Abstract
Study design: Case report and review of literature.
Objectives: Intracranial chronic subdural hematoma (SDH) is a well-recognized complication of ventriculoperitoneal (VP) shunt. Spinal chronic SDH is very rarely associated with VP shunt.
Setting: Kaohsiung Medical University Hospital, Kaohsiung, Taiwan.
Case report: We describe a spinal chronic SDH, developing after a minor trauma, in a patient who underwent a VP shunt surgery for hydrocephalus 6 months previously. A good outcome was achieved after decompressive surgery.
Conclusion: Spinal chronic SDH should be considered in the diagnosis of progressive spinal compression, especially in the patients with VP shunt after minor trauma.
Similar content being viewed by others
Introduction
Spinal chronic subdural hematoma (SDH) is a rare entity among spinal hematomas. Only 22 cases of spinal chronic SDH have been reported in the literature.1, 2 Spinal chronic SDH is frequently spontaneous or related to minor trauma.1, 3, 4, 5 Here, we describe a spinal chronic SDH, developing after a minor trauma, in a patient with a history of ventriculo-peritoneal (VP) shunt surgery for hydrocephalus 6 months previously.
Case report
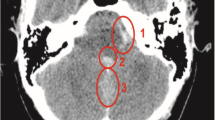
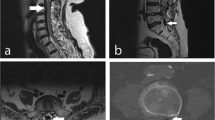
A 78-year-old male presented with progressive right leg weakness for 1 month. Six months ago, he had a VP shunt surgery for normal pressure hydrocephalus in our hospital, with the symptom of unsteady gait. The gait was markedly improved after the shunting procedure. One month before, he slipped with the impact being on one buttock. Right leg weakness developed progressively. A brain computerized tomography (CT) scan was arranged and did not display intracranial hematoma. Plain X-ray films of T-L spine showed degenerative change. Lumbar spine magnetic resonance image (MRI) revealed a mass filling of the dural sac at the level of L3-4-5. The sagittal T1-weighted MRI showed a slightly hyperintense lesion dorsally and T2-weighted MRI showed a isointense lesion with some hyperintense fields, suggesting a spinal chronic subdural hematoma (Figure 1).
Laminectomy at the level of L3-4-5 was performed. No extradural lesion was found. The epidural fat looked dark-yellowish and inflammation-like. Dural matter was opened and a thick grayish membrane was found. The membrane was incised and approximately 5 ml motor oil-like blood was found. After the blood was drained, the arachnoid was seen and it was intact. After operation, a significant improvement in the muscle power of the right leg was achieved. The MRI did not show recurrent subdural hematoma 3 months postoperatively.
Discussion
Although spinal chronic SDH is frequently spontaneous or related to minor trauma, coagulopathy is uncommon.1, 3 The spinal chronic SDH most often occurs in patients aged between 50 and 70 years. The lumbar and thoracolumbar regions are the most common sites. Spinal chronic SDH presented with progressive symptoms of spinal cord compression. The MRI facilitates definite diagnosis preoperatively.1, 6, 7 The pathogenesis of chronic spinal subdural hematoma remains unclear. Initial hemorrhage in the subarachnoid space is thought to be the primary lesion that eventually dissects the subdural space.1, 8 However, the arachnoid in our case was intact and there was no hematoma in the subarachnoid space.
The formation of an intracranial SDH is a well-recognized complication of ventricular shunting procedures.9, 10 The correlation between spinal chronic SDH and VP shunt is still unclear. Following ventricular drainage, the intracranial dural-arachnoid separates, increasing tension on the bridging veins and increasing the chance of rupture with mild trauma, as well as providing a space for blood and CSF to mix.10, 11 The presence of air within the intracranial subdural space was observed in up to 64% of all pneumoencephalograms shortly after the spinal air injection.9, 12 This supported previous reports that the intracranial and spinal subdural spaces are continuous.12, 13 If this is the case, it is surprising that spinal chronic SDH is not recognized among those patients with intracranial chronic SDH. Perhaps, just as intracranial chronic SDH may sometimes not cause symptoms,14 spinal chronic SDH may also remain silent. Until now, only one case presented a simultaneous thoracolumbar spinal and intracranial chronic SDH following VP shunting for hydrocephalus.9 In our case, intracranial SDH was excluded after the brain CT examination. Progressive right leg weakness and minor trauma history indicated MRI examination. Spinal SDH undergoes MRI signal changes as a result of the evolution of the clot that are similar to those of intracranial SDH.15, 16, 17 In acute cases, there is isointensity or hypointensity with T1 and T2 weighting. In chronic cases, there is more diffuse hyperintensity within the hematoma.17 In contrast to MRI findings of spinal chronic SDH in the literature, we observed that T1-weighted images showed irregular but well-circumscribed hyperintense lesion in the intradural space, and T2-weighted images showed isointense lesion with some hyperintense fields. The MRI findings are not typical of chronic SDH which make the preoperative diagnosis difficult.
The operative findings in spinal SDH correspond to the duration of symptoms and the evolution of the clinical syndrome.18 In acute cases, the clot shows variable volume, but is semiliquid and dark red. In subacute cases, the clot has organized to some degree. In chronic cases, a well-defined membrane enclosing a fluid-filled cavity is found. There was a membrane formation found in our case. Our case, documented by the inflammatory change of epidural fat and history of falling on his buttock, suggested that spinal chronic SDH is a result of trauma. Rader has proposed that spinal SDH results from an indirect spinal, SDH which in turn results from an indirect force on the intraspinal vessels. A sudden increase in abdominal and thoracic pressures elevates the intravascular pressure in the spinal subdural and subarachnoid spaces. This force would not be neutralized by a simultaneous increase in spinal fluid pressure because of the shielding effect of the spinal column and its ligaments. Such a momentary disparity between intravascular and extravascular pressures could result in rupture of a spinal vessel.19 Surgical decompression resulted in a good outcome. The review in the literature also showed 80% improvement in neurological function after operation.1, 3, 6
Conclusions
Spinal chronic SDH, although rare, should be considered in the diagnosis of progressive spinal compression, especially in the patients with VP shunting after a minor trauma. Good outcome can be achieved with prompt diagnosis and early surgical decompression.
References
Abla AA, Oh MY . Spinal chronic subdural hematoma. Neurosurg Clin N Am 2000; 11: 465–471.
Kotwica Z, Stawowy A, Polis L . Spinal chronic subdural hematoma in a 7-year-old girl. Eur J Pediatr 1989; 148: 779–780.
Brandt RA . Chronic spinal subdural hematoma. Surg Neurol 1980; 13: 121–123.
Friday RY, Pollack IF, Bowen A, Pollack A, Ragni M . Spontaneous spinal subdural hematoma in a young adult with hemophilia. J Natl Med Assoc 1999; 91: 289–294.
Wang CJ, Kung SS, Howng SL . Traumatic lumbar spinal subdural hematoma – a case report. Kaohsiung J Med Sci 2001; 17: 576–578.
Leber KA, Pendl G, Kogler S, Kammerhuber F, Ebner F . Simultaneous spinal and intracranial chronic subdural hematoma. Case illustration. J Neurosurg 1997; 87: 644.
Shimada Y, Sato K, Abe E, Miyakoshi N, Tsutsumi Y . Spinal subdural hematoma. Skeletal Radiol 1996; 25: 477–480.
Vinters HV, Barnett HJ, Kaufmann JC . Subdural hematoma of the spinal cord and widespread subarachnoid hemorrhage complicating anticoagulant therapy. Stroke 1980; 11: 459–464.
Silver JM, Wilkins RH . Spinal subdural hematoma formation following ventriculoperitoneal shunting for hydrocephalus Case report. Acta Neurochir (Wien) 1991; 108: 159–162.
Samuelson S, Long DM, Chou SN . Subdural hematoma as a complication of shunting procedures for normal pressure hydrocephalus. J Neurosurg 1972; 37: 548–551.
Portnoy HD, Schulte RR, Fox JL, Croissant PD, Tripp L . Anti-siphon and reversible occlusion valves for shunting in hydrocephalus and preventing post-shunt subdural hematomas. J Neurosurg 1973; 38: 729–738.
Paul LW, Erickson TC . Observations on the presence of subdural gas after pneumoencephalography. Radiology 1946; 46: 139–147.
Hemmingson H . Roentgenologic investigations on the intracranial subdural space with a view to revealing the presence of subdural adhesions. Acta Radiol (Stockh) 1940; 21: 379–391.
Reigel DH . Changes in the subdural space following cerebrospinal fluid shunts. In: Raimondi AJ (ed) Concepts in Pediatric Neurosurgery, Vol 3. Basel: S Karger 1983, pp 145–146.
Duprez T, Grandin C, Malghem J . MRI monitoring of an acute spinal subdural hematoma with spontaneous resolution. Acta Neurol Belg 1995; 95: 101–103.
Firsching R, Zanella F, Lanfermann H . The dynamics of magnetic resonance findings in patients with a spinal hematoma. Paraplegia 1993; 31: 180–185.
Kulkarni AV, Willinsky RA, Gray T . Serial magnetic resonance imaging findings for a spontaneously resolving spinal subdural hematoma: case report. Neurosurgery 1988; 42: 398–401.
Russell N, Benoit BG . Spinal subdural hematoma: a review. Surg Neurol 1983; 20: 133–137.
Rader JP . Chronic subdural hematoma of the spinal cord: report of a case. N Engl J Med 1955; 253: 374–376.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Su, YF., Hwang, YF., Lee, KS. et al. Spinal chronic subdural hematoma in a patient with ventriculo-peritoneal shunting after a minor trauma. Spinal Cord 42, 717–719 (2004). https://doi.org/10.1038/sj.sc.3101643
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101643