Abstract
The BCL-6 proto-oncogene is expressed in germinal center B lymphocytes, in their neoplastic counterparts, and in a subpopulation of germinal center and perifollicular T lymphocytes. Rearrangements and/or mutations of the 5′ noncoding region of the bcl-6 gene have been demonstrated in a large majority of diffuse large B cell lymphomas. Some, but not all, of these genetic alterations lead to dysregulation of the protein. Recently, anaplastic large cell lymphomas with T and null cell phenotypes, as well as T lymphoblastic lymphomas, have also been reported to exhibit immunoreactivity to the anti-BCL-6 antibody. We collected 33 T cell non-Hodgkin lymphomas (T-NHLs) and analyzed their expression of the BCL-6 protein by immunohistochemistry and investigated the organization of the bcl-6 gene by Southern blot and single strand conformation polymorphism (SSCP). The expression of BCL-6 was demonstrated in 37.5% of lymphoblastic (LBL), 40% of anaplastic large cell (ALCL), and 33% of peripheral T cell lymphomas (PTCL). BCL-6–positive malignant cells exhibited the CD4+ or CD4+/CD8+ phenotype. The bcl-6 gene was in a germline configuration in all T-NHLs examined, and a mutation at the first exon-intron boundary region structure of the wild-type bcl-6 gene was detected in 3 of 12 PTCL. One case of PTCL with mutations of the 5′ noncoding region expressed BCL-6. In conclusion, expression of the BCL-6 protein is demonstrable independently of bcl-6 alterations in T-NHLs. This further suggests that molecular mechanisms other than rearrangements and/or mutations of the 5′ noncoding region of the bcl-6 gene can result in expression of the protein. Whether these lymphomas arose from T cells expressing BCL-6 or expressed BCL-6 as part of the malignant transformation process needs to be determined. Finally, structural alterations of bcl-6 are rare in T-NHLs, but mutations do occur in the 5′ noncoding region. We suggest that expression of BCL-6 in T cells may facilitate lymphomagenesis by repressing critical cytokines and cell cycle regulators.
Similar content being viewed by others
Introduction
The bcl-6 proto-oncogene was originally identified in B cell non-Hodgkin's lymphomas by analysis of a translocation involving the chromosome band 3q27 (Baron et al, 1993; Deweindt et al, 1993; Kerckaert et al, 1993; Ye et al, 1993b). The translocation breakpoint occurs in the 5′ flanking region containing the promoter, the noncoding first exon and first intron of bcl-6. This results in a truncation and replacement of the 5′ regulatory region of the gene by various reciprocal chromosomal partners in a process termed promiscuous translocation (Chen et al, 1998; Wlodarska et al, 1995; Ye et al, 1993a; 1993b). In addition to the immunoglobulin locus, products of other fusion partners displayed persistent expression in later stages of B cell development, as in immunoblasts and plasma cells (Chen et al, 1998). Thus, the promoter substitution caused by this translocation might lead to constitutive production of BCL-6. By Southern blot analysis (Bastard et al, 1994; Gaidano et al, 1994; Lo Coco et al, 1994; Miki et al, 1994; Otsuki et al, 1995; Pescarmona et al, 1995), rearrangement of bcl-6 has been found in 30% to 45% of the diffuse large B cell lymphomas (DLCL), in 6% to 14% of the follicular lymphomas (FL), and in 20% of the AIDS-related diffuse large cell lymphomas. Somatic mutations also occur in the 4-kilobase (kb) 5′ noncoding region of the gene (Migliazza et al, 1995). Such mutations result in dysregulation of the gene and altered expression of the protein and may contribute to lymphomagenesis. Point mutations and/or deletions have been detected in 70% of DLCLs, in 45% of the follicular lymphomas, and in 58% of the AIDS-related lymphomas, with or without rearrangement (Gaidano et al, 1997; Migliazza et al, 1995). Therefore, bcl-6 genetic alterations (rearrangement and/or mutations) occur in virtually all DLCL and are the most frequent structural alterations in AIDS-related lymphomas identified thus far. Furthermore, bcl-6 mutations have been identified in Hodgkin's disease cell lines, suggesting the transit of these cells through the germinal center and their B cell origin (Carbone et al, 1998). Cells of posttransplantation lymphoproliferative disorders harbor bcl-6 mutations in 44% of the cases, and the presence of these mutations may help in predicting response to therapy and clinical outcome (Cesarman et al, 1998).
BCL-6 is a POZ/zinc finger protein with a transcription repressor function (Chang et al, 1996; Seyfert et al, 1996). It is capable of binding signal transducer and activator of transcription (STAT)-6 response elements and block STAT6-mediated interleukin (IL)-4 signaling (Dent et al, 1997). The BCL-6 DNA recognition motif resembles that of several STATS and could interfere with several cytokine signaling pathways. The disrupted bcl-6 gene in mouse models demonstrated that an intact protein is necessary for germinal center formation and for the T-cell–dependent antibody response. Furthermore, bcl-6 controls T-cell–mediated responses because BCL-6 deficient mice develop a Th2-type inflammatory disorder, probably as a result of abnormal production of Th2-like lymphokines (Dent et al, 1997; Ye et al, 1997).
BCL-6 is expressed at its highest level in germinal-center B lymphocytes, but not in pre-B cells or differentiated immunoblasts or plasmocytes (Allman et al, 1996; Cattoretti et al, 1995; Flenghi et al, 1995; Onizuka et al, 1995). Shaffer et al (2000) proposed that elevated expression of BCL6 in some B cells early in the antigen response may direct these cells toward a germinal center differentiation pathway and away from plasma cell differentiation. BCL-6 is also detectable in cortical thymocytes and in CD4+ germinal-center and perifollicular T cells. Among neoplastic lymphoproliferations, diffuse large B cell lymphomas, follicular lymphomas, and Burkitt's lymphomas exhibit immunoreactivity to the BCL-6 antibody, providing further evidence of their germinal-center origin (Allman et al, 1996; Cattoretti et al, 1995; Flenghi et al, 1995; Onizuka et al, 1995; Otsuki et al, 1995). Expression of the protein is independent of bcl-6 rearrangements in these tumors (Flenghi et al, 1996, 1995; Onizuka et al, 1995). Furthermore, BCL-6 production was demonstrated in nodular-lymphocyte-predominant Hodgkin's disease (Kraus and Haley, 2000) and in a small percentage of Reed-Sternberg and Hodgkin cells in classical Hodgkin's disease (Carbone et al, 1998; Falini et al, 1996).
Carbone et al (1997) reported BCL-6 production in 45% of anaplastic large cell lymphomas with T and null phenotype, suggesting that these lymphomas could arise from transformed extrafollicular CD30+ cells. More recently, Hyjek et al (2001) investigated T-lymphoblastic lymphomas for BCL6 production and organization of the gene. They did not find mutations or rearrangements of the gene, whereas production of the protein was detected in half of the cases. In this study we analyzed a large group of T cell non-Hodgkin's lymphomas to determine whether structural alterations of bcl-6 and/or production of the protein correlate with the type of T cell non-Hodgkin lymphoma (T-NHL) and the behavior of these cancers.
Results
Analysis of bcl-6 Mutations
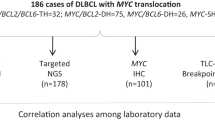
All 33 samples of T-NHLs were subjected to polymerase chain reaction–single strand conformation polymorphism (PCR-SSCP) analysis to screen for mutations in the 5′ noncoding region of bcl-6. Five overlapping primers encompassing the 1263 bp region of the first exon-intron boundary and the 5′ sequences of the first intron were used. This region has been shown to harbor mutations in B cell lymphomas with germinal-center cell origin. Three cases (9%) exhibited a shift in electrophoretic mobility when compared with the negative control and the known polymorphic variants upon SSCP analysis. Representative samples are shown in Figure 1. Mutations were detected in 3 of 12 (25%) peripheral T cell lymphomas (PTCLs) (including 1 immunoblastic T-NHL), but not in the other histological categories of T-NHLs. Mutations clustered in the 508-bp region of the first intron, corresponding to PCR fragments E 1.11 (2 cases) and E 1.12 (1 case). None of the cases exhibited multiple mutations in the regions analyzed. Wild-type bands next to the abnormally migrating bands were found in all samples, probably reflecting the lack of involvement of both alleles. Alternatively, the presence of the wild-type pattern could be attributed to the nontumoral compartment of the lymphoproliferation. Sequence analysis of the SSCP products was performed to characterize the mutations. PCR products from all three samples with an altered pattern were cloned and sequenced. The following mutations were identified: Case 20, region E1.11: G → A (499), G → A (608); Case 27, region E1.11: G → A (596), A → C (636); Case 26, region E1.12: del. G (813), A → G (82 1) (Fig. 1).
A, Giemsa-stained paraffin sections (upper row) and frozen sections stained with the BCL-6 mAb (lower row) of the three peripheral T cell lymphoma (PTCL) cases with mutations of the 5′ noncoding region of the bcl-6 gene. A few scattered and faint BCL-6+ cells are detectable in Cases 20 and 26. Case 27 expresses the BCL-6 protein. B, Single strand conformation polymorphism (SSCP, upper row) and the sequence analyses (lower row) of the DNA samples from the same cases. Arrows indicate the abnormally migrating bands caused by nucleotide substitution in these regions. ND, nondenatured DNA; DNA from normal placenta was used as a wild-type sequence negative control (NC). P, polymorphic control; the numbers above each lane correspond to the case numbers. The lower row displays representative mutations detected by sequence analyses of these cases.
Southern Blot Analysis of the bcl-6 Gene
Two probes detecting the truncation and translocation of bcl-6 in DLCLs and FLs were used to analyze the genomic organization of bcl-6 in T-NHLs. None of the samples exhibited detectable rearrangement by any of the probes hybridized to the DNA samples digested with two appropriate restriction endonucleases (data not shown).
Immunohistochemical Pattern of the T Cell Lymphomas
The phenotype of T-NHLs was determined by immunohistochemical analysis of frozen or paraffin-embedded tissue sections using antibodies to the CD1a, CD3, CD4, CD5, CD8, CD10, CD21, CD23, CD30, CD34, CD38, CD45RO, TdT, MIB1, and epithelial membrane antigens (EMA). All T-NHLs expressed CD3 antigen. A total of 23 of 29 T-NHLs exhibited immunoreactivity to the CD4 antibody and 9 of 29 to the CD8 antibody. Coexpression of CD4 and CD8 was detected in 3 of 29 cases. CD30 expression was demonstrated in 10 of 30 cases and restricted to the anaplastic large cell lymphoma (ALCL) category. Some ALCLs did express EMA. In addition, CD30 positivity was detected in individual cells in almost all samples, but those cells belonged to the reactive compartment accompanying the neoplastic proliferation. Lymphoblastic lymphomas were characterized by TdT positivity, CD1a expression, and the occurrence of double-positive (CD4/CD8) cases. Peripheral T cell lymphomas were tested for the occurrence of vessels and diffusely distributed networks of follicular dendritic cells (CD24, CD21, CD23). The distribution of the CD4, CD8, and CD30 expression among the histological subtypes is shown in Table 1.
BCL-6 Expression in T-NHLs
A fine granular nuclear staining with the monoclonal BCL-6 antibody PG-B6p was detected in 12 of 33 T-NHLs. In all positive cases, anti–BCL-6 stained the nuclei of neoplastic cells with faint-to-strong intensity. Representative cases are shown in Figures 2 and 3. A lymphoproliferation was considered positive if more than 10% of the neoplastic cells expressed BCL-6, as has been suggested previously (Carbone et al, 1997). The following frequency of BCL-6 production was observed in the different histological categories: 3 of 8 (37.5%) of lymphoblastic lymphomas (LBLs), 4 of 10 (40%) of ALCLs, 1 of 2 T-immunoblastic lymphoma (IBLs), 4 of 12 (33%) of PTCLs (including 1 of 2 T-IBLs), and 1 of 2 of angioimmunoblastic lymphoadenopathies (AILDs). The single case of mycosis fungoides (MF) included in our study could not be tested for BCL-6 expression for lack of sufficient material. The number of BCL-6–positive cells in a given T-NHL ranged from 20% to 60%, with the average of 25% to 30%. The BCL-6 positivity in the individual T cells is heterogeneous with regard to the level of protein expression. In fact, T cells expressing BCL-6 in normal lymph node and thymus samples exhibit variable staining intensities and usually display a weaker signal than germinal-center or neoplastic B cells (Fig. 3). In our hands, immunohistochemistry for BCL-6 on frozen sections gave weaker signals than paraffin sections. We used frozen sections for double-labeling immunohistochemistry. The BCL-6–positive cases were CD4+, with the exception of one CD8+, ALCL, and two LBLs coexpressing CD4 and CD8. The T cell nature of the BCL-6–expressing cells was demonstrated by a positive double immunohistochemical staining with the BCL-6 and CD3 and/or CD4 antibodies (Fig. 2.). Scattered BCL-6–positive cells of undetermined lineage, with B or T cell phenotype have also been identified in almost all cases. Coexpression of BCL-6 and CD30 was demonstrated exclusively in ALCL cases.
Frozen sections stained with the BCL-6 mAb of representative T cell non-Hodgkin lymphomas (T-NHLs) expressing the BCL-6 protein. A, Anaplastic large cell lymphoma (ALCL, Case 10); B, lymphoblastic lymphoma (LBL, Case 3). Two-color staining of a reactive lymph node (C) and a thymus specimen (D) with BCL-6 and CD4 mAbs. The intra- and interfollicular BCL-6–positive cells and certain cortical thymocytes exhibit the double staining. GC, germinal center.
Giemsa-stained LBL (A), PTCL (D), and immunoblastic lymphoma (IBL) (G) paraffin-embedded sections of representative cases of T-NHLs expressing the BCL-6 protein (original magnification, ×60). B, E, and H, Two-color staining with BCL-6 and CD4 mAbs of frozen sections (original magnification, ×40) of the same cases. Approximately 30% (B), 40% (E), and 20% (H) of the cells exhibit nuclear staining with the BCL-6 mAb. C, F, and I, The majority of the BCL-6–positive cells exhibit membrane staining with the CD4 mAb (original magnification, ×100).
Correlation between BCL-6 Expression and the bcl-6 Structural Alterations
One PTCL case expressing BCL-6 in 20% of the neoplastic T cells harbored a mutation of the 5′ noncoding region of bcl-6. Mutations were demonstrated in two additional BCL-6–negative PTCLs. Truncation of the gene in the 5′ region was not detected in any of the T-NHLs by Southern blot analyses. Therefore, there was no correlation between the molecular genetic lesions and the expression of the protein.
Discussion
BCL-6 expression was recently demonstrated in 50% of the precursor T cell lymphoblastic lymphomas studied (Hyjek et al, 2001). In addition, ALCLs (another type of T-NHL) were reported to be BCL-6–positive in 45% of the cases with T or null cell phenotype, suggesting that these lymphoproliferations might arise from the CD30+/BCL-6+ extrafollicular T lymphocytes (Carbone et al, 1997). Our report provides further evidence for this contention. However, in contrast to Carbone et al, our findings suggest that peripheral T-NHLs other than ALCL can also express BCL-6. We show BCL-6 expression in 40% of the ALCLs. In addition, 38% of LBLs, 33% of PTCLs, and one case of two AILDs also express BCL-6.
BCL-6 is expressed in a subpopulation of CD4+ inter- and intrafollicular T cells and in CD30+ interfollicular cells, besides germinal-center B lymphocytes. In addition, BCL-6 is found in the majority of cortical thymocytes, but only in a few scattered medullary thymocytes, suggesting that expression of BCL-6 may be regulated by signals operative during T cell development and differentiation. It has been suggested that the BCL-6+/CD30+ ALCL tumor cells might constitutively maintain their activated state and express BCL-6 (Carbone et al, 1997). Alternatively, a structural alteration of the gene may lead to the expression of the protein. Therefore, we subjected the DNA samples from 33 T-NHLs to SSCP and Southern blot analyses to investigate the structure of the 5′ noncoding region of the bcl-6 gene frequently altered in B cell neoplasms arising from the germinal center. Mutations and chromosomal breakpoints span a 4-kb region 5′ to the coding gene but tend to cluster in the first exon-intron boundary and the 5′ region of the first intron. No rearrangement was detected in this region in the T-NHLs analyzed, and only 3 of 33 (9%) cases exhibited somatic mutations in the 5′ noncoding region of bcl-6. The identified genetic lesions did not correlate with BCL-6 expression in these lymphomas, with one exception. Indeed, only certain translocations result in a promoter replacement and subsequent constitutive overexpression of BCL-6, as was demonstrated in B cell NHLs (B-NHLs) (Chen et al, 1998; Ye et al, 1995). Somatic mutations of the 5′ noncoding region could interfere with the function of this regulatory region of the gene and result in the overexpression of the protein. However, certain B-NHLs express the protein without any evidence of genetic lesions. Therefore, mechanisms other than truncation and/or mutation of the 5′ regulatory region of the gene could lead to dysregulated gene expression. BCL-6 expression might occur as a consequence of dysregulation of the translation process. This phenomenon is well known in certain lymphomas overexpressing BCL-1 as a result of structural alterations of its 3′ untranslated terminal region (UTR), which regulates the translation (Rimokh et al, 1994). Furthermore, nucleophosmin anaplastic lymphoma kinase (NPM-ALK) protein overexpression can be demonstrated in some ALCL cases without the detectable t(2;5) (Delsol et al, 1997).
Except for the one case of PTCL with a mutation on the 5′ noncoding region of bcl-6 with protein expression, BCL-6 protein expression in T-NHLs is not correlated with structural alterations of the gene. Rather, the tumor cells may constitutively maintain BCL-6 production because of a disturbed local cytokine network or sustained antigenic stimulation. The hypothesis of BCL-6 interfering with cytokine/chemokine networks was recently supported by the findings of Shaffer et al (2000). Using the Lymphochip microarrays, it was found that BCL-6 represses a number of genes, some of them involved in inflammation, such as IP10, a CXC chemokine known to attract activated T cells, B cells, and natural killer (NK) cells, or macrophage inflammatory protein-1α (MIP1α), known to recruit lymphocytes, monocytes, eosinophils, and mast cells (Alizadeh et al, 1999; 2000). We could speculate that malignancies might arise in cells expressing BCL-6, a protein that represses critical cytokines and regulates cell cycle progression by repressing, for instance, p27/kip1. The neoplastic phenotype could be achieved in cells escaping the regulatory influences of the cytokine network and capable of rapidly progressing through the cell cycle. Further, bcl-6 mutant mice develop preferentially Th2-type immune responses, emphasizing the capacity of BCL-6 to interfere with cytokine networks (Shaffer et al, 2000). Mutations in the 5′ noncoding region of bcl-6 are rare in T-NHLs, and the fact that two additional mutated cases exhibited no significant protein expression suggests that these structural alterations are probably not linked to the relatively high percentage of BCL-6 expression in T-NHLs. These mutations should be considered as part of the accumulating genetic alterations occurring during neoplastic transformation and reflecting the genetic instability of these cells.
Alternatively, the somatic mutation machinery that sometimes targets the T cell receptor gene in germinal center T cells (Zheng et al, 1994) might also target the bcl-6 during T cell maturation. In this context, the precursor lymphoma cells would already harbor the mutation, and one could argue that rare PTCLs may arise from germinal center T cells.
The role of BCL-6 during the T cell differentiation is not fully understood. CD4-positive inter- and intrafollicular T cells with strong nuclear immunoreactivity to the BCL-6 antibody are readily detectable in tonsil and lymph node specimens (Fig. 2). Nonspecific stimulation (phorbol esters) or antigenic stimulus can increase the number of these BCL-6–positive T cells, suggesting that the activation would be accompanied by the expression of the protein (Falini et al, 1996). The accumulation of BCL-6+/CD4+ reactive T cells around the lymphocytic and/or histiocytic (L&H) cells in the neoplastic nodules of nodular lymphocyte-predominant Hodgkin's disease has been observed. This suggests the possible induction of BCL-6 by locally released cytokines from the tumor cells (Falini et al, 1996). Interestingly, the neoplastic T cells expressed BCL-6 in 33% of the PTCLs in our study. This suggests that a subgroup of the PTCLs might arise from the CD4+/BCL-6+ intra- or interfollicular T cells.
Furthermore, certain cortical thymocytes also exhibit immunoreactivity to the BCL-6 antibody. In 37.5% of the LBLs, expression of the BCL-6 protein was detected in 20% to 30% of the neoplastic cell population. Two additional cases showed small numbers of BCL-6–positive cells (<10%). Indeed, BCL-6 staining of a thymus specimen demonstrates two populations of T cells, one strongly expressing the protein in the nuclei and another predominant cell population with a lower level of expression. Most BCL-6+ cells are CD3+ and, to a lesser extent, CD4+, whereas others show undetermined phenotypes (Fig. 2). Hyjek et al (2001) have clearly demonstrated with elegant tri-color immunohistochemistry that these are double-positive cortical thymocytes strongly expressing BCL-6 in a majority of cells and medullary single-positive thymocytes only occasionally expressing BCL-6. Therefore, it can be hypothesized that some of the tumor cells in LBLs arose in the BCL-6–positive compartment of the thymus. This could explain the well-known phenomenon of immunophenotypic heterogeneity of T cell LBLs. Certain LBLs display neoplastic cells with variable T cell differentiation-associated antigen expression, probably reflecting the presence of multiple neoplastic subpopulations at different stages of T cell development (Knowles, 2001). It is conceivable that certain LBLs include a significant number of neoplastic cells maintaining BCL-6 expression. It has been recently proposed that T-LBLs may arise through clonal expansion of cortical thymocytes normally expressing BCL-6 (Hyjek et al, 2001). In addition, these authors stressed that T-LBLs coexpress the antiapoptotic proteins BCL-2 and BCL-X, which could provide a growth advantage for the lymphoma cells, as in follicular lymphomas. The role of the BCL-6 protein expression in the developing T cells, before any antigenic stimulus, remains to be elucidated.
The conclusion of our study is that BCL-6 expression is detectable in a large proportion of T-NHLs. In addition to ALCLs and T-LBLs, BCL-6–positive lymphoma cells were identified in a subgroup of PTCLs as well. The protein expression in T cell lymphomas usually occurs independently of the truncation and/or somatic mutations of the 5′ noncoding region of the gene. Overall, these genetic alterations, found frequently in B cell neoplasms with germinal-center cell origin, are rare in T-NHLs, accounting for 9% of the cases. Interestingly, the somatic mutations detected here fall into the PTCL histological category, involving 25% of these cases. Our data suggest that the BCL-6 expression in T-NHLs is rather the result of the maintained protein production and probably reflects the activation status of the lymphoma cells and the percentage of the activated T cells before the neoplastic transformation. Our study also provides further suggestions that the BCL-6 protein may be involved in the T cell differentiation process and in T cell lymphomagenesis via repression of both inflammatory and cell cycle control genes. This may especially hold true for PTLDs. Moreover, the regulation of bcl-6 transcription is most likely a complex mechanism, and factors other than the mutation of the 5′ noncoding regulatory region of the gene determine this function.
Materials and Methods
Pathologic Samples
Thirty-three malignant T cell neoplasms were included in this study. Primary samples were derived from lymph nodes (23), skin (5), nasal mucosa (2), bone marrow (1), testicle (1), and soft tissue (1) biopsies. Diagnoses were based on correlative histopathologic, immunophenotypic, and, if necessary, immunogenotypic analyses, such as T cell receptor (TCR) and immunoglobulin H (IgH) rearrangement studies via Southern blot or PCR, and classified according to the Revised European American Lymphoma (REAL) classification of malignant lymphomas (Harris et al, 1994). The diagnoses revealed 8 cases of LBL, 10 cases of ALCL, 12 cases of PTCL, including 2 T-immunoblastic lymphomas (IBs), 2 cases of AILD, and one mycosis fungoides (MF) (Table 1). All T-NHL subjected to immunogenotypic analyses showed clonal TCR rearrangements, except for one case of AILD, which was polyclonal. Several nonneoplastic lymphoid tissue samples (T-zone hyperplasias) were also included in the study as controls.
Immunophenotypic Analysis
The immunophenotypic profile of the samples was determined by immunoperoxidase staining of frozen and/or paraffin-embedded tissue sections. The number and type of antibodies used in each case depended on the antibody panel needed to confirm the diagnosis. These included essentially CD3, CD4, CD8, CD45RO, CD15, CD20, CD79, CD30 (DAKO, Glostrup, Denmark). In adequate cases, CD1a, CD5, CD7, CD10, CD21, CD23, CD34, CD38, BCL-2, EMA, and MIB1 (Ki 67) TdT were added to the panel. Cases were assigned to T cell immunophenotype if positive staining was obtained with either CD45RO or CD3 antibodies without B cell markers. In individual cases, the T cell nature of the lymphoma was verified by TCR rearrangement. BCL-6 immunostaining was performed on frozen or paraffin-embedded tissue sections using a monoclonal anti–BCL-6 antibody (PG-B6p). For BCL-6 double staining, 4-μm-thick frozen sections were fixed in formalin (2 hours, room temperature). Antigen retrieval was achieved by pressure cooking at maximal pressure in 10 mm citrate buffer (pH 6.0). Sections were incubated with BCL-6 antibody, and immunoreaction was detected using the streptavidin-horseradish peroxidase detection system (DAKO). For the respective second antibody, the same sections were incubated with antibody followed by a streptavidin-alkaline phosphatase detection system (DAKO). (Flenghi et al, 1995; 1996). Double-staining with CD3, CD4, and BCL-6 and with CD30 and BCL-6 was performed to demonstrate the T cell nature of the BCL-6–positive cells in T cell NHLs.
DNA Extraction and Southern Blot Analysis
Genomic DNA was extracted from frozen tissue sections after proteinase K digestion using a “salting out” procedure not requiring an organic extraction (Miller et al, 1988). DNA samples were then subjected to Southern blot and SSCP analyses. The organization of the BCL-6 locus was analyzed by hybridization of BamHI and XbaI digested DNA to the human bcl-6 probe Sac4.0 and/or Sac0.8 detecting the cluster of bcl-6 rearrangements in B cell NHLs (Gaidano et al, 1994; Lo Coco et al, 1994). A total of 6 μg genomic DNA was digested with the appropriate restriction endonucleases, electrophoresed on a 0.8% agarose gel, denatured in alkali, neutralized, and transferred to Hybond C+ filters and hybridized to probes that had been P32-labeled by the random priming extension method (Prime-It, Stratagene, La Jolla, California). Filters were washed in 0.1 × SDS and 0.2 × SSC (NaCl/NaCitrate) for 2 hours at 60° C. Autoradiography was performed at −80° C for 24 to 72 hours.
Oligonucleotides
All the oligonucleotides used for the SSCP analyses in this study were synthesized by the solid-phase triester method. The sequences of oligonucleotides corresponding to BCL-6 first intron region (fragments E1.9, E1.10, E1.11, E1.12 and E1.13) used in this study were as follows:
E1.19 5′GGGTTCTTAGAAGTGGTG3′,
E1.20 5′CAAAGCATTTGGCAAGAG3′,
E1.21 5′CTCTTGCCAAATGCTTTG3′,
E1.24 5′TAATTCCCCTCCTTCCTC3′,
E1.23 5′AGGAAGGAGGGGAATTAG3′,
IP1.6 5′AAGCAGTTTGCAAGCCAG3′,
IP1 1. 5′TTCTCGCTTGCAAACTGC3′,
E1.26 5′CACGATACTTCATCTCATC3′,
E1.25 5-GATGAGATGAAGTATCGTG3′,
IP2.B 5′ACACTGAAAGGCATCGCA3′, as have been reported previously (Migliazza et al, 1995).
PCR and SSCP
Briefly, 500 ng of genomic DNA, 10 pMol of each primer, 25 μmol/l dNTPs, 1 μCi of (α-P32) dCTP, and 0.1 U AmpliTaq Polymerase (Perkin-Elmer, Branchburg, New Jersey) were mixed in a final volume of 20 μl. Thirty cycles of denaturation (94° C), annealing (temperatures were optimized for each pair of primers: 54° C for E1.12, 56° C for E1.10 and E1.13, 58° C for E1.11, and 60° C for E1. 9), and extension (72° C) were performed in a temperature controller (DNA Thermal Cycler, Perkin-Elmer). Samples were heated at 95° C for 5 minutes, chilled on ice, and immediately loaded onto a 6% acrylamide-TRIS-borate gel containing 10% glycerol. Gels were run at 8 W for 16 hours at room temperature, vacuum dried, and analyzed by autoradiography.
DNA Sequencing Procedures
PCR products were subcloned into the pGEM-T vector (pGem-T Easy Vector System II; Promega Corporation, Madison, Wisconsin). Four independent clones were sequenced by using the T7 Sequenase, version 2.0, DNA sequencing kit (Amersham Life Science, Inc., Cleveland, Ohio) with universal primers and following the manufacturer's instructions.
References
Alizadeh A, Eisen M, Davis RE, Ma C, Sabet H, Tran T, Powell JI, Yang L, Marti GE, Moore DT, Hudson JR Jr, Chan WC, Greiner T, Weisenburger D, Armitage JO, Lossos I, Levy R, Botstein D, Brown PO, and Staudt LM (1999). The lymphochip: A specialized cDNA microarray for the genomic-scale analysis of gene expression in normal and malignant lymphocytes. Cold Spring Harb Symp Quant Biol 64: 71–78.
Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, Boldrick JC, Sabet H, Tran T, Yu X, Powell JI, Yang L, Marti GE, Moore T, Hudson J Jr, Lu L, Lewis DB, Tibshirani R, Sherlock G, Chan WC, Greiner TC, Weisenburger DD, Armitage JO, Warnke R, and Staudt LM (2000). Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature 403: 503–511.
Allman D, Jain A, Dent A, Maile RR, Selvaggi T, Kehry MR, and Staudt LM (1996). BCL-6 expression during B-cell activation. Blood 87: 5257–5268.
Baron B, Nucifora G, McCabe N, Espinosa R, LeBeau MM, and McKeithan TN (1993). Identification of the gene associated with the recurring chromosomal translocations t(3;14)(q27;q32) and t(3;22)(q27;11) in B cell lymphomas. Proc Natl Acad Sci USA 90: 5262–5266.
Bastard C, Deweindt C, and Kerekaert J (1994). LAZ3 rearrangements in non- Hodgkin's lymphoma: Correlation with histology, immunophenotype, karyotype, and clinical outcome in 217 patients. Blood 83: 2423–2427.
Carbone A, Gloghini A, Gaidano G, Dalla-Favera R, and Falini B (1997). Bcl- 6 protein expression in human peripheral T-cell neoplasms is restricted to CD30 positive anaplastic large cell lymphomas. Blood 90: 2445–2450.
Carbone A, Gloghini A, Gaidano G, Franceschi S, Capello D, Drexler HG, Falini B, and Dalla-Favera R (1998). Expression status of BCL-6 and syndecan-1 identifies distinct histogenetic subtypes of Hodgkin's disease. Blood 92: 2220–2228.
Cattoretti G, Chang CC, Cechova K, Zhang J, Ye BH, Falini B, Louie DC, Offit K, Chaganti RS, and Dalla-Favera R (1995). BCL-6 protein is expressed in germinal-center B cells. Blood 86: 45–53.
Cesarman E, Chadburn A, Liu YF, Migliazza A, Dalla-Favera R, and Knowles D (1998). Bcl-6 gene mutations in post-transplantation lymphoproliferative disorders (PT-LPDs) predict response to therapy and clinical outcome. Blood 92: 2294–2302.
Chang CC, Ye BH, Chaganti RS, and Dalla-Favera R (1996). BCL-6, a POZ/zinc-finger protein, is a sequence-specific transcriptional repressor. Proc Natl Acad Sci USA 93: 6947–6952.
Chen W, Lida S, Louie D, Dalla-Favera R, and Chaganti R (1998). Heterologous promoters fused to Bcl-6 gene by chromosomal translocation affecting band 3q27 cause its deregulated expression during B-cell differentiation. Blood 91: 603–607.
Delsol G, Lamant L, Mariame B, Pulford K, Dastugue N, Brousset P, Rigal-Huguet F, al Saati T, Cerretti DP, Morris SW, and Mason DY (1997). A newsubtype of large B-cell lymphoma expressing the ALK kinase and lacking the 2;5 translocation. Blood 89: 1483–1490.
Dent A, Shaffer A, Yu X, Allman D, and Staudt L (1997). Control of inflammation, cytokine expression, and germinal center cell formation by BCL-6. Science 276: 589–592.
Deweindt C, Kerckaert J, Tilly H, Quief S, Nguyen V, and Bastard C (1993). Cloning of a breakpoint cluster region at band 3q27 involved in human non Hodgkin's lymphoma. Gene Chromosomes Cancer 8: 149–154.
Falini B, Bigerna B, Pasqualucci L, Fizzotti M, Martelli MF, Pileri S, Pinto A, Carbone A, Venturi S, Pacini R, Cattoretti G, Pescarmona E, Lo Coco F, Pelicci PG, Anagnastopoulos I, Dalla-Favera R, and Flenghi L (1996). Distinctive expression pattern of the BCL-6 protein in nodular lymphocyte predominance Hodgkin's disease. Blood 87: 465–471.
Flenghi L, Bigerna B, Fizzotti M, Venturi S, Pasqualucci L, Pileri S, Ye BH, Gambacorta M, Pacini R, Baroni CD, Pescarmona E, Anagnostopoulos I, Stein H, Asdrubali G, Martelli MF, Pelicci PG, Dalla-Favera R, and Falini B (1996). Monoclonal antibodies PG-B6a and PG-B6p recognize, respectively, a highly conserved and a formol-resistant epitope on the human BCL-6 protein amino-terminal region. Am J Pathol 148: 1543–1555.
Flenghi L, Ye BH, Fizzotti M, Bigerna B, Cattoretti G, Venturi S, Pacini R, Pileri S, Lo Coco F, and Pescarmona E (1995). A specific monoclonal antibody (PG-B6) detects expression of the BCL-6 protein in germinal center B cells. Am J Pathol 147: 405–411.
Gaidano G, Carbone A, Pastore C, Capello D, Migliazza A, Gloghini A, Roncella S, Ferrarini M, Saglio G, and Dalla-Favera R (1997). Frequent mutation of the 5′ noncoding region of the BCL-6 gene in acquired immunodeficiency sydrome-related non-Hodgkin's lymphomas. Blood 89: 3755–3762.
Gaidano G, Lo Coco F, Ye BH, Shibata D, Levine A, Knowles DM, and Dalla-Favera R (1994). Rearrangements of the BCL-6 gene in acquired immunodeficiency syndrome-associated non-Hodgkin's lymphoma: Association with diffuse large-cell subtype. Blood 15: 397–402.
Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, Delsol G, De Wolf-Peeters C, Falini B, Gatter KC, Grogan TM, Isaacson PG, Knowles DM, Mason DY, Muller-Hermelink HK, Pileri SA, Piris MA, Ralfkiaer E, and Warnke RA (1994). A revised European-American classification of lymphoid neoplasms: A proposal from the International Lymphoma Study Group. Blood 84: 1361–1392.
Hyjek E, Chadburn A, Liu Y-F, Cesarman E, and Knowles DM (2001). BCL- 6 protein is expressed is expressed in precursor T-cell lymphoblastic lymphoma and in prenatal thymus. Blood 97: 270–276.
Kerckaert J, Deweindt C, Tilly H, Quief S, Lecocq G, and Bastard C (1993). LAZ3, a novel zinc finger encoding gene is disrupted by recurring chromosome 3q27 translocations in human lymphoma. Nat Genet 5: 66–70.
Knowles DM (2001). Neoplastic hematopathology. Philadelphia: Lippincott, Williams and Wilkins, 915–951.
Kraus MD and Haley J (2000). Lymphocyte predominance disease: The use of cl-6 and CD57 in diagnosis and differential diagnosis. Am J Surg Pathol 24: 1068–1078.
Lo Coco F, Ye BH, Lista F, Corradini P, Offit K, Knowles DM, Chaganti RS, and Dalla-Favera R (1994). Rearrangements of the bcl-6 gene in diffuse large cell non-Hodgkin's lymphoma. Blood 83: 1757–1759.
Migliazza A, Martinotti S, Chen W, Fusco C, Ye BH, Knowles DM, Offit K, Chaganti RS, and Dalla-Favera R (1995). Frequent somatic hypermutation of the 5′ non-coding region of the BCL-6 gene in B-cell lymphoma. Proc Natl Acad Sci USA 92: 12520–12524.
Miki T, Karwanata N, Hirwosawa S, and Aoki N (1994). Gene involved in the 3q27 translocation associated with B-cell lymphoma Bcl-6, encodes a Krüppel- like zinc finger protein. Blood 83: 26–32.
Miller SA, Dykes DD, and Polesky HF (1988). A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16: 1215.
Onizuka T, Moriyama M, Yamochi T, Kuroda T, Kazama A, Kanazawa N, Sato K, Kato T, Ota H, and Mori S (1995). BCL-6 gene product, a 92- to 98kD nuclear phosphoprotein, is highly expressed in germinal center B cells and their neoplastic counterparts. Blood 86: 28–37.
Otsuki T, Yano T, Clark H, Bastard C, Kerkaert JP, Jaffe ES, and Raffeld M (1995). Analysis of LAZ3 (Bcl-6) status in B-cell non-Hodgkin's lymphoma: Results of rearrangement and gene expression studies and a mutational analysis of coding region sequences. Blood 85: 2877–2884.
Pescarmona E, Lo Coco F, Pacchiarotti A, Rapanotti MC, Cimino G, Di Paolo B, and Baroni CD (1995). Analysis of the BCL-6 gene configuration in diffuse B-cell non-Hodgkin's lymphomas and Hodgkin's disease. J Pathol 177: 21–25.
Rimokh R, Berger F, Bastard C, Klein B, French M, Archimbaud E, Rouault JP, Santa Lucia B, Duret L, Vuillaume M, Coiffier B, Bryon PA, and Magaud JP (1994). Rearrangement of CCND1 (BCL1/PRAD1) 3′ untranslated region in mantle-cell lymphomas and t(11q13)-associated leukemias. Blood 83: 3689–3696.
Seyfert VL, Allman D, He YS, and Staudt LM (1996). Transcriptional repression by the proto-oncogene BCL-6. Oncogene 12: 2331–2342.
Shaffer AL, Yu X, He Y, Boldrick J, Chan EP, and Staudt LM (2000). BCL- 6 represses genes that function in lymphocyte differentiation, inflammation, and cell cycle control. Immunity 13: 199–212.
Wlodarska I, Mecucci C, Stul M, Michaux L, Pittaluga S, Hernandez JM, Cassiman JJ, De Wolf-Peeters C, and Van den Berghe H (1995). Fluorescence in situ hybridization identifies new chromosomal changes involving 3q27 in non-Hodgkin's lymphomas with BCL-6/LAZ3 rearrangement. Genes Chromosomes Cancer 14: 1–7.
Ye BH, Cattoretti G, Shen Q, Zhang J, Hawe N, de Waard R, Leung C, Nouri-Shirazi M, Orazi A, Chaganti RS, Rothman P, Stall AM, Pandolfi PP, and Dalla-Favera R (1997). The BCL-6 proto-oncogene controls germinal center formation and Th2-type inflammation. Nat Genet 16: 161–170.
Ye BH, Chaganti S, Chang CC, Niu H, Corradini P, Chaganti RS, and Dalla-Favera R (1995). Chromosomal translocations cause deregulated Bcl-6 expression by promoter substitution in B-cell lymphoma. EMBO J 14: 6209–6217.
Ye BH, Lista F, Lo Coco F, Knowles DM, Offit K, Chaganti RS, and Dalla-Favera R (1993a). Alterations of a zinc finger-encoding gene, BCL-6, in diffuse large-cell lymphoma. Science 262: 747–750.
Ye BH, Rao PH, Chaganti RS, and Dalla-Favera R (1993b). Cloning of bcl- 6, the locus involved in chromosome translocations affecting band 3q27 in B-cell lymphoma. Cancer Res 53: 2732–2735.
Zheng B, Xue W, and Kelsoe G (1994). Locus-specific somatic hypermutation in germinal centre T cells. Nature 372: 556–559.
Acknowledgements
Supported in part by the Swiss National Science Foundation Grant No. 31.49681.96 to BB.
We are indebted to Dr. Brunangelo Falini, University of Perugia, Italy, for providing the BCL-6 antibody and to the Institute of Pathology, University of Berne, Switzerland, for providing the paraffin blocks. We thank Dr. Daniel Hoessli for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kerl, K., Vonlanthen, R., Nagy, M. et al. Alterations on the 5′ Noncoding Region of the BCL-6 Gene Are Not Correlated with BCL-6 Protein Expression in T Cell Non-Hodgkin Lymphomas. Lab Invest 81, 1693–1702 (2001). https://doi.org/10.1038/labinvest.3780382
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3780382
This article is cited by
-
Aberrant expression of Fra-2 promotes CCR4 expression and cell proliferation in adult T-cell leukemia
Oncogene (2008)
-
Rare expression of BSAP (PAX-5) in mature T-cell lymphomas
Modern Pathology (2007)
-
Peripheral T-cell lymphoma with involvement of the expanded mantle zone
Virchows Archiv (2006)
-
Follicle center lymphoma is associated with significantly elevated levels of BCL-6 expression among lymphoma subtypes, independent of chromosome 3q27 rearrangements
Leukemia (2002)