Abstract
Study design:
Experimental, controlled trial.
Objectives:
The purpose of this study was to evaluate over a 15-day period alterations in sleep pattern of rats after spinal cord injury (SCI).
Setting:
Federal University of São Paulo, Department of Psychobiology.
Methods:
In total, 20 male Wistar rats were used. The rats were divided in two groups: SHAM and SCI. The rats were submitted to the following procedures: electrode insertion surgery, 24 h duration baseline sleep recording, SCI (level T9) and subsequent sleep recording for 15 consecutive days.
Results:
The results showed a reduction in sleep efficiency in the light period for Days 1–3, 5, 10 and 12 after SCI in relation to the SHAM group, with alterations in total waking time and sleep stages. Limb movements were observed 4 days after SCI.
Conclusion:
The present findings suggest that SCI may be heavily involved in altering sleep pattern in SCI subjects and that the inactivity caused by SCI may be exacerbating this altered sleep pattern.
Sponsorship:
Associação Fundo de Incentivo à Psicofarmacologia (AFIP), FAPESP (03/06297–3, and CEPID 98/143033) and CNPQ.
Similar content being viewed by others
Introduction
Few studies have characterized sleep quality in spinal cord injury (SCI) individuals. Physiological and psychological alterations caused by SCI may lead to changes related to sleep patterns.
Animal-model studies have helped develop research to provide better explanations of sleep pattern in the different situations affecting its physiology – these influences may be due to external or internal causes.
Therefore, studies have been conducted to analyze a number of factors that intervene in sleep in an attempt to study and explain the physiopathology of different diseases. Andersen et al1 examined sleep patterns in a peripheral neuropathy model induced by constricting the sciatic nerve and showed that sciatic nerve constriction induced poor sleep quality with disrupted sleep in rats, particularly during the first week of this condition.
Previous study reported that after SCI, rats presented an altered sleep pattern with more arousals and paw movement during sleep.2
In studies in human beings in comparison with the normal population, the SCI individuals had more difficulty in falling asleep, showing more frequent awakenings, worse subjective sleep, having pills to sleep more frequently prescribed, the sleep hours increased, naps becoming more frequent and of longer duration, and they had snored more and for more years. In particular, signs like spasms, pain and paraesthesia as well as problems with voiding have been cited as part of the problems related to sleep.3
In this way, it is extremely important that the evaluation of the pattern of sleep was done for a longer period (15 days) after the SCI, to perceive if these alterations in the sleep patterns are a permanent consequence of the new condition or if the normal pattern would come back over time.
Thus, the purpose of this study was to evaluate alterations in rat sleep architecture caused by SCI over a 15-day period in order to achieve better understanding of these sleep patterns.
Methods
Subjects
Male Wistar rats aged 90 days were used, provided by the animal facilities of Psychobiology Department's at Federal University of São Paulo. All experimental procedures were approved by the Ethics Committee of Federal University of São Paulo (CET No. 0061/04).
The animals were maintained in control conditions for a 12-h light–dark cycle and automatically controlled temperature at 23±2°C. Chow and water were supplied freely in standard cages cleaned daily to remove and change sawdust used as lining.
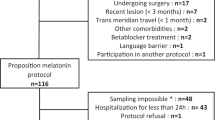
Groups
The rats were divided into two groups:
-
SHAM (n=10): only cutaneous incision around the spine was performed (not extending to more severe injury) and the spinal cord was not affected;
-
Spinal cord injury – SCI (n=10): SCI made at level T9.
The rats were submitted to the following procedures: electrode insertion surgery, 24-h duration baseline sleep recording, SCI (level T9) and subsequent sleep recording for 15 consecutive days.
Surgical preparation
Implanting the electrodes
Surgery was performed to implant electrodes for electroencephalography and electromyography sleep monitoring which allows to classify and quantify different sleep phases.
Two long, bipolar cortical ipsilateral recordings were performed of cortical electrical activity (ECoG). One was located lateral to the sagital plane, for ECoG with minimum theta activity level and another more medially to the sagital plane, for ECoG with maximum theta activity.4, 5
Anesthesia was performed using a combination of Diazepam (Valium), at 5.5 mg/kg, i.p. and Ketamin (Ketamin®) at 140.0 mg/kg i.p.
After anesthesia, the animals were submitted to trichotomy in the upper region of the head and the hind paws, and then placed in a stereotaxic apparatus (David Kopf™). Local asepsis was performed using polvidine. Xylocaine (0.5 ml 2% plus vasoconstrictor) was administered subcutaneously in the region of the future incision. Then a longitudinal incision was made on the scalp and the underlying tissue removed to expose the bone where sagital suture, bregma and lambda were visible.
Stereotaxic coordinates were then demarcated. A dental drill was used to very cautiously bore four holes avoiding injury to the dura mater. Four stainless steel micro screws (∅ 1.0 mm) were attached carefully touching only the dura mater (1±1.0 mm depth). Two electrodes were implanted in the dorsal muscle of the neck (trapeze), and one in each of the hind paws for electromyography analysis.
After implanting electrodes, a connector was fastened to the skull of the rat with self-polymerizing dental acrylic adhesive.
The rats were administered 0.5 ml/kg (i.m.) of poly-antibiotic suspension with streptomycins and penicillins (WYETH® Pentabiotic®) to prevent infection. The rats were also administered 10 mg/kg, i.p. of sodic diclofenac to assist postoperative analgesia and reduce surgical wound inflammation.
The rats were then taken to a photothermostimulation unit for approximately 12 h in order to avoid the hypothermic shock often found in a post-anesthesia period. After this period, they were taken to their cages and given free access to water and food for another 15 days before any experimental intervention.
Spinal cord injury
Before performing spinal cord surgery, the rats were anesthetized with Diazepan (Valium), dosage 5.5 mg/kg, i.p. and Ketamin (Ketamina®) dosage 140.0 mg/kg i.p.
After anesthesia set in, the thoracic level 9 (T9) processus spinalis was identified by tactile means and the rats submitted to dorsal region trichotomy. They were placed in a ventral decubitus position in the David Kopf stereotaxic apparatus. After asepsis of the back, an incision was made on the median line to expose the dorsal musculature. Muscles and ligaments were carefully dissected to expose the spinal apophyses of the T8–T9 vertebrae. Then the dorsal portion of the T9 vertebra was removed to expose the dorsal surface of the spinal cord. With the assistance of electronic magnifying apparatus, the dura mater was opened longitudinally and pressed down laterally. With the spinal cord exposed, it was carefully trans-sectioned using a scalpel, and then the surgical opening was sutured on both levels (muscular and cutaneous). In the SHAM group, an incision in the skin and muscles at level T9 was made but no SCI. After surgical suture asepsis, the rats were administered a poly-antibiotic suspension with streptomycin and penicillin (WYETH® Pentabiotic®), to prevent infection and sodic diclofenac for postoperative analgesia. After surgery, the rats were placed in a photo thermal stimulation cage for 12 h. After this period they were returned to their cages.
From surgery day through to the end of the experiment, the rats were examined every day to assess overall state of health, and abdominal massages were performed to assist urine excretion and defecation (if necessary), in an attempt to minimize as far as possible any signs or symptoms indicating suffering, such as lack of appetite, dehydration, surgical suture infection, abdominal swelling and prostration. If these signs were noted, the experiment was halted and the animal killed.
Electrocorticography
Polysomnography was recorded using a Nihon–Koden model QP 223 polygraph (digital signal acquisition) using five channels: two for electrocorticogram (ECoG), one for electromyogram (EMG) of the cervical musculature and two for EMG of both hind paws.
On concluding analysis, sleep parameters were quantified using the Polysmith Software program®.
Analysis of sleep records was divided in two periods of 12 h (light/dark). Periods of 30 sec were sequenced and low amplitude waves with rapid ECoG and EMG activation were classed as wakefulness (W); slow wave sleep (SWS) was indicated by large amplitude waves with slow ECoG and EMG activation, and paradoxical sleep characterized by fast ECoG activation, regular presence of hippocampus theta rhythm and muscular atone.6
The rats were submitted to two stages of sleep recording: baseline registration, 10 days after surgery to implant the electrodes, for 24 h and post SCI surgery after 24 h for 15 days continuously.
The sleep parameters examined were sleep efficiency, sleep latency, total wakefulness time, SWS, paradoxical sleep, and number of arousals.
The sleep parameters of the SHAM group animals were recorded for 15 days.
Histopathological study
The anatomopathological diagnosis of the degree of SCI was established by microscopic appearance, and the definition of lesion types was based on the length of the SCI.
The rats were killed using chloral hydrate (lethal doses) and the spinal cord removed and placed in 10% buffered formalin. Then samples from the cervical, thoracic, lumbar and sacral levels were kept in paraffin, as per routine optical microscope procedures. The 5-μ M histological sections were dyed using hematoxylin–eosin (HE) for histopathological examination.
Statistical analysis
The sleep pattern variables for the 2–12 h light/dark periods – with periodic measurements level, normal distribution and similar variances were analyzed using the two-factor ANOVA test (GROUP factor: SHAM and SCI; DAY factor: baseline, D1, D2, D3…D15), with repeated measures for the day factor. The Tukey's test was applied as necessary. SHAM and SCI groups were compared in terms of the number of animals presenting limb movement using the exact Fisher test each day. All analyses used a 0.05 significance level and results were presented as mean±standard deviations.
Results
Sleep parameters
Efficiency
A significant reduction was detected on the first day of the SCI group in relation to baseline registration and on Days 1–3, 5, 10 and 12 in relation to the same day for the SHAM group (F(15, 285)=3.175; P<0.05).
In relation to the dark period Days 1 and 2 after SCI presented higher sleep efficiency in relation to the baseline and to the same day for the SHAM group (F(15, 285)=3.647; P<0.05).
On joining the light and dark sleep periods, no difference was found on Days 2 (P=0.21) and 3 (P=0.06).
Total wakefulness time
When total wakefulness time in the light period was analyzed, the SCI group showed a significant increase on Days 1–3, 5, 10 and 12 in relation to their baseline record (F(15, 285)=3.175; P<0.05). No differences were found in relation to the SHAM group.
In the dark period, there was a reduction on Days 1 and 2 when the SCI group was compared to its baseline record (F(15, 285)=3.663; P<0.05) (Figure 1).
Sleep efficiency (%) and Wakefulness (%) on baseline day (b), and the next 15 days for SCI rats (n=10) and SHAM (n=10) rats during light (a) and dark (b) session recording. Values are expressed as mean±SD. Statistical analysis included two-way ANOVA. *Significant differences between baseline and post-SCI days. #Significant differences between the two groups (P<0.05)
Sleep stage
After SCI, the rats tended to present longer SWS total times during the light period. Day 1 of the SCI group differed in relation to baseline registration and group SHAM on the same day, whereas the 14 differed only from its baseline record (F(15, 285)=2.93; P<0.05).
In the dark period of Day 1 after SCI, the rats showed an increase in total time in SWS in relation to the baseline and to SHAM for the same day. Day 2 after SCI also presented an increase in relation to the SHAM group for the same day and Day 13 after SCI presented significant increase in relation to the baseline (F(15, 270)=4.68; P<0.05).
Paradoxical sleep
On analyzing paradoxical sleep, the SCI group presented a daytime variation in sleep with a reduction on Day 1 in relation to the baseline and SHAM for the same day. On Day 3, a difference was found in relation to SHAM for the same day (F(15, 285)=3.63; P<0.05).
However, no significant difference was observed in the dark period (Figure 2).
Non-REM (%) and paradoxical sleep (%) on baseline day (b), and the next 15 subsequent days for SCI rats (n=10) and SHAM (n=10) rats during light (a) and dark (b) session recording. Values are expressed as mean±SD. Statistical analysis included two-way ANOVA. *Significant differences between baseline and post-SCI days. #Significant differences between the two groups (P<0.05)
Arousal
After SCI, the rats showed an increase in the number of arousals on Days 1 and 12 in relation to baseline in the light period. After SCI, Day 1 differed from days 3, 4, 9–12 and 15 (F(15, 285)=2.28; P<0.05).
In the dark period on days 1 and 2, the SDCI group presented a significant increase in relation to its baseline registration. Furthermore, these days also presented significantly higher values on comparing them with Days 4–6, 8–11, 14 and 15 in the same group (F(15, 285)=3.68; P<0.05) (Figures 3 and 4).
Arousals (number) on baseline day (b), and the next 15 days for SCI rats (n=10) and SHAM (n=10) rats during light (a) and dark (b) session recording. Values are expressed as mean±SD. Statistical analysis included two-way ANOVA. *Significant differences between baseline and post-SCI days. # Significant differences between day 1 and the other days post SCI (P<0.05)
Latency
Sleep latency on Day 1 after SCI showed a tendency to increase, no statistical differences were found in either the light or dark period (P=0.06).
Limb movements
The SCI group rats began to show paw movements during sleep as of Day 4 after SCI. The numbers of animals presenting limb movements were statistically significant on Days 4–15 (P<0.05 – Fisher) when compared to baseline recording and the SHAM group. The animals in the SHAM group did not present limb movement during the 8-day recording period. The average duration of limb movements during sleep was 3–9 s. Some rats presented isolated movements, whereas others presented series of movements during some sleep periods.
Histopathological study
Histopathological examination revealed morphologic alterations in all spinal cords submitted to surgical procedure.
Of lesion were seen in the spinal cord were lesion affecting almost all the spinal cord (dorsal column and ventral column).
Discussion
The purpose of this study was to investigate differential changes in sleep architecture in rats studied 15 days after SCI. The present findings show SCI rats with reduced sleep efficiency, fragmented sleep with more arousals, thus increasing total wakefulness time in relation to baseline. Also shown were increased total slow wave sleep time and decreased total paradoxical sleep time. All those parameters remained unaffected during the 15-day period in the SHAM group.
These results are similar to our previous 7-day-period study that found reduced sleep efficiency on Day 1 after SCI, and an increased number of arousals and appearance of paw movements during post-SCI sleep.2
The rats presented disrupted circadian rhythm after SCI. On grouping sleep efficiency in the light and dark periods, there were no differences on the second and third days, in other words, on those 2 days both the light and dark period presented similar sleep efficiency levels rather than the pattern reported by Van Luijtelarr and Coenen7 with 62% predominance of sleep in the light period and 33% in the active or dark period.
In view of the results of the present study, in which the rats tended to reduce sleep efficiency in relation to the SHAM group on the seventh day after SCI, a number of questions may be posed. Is this reduced sleep efficiency due to discomfort caused by SCI? Or does the quality of sleep deteriorate over time the longer the animal remains in this condition without any other stimulus?
On comparing sleep pattern with our previous 7-day SCI-period study, we note that the rats presented similar sleep architecture during the first 7 days after SCI. After 7 days, the sleep pattern presents alterations and there are variations in its architecture. These alterations may be due to inherent patterns arising from SCI, such as the appearance of paw movements during sleep,2 or a longer period of inactivity, as the rat obviously reduces movement after SCI.
We know that alterations in sleep pattern in SCI individuals may be due to the consequences of the injury for the individual, and pain and inactivity are very often characteristics of this population.
In a study conducted by Budh et al8 the quality of the SCI individuals sleep was analyzed and the patients presenting pain symptoms were compared with the others. The patients presented average SCI time of 15.6 years±11.3, and 129 patients presented incomplete SCI (ASIA impairment grades B–E) and 57 presented complete SCI (ASIA impairment grade A). The results showed that subjectively reported sleep quality tended to be worse in the SCI patients presenting continuous or intermittent pain than in the non-pain patients. In general, the severity of pain cannot be seen as a predictive factor for lower quality sleep, but sleep disorders and intense increase in pain do coincide in many studies.9, 10
Respiratory disorders11 and periodic limb movements are the most frequent sleep disorders found in SCI patients.12, 13, 14, 15 These sleep disorders reduce sleep efficiency, and one of the factors leading to this reduction may well be the increased number of arousals during sleep.
In studies conducted by De Mello et al14 with SCI patients presenting PLM, it was found that the level of movement diminished after physical exercise.
The rats in the present study presented paw movements during sleep after SCI, thus corroborating the data described in the previous study.2 All the rats in the previous study2 and those in the present study presented SCI. A number of hypotheses were posed to explain the presence of these paw movements during sleep: possible involvement of the gracilis and cuneate fascicles in generating spontaneous movements during sleep and participation of the spinal dopaminergic system in pain modulation and autonomic and motor responses, in view of the fact that a dysfunction of spinal dopaminergic neurons may be involved in the pathophysiology of certain conditions, such as Parkinson's disease.16
Movement disorders were also reported by Garcia-Garcia et al17 using a Parkinson's disease animal model. These motor disorders inhibit the progression into deep sleep, causing light and fragmented sleep throughout the night. These changes probably affect sleep.
Our findings of alterations in sleep patterns during the 15-day period of electroencephalographic recording in SCI rats showed that SCI may be a key factor in altering sleep pattern in SCI subjects and that the inactivity caused by SCI may be exacerbating this altered sleep pattern. Studies in animal models are of fundamental importance. As tools for the in-depth analysis required to understand the mechanisms generating these behaviors, they can provide better quality of life for persons affected by SCI.
Advances and continued improvements in the current use of SCI animal models should be encouraged and more laboratory work should focus this relatively neglected area of experimental SCI.
References
Andersen ML, Tufik S . Sleep patterns over 21-day period in rats with chronic constriction of sciatic nerve. Brain Res 2003; 12: 84–92.
Esteves AM, De Mello MT, Lancellotti CL, Natal CL, Tufik S . Occurrence of limb movement during sleep in rats with spinal cord injury. Brain Res 2004; 13: 32–38.
Biering-Sorensen F, Biering-Sorensen M . Sleep disturbances in the spinal cord injured: an epidemiological questionnaire investigation, including a normal population. Spinal Cord 2001; 39: 505–513.
Ronsemberg RS, Bergmann BM, Rechtschaffen A . Variations in slow wave activity during sleep in the rat. Physiol Behav 1976; 17: 931–938.
Bergmann MB, Kushida CA, Everson CA, Gilliland MA, Obermeyer W, Rechtschaffen A . Sleep deprivation in the rat: II. Methodology. Sleep 1989; 12: 5–12.
Timo-Iaria C, Negrao N, Schmidek WR, Hoshino K, Menezes CEL, Rocha TL . Phases and states of sleep in the rat. Physiol Behav 1970; 5: 1057–1062.
Eljm VL, Aml C . An EEG averaging technique for automated sleep–wake stage identification in the rat. Physiol Behav 1984; 33: 837–841.
Budh Norrbrink C, Hultling C, Lundeberg T . Quality of sleep in individuals with spinal cord injury: a comparison between patients with and without pain. Spinal Cord 2005; 43: 85–95.
Sayaar K, Arikan M, Yontem T . Sleep quality in chronic pain patients. Can J Psychiatry 2002; 47: 844–848.
Morin CM, Gibson D, Wade J . Self-reported sleep and mood disturbance in chronic pain patients. Clin J Pain 1998; 75: 75–84.
Klefbeck B, Sternhag M, Weinberg J, Levi R, Hultling C, Borg J . Obstructive sleep apneas in relation to severity of cervical spinal cord injury. Spinal Cord 1998; 36: 621–628.
De Mello MT, Lauro FAA, Silva AC, Tufik S . Incidence of periodic leg movements and restless legs syndrome during sleep following acute physical activity in spinal cord injury subjects. Spinal Cord 1996; 34: 294–296.
De Mello MT, Silva AC, Rueda AD, Poyares D, Tufik S . Correlation between K complex, periodic leg movements (PLM), and myoclonus during sleep in paraplegic adults before and after an acute physical activity. Spinal Cord 1997; 35: 248–252.
De Mello MT, Silva AC, Esteves AM, Tufik S . Reduction of periodic leg movement in individuals with paraplegia following aerobic physical exercise. Spinal Cord 2002; 40: 646–649.
De Mello MT, Esteves AM, Tufik S . Comparison between dopaminergic agents and physical exercise as treatment for periodic limb movements in patients with spinal cord injury. Spinal Cord 2004; 42: 218–221.
Lindvall O, Bjorklund A, Skagerberg G . Dopamine-containing neurons in the spinal cord: anatomy and some functional aspects. Ann Neurol 1983; 14: 255–260.
Garcia-Garcia F, Ponce S, Brown R, Cussen V, Krueger JM . Sleep disturbances in the rotenone animal model of Parkinson disease. Brain Res 2005; 1042: 160–168.
Acknowledgements
This work was supported by grants from Associação Fundo de Incentivo à Psicofarmacologia (AFIP), FAPESP (03/06297-3, and CEPID 98/143033) and CNPQ.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Esteves, A., Mello, M., Squarcini, C. et al. Sleep patterns over 15-day period in rats with spinal cord injury. Spinal Cord 45, 360–366 (2007). https://doi.org/10.1038/sj.sc.3101971
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101971