Abstract
Study design:
Pilot study; prospective design.
Setting:
University Hospital, Virginia, USA.
Objective:
To examine a phosphorus supplement as a urine-acidifying agent in patients with neurogenic bladder on clean intermittent catheterization.
Methods:
Seven patients were followed for 4 weeks. For the first week of study urine pH was measured three times a day: first morning urine sample, afternoon sample, evening sample. For the second and third weeks urine pH was measured and the patients drank a phosphorus supplement three times a day. For the fourth week of study the patients did not take the phosphorus supplement but the measurement of urine pH was continued. The patients were visited in their homes twice a week. During each visit a sample of urine was collected for culture. A supplement container count was performed and urine pH recordings were checked.
Results:
There was no significant change in urine pH during the 2-week period when a patient was on phosphorus supplementation compared to when the patient was off supplementation. In addition, urine acidification was not achieved over the time period when urine pH was monitored.
Conclusion:
Phosphate supplementation had no effect on urine pH in patients with neurogenic bladder.
Similar content being viewed by others
Introduction
Patients with neurogenic bladder on clean intermittent catheterization (CIC) for bladder emptying have a high frequency of bacteriuria most commonly due to Escherichia coli.1 In an effort to decrease the high frequency of bacteriuria in this population we conducted two randomized controlled treatment trials. In separate studies, we examined the effect of daily nitrofurantoin prophylaxis2 and cranberry prophylaxis3 on the rates of bacteriuria. We found that these prophylactic agents had no effect on the rate of bacteriuria in patients with neurogenic bladder on CIC.
Urine-acidifying agents, which have been used for prophylaxis in this population are appealing because they do not alter gastrointestinal flora, do not induce bacterial resistance and are inexpensive. Investigators have proposed that urine-acidifying agents inhibit bacterial growth due to the effect of undissociated organic acids.4 These organic acids are in high concentrations in acidic urine. Previous therapeutic trials using urine-acidifying agents as methenamine salts and ascorbic acid in patients with neurogenic bladder5, 6, 7, 8 have not reliably produced urine acidification over a 24 h period.
Another urine-acidifying agent that has not been studied in this population is inorganic phosphates.9 Phosphorus in the form of inorganic phosphate is commonly used as a dietary supplement and for phosphate replacement in patients with proximal tubulopathies and osteomalacia. Phosphates (H2PO4) are excreted at the distal renal tubule where hydrogen ion is exchanged for sodium ion causing a decrease in urine pH. In this pilot study, we looked at the effectiveness of a commonly used phosphorus supplement as a urine-acidifying agent in patients with neurogenic bladder on CIC. If urine acidification was achieved over a 24 h period our intention was to design a larger treatment trial to ascertain whether acidification decreased the frequency of bacteriuria in this population.
Methods
Seven young adults with neurogenic bladder who lived at home, had a normal renal ultrasound and performed CIC four times a day were enrolled. Exclusion criteria included pregnancy, a history of kidney or liver disease, hypercalcemia, hyperphosphatemia, urolithiasis or recent surgery. Use of antacids, antihypertensives, diuretics, corticosteroids, calcium, phosphorus and/or vitamin D preparations also precluded enrollment. Patients with spinal cord injury were enrolled 2 or more years postinjury. All patients continued to receive medical care from their primary physician; no therapies were withheld or altered. The urine cultures obtained for the study did not influence the patient's care, because the results were kept on file by a research technologist and were not available either to the child's physician or to the investigator. The protocol was approved by the University of Virginia Human Investigation Committee.
Each patient was followed for 4 weeks: 1 week prior to supplementation, 2 weeks on supplementation and 1 week off supplementation. Patients were instructed on preparation of the supplement and measurement of urine pH prior to initiation of the study. For the first week the patient recorded urine pH three times a day: the first morning urine sample, an afternoon sample and an evening sample. For this, urine was collected after catheterization for voiding. A pH indicator strip (colorpHast®, EM Science, Gibbstown, NJ, USA) was immersed in urine then read after 1 min according to the color on the strip. The pH indicated by the color was then recorded. For the second and third week the patient continued to record urine pH three times a day. In addition, the patient drank a phosphorus supplement (Neutra-phos®, Alza Pharmaceuticals, Mountain View, CA, USA) three times a day (morning, afternoon and evening). The phosphorus supplement was a powder concentrate supplied in a packet. Each packet contained 240 mg of phosphorus, 164 mg of sodium and 278 mg of potassium. For ingestion, the packet was opened and the powder mixed with 3 ounces of water; then the mixture was immediately taken by mouth. For the fourth week the patient did not take a phosphorus supplement but did continue to record urine pH three times a day. Each patient was visited twice a week at home during the study. At each visit a packet count and recording of urine pH was checked to assess compliance. In addition, a sample of bladder urine collected for culture during routine CIC on the day of the visit was immediately refrigerated and plated within 10 hours. A positive urine culture (bacteriuria) was defined as ⩾104 colony-forming units of a pathogen per milliliter of urine as previously described.1
Results
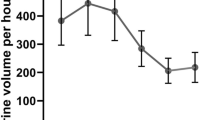
From March 1 to August 1, 2004, seven patients were followed for 28 patient-weeks (Table 1). There were three males and four females, 18–29 years of age. Five patients had neurogenic bladder caused by myelomeningocele (Nos 1, 2, 3, 4, 5); the two patients with neurogenic bladder due to traumatic spinal cord injury were studied 5 years after injury. There was no significant change in urine pH during the 2-week period when a patient was on phosphorus supplementation compared to when the patient was off supplementation (Table 1). In three patients the mean pH value dropped 0.1–0.4 units during supplementation; in three patients the mean pH value increased by 0.2–0.6 units during supplementation, and in one patient the mean pH value did not change. In addition, urine acidification was not achieved over the time period when urine pH was monitored. Of interest was the observation that the frequency of bacteriuria in an individual patient was similar on and off supplementation.
Discussion
In 1917 Shohl and Janney10 reported that the optimal growth of E. coli in urine occurred between pH of 6.0 and 7.0 and that inhibition of growth was produced at pH 5.0 and below. Using in vitro models investigators demonstrated that when the pH of pooled urine was decreased to <5.5, the growth of E. coli was inhibited for 4–24 h.11, 12
Urine acidification over a 24 h period has been difficult to achieve in patients with neurogenic bladder.6, 7, 8, 9 Inability to maintain urine acidity in the neurogenic bladder may be due to chronic colonization of bladder urine with bacteria as Proteus species13 diet and dietary supplements and the use of antibiotics.14 Recent work by Cahill et al15 revealed that urine pH is modified from an acid pH to an alkaline pH as it passes from the renal pelvis to the bladder. These investigators proposed that the pH of bladder urine may not reflect the pH of the upper tract.
We found that phosphate supplementation had no significant effect on urine pH in patients with neurogenic bladder. As phosphate was not found to cause urine acidification, further study on the effect of phosphate in decreasing bacteriuria will not be pursued.
References
Schlager TA, Dilks S, Trudell J, Whittam TS, Hendley JO . Bacteriuria in children with neurogenic bladder treated with intermittent catheterization: natural history. J Pediatr 1995; 126: 490–496.
Schlager TA, Anderson S, Trudell J, Hendley JO . Nitrofurantoin prophylaxis for bacteriuria and urinary tract infection in children with neurogenic bladder on intermittent catheterization. J Pediatr 1998; 132: 704–708.
Schlager TA, Anderson S, Trudell S, Hendley JO . Effect of cranberry juice on bacteriuria in children with neurogenic bladder receiving intermittent catheterization. J Pediatr 1999; 135: 698–702.
Kass E, Zangwill D In: E. Kass (ed). Biology of Pyelonephritis. Boston 1960, pp 663.
Pearman J, Peterson GJ, Nash JB . The antimicrobial activity of urine of paraplegic patients receiving methenamine mandelate. Invest Urol 1978; 16: 91–98.
Devenport JK, Swenson JR, Dukes GE, Sonsalla PK . Formaldehyde generation from methenamine salts in spinal cord injury. Arch Phys Med Rehabil 1984; 65: 257–259.
Hetey S, Kleiberg M, Watson DP, Johnson EW . Effect of ascorbic acid on urine pH in patients with injured spinal cords. Am J Hosp Pharm 1980; 37: 235–237.
Lamid S . Ascorbic acid and methenamine mandelate on the urinary pH of spinal cord injury patients. J Urol 1983; 129: 245–246.
Haynes R, Murad F . Agents affecting calcification. In: Goodman LS and Gilman A (ed). The Pharmacological Basis of Therapeutics, 6th edn. Macmillan Publishing: New York, NY 1980, pp 1524–1531.
Shohl A, Janney JH . Optimal growth of E. coli in urine. J Urol 1917; 1: 211.
Asscher AW, Sussman M, Waters WE, Davis RH, Chick S . Urine as a medium for bacterial growth. Lancet 1966; 2: 1037–1041.
Kaye D . Antibacterial activity of human urine. J Clin Invest 1968; 47: 2374–2390.
Mobley H . Virulence of proteus mirabilis. In: Mobley H and Warren JW (ed). Molecular Pathogenesis and Clinical Management, 1st edn. American Society of Microbiology: Washington DC 1996, pp 245–269.
Murphy JL . Renal tubular acidosis in children treated with trimethoprim-sulfamethoxazole during therapy for acute lymphoid leukemia. Pediatrics 1992; 89: 1072–1074.
Cahill D, Fry CH, Foxall, P . Variation in urine composition in the human urinary tract: evidence of urothelial function in situ. J Urol 2003; 169: 871–874.
Acknowledgements
This work was supported by a grant from the EM Faculty Research Fund and the Pendleton Pediatric Infectious Disease Research Laboratory.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Schlager, T., Ashe, K. & Hendley, J. Effect of a phosphate supplement on urine pH in patients with neurogenic bladder receiving intermittent catheterization. Spinal Cord 43, 187–189 (2005). https://doi.org/10.1038/sj.sc.3101700
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101700