published from Singapore comparing unaugmented trabeculectomy to trabeculectomy augmented with intraoperative 5-FU. In the first, a retrospective review of 89 patients with a follow-up of around 36 months, it was found that IOP<22 mmHg without medication was achieved in 36.4% in the control group and 65.8% in the 5-FU group, which was significant.53 Conversely, Wong and Seah54 found in a series of 135 eyes, 27 of which had 5-FU-augmented trabeculectomies and 108 controls, that success (IOP<22 mmHg, no medications) at 1 year was 75.9% in the control group and 63% in the 5-FU group. This unusual result may be explained by the 5-FU group having a higher proportion of high-risk cases compared to the control group. Both studies had a similar racial distribution (mainly ethnic Chinese) and both had patients with POAG and PACG.
The relatively poor results even with 5-FU prompted some to see if MMC gave better results. A study from China in 1992 randomly assigned 40 eyes of 30 patients to receive unaugmented trabeculectomy or trabeculectomy augmented with 0.4 mg/ml MMC.55 Most of the eyes were at high risk of failure including uveitics, neovascular glaucomas, etc. The MMC group had a 67% drop in IOP at 1 year compared to 33% drop in the control group. Complications were minimal, with macular oedema being the most common (14% in the MMC group). A larger series from Hong Kong56 looked at 48 eyes, which underwent trabeculectomy augmented with 0.4 mg/ml MMC and had a follow-up of 21.8 months, found that 47.9% had IOP<22 mmHg (no medications). In all, 4% developed hypotony maculopathy and 2% required resuturing of a leaking conjunctival wound.
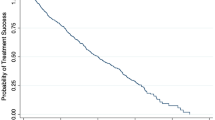
The data from Japan are more substantial. In a retrospectively analysed series of 427 eyes which underwent unaugmented trabeculectomy (mixed diagnoses and follow-up of 3 months to 5 years), the success rate was only 25% (IOP<21 mmHg, no medications).57 Complication rates were not reported. Two studies comparing trabeculectomy with postoperative subconjunctival injections of 5-FU vs control showed a much higher success rate with 5-FU.58, 59 Trabeculectomy augmented with MMC also had good results in one series of 59 eyes with 90% having IOP<21 mmHg at 2 years. A prospective comparative study between trabeculectomy with intraoperative MMC vs subconjunctival injections of 5-FU found MMC to be superior with success rates (IOP<21 mmHg without medications) of 88% vs 47% and no significant differences in complications.60
On the whole, complications in Japanese eyes seem to be more common than those in white Caucasian eyes. One large study of 211 eyes showed an incidence rate of 10% of flat anterior chamber after unaugmented trabeculectomies.58 This compares to a rate of only 0.2% in the UK survey. Furthermore, the rate of choroidal detachments has been reported as 31% for unaugmented trabeculectomies59 and as high as 47% for trabeculectomies with postoperative 5-FU injections60—this compares to 14% in the UK survey. Table 1 summarises the data from East Asia.
Characteristics of East Asian Eyes
The above statistics reveal a general trend of poorer success rates of both augmented and unaugmented trabeculectomy for East Asians in comparison with other races, including blacks, and arguably higher complication rates. There are a number of characteristics of East Asian eyes that could potentially account for this.
People of East Asian descent have a higher rate of PACG than those of European descent,1 with approximately 50–75% of East Asian glaucoma patients suffering from PACG.61, 62, 63 In Mongolia, the prevalence of PACG is 1.4%,64 while in the Inuit of Greenland, which share a common ancestry with the Sino-Mongoloid races of North-east Asia, this rises to 5%.65 Indeed, the preponderance of PACG over POAG is evident over much of East Asia.64, 66, 67, 68 A number of biometric features associated with the development of PACG have been identified, including shallow anterior chamber,69, 70 anterior lens position,70, 71 thick lens,72, 73 smaller corneal diameter,74, 75 and short axial length.76, 77 One can imagine that trabeculectomy in eyes that have the biometric features described above are at greater risk of lenticulo-corneal touch, as the anterior chamber has been shown to shallow after trabeculectomy.78, 79, 80 Cataract formation after trabeculectomy would be one of the expected consequences, but comparative data between East Asians and others are not yet available in this regard. There is conflicting evidence that East Asian eyes not known to have PACG may also have shallower and/or more crowded anterior chambers than Caucasians, and therefore have the same risk factors for post-trabeculectomy complications.74, 81
The main cause for failure of trabeculectomy remains excessive fibrosis at the conjunctival–scleral interface.82, 83, 84, 85 The differences in conjunctival cell profile between blacks and whites have already been investigated.86, 87 It was shown that blacks have a greater number of fibroblasts and macrophages in their conjunctiva compared to whites, and it has been postulated that this may be why black patients fail more than whites. Such comparative studies have not been performed on East Asian eyes. The skin of East Asians has been found to differ in structural and functional ways compared to the skin of whites.88 A study analysing the response to skin trauma found that the Chinese produced more keloid scarring than the darker skinned Malays.89 Such differences in the skin response to trauma may indicate similar differences in the response to trauma at the conjunctival–scleral interface, since the healing mechanism in skin and conjunctiva is thought to be similar.90
Another issue frequently overlooked in studies examining trabeculectomy success rates is the use of preoperative medications. A study comparing the success rates of trabeculectomy between patients on beta-blockers and pilocarpine vs those on beta-blockers alone found that the former group had a significantly higher failure rate.91 The conjunctival cell profile of those patients receiving pilocarpine and who failed contained significantly more fibroblasts and macrophages than those who did not. The same investigators also found that stopping of the antiglaucoma medication and prescribing 1 month course of topical steroid reversed these conjunctival changes.92 The preponderance of PACG in the East Asian population as well as for economic reasons means that the use of pilocarpine is likely to be much more prevalent among those glaucoma sufferers who undergo trabeculectomy. In an ongoing trial in Singapore, 61% of glaucoma patients assessed for primary trabeculectomy had used pilocarpine for more than 6 months (unpublished data, Husain et al). An examination of the conjunctival cell profile in this population, with perhaps a comparison between those that are taking pilocarpine and those that are not, is warranted.
The incidence of hypotony in different racial populations is difficult to determine, although a trend towards a greater incidence in whites and East Asians populations is evident. Hypotony rates have been reported between 10 and 33% in these populations.44, 93, 94, 95, 96 Blacks and Indians appear to have less incidence of hypotony or hypotony-related complications. In a study of 5-FU- and MMC-augmented trabeculectomy in a West African population, Singh et al45 found no cases of hypotony maculopathy or choroidal detachment and only three cases of flat anterior chamber in 101 eyes. A report by Ramakrishnan et al97 reported an incidence of only 0.7% of hypotony maculopathy in 778 Indian eyes which had had trabeculectomy augmented with MMC. Hypotony occurs with antimetabolite use due to overfiltration at the bleb site or underproduction of aqueous by the effect of antimetabolites on the ciliary body, or both.98, 99 It has been suggested that a thin sclera predisposes an eye to postoperative hypotony.100, 101, 102 The high prevalence of myopia (and hence thinner sclera) in the Chinese population may be relevant in this respect.103 The thickness of the sclera at the point of exposure to antimetabolite and subsequent damage to the ciliary body also needs to be considered. The racial variation of scleral thickness has not been examined before, but is likely to have relevance in this scenario.
One would expect higher rates of malignant glaucoma in Asian eyes due to their biometric features described above. Surprisingly, this has rarely been reported, although it is unclear whether this is due to low incidence or deficiencies in reporting.
Glaucoma in East Asians, both POAG and PACG, has similarities and differences with the disease profile in other races. It is still very much a disease of old age, with the median age for POAG and PACG being over 70 years in the Chinese Singaporean population,104 although one population-based study of 10 414 subjects from China found POAG to be far more prevalent in those aged under 40 years (methodological issues may account for this unusual result).105 The association between high intraocular pressures and glaucoma has been observed in most studies on East Asian peoples, the notable exception being the high prevalence of normal pressure glaucoma (NTG) in the Japanese population. This has been consistently reported and merits further investigation into the possibility of a different pathogenesis of glaucoma in this distinct population. It may be of relevance that the mean IOP in East Asian populations tends to be lower than that in Europeans68, 106 and therefore a re-classification of what constitutes ‘high’ and ‘normal’ pressures may result in a lower prevalence of NTG. The speed of progression of glaucoma also has an important role in management of the disease. Blacks are thought to have a more rapid disease progression than whites;107 the corresponding longitudinal data on East Asians are lacking and much needed.
Reports from Singapore,103 Taiwan,108 Hong Kong,109 and Japan110 have suggested that the prevalence of myopia is higher in East Asians than in European-derived populations. This has led to much debate on the aetiology of myopia and the role of genetic and environmental factors. The association between myopia and POAG have been reported previously,111, 112 as have the challenges of filtration surgery on the highly myopic eye.101 More recently, interest has focused on the associations between myopia, ocular dimensions, and PACG. PACG occurs more often in eyes with shallow anterior chambers and short axial lengths.69, 76 Myopia, which tends to be more prevalent in societies with high educational standards,113 is associated with deeper anterior chambers and longer eyes.114 The economic boom evident in much of East Asia has been accompanied by higher standards of living and higher prevalence of myopia.103, 108, 115, 116 This is particularly evident in Singapore where increasing prosperity since the 1970s has led to a highly educated young population which has a higher rate of myopia than the older population.103 If this really is due to a cohort effect rather than reflecting an actual change in refractive status of the eye with age, this will have profound implications for glaucoma screening and management, due to a likely shift in the balance between POAG and PACG incidence as the population ages.
Summary
The race of a person has been shown to affect the outcome of trabeculectomy. East Asian eyes have characteristics which make it likely that the natural history of trabeculectomy in these patients would differ from that in whites and blacks in whom most of the data are available. Glaucoma is the world's leading cause of irremediable blindness and half the world's 67 million glaucoma sufferers are of East Asian origin.1 It is likely that trabeculectomy is needed in many of these cases if the IOP is to be lowered to the target levels recently found to have the best chance of preventing glaucomatous progression. It is therefore of utmost importance to study the natural history of the eyes after trabeculectomy and in particular examine the effects of antimetabolites, preoperative topical medication use, scleral thickness, and postoperative complications such as hypotony and cataract formation.
At present, a prospective, randomised, placebo-controlled trial of the use of intraoperative 5-FU in glaucoma-filtering surgery is underway in Singapore. The trial will end in 2004 when all patients will have reached at least 3 years follow-up and it is hoped that analysis of the results will provide, for the first time, much needed data on the natural history of trabeculectomy in East Asia, and in particular, the effect of intraoperative 5-FU. It is hoped that this will enable ophthalmologists to modify filtration procedures such that the ocular morbidity due to glaucoma is reduced.
References
Quigley HA . Number of people with glaucoma worldwide. Br J Ophthalmol 1996; 80: 389–393.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713.
Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Collaborative Normal-Tension Glaucoma Study Group (see comments) (published erratum appears in Am J Ophthalmol 1999;127(1):120). Am J Ophthalmol 1998; 126: 487–497.
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial (comment). Arch Ophthalmol 2002; 120: 1268–1279.
Lichter PR, Musch DC, Gillespie BW, Guire KE, Janz NK, Wren PA et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmol 2001; 108: 1943–1953.
Investigators AGIS . The Advanced Glaucoma Intervention Study (AGIS): 9. Comparison of glaucoma outcomes in black and white patients within treatment groups. Am J Ophthalmol 2001; 132: 311–320.
Cairns JE . Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol 1968; 5: 673–677.
Smith MF, Doyle JW, Nguyen QH, Sherwood MB . Results of intraoperative 5-fluorouracil or lower dose mitomycin-C administration on initial trabeculectomy surgery. J Glaucoma 1997; 6: 104–110.
Five-year follow-up of the Fluorouracil Filtering Surgery Study. The Fluorouracil Filtering Surgery Study Group. Am J Ophthalmol 1996; 121: 349–366.
Goldenfeld M, Krupin T, Ruderman JM, Wong PC, Rosenberg LF, Ritch R et al. 5-Fluorouracil in initial trabeculectomy. A prospective, randomized, multicenter study. Ophthalmol 1994; 101: 1024–1029.
Ruderman JM, Welch DB, Smith MF, Shoch DE . A prospective, randomized study of 5-fluorouracil and filtration surgery. Trans Am Ophthalmol Soc 1987; 85: 238–253.
Ophir A, Ticho U . A randomized study of trabeculectomy and subconjunctival administration of fluorouracil in primary glaucomas. Arch Ophthalmol 1992; 110: 1072–1075.
Anand N, Sahni K, Menage MJ . Modification of trabeculectomy with single-dose intraoperative 5- fluorouracil application. Acta Ophthalmol Scand 1998; 76: 83–89.
Bell RW, Habib NE, O'Brien C . Long-term results and complications after trabeculectomy with a single per-operative application of 5-fluorouracil. Eye 1997; 11(Part 5): 663–671.
Lanigan L, Sturmer J, Baez KA, Hitchings RA, Khaw PT . Single intraoperative applications of 5-fluorouracil during filtration surgery: early results. Br J Ophthalmol 1994; 78: 33–37.
Borisuth NS, Phillips B, Krupin T . The risk profile of glaucoma filtration surgery. (Review) (26 refs). Curr Opin Ophthalmol 1999; 10: 112–116.
Mermoud A, Salmon JF, Murray AD . Trabeculectomy with mitomycin C for refractory glaucoma in blacks. Am J Ophthalmol 1993; 116: 72–78.
Morris DA, Peracha MO, Shin DH, Kim C, Cha SC, Kim YY . Risk factors for early filtration failure requiring suture release after primary glaucoma triple procedure with adjunctive mitomycin. Arch Ophthalmol 1999; 117: 1149–1154.
Shin DH, Hughes BA, Song MS, Kim C, Yang KJ, Shah MI et al. Primary glaucoma triple procedure with or without adjunctive mitomycin. Prognostic factors for filtration failure (comment). Ophthalmol 1996; 103: 1925–1933.
Welsh NH . Trabeculectomy with fistula formation in the African. Br J Ophthalmol 1972; 56: 32–36.
Budenz DL, Singh K . Glaucoma care in West Africa. J Glaucoma 2001; 10: 348–353.
Freedman J, Shen E, Ahrens M . Trabeculectomy in a Black American glaucoma population. B J Ophthalmol 1976; 60: 573–574.
Chew PT, Aung T . Primary angle-closure glaucoma in Asia (Review) (16 refs). J Glaucoma 2001; 10(Suppl 8): S7–S8.
Diamond JM . Guns, Germs and Steel: The Fates of Human Societies. 1st ed. WW Norton and Company: New York, 1999.
Edmunds B, Thompson JR, Salmon JF, Wormald RP . The National Survey of Trabeculectomy. II. Variations in operative technique and outcome (comment). Eye 2001; 15: 4–8.
Edmunds B, Thompson JR, Salmon JF, Wormald RP . The National Survey of Trabeculectomy. I. Sample and methods (see comments). Eye 1999; 13: 524–530.
Edmunds B, Thompson JR, Salmon JF, Wormald RP . The National Survey of Trabeculectomy. III. Early and late complications. Eye 2002; 16: 297–303.
Watson PG, Jakeman C, Ozturk M, Barnett MF, Barnett F, Khaw KT . The complications of trabeculectomy (a 20-year follow-up). Eye 1990; 4: 425–438.
Chen TC, Wilensky JT, Viana MA . Long-term follow-up of initially successful trabeculectomy. Ophthalmol 1997; 104: 1120–1125.
Suzuki R, Dickens CJ, Iwach AG, Hoskins Jr HD, Hetherington Jr J, Juster RP et al. Long-term follow-up of initially successful trabeculectomy with 5-fluorouracil injections. Ophthalmol 2002; 109: 1921–1924.
The Advanced Glaucoma Intervention Study (AGIS): 4. Comparison of treatment outcomes within race. Seven-year results (comment). Ophthalmol 1998; 105: 1146–1164.
Varma R . Trabeculoplasty, trabeculectomy, and race: is there a difference in response to treatment between blacks and whites? (comment). Ophthalmol 1998; 105: 1135–1136.
Drance SM . Glaucoma: a look beyond intraocular pressure. Am J Ophthalmol 1997; 123: 817–819.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J et al. Relationship between intraocular pressure and primary open-angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch Ophthalmol 1991; 109: 1090–1095.
Leske MC, Connell AM, Schachat AP, Hyman L . The Barbados Eye Study. Prevalence of open angle glaucoma. Arch Ophthalmol 1994; 112: 821–829.
Mason RP, Kosoko O, Wilson MR, Martone JF, Cowan Jr CL, Gear JC et al. National survey of the prevalence and risk factors of glaucoma in St. Lucia, West Indies. Part I. Prevalence findings. Ophthalmol 1989; 96: 1363–1368.
Fraser S, Bunce C, Wormald R . Retrospective analysis of risk factors for late presentation of chronic glaucoma. Br J Ophthalmol 1999; 83: 24–28.
The Advanced Glaucoma Intervention Study (AGIS): 4. Comparison of treatment outcomes within race. Seven-year results (comment). Ophthalmol 1998; 105: 1146–1164.
Merritt JC . Filtering procedures in American blacks. Ophthalmic Sur 1980; 11: 91–94.
Quigley HA, Buhrmann RR, West SK, Isseme I, Scudder M, Oliva MS . Long term results of glaucoma surgery among participants in an east African population survey. Br J Ophthalmol 2000; 84: 860–864.
Yorston D, Khaw PT . A randomised trial of the effect of intraoperative 5-FU on the outcome of trabeculectomy in east Africa. Br J Ophthalmol 2001; 85: 1028–1030.
Egbert PR, Williams AS, Singh K, Dadzie P, Egbert TB . A prospective trial of intraoperative fluorouracil during trabeculectomy in a black population. Am J Ophthalmol 1993; 116: 612–616.
Lachkar Y, Leyland M, Bloom P, Migdal C . Trabeculectomy with intraoperative sponge 5-fluorouracil in Afro- Caribbeans. Br J Ophthalmol 1997; 81: 555–558.
Shields MB, Scroggs MW, Sloop CM, Simmons RB . Clinical and histopathologic observations concerning hypotony after trabeculectomy with adjunctive mitomycin C. Am J Ophthalmol 1993; 116: 673–683.
Singh K, Byrd S, Egbert PR, Budenz D . Risk of hypotony after primary trabeculectomy with antifibrotic agents in a black west African population. J Glaucoma 1998; 7: 82–85.
Chen PP, Yamamoto T, Sawada A, Parrish RK, Kitazawa Y . Use of antifibrosis agents and glaucoma drainage devices in the American and Japanese Glaucoma Societies. J Glaucoma 1997; 6: 192–196.
Singh K, Mehta K, Shaikh NM, Tsai JC, Moster MR, Budenz DL et al. Trabeculectomy with intraoperative mitomycin C versus 5-fluorouracil. Prospective randomized clinical trial. Ophthalmology 2000; 107: 2305–2309.
Khaw PT . Advances in glaucoma surgery: evolution of antimetabolite adjunctive therapy (review) (22 refs). J Glaucoma 2001; 10(Suppl 4): S81–S84.
Lamba PA, Pandey PK, Raina UK, Krishna V . Short-term results of initial trabeculectomy with intraoperative or postoperative 5-fluorouracil for primary glaucomas. Indian J Ophthalmol 1997; 45: 173–176.
Ramakrishnan R, Michon J, Robin AL, Krishnadas R . Safety and efficacy of mitomycin C trabeculectomy in southern India. A short-term pilot study. Ophthalmol 1993; 100: 1619–1623.
Tan C, Chew PT, Lum WL, Chee C . Trabeculectomy—success rates in a Singapore hospital. Singapore Med J 1996; 37: 505–507.
Sharif FM, Selvarajah S . The outcome of trabeculectomy for primary glaucoma in adult patients in UKM. Med J Malaysia 1997; 52: 17–25.
Wong JS, Yip L, Tan C, Chew P . Trabeculectomy survival with and without intra-operative 5-fluorouracil application in an Asian population. Aust N Z J Ophthalmol 1998; 26: 283–288.
Wong HT, Seah SK . Retrospective analysis of outcome of trabeculectomies for primary glaucoma. Asia-Pacific Ophthalmol 1998; 10: 12–15.
Wu L, Yin JF . The efficacy of mitomycin C for filtration surgery in refractory glaucoma. Chin J Ophthalmol 1996; 32: 32–34.
Ng PW, Yeung BY, Yick DW, Yu CB, Lam DS . Fornix-based trabeculectomy with Wise's suture technique in Chinese patients. Ophthalmol 2000; 107: 2310–2313.
Inaba Z . Long-term results of trabeculectomy in the Japanese: an analysis by life-table method. Jpn J Ophthalmol 1982; 26: 361–373.
Araie M, Shoji N, Shirato S, Nakano Y . Postoperative subconjunctival 5-fluorouracil injections and success probability of trabeculectomy in Japanese: results of 5-year follow-up. Jpn J Ophthalmol 1992; 36: 158–168.
Nakano Y, Araie M, Shirato S . Effect of postoperative subconjunctival 5-fluorouracil injections on the surgical outcome of trabeculectomy in the Japanese. Graefes Arch Clin Exp Ophthalmol 1989; 227: 569–574.
Kitazawa Y, Kawase K, Matsushita H, Minobe M . Trabeculectomy with mitomycin. A comparative study with fluorouracil. Arch Ophthalmol 1991; 109: 1693–1698.
Congdon NG, Quigley HA, Hung PT, Wang TH, Ho TC, Glovinsky Y . Impact of age, various forms of cataract, and visual acuity on whole-field scotopic sensitivity screening for glaucoma in rural Taiwan. Arch Ophthalmol 1995; 113: 1138–1143.
Congdon N, Quigley HA, Hung PT, Wang TH, Ho TC . Screening techniques for angle-closure glaucoma in rural Taiwan. Acta Ophthalmol 1996; 74: 113–119.
Foster PJ, Johnson GJ . Glaucoma in China: how big is the problem? Br J Ophthalmol 2001; 85: 1277–1282.
Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ . Glaucoma in Mongolia. A population-based survey in Hovsgol province, northern Mongolia. Arch Ophthalmol 1996; 114: 1235–1241.
Clemmesen V, Alsbirk PH . Primary angle-closure glaucoma (a.c.g.) in Greenland. Acta Ophthalmol 1971; 49: 47–58.
Congdon N, Wang F, Tielsch JM . Issues in the epidemiology and population-based screening of primary angle-closure glaucoma. Surv Ophthalmol 1992; 36: 411–423.
Nguyen N, Mora JS, Gaffney MM, Ma AS, Wong PS, Iwach AG et al. A high prevalence of occludable angles in a Vietnamese population. Ophthalmol 1996; 103: 1426–1431.
Shiose Y, Kitazawa Y, Tsukahara S, Akamatsu T, Mizokami K, Futa R et al. Epidemiology of glaucoma in Japan—a nationwide glaucoma survey. Jpn J Ophthalmol 1991; 35: 133–155.
Lowe RF . Causes of shallow anterior chamber in primary angle closure glaucoma. Ultrasonic biometry of normal and angle-closure eyes. Am J Ophthalmol 1969; 67: 87–93.
Marchini G, Pagliarusco A, Toscano A, Tosi R, Brunelli C, Bonomi L . Ultrasound biomicroscopic and conventional ultrasonographic study of ocular dimensions in primary angle-closure glaucoma. Ophthalmol 1998; 105: 2091–2098.
Lowe RF . Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol 1970; 54: 161–169.
Markowitz SN, Morin JD . Angle-closure glaucoma: relation between lens thickness, anterior chamber depth and age. Canad J Ophthalmol 1984; 19: 300–302.
Qi Y . Ultrasonic evaluation of the lens thickness to axial length factor in primary closure angle glaucoma. Yen Ko Hsueh Pao (Eye Sci) 1993; 9: 12–14.
Congdon NG, Qi Y, Quigley HA, Hung PT, Wang TH, Ho TC et al. Biometry and primary angle-closure glaucoma among Chinese, White and Black populations. Opthalmol 1997; 104: 1489–1495.
Tomlinson A, Leighton DA . Ocular dimensions in the heredity of angle-closure glaucoma. Br J Ophthalmol 1973; 57: 475–485.
Lowe RF . Primary angle-closure glaucoma: a review of ocular biometry. Austr J Ophthalmol 1977; 5: 9–17.
Alsbirk PH . Primary angle-closure glaucoma. Oculometry, epidemiology, and genetics in a high risk population. Acta Ophthalmol 1976; 54: 5–31.
Cunliffe IA, Dapling RB, West J, Longstaff S . A prospective study examining the changes in factors that affect visual acuity following trabeculectomy. Eye 1992; 6: 618–622.
Stewart WC, Shields MB . Management of anterior chamber depth after trabeculectomy. Am J Ophthalmol 1988; 106: 41–44.
Martinez-Bello C, Rodriguez-Ares T, Pazos B, Capeans C, Sanchez SM . Changes in anterior chamber depth and angle width after filtration surgery: a quantitative study using ultrasound biomicroscopy. J Glaucoma 2000; 9: 51–55.
Foster PJ, Alsbirk PH, Baasanhu J, Munkhbayar D, Uranchimeg D, Johnson GJ . Anterior chamber depth in Mongolians: variation with age, sex, and method of measurement. Am J Ophthalmol 1997; 124: 53–60.
Hitchings RA, Grierson I . Clinico pathological correlation in eyes with failed fistulizing surgery. Trans Ophthalmol Soc UK 1983; 103: 84–88.
Addicks EM, Quigley HA, Green WR, Robin AL . Histologic characteristics of filtering blebs in glaucomatous eyes. Arch Ophthalmol 1983; 101: 795–798.
Maumenee AE . External filtering operations for glaucoma. The mechanism of function and failure. Trans Am Ophthalmol Soc 1960; 58: 319–328.
Skuta GL, Parrish RK . Wound healing in glaucoma filtering surgery (review) (197 refs). Surv Ophthalmol 1987; 32: 149–170.
Broadway D, Grierson I, Hitchings R . Racial differences in the results of glaucoma filtration surgery: are racial differences in the conjunctival cell profile important? Br J Ophthalmol 1994; 78: 466–475.
Broadway DC, Chang LP . Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva (review) (166 refs). J Glaucoma 2001; 10: 237–249.
Berardesca E, Maibach H . Racial differences in skin pathophysiology (review) (50 refs). J Am Acad Dermatol 1996; 34: 667–672.
Taylor SC . Skin of color: biology, structure, function, and implications for dermatologic disease (review) (144 refs). J Am Acad Dermatol 2002; 46(Suppl 62): S41–S62.
Lama PJ, Fechtner RD . Antifibrotics and wound healing in glaucoma surgery (review) (129 refs). Surv Ophthalmol 2003; 48: 314–346.
Broadway DC, Grierson I, O'Brien C, Hitchings RA . Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery (see comments). Arch Ophthalmol 1994; 112: 1446–1454.
Broadway DC, Grierson I, Sturmer J, Hitchings RA . Reversal of topical antiglaucoma medication effects on the conjunctiva. Arch Ophthalmol 1996; 114: 262–267.
Kitazawa Y, Suemori-Matsushita H, Yamamoto T, Kawase K . Low-dose and high-dose mitomycin trabeculectomy as an initial surgery in primary open-angle glaucoma. Ophthalmol 1993; 100: 1624–1628.
Costa VP, Wilson RP, Moster MR, Schmidt CM, Gandham S . Hypotony maculopathy following the use of topical mitomycin C in glaucoma filtration surgery. Ophthalmic Surg 1993; 24: 389–394.
Suemori-Matsushita H, Okabe I, Yamamoto T, Hayakawa T, Kondo Y, Miyake K et al. Hypotonous maculopathy following trabeculectomy with mitomycin C (Japanese). Nippon Ganka Gakkai Zasshi—Acta Soc Ophthalmol Jpn 1995; 99: 312–317.
Zacharia PT, Deppermann SR, Schuman JS . Ocular hypotony after trabeculectomy with mitomycin C. Am J Ophthalmol 1993; 116: 314–326.
Ramakrishnan R, Robin AL, Krishnadas R, Vijayalakshmi P . Low incidence of hypotony maculopathy following mitomycin trabeculectomy in pigmented Indian eyes (abstract). Ophthalmol 1995; 102 (Suppl): 136.
Schraermeyer U, Diestelhorst M, Bieker A, Theisohn M, Mietz H, Ustundag C et al. Morphologic proof of the toxicity of mitomycin C on the ciliary body in relation to different application methods. Graefes Arch Clin Exp Ophthalmol 1999; 237: 593–600.
Mietz H . The toxicology of mitomycin C on the ciliary body (review) (50 refs). Curr Opin Ophthalmol 1996; 7: 72–79.
Gass JD . Contemporary Ophthalmology: Honoring Sir Stewart Duke Elder, 1st ed. Williams and Wilkins: Baltimore, 1972, pp 343–366.
Stamper RL, McMenemy MG, Lieberman MF . Hypotonous maculopathy after trabeculectomy with subconjunctival 5- fluorouracil. Am J Ophthalmol 1992; 114: 544–553.
Jampel HD, Pasquale LR, Dibernardo C . Hypotony maculopathy following trabeculectomy with mitomycin C. Arch Ophthalmol 1992; 110: 1049–1050.
Wong TY, Foster PJ, Hee J, Ng TP, Tielsch JM, Chew SJ et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci 2000; 41: 2486–2494.
Foster PJ, Oen FT, Machin D, Ng TP, Devereux JG, Johnson GJ et al. The prevalence of glaucoma in Chinese residents of Singapore: a cross-sectional population survey of the Tanjong Pagar district. Arch Ophthalmol 2000; 118: 1105–1111.
Hu Z, Zhao ZL, Dong FT . An epidemiological investigation of glaucoma in Beijing and Shun-yi county (Chinese). Chung-Hua Yen Ko Tsa Chih (Chin J Ophthalmol) 1989; 25: 115–118.
Foster PJ, Machin D, Wong TY, Ng TP, Kirwan JF, Johnson GJ et al. Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar Study. Invest Ophthalmol Vis Sci 2003; 44: 3885–3891.
Wilson MR, Kosoko O, Cowan Jr CL, Sample PA, Johnson CA, Haynatzki G et al. Progression of visual field loss in untreated glaucoma patients and glaucoma suspects in St. Lucia, West Indies. Am J Ophthalmol 2002; 134: 399–405.
Lin LL, Shih YF, Tsai CB, Chen CJ, Lee LA, Hung PT et al. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optometry Vision Sci 1999; 76: 275–281.
Van Newkirk MR . The Hong Kong vision study: a pilot assessment of visual impairment in adults. Trans Am Ophthalmol Soc 1997; 95: 715–749.
Hosaka A . Population studies—myopia experience in Japan. Acta Ophthalmol—Suppl 1988; 185: 37–40.
Mitchell P, Hourihan F, Sandbach J, Wang JJ . The relationship between glaucoma and myopia. The Blue Mountains Eye Study. Ophthalmol 1999; 106: 2010–2015.
Ramakrishnan R, Nirmalan PK, Krishnadas R, Thulasiraj RD, Tielsch JM, Katz J et al. Glaucoma in a rural population of southern India: the Aravind comprehensive eye survey. Ophthalmol 2003; 110: 1484–1490.
Rosner M, Belkin M . Intelligence, education, and myopia in males. Arch Ophthalmol 1987; 105: 1508–1511.
Wong TY, Foster PJ, Ng TP, Tielsch JM, Johnson GJ, Seah SK . Variations in ocular biometry in an adult Chinese population in Singapore: the Tanjong Pagar Survey. Invest Ophthalmol Vis Sci 2001; 42: 73–80.
Lin LL, Chen CJ, Hung PT, Ko LS . Nation-wide survey of myopia among schoolchildren in Taiwan, 1986. Acta Ophthalmol—Suppl 1988; 185: 29–33.
Wu HM, Seet B, Yap EP, Saw SM, Lim TH, Chia KS . Does education explain ethnic differences in myopia prevalence? A population-based study of young adult males in Singapore. Optometry Vision Sci 2001; 78: 234–239.
Ng PW, Yeung BY, Yick DW, Yu CB, Lam DS . Fornix-based trabeculectomy with Wise's suture technique in Chinese patients. Ophthalmol 2000; 107: 2310–2313.
Tan C, Chew PT, Lum WL, Chee C . Trabeculectomy—success rates in a Singapore hospital. Singapore Med 1996; 37: 505–507.
Wong DWK, Seah SK . Trabeculectomy with single intraoperative application of 5-fluorouracil: preliminary results. Asia-Pacific J Ophthalmol 1995; 7: 16–19.
Uchida S, Suzuki Y, Araie M, Shigeeda T, Hara T, Shirato S . Long-term follow-up of initial 5-fluorouracil trabeculectomy in primary open-angle glaucoma in Japanese patients. J Glaucoma 2001; 10: 458–465.
Oh SY, Youn DH, Kim DM, Hong C . The effects of intraoperative mitomycin-C or 5-fluorouracil on glaucoma filtering surgery. Kor J Ophthalmol 1994; 8: 6–13.
Acknowledgements
This study is supported in part by the Singapore National Eye Centre, Singapore Eye Research Institute, Singapore National Medical Research Council (grant NMRC/0044/1994), United Kingdom Medical Research Council (grant MRCG9330070), Moorfields Trustees, and the Michael and Ilse Katz Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Husain, R., Clarke, J., Seah, S. et al. A review of trabeculectomy in East Asian people—the influence of race. Eye 19, 243–252 (2005). https://doi.org/10.1038/sj.eye.6701477
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701477
Keywords
This article is cited by
-
The Japan Glaucoma Society guidelines for glaucoma 5th edition
Japanese Journal of Ophthalmology (2023)
-
Recent trends in glaucoma surgery: a nationwide database study in Japan, 2011–2019
Japanese Journal of Ophthalmology (2022)
-
Outcomes of surgical bleb revision at a tertiary Singapore eye hospital
International Ophthalmology (2022)
-
Evaluating CO2 laser-assisted sclerectomy surgery with mitomycin C combined with or without phacoemulsification in adult Asian glaucoma subjects
International Ophthalmology (2021)
-
Reoperation rates after Ex-PRESS versus trabeculectomy for primary open-angle or normal-tension glaucoma: a national database study in Japan
Eye (2020)