Abstract
Cetrorelix, a luteinising hormone-releasing hormone (LHRH) analogue, has been shown to limit growth of the human androgen-independent prostate cell line DU-145, although other inhibitory actions may also be affected. Both growth and invasion of DU-145 cells are linked to autocrine epidermal growth factor receptor (EGFR) signalling. Invasiveness requires not only cells to migrate to conduits, but also reduced adhesiveness between tumour cells to enable separation from the tumour mass. Thus, we investigated whether Cetrorelix alters the DU-145 cell–cell adhesion and if this occurs via altered EGFR signalling. Pharmacologic levels of Cetrorelix limited the invasiveness of a highly invasive DU-145 subline overexpressing full-length EGFR (DU-145 WT). Extended exposure of the cells to Cetrorelix resulted in increased levels of the cell–cell adhesion complex molecules E-cadherin, α- and β-catenin, and p120. Puromycin blocked the increases in E-cadherin and β-catenin levels, suggesting that de novo protein synthesis is required. The Cetrorelix effect appears to occur via transmodulation of EGFR by a protein kinase C (PKC)-dependent mechanism, as there were no changes in DU-145 cells expressing EGFR engineered to negate the PKC transattenuation site (DU-145 A654); downregulation of EGFR signalling produced a similar upregulation in adhesion complex proteins, further suggesting a role for autocrine signalling. Cetrorelix increased the cell–cell adhesiveness of DU-145 WT cells to an extent similar to that seen when autocrine EGFR signalling is blocked; as expected, DU-145 A654 cell–cell adhesion also was unaffected by Cetrorelix. The increased adhesiveness is expected as the adhesion complex molecules moved to the cells' periphery. These data offer direct insight into the possible crosstalk pathways between the LHRH and EGFR receptor signalling. The ability of Cetrorelix to downregulate EGFR signalling and subsequently reverse the antiadhesiveness found in metastatic prostate cancer highlights a novel potential target for therapeutic strategies.
Similar content being viewed by others
Main
Adhesion between normal epithelial cells is usually strong and stable, limiting cell movement. In carcinomas, these tight cell associations must first be disrupted or prevented from forming before tumour cells are able to disseminate and metastasise. Cell–cell association is often disorganised in tumours, and has been linked to tumour invasiveness and metastasis (Pignatelli and Vessey, 1994; Shino et al, 1995; Richmond et al, 1997). Acquisition of invasive potential by malignant cancer cells results from an accumulation of characteristics, including increased cell motility, secretion of proteolytic enzymes, and alterations of cell–substrate and cell–cell adhesion (Fidler, 2003; Grunert et al, 2003). The molecular mechanisms responsible for this latter process, altered cell–cell adhesion, in invasive cancer cells are poorly understood (Comoglio and Trusolino, 2002). However, the net result is a reduction in cadherin/catenin complexes at the cells' periphery (Morita et al, 1999; Davies et al, 2000). Thus, to better understand the mechanisms of tumour cell dissociation, the role of cadherins must be taken into account, as they are crucial in cell–cell adhesion (Takeichi, 1993; Kim et al, 1999; Suyama et al, 2002).
Cadherins comprise a family of transmembrane cell surface glycoproteins that mediate calcium (Ca2+)-dependent, homotypic cell–cell interactions through their extracellular domains, and regulate a variety of biological processes during development, morphogenesis, and tumour metastasis (Gumbiner, 1996; Yap et al, 1997; Conacci-Sorrell et al, 2002). Ca2+-dependent cell–cell adhesion usually consists of rapid localisation of surface E-cadherin molecules to the regions of contact, resulting in homotypic binding that fosters the maintenance of normal cellular structure. However, metastatic cancer cells are able to over-ride or avoid contact inhibition signals employed by normal epithelial cells to control proliferation and cell movement.
The linkage between E-cadherin and the cellular cytoskeleton is a complex interaction involving a number of structural and signalling cytoplasmic proteins such as α- and β-catenin and p120 (Van Aken et al, 2001; Mason et al, 2002). Early studies identified E-cadherin/catenin interactions as imperative for cell–cell adhesion (Chitaev and Troyanovsky, 1998). β-Catenin binds with high affinity to the carboxyl-terminal region of the cadherin cytoplasmic tail, while α-catenin serves as an anchor, by bridging to α-actinin, to link the complex to the actin cytoskeleton (Aberle et al, 1994; Hulsken et al, 1994; Funayama et al, 1995; Jou et al, 1995; Rimm et al, 1995). These molecules not only play structural roles but also alter cell responses and phenotypes. β-Catenin is also found to immunoprecipitate with the APC tumour suppressor protein (Su et al, 1993; Hulsken et al, 1994; Shibata et al, 1994), and has been recently identified as an oncogene (Kim et al, 2002; Minamoto et al, 2002; Kielhorn et al, 2003; Schneider et al, 2003). It is also central to cell signalling, as upon dissociation from E-cadherin, it transits to the nucleus to alter transcriptional profiles (Mason et al, 2002; van de Wetering et al, 2002). A reduction in β-catenin expression decreases the stability of the adhesion complex and likely results in impairment in E-cadherin function (Willert and Nusse, 1998; Lowy et al, 2002; Mason et al, 2002). Similarly, a reduction in E-cadherin often results in β-catenin degradation (Liu et al, 2002). Another protein associated with E-cadherin, p120 (Thoreson et al, 2000), is phosphorylated on both tyrosine and serine residues in response to a variety of growth factors such as epidermal growth factor (EGF), platelet-derived growth factor (PDGF), and colony stimulating factor (CSF)-1, suggesting involvement in active signalling (Downing and Reynolds, 1991; Shibamoto et al, 1995). Thus, cell–cell adhesion serves not only a structural role but dictates cellular behaviour.
As carcinomas progress to the invasive and metastatic stages, select adhesive epithelial cells usually undergo a mesenchymal-like transition that enables their movement from the primary tumour mass (Comoglio and Boccaccio, 2001; Conacci-Sorrell et al, 2002). During this process in breast, gastric, and pancreatic metastatic carcinomas, E-cadherin expression is frequently downregulated or even undetectable (Birchmeier and Behrens, 1994; Lowy et al, 2002). This pattern of E-cadherin expression also persists in disseminated prostate carcinomas when compared to nonmetastatic prostate cells (Umbas et al, 1992; Davies et al, 2000; Mason et al, 2002). In addition, the loss of E-cadherin expression has been shown as a consequence of autocrine activation of epidermal growth factor receptor (EGFR) signalling (Jawhari et al, 1999). This combination of autocrine EGFR signalling and loss of E-cadherin expression leads to cell proliferation, dedifferentiation, and induction of cell motility (Hazan and Norton, 1998). Such an association has been suggested in the progression of breast carcinoma cells to a more invasive phenotype, which correlates with downregulation of E-cadherin and overexpression of EGFR (Sorscher et al, 1995a, 1995b; Hazan and Norton, 1998). On a molecular level, EGFR signalling leads to tyrosine phosphorylation of the catenin complex with subsequent breakdown of cell adhesion (Shiozaki et al, 1995; Jawhari et al, 1999; Mariner et al, 2004).
In this study, we examined whether the beneficial anticancer effects of Cetrorelix include effects in addition to the established antiproliferative effects. Luteinising hormone-releasing hormone (LHRH) receptors have increased expression in many cancers compared to normal cells (Emons et al, 1998; Schally et al, 2001; Straub et al, 2001), with increased expression in benign prostate hyperplasia (BPH) as well (Straub et al, 2003). The presence of these receptors enables LHRH analogues to affect directly prostate tumour cells (Qayum et al, 1990; Halmos et al, 2000) in addition to the indirect central androgen suppression. In addition, it has been shown that LHRH agonists directly inhibit cell proliferation of DU-145 and LNCaP prostate cancer cell lines (Dondi et al, 1994, 1998; Limonta et al, 2001). In line with these observations, the LHRH analogue Cetrorelix has been shown to have direct antiproliferative actions on DU-145 cells (Jungwirth et al, 1997b). As a consequence of this exposure, LHRH analogues have caused decreased levels of EGFR expression (Moretti et al, 1996; El-Bahrawy and Pignatelli, 1998; Lamharzi et al, 1998).
Previously, we have shown that DU-145 WT, a subline of the human prostate carcinoma cell line DU-145, presents autocrine EGFR signalling that is critical to both cell proliferation and invasion (Xie et al, 1995; Turner et al, 1996). Recently, we demonstrated under both in vivo and in vitro conditions that a LHRH agonist inhibited enhanced invasiveness of EGFR-dependent proliferation in DU-145 WT through interference with EGFR signalling (Wells et al, 2002). Therefore, these data taken together lead us to hypothesise that the LHRH analogue Cetrorelix would abrogate EGFR signalling. This abrogation would in turn decrease phosphorylation of the associated catenins, thus leading to upregulation of the cell adhesion molecule E-cadherin, which may ultimately result in inhibition of prostatic tumour progression.
Materials and methods
Materials
The LHRH analogue Cetrorelix ((Ac-D-Nal (2)1, D-Phe (4Cl)2, D-Pal (3)3, D-Cit6, D-Ala10) LH-RH) was obtained from ASTA Medica (Frankfurt/Main, Germany) and dissolved in serum-free Dulbecco's modified Eagle's medium (DMEM). The primary antibodies used were mouse monoclonal antibodies to E-cadherin, α- and β-catenin, and p120 (Transduction Laboratories, California, USA), phosphorylated MARCKS (Cell Signaling, Massachusetts, USA), phosphorylated EGFR (Cell Signaling, Massachusetts, USA), and EGFR (Zymed Laboratories, California, USA). FITC-conjugated secondary antibodies were obtained from BD Biosciences (California, USA). Secondary antibodies for the immunofluorescence were obtained from Molecular Probes (Oregon, USA). Inhibitors included the EGFR-specific tyrosine kinase inhibitor PD153035 (CalBiochem, California, USA), monoclonal antibody (528) EGFR (Oncogene, Massachusetts, USA), EGFR siRNA (Upstate, Virginia, USA), and the transcriptional and translational inhibitor puromycin (Sigma, Missouri, USA). Other reagents were obtained from Sigma.
DU-145 cell lines
The cell line DU-145 was originally derived from a brain metastasis of a human prostate adenocarcinoma (Stone et al, 1978); it retains the androgen independence of the original tumour and does not express a functional androgen receptor (Dondi et al, 1998). This cell line possesses both LHRH and EGF receptors and produces EGFR ligands TGF-α and EGF (Xie et al, 1995; Jungwirth et al, 1997a). We have expressed exogenously encoded EGFR in DU-145 cells (Xie et al, 1995). Utilising established protocols, DU-145 cells were transfected by retroviral-containing EGFR constructs (Wells et al, 1990). The wild-type (WT) EGFR construct is a full-length cDNA derived from a placental cDNA library. Cells expressing WT EGFR at levels that escape downregulation demonstrate enhanced invasiveness in vitro (Xie et al, 1995) and in vivo (Turner et al, 1996).
The DU-145 WT subline expresses EGFRs that are phosphorylated and negatively modulated by protein kinase C (PKC); thus, we have generated an additional DU-145 subline that is not negatively modulated by PKC (Wells et al, 2002). This subline is identical to DU-145 WT except that it contains a full-length EGFR in which the target site for PKC phosphorylation, amino-acid threonine 654 (T654), has been replaced with alanine (DU-145 A654) by site-directed mutagenesis; this construct is resistant to PKC phosphorylation and negative transmodulation (Welsh et al, 1991; Chen et al, 1996).
The DU-145 WT and A654 cells were maintained in DMEM (4.5 g ml−1 glucose) (Cellgro, Virginia, USA) containing 10% FBS and supplemented with L-glutamine (2 mM), penicillin/streptomycin (100 U ml−1), nonessential amino acids (0.1 mM), and sodium pyruvate (1 mM) (37°C, 90% humidity, 5% CO2 and 95% air). For stable selection of WT or A654 EGFR, cells were grown in G418 (1000 μg ml−1) (Gibco, New York, USA), although all experiments were performed in the absence of G418.
Invasion assay
Cell invasiveness in vitro was determined by the ability of cells to transmigrate a layer of extracellular matrix, Matrigel, in a Boyden Chamber assay. Matrigel invasion chamber plates were obtained from Becton Dickinson Labware (Bedford, Massachusetts, USA). A total of 20 000 cells were plated in the Matrigel-containing chamber in serum-free media containing 1% BSA for the first 24 h; this was then replaced with Cetrorelix serum-free media for the remaining 24 h. Enumeration of the cells that invaded through the matrix over a 48 h period was accomplished by visually counting cells on the bottom of the filter. All experiments were performed in triplicate chambers.
Flow cytometry
Cells (3 × 105) were grown for 2 days or to 80% confluency in 60 mm plates. The LHRH analogue Cetrorelix (10−5 M) was added for time intervals of 6, 12, and 24 h and compared to diluent alone. Samples were washed with PBS and fixed with paraformaldehyde, and permeabilised with 1% Triton X-100. Samples were blocked with 5% BSA and incubated with the appropriate FITC-conjugated primary antibody or primary antibody (anti-EGFR, anti-E-cadherin, anti-α-catenin, anti-β-catenin, and anti-p120) at 37°C for 1 h. For unconjugated samples, FITC-conjugated secondary antibody was added. Fluorescence was measured by a flow cytometer (Coulter, Florida, USA).
Immunoblotting
Cells (3 × 105) were grown for 2 days or to 80% confluency in six-well plates. The LHRH analogue Cetrorelix (10−5 M) was incubated for 6, 12, and 24 h time intervals and compared to diluent alone. Protein lysates were prepared from cultured cells in the following buffer: 50 mM Tris, pH 7.5, 120 mM NaCl, 0.5% Nonidet P-40, 40 μ M phenylmethylsulphonylfluoride (PMSF), 50 μg ml−1 leupeptin, and 50 μg ml−1 aprotinin (all from Sigma). Cells were allowed to lyse for 1 h on ice; the lysed cell solution was centrifuged and the resulting supernatants were extracted and quantitated using a Bradford assay. Protein lysates (30 μg) were separated by 7.5% SDS–PAGE, immunoblotted, and analysed using chemiluminescence (Amersham Biosciences, New Jersey, USA). Primary antibodies used included anti-EGFR (Zymed Diagnostics, California, USA), anti-E-cadherin, anti-β-catenin, and anti-p120 (Transduction Laboratories, Kentucky, USA), and anti-α-catenin (Santa Cruz Biotechnology, California, USA). The staining was visualised by a secondary anti-mouse IgG or anti-rabbit antibody linked to horseradish peroxidase (Promega, Wisconsin, USA).
siRNA for EGFR
A total of 2 × 105 cells were plated in six-well plates equalling 60–70% confluency. The EGFR siRNA (160 pmol) was diluted in 200 μl of Opti-MEM (Invitrogen, California, USA). A 4 μl portion of Lipofectamine 2000 (Invitrogen, California, USA) was diluted in 200 μl of Opti-MEM and incubated for 5 min at room temperature. The diluted siRNA and Lipofectamine 2000 were mixed and incubated for 20 min at room temperature. Complexes were added to each well and incubated for 24 h. Media were changed and incubated for an additional 24 h. Cells were lysed according to established protocols.
Immunofluorescence microscopy
A total of 3 × 105 cells were grown for 2 days or to 80% confluency on glass coverslips and then treated with or without Cetrorelix (10−5 M) and compared to diluent alone. Cells were then fixed in 4% paraformaldehyde, permeabilised with 100 mM Tris-HCl pH 7.4, 150 mM NaCl, 10 mM EGTA, 1% Triton X-100, 1 mM PMSF, and 50 μg ml−1 aprotinin (all from Sigma), and subsequently blocked with 5% BSA for 1 h at room temperature. Samples were incubated with indicated primary antibodies diluted in blocking buffer at 4°C overnight. FITC-conjugated secondary antibody was then added (BD Biosciences, California, USA). Cells were then stained with propidium iodine for nuclear staining. Cells were analysed with laser confocal microscopy using a Leica TCSNT 3 laser 4 PMT system (Olympus, New York, USA).
Cell aggregation assay
Calcium-dependent aggregation of the DU-145 sublines was measured as previously described by Takeichi (1995) with the following modifications. Cell monolayers grown to 80% confluence were incubated for 24 or 48 h in 10% FBS in DMEM with or without 10−5 M Cetrorelix. Cell monolayers were detached from the culture dishes by incubating in cell stripper (Cell Gro, Virginia, USA) for 5–10 min at 37°C. Any remaining cells were detached using a rubber policeman, washed once with PBS, and collected by centrifugation. Cells were resuspended in 10% FBS in DMEM and single-cell suspensions made by trituration with a Pasteur pipette. Cell number was determined in the Coulter Counter Z1 (Coulter, Florida, USA). Cells were plated in triplicate wells of a 24-well plate at 2 × 105 cells well−1 in 10% FBS in DMEM with 1 mM CaCl2 and allowed to aggregate for 60 min on a gyratory shaker at 80 r.p.m. at 37°C. Assays were stopped at 0 and 60 min by fixing the cells in 0.5% paraformaldehyde. The extent of cell–cell binding was monitored by measuring the disappearance of single cells using the Coulter Counter Z1. The index of the degree of aggregation was measured utilising the formula 100 × (N0/N60), where N0 is the total cell number per well and N60 is the total number of particles after 60 min of incubation as determined by counting in a Coulter Counter Z1.
Statistical analysis
Statistics for all experiments were performed using the Sigma Plot statistical program (Jandel Scientific, California, USA). Independent Student's t-test was utilised to determine a statistical difference between experimental and the controls for individual experiments.
Results
The LHRH analogue Cetrorelix decreases invasion in DU-145 sublines
To confirm and extend the inhibitory effects of Cetrorelix on prostate carcinomas, we utilised a genetically engineered human androgen-independent prostate carcinoma cell line that overexpresses a full-length EGFR, DU-145 WT. This subline is highly invasive in response to upregulation of autocrine EGFR signalling (Xie et al, 1995; Turner et al, 1996) that exists in practically all prostate carcinomas (Kim et al, 1999). In determining the utilised dose of Cetrorelix, we selected the pharmacologic dose of 10−5 M based on literature reports for Cetrorelix (Tang et al, 2002) and a related LHRH analogue goserelin (Dondi et al, 1994; Jungwirth et al, 1997a, 1997b; Limonta et al, 1998; Wells et al, 2002). In addition, growth studies from our laboratory utilising Cetrorelix at 10−5 M inhibited DU-145 WT proliferation without causing cell death (data not shown).
To probe the extent of effectiveness of Cetrorelix against prostate cancer progression, we determined whether invasion was abrogated. Cetrorelix exposure reduced the invasiveness of the DU-145 WT sublines through a Matrigel barrier from 100% down to 23±14% (Figure 6; n=4, P<0.05). This level of inhibition is comparable to the decreases noted when either EGFR motility signalling via PLCγ or calpain signalling is abrogated (Xie et al, 1995; Turner et al, 1996; Kassis et al, 1999; Mamoune et al, 2003).
Cetrorelix reduced the invasiveness of the DU-145 parental (□) and DU-145 WT (▪) cells while only partly affecting that of DU-145 A654 (▒) cells. Invasiveness was measured by the cells' ability to transmigrate the extracellular matrix, Matrigel, in a Boyden Chamber assay. Data are the mean±s.e.m. (n=4). *P<0.05, Cetrorelix-treated (48 h) groups vs controls (diluent only), without drug; also P<0.05 between the extent of decreased invasiveness of WT and A654 cells in the presence of Cetrorelix.
Cetrorelix increases levels of cell adhesion molecules
To determine the effectiveness of Cetrorelix treatment on altering protein expression levels, we measured EGFR, E-cadherin, and its associated adhesion molecules (α- and β-catenins, and p120) by flow cytometry. After 6 h of Cetrorelix exposure, EGFR levels were significantly reduced in DU-145 WT cells when compared to nontreated, control levels. This significant reduction in EGFR levels continued throughout the 24 h experimental time period (Figure 1A; P<0.05). While Cetrorelix decreased EGFR surface expression, it induced an increase in E-cadherin levels (Figure 1B). Likewise, the E-cadherin-associated molecules α-catenin, β-catenin, and p120 also demonstrated a continual increase in their expression, with all showing significant increases after 24 h of Cetrorelix exposure (Figure 1C–E; P<0.05%). To confirm results obtained from the flow cytometry experiments, we immunoblotted for whole-cell protein content of total EGFR and adhesion molecules E-cadherin and β-catenin. Again a similar pattern was seen, with a reduction in EGFR levels and an increase in E-cadherin and β-catenin levels (data not shown).
Expression levels were measured as the mean of per cent positive fluorescence at time zero±s.e.m. at various time intervals. (A) DU-145 WT cells labelled with FITC-conjugated anti-EGFR were analysed by flow cytometry. (B) DU-145 WT cells labelled with FITC-conjugated anti-E-cadherin were analysed by flow cytometry. (C) DU-145 WT cells labelled with FITC-conjugated anti-β-catenin were analysed by flow cytometry. (D) DU-145 WT cells labelled with FITC-conjugated anti-α-catenin were analysed by flow cytometry. (E) DU-145 WT cells labelled with FITC-conjugated anti-p120 were analysed by flow cytometry. Data are the mean±s.e.m. of three experiments each performed in triplicate. *P<0.05 compared to untreated.
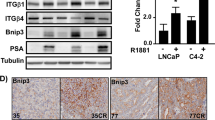
To thoroughly examine if the increases in protein and expression levels of E-cadherin and β-catenin were associated with upregulation in transcription, we used the protein synthesis inhibitor puromycin. Puromycin exposure was able to block completely the enhanced ability of Cetrorelix to restore the E-cadherin and β-catenin expression levels (Figure 2).
DU-145 WT cells were challenged with ±puromycin (40 μ M) in the presence of Cetrorelix (10−5 M) for 24 h. Lysates were collected and separated by SDS–PAGE, transferred, and immunoblotted with antibody to E-cadherin, antibody to β-catenin, or antibody to the loading control β-actin. Shown are representative blots of two experiments.
Reversal in adhesion molecule profile is related to EGFR signalling
A role for Cetrorelix in the stimulation of PKC activity was determined by phosphorylation of the MARCKS substrate for classical and novel PKC isoforms or by probing for generalised increased phosphorylation of canonical PKC target serines (Figure 3) (Fujise et al, 1994; Nishikawa et al, 1997). This was further confirmed through the use of chelerythrine, a pan-PKC inhibitor (Wells et al, 2002), to prevent such phosphorylation (data not shown).
Top immunoblot: DU-145 WT cells were exposed to Cetrorelix (10−5 M) from 30 min to 4 h. Lysates were collected and separated by SDS–PAGE, transferred, and immunoblotted with antibody recognising phosphorylated MARCKS. Bottom immunoblot: DU-145 WT cells were challenged and immunoblotted with antibody recognising phosphorylated serine in the context of canonical PKC target sites. The bottom immunoblot demonstrates loading control of β-actin. Increases observed in the top two immunoblots are comparable to PMA-positive control. Shown are representative blots of three experiments.
If Cetrorelix acts via PKC-mediated attenuation of EGFR signalling, then an EGFR variant lacking the PKC target site should be resistant. We utilised a DU-145 subline expressing an EGFR construct in which the target PKC site, threonine 654, was replaced by an alanine (DU-145 A654). Since Cetrorelix decreased EGFR surface levels (Figure 1A) and increased surface levels and protein levels of cell adhesion molecules (Figures 1B–E and 2), cells expressing this EGFR A654 construct should be at least partly resistant to Cetrorelix. Through the use of immunoblotting techniques, we examined the protein levels of the cell adhesion molecules after 24 h of Cetrorelix exposure. Phosphorylated and total EGFR levels, as well as total E-cadherin and β-catenin levels were not extensively altered in the DU-145 A654 cells when compared to changes observed in DU-145 WT cells (Figure 4). These findings indicate that direct abrogation of EGFR signalling by various means should yield a similar increase in E-cadherin and β-catenin levels. Both the specific tyrosine kinase inhibitor PD153035 and the anti-EGFR antibody (mb528) increased E-cadherin and β-catenin levels similarly to those observed in DU-145 WT after Cetrorelix treatment (Figure 5A and B). Finally, exposure of DU-145 WT cells to EGFR siRNA resulted in the downregulation of EGFR levels and an increase in E-cadherin levels when compared to cells exposed to the nonrelevant siGFP (Figure 5C).
DU-145 WT (left immunoblots) and A654 (right immunoblots) cells were exposed to Cetrorelix (10−5 M) for up to 24 h. Lysates were collected and separated by SDS–PAGE, transferred, and immunoblotted with antibodies to p-EGFR, EGFR, E-cadherin, and β-catenin. Similar data were seen with α-catenin and p120 (data not shown). Shown are representative examples of three experiments.
(A) DU-145 WT cells were exposed to PD153035 for 6, 12, and 24 h. (B) DU-145 WT cells were exposed to monoclonal antibody (528) against EGFR for 6, 12, and 24 h. (C) The EGFR siRNA was exposed to cells for 24 h and compared to the GFP siRNA. Lysates were collected and separated by SDS–PAGE, transferred, and immunoblotted with antibodies recognising EGFR, E-cadherin and β-catenin. Both β-actin and GAPDH were used as loading controls. One of two experiments for each point is shown.
Cetrorelix diminished prostate cancer cell invasiveness
The functional consequences of EGFR signalling crossattenuation by Cetrorelix extend to the invasive potential of the prostate carcinoma cells. While Cetrorelix significantly reduced the invasiveness of the DU-145 parental and WT cells, the invasiveness of DU-145 A654 was limited to a lesser extent (Figure 6; P<0.05, comparing Matrigel invasion after Cetrorelix treatment of DU-145 A654 and WT cells). These findings suggest that the effects of Cetrorelix on both cell–cell adhesion molecules and cell invasiveness are mediated through its interference with the EGFR signalling cascade.
Cetrorelix exposure increases cell–cell aggregation
To further assess the functional consequences of the concurrent Cetrorelix-related decrease in EGFR levels and the increase in E-cadherin and its associated proteins observed in the DU-145 WT subline, a calcium-dependent aggregation assay was used after 48 h of Cetrorelix exposure (Figure 7). In these experiments, the aggregation index of DU-145 WT and A654 cells treated with Cetrorelix was compared to that of nontreated cells. We observed that DU-145 WT cells exposed to Cetrorelix formed significantly more cell–cell aggregates compared to either nontreated WT cells or treated and nontreated A654 cells, while Cetrorelix-induced DU-145 A654 aggregation was indistinguishable from nontreated cells (Figure 7; P<0.05). We were also able to see similar results when we exposed DU-145 WT cells to PD153035 to block EGFR signalling (Figure 7B; P<0.05%).
(A) Cetrorelix increased the cell–cell aggregation of the DU-145 WT (▪) cells after 48 h of exposure, while not affecting DU-145 A654 (▒) cells. (B) The EGFR inhibitor PD153035 increased the cell–cell aggregation of the DU-145 WT after 48 h of exposure. Results are expressed as the mean of the index of the degree of aggregation vs time zero±s.e.m. at 1 h (n=3, each in triplicate). *P<0.05, Cetrorelix-treated (+) groups vs controls (−), without drug.
Cell–cell aggregation requires E-cadherin to be present on the cell surface and its associate molecules at the inner face of the plasma membrane. In DU-145 WT cells, these adhesion complex molecules were distributed throughout the cytosol (Figure 8). Upon Cetrorelix treatment, not only did the levels increase, but also the molecules were redistributed to the cells' periphery; this was particularly evident at sites of cell–cell contacts, regardless of the degree of cell confluence. In aggregate, these data further confirmed with functional application that the increases observed in E-cadherin, α-and β-catenins, and p120 levels in Cetrorelix-exposed DU-145 WT cells are the results of a reversal of the cells invasive phenotype to one that resembles a more normal phenotype and that Cetrorelix exerts at least some of its effects via abrogation of autocrine EGFR cell signalling.
Cells were exposed to Cetrorelix for up to 48 h prior to immunofluorescent localisation of E-cadherin (top panels), α- and β-catenins (second and third panels, respectively), or p120 (bottom panels) and compared to 48 h diluent alone (right panel). Shown are representative photomicrographs of two independent experiments; the target molecules are green and nuclei are red.
Discussion
The LHRH analogue Cetrorelix is undergoing evaluation for prostate cancer treatment. While initially considered for treatment due to its central androgen suppression mechanism, direct cancer cell efficacy has been shown. Cetrorelix has been demonstrated to limit proliferation of a variety of human cancer cell lines, including breast, ovarian, endometrial (Yap et al, 1997; Schally, 1999), and prostate cancer cell lines (Qayum et al, 1990; Halmos et al, 2000). Herein, we examined whether Cetrorelix altered an important phenotype of tumour cells, decreased cell–cell adhesion. We found that Cetrorelix exposure increased the levels of cell adhesion molecules and enhanced the resultant cell–cell adhesion. Furthermore, Cetrorelix appears to function, at least in part, by crossattenuation of signalling from the EGFR.
Several studies have long established that the loss of the homotypic E-cadherin binding machinery correlates with an invasive phenotype in prostate carcinomas (Behrens et al, 1989; Vleminckx et al, 1991; Bussemakers et al, 1992). Thus, it is logical that this cell–cell zipper would disappear concomitant with increased cellular invasion (Shibata et al, 1994). This disappearance of E-cadherin and/or any of the major adhesion components affiliated with it is noted in most advanced carcinoma cells (Takeichi, 1977; Hazan and Norton, 1998; Takeda et al, 1999). In fact, re-expression of E-cadherin has been shown to reduce the tumorigenicity of some carcinoma cell lines (Jawhari et al, 1999; Lowy et al, 2002). Interestingly, Cetrorelix exposure increases the levels of all of the major adhesion molecules probed; this could be secondary to either increased transcription or decreased degradation. This should subsequently lead to the reforming of the zipper. This was corroborated in our invasion (Figure 6) and aggregation studies (Figure 7A and B) where, after extended Cetrorelix exposure, the highly invasive WT cell line became less invasive and aggregated to a greater extent than nontreated cells.
The ability to exploit the findings that Cetrorelix treatment increases both cell–cell adhesion and the levels of the key molecules involved in the adhesion process is vastly improved by defining the underlying basis for this occurrence. Other LHRH analogues have been shown to limit prostate carcinoma cell growth secondary to downregulation of EGFR (Moretti et al, 1996; Jungwirth et al, 1997a, 1997b) or through interference with signalling pathways initiated by the EGFR (Wells et al, 2002). This occurred via PKC-mediated crossattenuation (Wells et al, 2002) secondary to phosphorylation on threonine 654 of EGFR (Lin et al, 1986; Welsh et al, 1991). In this study, we show direct activation of PKC substrate MARCKS by LHRH receptors in a time-dependent manner (Figure 3). These findings led us to believe that DU-145 cells engineered to express the PKC-resistant A654 EGFR should be impervious to Cetrorelix treatment. This was borne out by our findings that EGFR levels remained high and cell adhesion molecule levels low in these cells in the face of Cetrorelix exposure (Figure 4). The importance of EGFR signalling was further demonstrated in a time-dependent manner from the exposure of the DU-145 WT subline to an EGFR-specific tyrosine kinase inhibitor, PD153035, and a monoclonal antibody against EGFR (mb528) (Figure 5A and B). Cetrorelix and PD153035 both increased cell–cell adhesion in DU-145 WT, but had little effect on DU-A654 cells (Figure 7). The results of all of our findings taken together indicate that the ability of the LHRH analogue Cetrorelix to alter the adhesive profile of these cells is at least partly mediated through altered EGFR signalling.
That Cetrorelix restores cell–cell adhesion secondary to disrupting EGFR signalling would be supported if EGFR signalling could be shown to downregulate cell–cell adhesion. This was shown to occur at least in the DU-145 WT cells by their increased aggregation upon disruption of autocrine EGFR signalling (Figure 7). Epidermal growth factor receptor signalling, upregulated in an autocrine manner in prostate carcinomas (Kim et al, 1999), was shown to be responsible, at least in part, for the downregulation of cadherin-mediated adhesion and levels of molecules noted in these tumours as it is in many other carcinomas (Sorscher et al, 1995a, 1995b; Wilding et al, 1996; Jawhari et al, 1999; Andl et al, 2003). Another report indicated that EGFR downregulation resulted in decreasing E-cadherin and catenins in ovarian carcinoma cells (Alper et al, 2000). Although the reason for this opposite effect in these cells was not obvious, it may be related to the distinct nature of some ovarian cell types. Presumably, such a reduction in the levels of adhesion molecules plays a major role in prostate cancer progression (Wells, 2000). How EGFR signalling limits cadherin-mediated adhesions is still being deciphered (Ackland et al, 2003; Cozzolino et al, 2003). However, this appears to involve both acute phosphorylation of PKC and the dissociation and subsequent degradation of key adhesion components. Regardless of the actual mechanism, the end result is witnessed in the long-term downregulation of these molecules.
In summary, we found that Cetrorelix restored the adhesiveness of the human prostate carcinoma cells (and significantly inhibited cellular proliferation) at similarly high pharmacologic doses used by others (Jungwirth et al, 1997a; Tang et al, 2002). Additionally, the LHRH agonist Zoladex was shown to only inhibit in vitro cell proliferation of androgen-dependent (LNCaP) and androgen-independent (DU-145) cell lines at similarly high concentrations (Moretti et al, 1996; Wells et al, 2002). Thus it seems that higher concentrations of LHRH analogues are needed to accomplish direct cell growth inhibition than to achieve androgen suppression. There are obvious speculative reasons for this, but regardless of the mechanism, these studies serve as proofs of concepts that this signalling axis can be exploited to limit prostate tumour progression. It remains to be determined whether therapeutic interventions will exploit this using higher affinity analogues or indirect augmentation of the described pathway that crossattenuates the autocrine EGFR signalling pathway in tumour promotion.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aberle H, Butz S, Stappert J, Weissig H, Kemler R, Hoschuetzky H (1994) Assembly of the cadherin–catenin complex in vitro with recombinant proteins. J Cell Sci 107 (Part 12): 3655–3663
Ackland ML, Newgreen DF, Fridman M, Waltham MC, Arvanitis A, Minichiello J, Price JT, Thompson EW (2003) Epidermal growth factor-induced epithelio-mesenchymal transition in human breast carcinoma cells. Lab Invest 83: 435–448
Alper O, De Santis ML, Stromberg K, Hacker NF, Cho-Chung YS, Salomon DS (2000) Anti-sense suppression of epidermal growth factor receptor expression alters cellular proliferation, cell-adhesion and tumorigenicity in ovarian cancer cells. Int J Cancer 88: 566–574
Andl CD, Mizushima T, Nakagawa H, Oyama K, Harada H, Chruma K, Herlyn M, Rustgi AK (2003) Epidermal growth factor receptor mediates increased cell proliferation, migration, and aggregation in esophageal keratinocytes in vitro and in vivo. J Biol Chem 278: 1824–1830
Behrens J, Mareel MM, Van Roy FM, Birchmeier W (1989) Dissecting tumor cell invasion: epithelial cells acquire invasive properties after the loss of uvomorulin-mediated cell–cell adhesion. J Cell Biol 108: 2435–2447
Birchmeier W, Behrens J (1994) Cadherin expression in carcinomas: role in the formation of cell junctions and the prevention of invasiveness. Biochim Biophys Acta 1198: 11–26
Bussemakers MJ, van Moorselaar RJ, Giroldi LA, Ichikawa T, Isaacs JT, Takeichi M, Debruyne FM, Schalken JA (1992) Decreased expression of E-cadherin in the progression of rat prostatic cancer. Cancer Res 52: 2916–2922
Chen P, Xie H, Wells A (1996) Mitogenic signaling from the egf receptor is attenuated by a phospholipase C-gamma/protein kinase C feedback mechanism. Mol Biol Cell 7: 871–881
Chitaev NA, Troyanovsky SM (1998) Adhesive but not lateral E-cadherin complexes require calcium and catenins for their formation. J Cell Biol 142: 837–846
Comoglio PM, Boccaccio C (2001) Scatter factors and invasive growth. Semin Cancer Biol 11: 153–165
Comoglio PM, Trusolino L (2002) Invasive growth: from development to metastasis. J Clin Invest 109: 857–862
Conacci-Sorrell M, Zhurinsky J, Ben-Ze'ev A (2002) The cadherin–catenin adhesion system in signaling and cancer. J Clin Invest 109: 987–991
Cozzolino M, Stagni V, Spinardi L, Campioni N, Fiorentini C, Salvati E, Alema S, Salvatore AM (2003) p120 catenin is required for growth factor-dependent cell motility and scattering in epithelial cells. Mol Biol Cell 14: 1964–1977
Davies G, Jiang G, Mason MD (2000) Cell–cell adhesion molecules and signaling intermediates and their role in the invasive potential of prostate cancer cells. J Urol 163: 985–992
Dondi D, Limonta P, Moretti RM, Marelli MM, Garattini E, Motta M (1994) Antiproliferative effects of luteinizing hormone-releasing hormone (LHRH) agonists on human androgen-independent prostate cancer cell line DU 145: evidence for an autocrine-inhibitory LHRH loop. Cancer Res 54: 4091–4095
Dondi D, Moretti RM, Montagnani Marelli M, Pratesi G, Polizzi D, Milani M, Motta M, Limonta P (1998) Growth-inhibitory effects of luteinizing hormone-releasing hormone (LHRH) agonists on xenografts of the DU 145 human androgen-independent prostate cancer cell line in nude mice. Int J Cancer 76: 506–511
Downing JR, Reynolds AB (1991) PDGF, CSF-1, and EGF induce tyrosine phosphorylation of p120, a pp60src transformation-associated substrate. Oncogene 6: 607–613
El-Bahrawy MA, Pignatelli M (1998) E-cadherin and catenins: molecules with versatile roles in normal and neoplastic epithelial cell biology. Microsc Res Tech 43: 224–232
Emons G, Muller V, Ortmann O, Schulz KD (1998) Effects of LHRH-analogues on mitogenic signal transduction in cancer cells. J Steroid Biochem Mol Biol 65: 199–206
Fidler IJ (2003) The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer 3: 453–458
Fujise A, Mizuno K, Ueda Y, Osada S, Hirai S, Takayanagi A, Shimizu N, Owada MK, Nakajima H, Ohno S (1994) Specificity of the high affinity interaction of protein kinase C with a physiological substrate, myristoylated alanine-rich protein kinase C substrate. J Biol Chem 269: 31642–31648
Funayama N, Fagotto F, McCrea P, Gumbiner BM (1995) Embryonic axis induction by the armadillo repeat domain of beta-catenin: evidence for intracellular signaling. J Cell Biol 128: 959–968
Grunert S, Jechlinger M, Beug H (2003) Diverse cellular and molecular mechanisms contribute to epithelial plasticity and metastasis. Nat Rev Mol Cell Biol 4: 657–665
Gumbiner BM (1996) Cell adhesion: the molecular basis of tissue architecture and morphogenesis. Cell 84: 345–357
Halmos G, Arencibia JM, Schally AV, Davis R, Bostwick DG (2000) High incidence of receptors for luteinizing hormone-releasing hormone (LHRH) and LHRH receptor gene expression in human prostate cancers. J Urol 163: 623–629
Hazan RB, Norton L (1998) The epidermal growth factor receptor modulates the interaction of E-cadherin with the actin cytoskeleton. J Biol Chem 273: 9078–9084
Hulsken J, Birchmeier W, Behrens J (1994) E-cadherin and APC compete for the interaction with beta-catenin and the cytoskeleton. J Cell Biol 127: 2061–2069
Jawhari AU, Farthing MJ, Pignatelli M (1999) The E-cadherin/epidermal growth factor receptor interaction: a hypothesis of reciprocal and reversible control of intercellular adhesion and cell proliferation. J Pathol 187: 155–157
Jou YS, Layhe B, Matesic DF, Chang CC, de Feijter AW, Lockwood L, Welsch CW, Klaunig JE, Trosko JE (1995) Inhibition of gap junctional intercellular communication and malignant transformation of rat liver epithelial cells by neu oncogene. Carcinogenesis 16: 311–317
Jungwirth A, Pinski J, Galvan G, Halmos G, Szepeshazi K, Cai RZ, Groot K, Vadillo-Buenfil M, Schally AV (1997a) Inhibition of growth of androgen-independent DU-145 prostate cancer in vivo by luteinising hormone-releasing hormone antagonist Cetrorelix and bombesin antagonists RC-3940-II and RC-3950-II. Eur J Cancer 33: 1141–1148
Jungwirth A, Schally AV, Pinski J, Halmos G, Groot K, Armatis P, Vadillo-Buenfil M (1997b) Inhibition of in vivo proliferation of androgen-independent prostate cancers by an antagonist of growth hormone-releasing hormone. Br J Cancer 75: 1585–1592
Kassis J, Moellinger J, Lo H, Greenberg NM, Kim HG, Wells A (1999) A role for phospholipase C-gamma-mediated signaling in tumor cell invasion. Clin Cancer Res 5: 2251–2260
Kielhorn E, Provost E, Olsen D, D'Aquila TG, Smith BL, Camp RL, Rimm DL (2003) Tissue microarray-based analysis shows phospho-beta-catenin expression in malignant melanoma is associated with poor outcome. Int J Cancer 103: 652–656
Kim H, Turner T, Kassis J, Souto J, Wells A (1999) EGF receptor signaling in prostate development. Histol Histopathol 14: 1175–1182
Kim JS, Crooks H, Foxworth A, Waldman T (2002) Proof-of-principle: oncogenic beta-catenin is a valid molecular target for the development of pharmacological inhibitors. Mol Cancer Ther 1: 1355–1359
Lamharzi N, Halmos G, Jungwirth A, Schally AV (1998) Decrease in the level and mRNA expression of LH-RH and EGF receptors after treatment with LH-RH antagonist Cetrorelix in DU-145 prostate tumor xenografts in nude mice. Int J Oncol 13: 429–435
Limonta P, Montagnani Marelli M, Moretti RM (2001) LHRH analogues as anticancer agents: pituitary and extrapituitary sites of action. Expert Opin Investig Drugs 10: 709–720
Limonta P, Pratesi G, Moretti RM, Montagnani Marelli M, Motta M, Dondi D (1998) Comments on inhibition of growth of androgen-independent DU-145 prostate cancer in vivo by luteinising hormone-releasing hormone antagonist Cetrorelix and bombesin antagonists RC-3940-II and RC-3950-II, Jungwirth et al., Eur J Cancer 1997, 33(7), 1141–1148. Eur J Cancer 34: 1134–1136
Lin CR, Chen WS, Lazar CS, Carpenter CD, Gill GN, Evans RM, Rosenfeld MG (1986) Protein kinase C phosphorylation at Thr 654 of the unoccupied EGF receptor and EGF binding regulate functional receptor loss by independent mechanisms. Cell 44: 839–848
Liu J, Ikeguchi M, Nakamura S, Kaibara N (2002) Re-expression of the cadherin–catenin complex in lymph nodes with metastasis in advanced gastric cancer: the relationship with patient survival. J Exp Clin Cancer Res 21: 65–71
Lowy AM, Knight J, Groden J (2002) Restoration of E-cadherin/beta-catenin expression in pancreatic cancer cells inhibits growth by induction of apoptosis. Surgery 132: 141–148
Mamoune A, Luo JH, Lauffenburger DA, Wells A (2003) Calpain-2 as a target for limiting prostate cancer invasion. Cancer Res 63: 4632–4640
Mariner DJ, Davis MA, Reynolds AB (2004) EGFR signaling to p120-catenin through phosphorylation at Y228. J Cell Sci 117: 1339–1350
Mason MD, Davies G, Jiang WG (2002) Cell adhesion molecules and adhesion abnormalities in prostate cancer. Crit Rev Oncol/Hematol 41: 11–28
Minamoto T, Ougolkov AV, Mai M (2002) Detection of oncogenes in the diagnosis of cancers with active oncogenic signaling. Expert Rev Mol Diagn 2: 565–575
Moretti RM, Marelli MM, Dondi D, Poletti A, Martini L, Motta M, Limonta P (1996) Luteinizing hormone-releasing hormone agonists interfere with the stimulatory actions of epidermal growth factor in human prostatic cancer cell lines, LNCaP and DU 145. J Clin Endocrinol Metab 81: 3930–3937
Morita N, Uemura H, Tsumatani K, Cho M, Hirao Y, Okajima E, Konishi N, Hiasa Y (1999) E-cadherin and alpha, beta, gamma-catenin expression in prostate cancers: correlation with tumor invasion. Br J Cancer 79: 1879–1883
Nishikawa K, Toker A, Johannes FJ, Songyang Z, Cantley LC (1997) Determination of the specific substrate sequence motifs of protein kinase C isozymes. J Biol Chem 272: 952–960
Pignatelli M, Vessey CJ (1994) Adhesion molecules: novel molecular tools in tumor pathology. Hum Pathol 25: 849–856
Qayum A, Gullick W, Clayton RC, Sikora K, Waxman J (1990) The effects of gonadotrophin releasing hormone analogues in prostate cancer are mediated through specific tumour receptors. Br J Cancer 62: 96–99
Richmond PJ, Karayiannakis AJ, Nagafuchi A, Kaisary AV, Pignatelli M (1997) Aberrant E-cadherin and alpha-catenin expression in prostate cancer: correlation with patient survival. Cancer Res 57: 3189–3193
Rimm DL, Sinard JH, Morrow JS (1995) Reduced alpha-catenin and E-cadherin expression in breast cancer. Lab Invest 72: 506–512
Schally AV (1999) Luteinizing hormone-releasing hormone analogs: their impact on the control of tumorigenesis. Peptides 20: 1247–1262
Schally AV, Comaru-Schally AM, Nagy A, Kovacs M, Szepeshazi K, Plonowski A, Varga JL, Halmos G (2001) Hypothalamic hormones and cancer. Front Neuroendocrinol 22: 248–291
Schneider SQ, Finnerty JR, Martindale MQ (2003) Protein evolution: structure–function relationships of the oncogene beta-catenin in the evolution of multicellular animals. J Exp Zool 295B: 25–44
Shibamoto S, Hayakawa M, Takeuchi K, Hori T, Miyazawa K, Kitamura N, Johnson KR, Wheelock MJ, Matsuyoshi N, Takeichi M (1995) Association of p120, a tyrosine kinase substrate, with E-cadherin/catenin complexes. J Cell Biol 128: 949–957
Shibata T, Gotoh M, Ochiai A, Hirohashi S (1994) Association of plakoglobin with APC, a tumor suppressor gene product, and its regulation by tyrosine phosphorylation. Biochem Biophys Res Commun 203: 519–522
Shino Y, Watanabe A, Yamada Y, Tanase M, Yamada T, Matsuda M, Yamashita J, Tatsumi M, Miwa T, Nakano H (1995) Clinicopathologic evaluation of immunohistochemical E-cadherin expression in human gastric carcinomas. Cancer 76: 2193–2201
Shiozaki H, Kadowaki T, Doki Y, Inoue M, Tamura S, Oka H, Iwazawa T, Matsui S, Shimaya K, Takeichi M (1995) Effect of epidermal growth factor on cadherin-mediated adhesion in a human oesophageal cancer cell line. Br J Cancer 71: 250–258
Sorscher SM, Green MR, Feramisco JR (1995a) Enhanced E-cadherin expression in epidermal growth factor receptor expressing cells. Biochem Biophys Res Commun 206: 518–524
Sorscher SM, Russack V, Graziano S, Cagle M, Feramisco JR, Green MR (1995b) Immunohistochemical evaluation of E-cadherin and epidermal growth factor receptor in non-small cell lung cancer. Mod Pathol 8: 450–455
Stone KR, Mickey DD, Wunderli H, Mickey GH, Paulson DF (1978) Isolation of a human prostate carcinoma cell line (DU 145). Int J Cancer 21: 274–281
Straub B, Muller M, Krause H, Schrader M, Goessl C, Heicappell R, Miller K (2001) Increased incidence of luteinizing hormone-releasing hormone receptor gene messenger RNA expression in hormone-refractory human prostate cancers. Clin Cancer Res 7: 2340–2343
Straub B, Muller M, Krause H, Schrader M, Miller K (2003) Real-time quantitative reverse transcriptase–polymerase chain reaction for luteinizing hormone-releasing hormone receptor gene mRNA expression in human prostate cancer. Urology 62: 172–176
Su LK, Vogelstein B, Kinzler KW (1993) Association of the APC tumor suppressor protein with catenins. Science 262: 1734–1737
Suyama K, Shapiro I, Guttman M, Hazan RB (2002) A signaling pathway leading to metastasis is controlled by N-cadherin and the FGF receptor. Cancer Cell 2: 301–314
Takeda H, Shimoyama Y, Nagafuchi A, Hirohashi S (1999) E-cadherin functions as a cis-dimer at the cell–cell adhesive interface in vivo. Nat Struct Biol 6: 310–312
Takeichi M (1977) Functional correlation between cell adhesive properties and some cell surface proteins. J Cell Biol 75: 464–474
Takeichi M (1993) Cadherins in cancer: implications for invasion and metastasis. Curr Opin Cell Biol 5: 806–811
Takeichi M (1995) Morphogenetic roles of classic cadherins. Curr Opin Cell Biol 7: 619–627
Tang X, Yano T, Osuga Y, Matsumi H, Yano N, Xu J, Wada O, Koga K, Kugu K, Tsutsumi O, Schally AV, Taketani Y (2002) Cellular mechanisms of growth inhibition of human epithelial ovarian cancer cell line by LH-releasing hormone antagonist Cetrorelix. J Clin Endocrinol Metab 87: 3721–3727
Thoreson MA, Anastasiadis PZ, Daniel JM, Ireton RC, Wheelock MJ, Johnson KR, Hummingbird DK, Reynolds AB (2000) Selective uncoupling of p120(ctn) from E-cadherin disrupts strong adhesion. J Cell Biol 148: 189–202
Turner T, Chen P, Goodly LJ, Wells A (1996) EGF receptor signaling enhances in vivo invasiveness of DU-145 human prostate carcinoma cells. Clin Exp Metast 14: 409–418
Umbas R, Schalken JA, Aalders TW, Carter BS, Karthaus HF, Schaafsma HE, Debruyne FM, Isaacs WB (1992) Expression of the cellular adhesion molecule E-cadherin is reduced or absent in high-grade prostate cancer. Cancer Res 52: 5104–5109
Van Aken E, De Wever O, Correia da Rocha AS, Mareel M (2001) Defective E-cadherin/catenin complexes in human cancer. Virchows Arch 439: 725–751
van de Wetering M, Sancho E, Verweij C, de Lau W, Oving I, Hurlstone A, van der Horn K, Batlle E, Coudreuse D, Haramis AP, Tjon-Pon-Fong M, Moerer P, van den Born M, Soete G, Pals S, Eilers M, Medema R, Clevers H (2002) The beta-catenin/TCF-4 complex imposes a crypt progenitor phenotype on colorectal cancer cells. Cell 111: 241–250
Vleminckx K, Vakaet Jr L, Mareel M, Fiers W, van Roy F (1991) Genetic manipulation of E-cadherin expression by epithelial tumor cells reveals an invasion suppressor role. Cell 66: 107–119
Wells A (2000) Tumor invasion: role of growth factor-induced cell motility. Adv Cancer Res 78: 31–101
Wells A, Souto JC, Solava J, Kassis J, Bailey KJ, Turner T (2002) Luteinizing hormone-releasing hormone agonist limits DU-145 prostate cancer growth by attenuating epidermal growth factor receptor signaling. Clin Cancer Res 8: 1251–1257
Wells A, Welsh JB, Lazar CS, Wiley HS, Gill GN, Rosenfeld MG (1990) Ligand-induced transformation by a noninternalizing epidermal growth factor receptor. Science 247: 962–964
Welsh JB, Gill GN, Rosenfeld MG, Wells A (1991) A negative feedback loop attenuates EGF-induced morphological changes. J Cell Biol 114: 533–543
Wilding J, Vousden KH, Soutter WP, McCrea PD, Del Buono R, Pignatelli M (1996) E-cadherin transfection down-regulates the epidermal growth factor receptor and reverses the invasive phenotype of human papilloma virus-transfected keratinocytes. Cancer Res 56: 5285–5292
Willert K, Nusse R (1998) Beta-catenin: a key mediator of Wnt signaling. Curr Opin Genet Dev 8: 95–102
Xie H, Turner T, Wang MH, Singh RK, Siegal GP, Wells A (1995) In vitro invasiveness of DU-145 human prostate carcinoma cells is modulated by EGF receptor-mediated signals. Clin Exp Metast 13: 407–419
Yap AS, Stevenson BR, Cooper V, Manley SW (1997) Protein tyrosine phosphorylation influences adhesive junction assembly and follicular organization of cultured thyroid epithelial cells. Endocrinology 138: 2315–2324
Acknowledgements
We thank Karlyn Bailey, Rich Bodnar, Cecelia Yates, and Diana Whaley for technical assistance and suggestions. We also thank ASTA Medica for graciously providing the Cetrorelix used in this study and Jennifer Grandis lab for providing the EGFR siRNA. The agent was provided without control over experimental design or publication. This study was supported by grants from the Department of Defense, Veterans Administration, and the Minority Biomedical Research Support and Research Centers in Minority Institutions grants from the National Institute of General Medical Sciences at the NIH.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Yates, C., Wells, A. & Turner, T. Luteinising hormone-releasing hormone analogue reverses the cell adhesion profile of EGFR overexpressing DU-145 human prostate carcinoma subline. Br J Cancer 92, 366–375 (2005). https://doi.org/10.1038/sj.bjc.6602350
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602350
Keywords
This article is cited by
-
Expression of E-cadherin and specific CXCR3 isoforms impact each other in prostate cancer
Cell Communication and Signaling (2019)
-
Gonadotropin-releasing hormone receptor activates GTPase RhoA and inhibits cell invasion in the breast cancer cell line MDA-MB-231
BMC Cancer (2012)
-
Hepatocyte induced re-expression of E-cadherin in breast and prostate cancer cells increases chemoresistance
Clinical & Experimental Metastasis (2012)
-
Detecting gene-gene interactions in prostate disease in African American men
Infectious Agents and Cancer (2011)
-
Agonists and antagonists of GnRH-I and -II reduce metastasis formation by triple-negative human breast cancer cells in vivo
Breast Cancer Research and Treatment (2011)