Abstract
Study design: Case report of an unusual use of AMS 800 (American Medical Systems, Inc., Minnetonka, Minnesota) artificial urinary sphincter cuff in a female patient affected by neurogenic urinary incontinence.
Objective: To describe this rare surgical solution.
Setting: Department of Urology in Italy.
Methods: A 43-year-old woman affected by flaccid paraplegia, acontractile bladder and incompetent bladder neck, underwent an implantation of an artificial urinary sphincter AMS 800. After 7 years, a mechanical failure of the device occurred and pubovaginal sling (PVS) utilizing the cuff of the sphincter was employed due to the poor quality of rectus fascia and the development of previous allergy for some heterologous materials.
Results: At 17 months follow-up, the patient is contnent and able to empty the bladder by clean intermittent self-catheterization (CIC).
Conclusion: The risk of developing an allergy reaction due to the employment of heterologous materials and the impossibility to use the rectus fascia obliged us to adopt the pre-existent cuff of the artificial urinary sphincter AMS 800.
Similar content being viewed by others
Introduction
In the last decade, the artificial urinary sphincter has been one of the major advances in the treatment of incontinence in adults. However, the surgical management of neurogenic sphincteric incontinence is still under debate. Some prefer the rectus fascial sling while others utilize the artificial urinary sphincter despite device placement complications widely reported in the literature.1, 2, 3, 4 In fact, the employment of artificial urinary sphincter causes urethral erosion in 32% of cases, mechanical complications in 13.8% and finally infections in 4.5%.5 Mechanical malfunction is usually repaired by replacing the nonfunctioning component or by inserting a new device.6, 7, 8
We present a case of an AMS 800 (American Medical Systems, Inc., Minnetonka, MN, USA) artificial urinary sphincter previously implanted in a patient affected by sphincteric neurogenic urinary incontinence who underwent pubovaginal sling (PVS), by using the urethral cuff component of the artificial device.
Case report
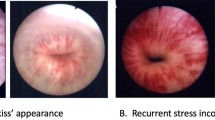
EB, a 43-year-old woman, suffered from flaccid paraplegia with areflexia of lower extremities, anaesthesia from D12-L1 and stress urinary incontinence owing to an intraoperative complication during a lumbar kyphosis operation carried out at the age of 16 years. The urodynamic evaluation demonstrated: (1) the presence of leakage of infusion water at 135 ml of infusion with filling rate of 20 ml/min (Figure 1); (2) maximum closure urethral pressure (MCUP) of 9 cm H2O (Figure 2). These results were compatible with an acontractile detrusor and an incompetent bladder neck due to a probable decentralization of parasympathetic and sympathetic components.
At 36 years of age, the patient underwent an implantation of an artificial urinary sphincter AMS 800 (American Medical Systems, Inc., Minnetonka, Minnesota). After 7 years of AMS 800 implantation, a mechanical failure of the device occurred in relation to pump malfunction of the fluid equilibrating resistor causing the reappearance of urinary incontinence while the spillage of the contrast liquid contained inside the reservoir produced an allergy for contrast agent and latex material. In consideration of this event, the patient refused the implantation of a new device and preferred a PVS operation with autologous material. The artificial urinary sphincter was removed through an abdominal and vaginal access. Since it was impossible to use the rectus fascia as sling, because it was of poor quality, or the fascia lata because it was not accepted by the patient for aesthetic reasons, we decided to employ the sphincter cuff just inside as a sling to reduce the risk of allergy caused by heterologous material. The section at 12 h was carried out and the sling was placed in order to support the bladder neck. Each end of the cuff was secured with a long 2/0 nonabsorbable suture. The sutures were tied together over the rectus fascia in midline without tension. An intraoperative and postoperative antibiotic therapy (Vancomycin 2 g/die for 1 day and Ampicillin 2 g/die for 7 days) was necessary to prevent prosthetic material infection. Postoperative care was not complicated by any infection of the sling. After 3 months, MRI showed the correct positioning of the sling (Figure 3) and at 17 months follow-up the patient was continent and able to empty the bladder by clean intermittent self-catheterization (CIC). The cystoscopic evaluation performed every 3 months after operation showed no evidence of urethral erosion. The urinalysis carried out quarterly always resulted negative for infection.
Conclusion
The challenge of finding an effective procedure to achieve long-term continence in subjects with neurogenic sphincteric incompetence remains unresolved. There are many reports on the success of PVS by using the rectus fascia for the treatment of sphincteric neurogenic incontinence both in children and in adults. The procedure is established in the neurological female patient as an alternative to the artificial urinary sphincter assuming that following PVS the patients will have to empty their bladders by intermittent catheterization.9 In these cases, the continence is high and with few complications.10, 11, 12 On the other hand, it is well known that up to now the rectus fascia is the gold standard material for bladder neck suspension in PVS operations. Nevertheless, some authors have recently showed that urethral erosion after a PVS procedure can occur irrespective of the sling material, and that an excessive sling tension is most probably the main cause of this complication.13 In our case, we placed the sling without tension to support the bladder neck to prevent the possibility of urethral erosion while the concurrent presence of an allergy for contrast agent, latex material and the fear that this clinical problem could be extended also to other substances obliged us to employ the pre-existent cuff of AMS 800 urinary sphincter as sling just because it was well tolerated by the patient. This surgical solution, never described before in the literature, should be considered necessary only in selected cases. In fact, in the case of neurologic patients the continent urinary diversion, as described by Mitrofanoff, is the best surgical solution even if some indications for a continent catheterizable stoma are the inability to perform self-catheterization through the normal urethral route due to severe urethral stricture or due to upper limb neurogenic partial deficit. In this case, the patient did not have neurogenic deficit of upper limbs and would not accept the presence of an eventual abdominal stoma. In conclusion, we consider this surgical solution as proposable only in particular cases as the above mentioned, but caution should be exercised in supporting the bladder neck without tension to reduce the risk of possible urethral erosion.
References
Thomas K, Venn SN, Mundy AR . Outcome of the artificial uriary sphincter in female patients. J Urol 2002; 167: 1720–1722.
Hajivassiliou CA . A review of the complications and results of implantation of the AMS Artificial Urinary Sphincter. Eur Urol 1999; 35: 36–44.
Diana M, Schettini M, Gallucci M . Evaluation and management of malfunctionings following implantation of the artificial urinary sphincter. Int Surg 1999; 84: 241–245.
Elliott DS, Barrett DM . Mayo Clinic long-term analysis of the functional durability of the AMS 800 artificial urinary sphincter: a review of 323 cases. J Urol 1998; 159: 1206–1208.
Fishman JI, Shabsigh R, Scott B . Experience with the artificial urinary sphincter model AS800 in 148 patients. J Urol 1989; 141: 307–310.
Wang Y, Hadley HR . Management of persistent or recurrent urinary incontinence after placement of artificial urinary sphincter. J Urol 1991; 146: 1005–1006.
Gundian JC, Barrett DM, Parulkar BG . Mayo Clinic experience with use of the AMS800 artificial urinary sphincter for urinary incontinence following radical prostatectomy. J Urol 1989; 142: 1459–1961.
Furlow WL, Barrett DM . Recurrent or persistent urinary incontinence in patients with the artificial urinary sphincter: diagnostic considerations and management. J Urol 1985; 133: 792–795.
McGuire EJ, Wang C, Usistalo H, Savastano J . Modified pubovaginal sling in girl with myelodysplasia. J Urol 1986; 135: 94–96.
Gomley EA, Bloom DA, McGuire EJ, Ritchey MI . Pubovaginal slings for the management of urinary incontinence in female adolescentes. J Urol 1994; 152: 822–825.
Walker RD et al. Rectus fascial wrap: early results of a modification of the rectus fascial sling. J Urol 1995; 154: 771–774.
Kakizaki H et al. Fascial sling for the management of urinary incontinence due to sphincter incompetence. J Urol 1995; 153: 644–647.
Amundsen CL, Flynn BJ, Webster GD . Urethral erosion after synthetic and nonsynthetic pubovaginal slings: differences in management and continence outcome. J Urol 2003; 170: 134–137.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Siracusano, S., Ciciliato, S., Benedetto, P. et al. An unusual use of AMS 800 artificial urinary sphincter cuff in the treatment of sphincteric neurogenic incontinence: case report. Spinal Cord 42, 652–654 (2004). https://doi.org/10.1038/sj.sc.3101624
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101624