Abstract
Study design:
Case report.
Setting:
Department of Neurosurgery, Sapporo Azabu Neurosurgical Hospital and Department of Neurosurgery, Hokkaido University Graduate School of Medicine, Sapporo, Japan.
Case report:
A patient presented to us with complete C4 tetraplegia after a 3-m fall. MRI performed 120 min after his fall showed spinal canal stenosis due to disk protrusion at the C3/4 level without spinal cord signal changes on T1- and T2-weighted images. He underwent laminoplasty between C2 and C6. Intraoperative ultrasound, performed 6 h after his fall, disclosed a hyperechoic lesion at the C3/4 level of the cervical cord; postoperative T2-weighted MRI, obtained at 8 h after his fall, showed high intensity at the same level.
Conclusion:
In patients with cerebral infarction, approximately 6 h between the insult and the acquisition of T2-weighted MRI are required to detect signal changes. We postulate that the time course on MRI scans obtained immediately after spinal cord injury is similar in patients with spinal cord injury and cerebral infarction and suggest that the absence of spinal cord abnormalities in the ultra-early post-injury stage is not always predictive of a good prognosis.
Similar content being viewed by others
Introduction
On MRI scans obtained within 48 h post-injury, spinal cord injury is observed as an isointense area compared to the normal spinal cord on T1- and as high intensity on T2-weighted images. MRI changes occur over time,1 however, little is known about the time course in the ultra-acute phase. We report a patient who sustained cervical cord injury upon taking a 3-m fall; although on admission he manifested tetraparesis, MRI detected no abnormalities. On intraoperative ultrasound images and postoperative MRI scans, there was evidence of definite changes in the cervical cord.
Case report
This 73-year-old man with a diagnosis of cervical ossification of the posterior longitudinal ligament (OPLL) had undergone anterior decompression and fixation between C4 and C7 for OPLL in 1999. In January 2006, he sustained a fall from a 3-m-high roof and arrived at our hospital within 60 min of the accident. At admission, he was hypotensive and in respiratory distress; he manifested complete tetraparesis with complete loss of sensation below the level of C4 and loss of anal reflex.
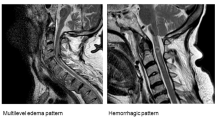
The first MRI scan was obtained 120 min after his fall. Although the spinal cord was compressed by a protruded disk at the C3/4 level, on T1- and T2-weighted images, there was no intramedullary signal change (Figure 1). No swelling, soft-tissue hemorrhage, or cervical fracture was recognized.
Although his symptoms were suggestive of complete spinal cord injury, we performed emergency surgical decompression considering his symptoms reversible because MRI identified no intramedullary lesions. Surgical decompression was achieved by laminoplasty through C2–C6. Intraoperative ultrasonography, performed 6 h after the fall, showed adequate amounts of the anterior and posterior subarachnoid space and spinal cord pulsation. These findings were suggestive of good decompression despite the protruded C3/4 disk. An intramedullary hyperechoic lesion was detected at the C3/4 level of the cord (Figure 2). On a postoperative MRI scan, acquired 8 h after the fall, an intramedullary high T2 signal lesion was recognized (Figure 3a). The spinal cord appeared normal on T1-weighted MRI (Figure 3b).
On MRI obtained 3 days after his fall, there was extension of the high T2 signal area upward and downward from the high-intensity lesion seen on postoperative T2-weighted images (Figure 4a); T1-weighted images showed isointensity edema (Figure 4b). Follow-up images were acquired 3 weeks and 3 months after the accident. They showed that the high-intensity area seen on the earlier T2-weighted images had gradually become more pronounced; a circumscribed compact lesion at the C3/4 level of the spinal cord was also noted (Figure 4c, e). Simultaneously, on T1-weighted images, the lesion manifested low intensity compared to the normal-appearing spinal cord, a finding indicative of softening of spinal cord (Figure 4d, f). Although his motor function and sensation had improved, his ASIA/IMSOP scale2 was C.
Time course of the injured spinal cord. (a, c, e) T2-weighted images; (b, d, f) T1-weighted images. (a, b) were obtained on the 3rd day, (c, d) at 3 weeks, and (e, f) at 3 months after the fall. The area of high intensity, indicating edema, on the T2-weighted image spread upward and downward along the spinal cord (a, c). Subsequently, the lesion changed into a compact, strong high-intensity area (e). Note that the isointensity edema observed at 3 days and 3 weeks (b, d) became a low-intensity lesion at the C3/4 level (f)
Discussion
The histopathology of traumatic spinal cord injury changes over time.3, 4 Just after the injury, the main event is microhemorrhage primarily in the gray matter with gradual enlargement and conglutination. The intramedullary lesion progresses to hemorrhagic necrosis, and edema and hemorrhage spreads to the white matter in the course of a period ranging from a few to 24 h post-injury. This change accounts for the primary damage elicited by direct trauma and the subsequent secondary injury. In the subacute phase, 2–3 weeks after the trauma, copious macrophages and new blood vessels are seen in the necrotic spinal cord tissue. In the chronic phase, a few months after the injury, cavity formation and gliosis occur at the damaged area. MRI findings of spinal cord injury gradually change with the time course of histopathological changes and depend on the degree of injury. Yuge et al1 reported that within 48 h, patients with severe spinal cord injury manifest T2 high-intensity lesions and those with hemorrhage show T2 low-intensity lesions with reference to the normal spinal cord. During the same period, isointensity compared to the normal spinal cord can be seen on T1-weighted images. The high-intensity area indicative of edema on T2-weighted images subsequently increases and the isointensity on T1-weighted images changes to mild hypointensity; in some cases, it is seen as a high-intensity area at 2 weeks post-injury. Subsequently, the lesion gradually becomes a smaller and more compact high-intensity area; traces of hemorrhage are of low intensity with reference to the normal spinal cord on T2-weighted images. Simultaneously, the lesion acquires low intensity compared to the normal spinal cord on T1-weighted images due to softening of the spinal cord.
By contrast, in patients with mild spinal cord injury who ultimately improve to the level of ASIA/IMSOP scale D or E between 48 h and 2 weeks post-injury, the lesion manifests as high intensity and then gradually shrinks. Within the first month post-injury, there is no signal change on T1-weighted images. Ueta5 reported that individuals with spinal cord concussion did not manifest abnormal T1- and T2-weighted MRI findings.
MRI findings are important because they help to assess the prognosis of patients with spinal cord injury. Spinal cord injury patients tend to have a poor prognosis if they manifest an intramedullary low-intensity signal on T2-weighted MRI obtained about 48 h post-injury, low intensity signals on T1-weighted images acquired after about 2 weeks, and a low-intensity lesion on T1-weighted images of axial cord sections obtained approximately 3 months post-injury. On the other hand, a good prognosis can be expected in patients with no signal change on either T2-weighted MRI acquired within 48 h or on T1-weighted images obtained 3 months post-injury.
There are few reports concerning the time course in the ultra-early stage, within 48 h, of severe spinal cord injury. Our search of the literature found only one report of a severe injury case; in this patient, there were no MRI findings at admission, although follow-up MRI study disclosed changes.5
T2-weighted images acquired 2 h post-injury in our patient showed no signal changes, although intraoperative ultrasonography performed at 6 h after his fall disclosed a slight hyperechoic lesion in the spinal cord; it was thought to be reflective of edema. On the postoperative T2-weighted image obtained 8 h post-injury, we noted high intensity at the C3/4 level of the spinal cord.
T2-weighted images acquired in the ultra-early stage of cerebral infarction may not show signal changes. Conventional MRI scans demonstrate changes that reflect an increase in the water content of tissue. For changes to be detectable on T2-weighted images, several hours may be required for the accumulation of a sufficient amount of tissue water at the stroke site.6 According to Mohr et al,7 in about half of their patients with infarction, this period was 4–6 h.
The intracellular velocity of water molecules decreases due to the cytotoxic edema that immediately follows an ischemic insult. As diffusion-weighted MRI (DWI) reflects this decrease, it can detect ischemic lesions earlier than conventional imaging sequences. In animal models, DWI routinely detects brain ischemic lesions within 30 min of the insult8 and studies on selected cases demonstrated that DWI may similarly detect ischemic lesions in humans with cerebral infarction.9, 10 Therefore, DWI is now widely used for the diagnosis of acute ischemic stroke. According to Gonzalez et al,6 the accuracy of DWI for diagnosing stroke within 6 h is high and its sensitivity and specificity are 100%.
On the other hand, DWI is not routinely used for diagnosing spinal cord pathology because of the small size of the neural tissue, its low spatial resolution, its susceptibility to magnetic artifacts introduced by surrounding bone and air, and the presence of nearby vascular and cerebrospinal fluid pulsation.11 However, Shen et al,12 who reported a patient with spinal cord injury who manifested no radiological abnormality, found that DWI but not T1- and T2-weighted MRI disclosed spinal cord signal changes.
Our patient underwent emergency surgical decompression based on negative findings on T2-weighted MRI acquired at admission. However, intraoperative ultrasonography disclosed an intramedullary hyperechoic lesion. Although we cannot rule out that the decompression procedure promoted tissue edema, we postulate that the initial negative spinal cord MRI findings were attributable not only to existing compression but also to the short interval between the injury and the MRI examination.
Our findings indicate that, as in cases with cerebral infarction, a lapse of several hours may be required to detect changes on T2-weighted MRI in patients whose spinal cord injury is not accompanied by spinal fracture or dislocation. On the other hand, DWI study performed at admission can be expected to demonstrate changes in patients with spinal cord injury, because this technique does not require an interval between the injury and the acquisition of imaging data.
We were unable to find published ultrasonographic documentation of intramedullary changes in patients with traumatic spinal cord injury. In brain tumor patients, perifocal edema is seen as a slight hyperechoic lesion.13 As edema is a common finding in patients with brain tumors and spinal cord injury, we postulate that it also presents as a hyperechoic lesion. In our patient the lesion was faint, that is hyperechoic, although not strongly so, homogeneous and the margin was not clear, and on postoperative MRI, there was no evidence of bleeding. The description ‘heterogeneous hyperechoic lesion’ may be applicable in patients with spinal cord injury who manifest intramedullary hemorrhage because hematoma is seen as a hyperechoic lesion.14
Conclusion
We presented a patient with spinal cord injury whose first MRI showed no signal change in the spinal cord despite the severity of his symptoms. Follow-up MRI showed a high T2 intensity lesion in the spinal cord. Based on our experience with this case, we postulate that the absence of spinal cord abnormalities in the ultra-early post-injury stage is not always predictive of a good prognosis.
References
Yuge I, Shiba K, Ueta T, Ohta H, Mori E, Takemitsu Y . MRI of cervical cord injuries (in Japanese). Sekitsui Sekizui 1997; 10: 423–431.
Maynard Jr FM et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Koyamagi I . Spine and spinal cord injury (in Japanese). In: Iwasaki Y and Hida K (eds). The Basic Textbook of Spinal Surgery. Miwa shoten: Tokyo 2006, pp 248–266.
Tator CH, Koyanagi I . Vascular mechanisms in the pathophysiology of human spinal cord injury. J Neurosurg 1997; 86: 483–492.
Ueta T . MRI of spine and spinal cord injuries (in Japanese). MB Orthopaed 1994; 7 (11 Suppl): 59–74.
Gonzalez RG et al. Diffusion-weighted MR imaging: diagnostic accuracy in patients imaged within 6 hours of stroke symptom onset. Radiology 1999; 210: 155–162.
Mohr JP et al. Magnetic resonance versus computed tomographic imaging in acute stroke. Stroke 1995; 26: 807–812.
Minematsu K et al. Effects of a novel NMDA antagonist on experimental stroke rapidly and quantitatively assessed by diffusion-weighted MRI. Neurology 1993; 43: 397–403.
Warach S, Chien D, Li W, Ronthal M, Edelman RR . Fast magnetic resonance diffusion-weighted image of acute human stroke. Neurology 1992; 42: 1717–1723.
Sorensen AG et al. Hyperacute stroke: evaluation with combined multisection diffusion-weighted and hemodynamically weighted echo-planar MR imaging. Radiology 1996; 199: 391–401.
Shinoyama M, Takahashi T, Shimizu H, Tominaga T, Suzuki M . Spinal cord infarction demonstrated by diffusion-weighted magnetic resonance imaging. J Clin Neurosci 2005; 12: 466–468.
Shen H et al. Applications of diffusion-weighted MRI in thoracic spinal cord injury without radiographic abnormality. Int Orthop 2006; 12 (E-pub ahead of print).
van Velthoven V . Intraoperative ultrasound imaging: comparison of pathomorphological findings in US versus CT, MRI and intraoperative findings. Acta Neurochir 2002; 85 (Suppl): 95–99.
Aoyama T, Terasaka S, Kashiwazaki D, Ushikoshi S, Nunomura M . Usefulness of intraoperative ultrasound in neurosurgery (in Japanese). Neurosonology 2005; 18: 63–68.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Aoyama, T., Hida, K., Akino, M. et al. Ultra-early MRI showing no abnormality in a fall victim presenting with tetraparesis. Spinal Cord 45, 695–699 (2007). https://doi.org/10.1038/sj.sc.3102014
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102014