Abstract
Study Design: The 5 year review of patients referred to one center.
Objective: To report spinal cord infarction secondary to vascular occlusion from disease in a lower thoracic intervertebral foramen.
Method: The clinical and imaging findings of two cases with acute spinal cord dysfunction are presented.
Setting: Midlands Centre for Spinal Injuries, England.
Results: The CT and MR imaging features revealed lower thoracic unilateral foraminal occlusion due to acute facet joint septic arthritis in a diabetic patient, and secondary to chronic hypertrophic osteophytes in a second hypertensive individual. The presumed mechanism of infarction was occlusion of the artery of Adamkiewicz.
Conclusion: Foraminal disease in the lower thoracic levels needs to be entertained in cases of unexplained nontraumatic acute spinal cord dysfunction.
Similar content being viewed by others
Introduction
The vascular supply of the spinal cord depends on an anastomotic network that is particularly precarious in the lower thoracic spine as it largely relies on the artery of Adamkiewicz. Spinal cord ischaemia may be due to occlusion at the level of the intervertebral foramen that harbours this important blood vessel. The foraminal occlusion can result in or promote catastrophic cord infarction with profound irreversible neurological deficit.
A review of patient records over the last 5 years in the Midlands Centre for Spinal Injuries revealed two patients who presented acutely with spinal cord infarction associated with occlusive unilateral intervertebral foraminal disease.
Patient A
A 46-year-old man, insulin-dependant diabetic, presented with acute onset of low thoracic back pain, feeling unwell with intact neurology. He was admitted to a district general hospital urological ward and was treated for urinary tract infection. The next day his right lower limb became weak and by the fourth day he became completely paralysed in both lower limbs. Clinical examination showed chronic infection of the base of first right metatarsal.
Conventional radiography of the lumbar spine showed no evidence of significant vertebral disease.
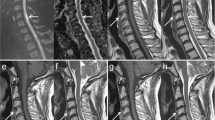
MR imaging of the thoracolumbar spine showed right T9/10 facet joint infection without any evidence of abscess formation. There was obliteration of the anatomical detail within the intervertebral foramen in keeping with soft tissue extension and oedema. There was no epidural abscess or cord compression. MR imaging showed the cord infarction and the changes in the facet joint and adjacent foramen. A CT scan of the area of pathology confirmed the articular destruction of facet joint (Figure 1). Blood culture showed Staphylococcus aureus as the infective organism.
Patient A (a) Sagittal T2 MR sequence showing extensive cord infarction in distal half of the cord (arrow). (b) Axial T1 MR image showing soft tissue inflammatory change within right half of T9/T10 neural canal with obliteration of fat planes. This is associated with destruction of right facet joint (arrow). (c) Axial CT showing destructive change of right T9/T10 joint extending into adjacent costovertebral joint due to infection (arrow)
Antibiotics according to sensitivity of the blood culture organism produced a good response. Weekly blood tests – complete blood count, E.S.R., C.R.P. showed that patient responded well. On discharge, 8 months after onset, he remained paralysed in both lower limbs.
Patient B
A 56-year-old lady, with well-controlled hypertension, presented with sudden onset of back pain radiating down to the legs while sedentary at home.
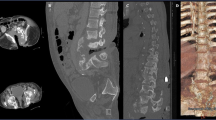
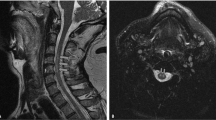
She gradually developed weakness in both lower limbs and retention of urine within 2 h. She was admitted to a district general hospital initially, and was subsequently transferred to a neighbouring hospital with better facilities for further management. MR imaging showed intrinsic cord signal changes at T10 without cord compression. Occlusion of the left T10/T11 foramen by osteophytic bony encroachment was seen on MR imaging and CT (Figure 2). Neurologically she presented with T10 complete paraplegia that showed no recovery. Lumbar puncture showed increase in protein, normal cell count, C.S.F immuno electrophoresis was negative and so was treponemal serology. Methylprednisolone was tried without improvement. Subsequently she was transferred to the Midlands Centre for Spinal Injuries for rehabilitation. Repeat MR imaging of the spinal cord showed atrophy at T11 level with a small area of cystic change, which is in keeping with a previous acute vascular insult. Clinically the patient remains completely paralysed in both lower limbs with incomplete sensory preservation below T10 to S5.
Discussion
The precarious nature of the blood supply of the spinal cord is well documented1 and this relies on an efficient anastomotic collateral circulation. The supply to the lower thoracic and lumbar cord along with the conus medullaris and filum terminale is supplemented by the artery of Adamkiewicz (great anterior medullary artery or great anterior radicular artery), which in the great majority of instances comes in at the lower thoracic and thoracolumbar level on the left-hand side. It is well acknowledged that this arterial anastomosis is suboptimal and critical, particularly in the lower thoracic levels.2, 3 It is understandable that at the levels where the major radicular arteries pass through the intervertebal foramina, foraminal disease can interfere with the blood supply to the cord accounting for some cases of ‘spontaneous spinal cord dysfunction.’
The location of the foraminal occlusive effect within the lower thoracic spine in our patients was felt to play a major role in the causation of spinal cord infarction. The effect of underlying diabetes mellitus (patient A) and hypertensive disease (patient B) could have been factors in predisposing to vascular insuffiency by direct involvement of the feeding main artery, or by limiting the potential for an adequate collateral circulation. In a postmortem study done on 50 cord specimens from patients with no previous symptoms of cord dysfunction, only five radicular vessels were found to be occluded out of a total of 777 radicular arteries examined angiographically and microscopically.4 On the one hand, this study suggests that asymptomatic occlusion is a rare event, but it also shows that occlusion of main radicular arteries can be present without cord infarction due to functional and structural changes in the collateral circulation. Arterial occlusion would need to be slow so as to allow the formation of an efficient collateral circulation. The acute pathological process in our first patient would not have provided sufficient time for the collateral circulation to develop. Although the osteophytic process in the second patient was undoubtedly slow in its formation, its thrombotic occlusive effects could still have developed acutely and not necessarily chronically. Pre-existing arterial disease was likely to have been present in both patients.
There are many medical and surgical causes for neurological deficit that need to be entertained as diagnostic possibilities in instances of acute paralysis.5, 6 Radiological investigation primarily by MRI and CT can exclude these possibilities and conclude that paralysis is due to spinal cord infarction. This is presumed to be spontaneous, if a direct cause is not identified. As the two cases we present indicate, it is vital to focus attention at intervetebral foraminal pathology as interference of the spinal cord blood supply can occur at foraminal level. Physicians need to be vigilant when a patient presents with neurological dysfunction and articular facet joint disease. Pre-existing diseases such as hypertension, diabetes mellitus and aortic aneurysm will predispose to spinal cord dysfunction if there is intraforaminal occlusion by different pathological processes. Even though the occlusion is at one foraminal level, the spinal cord infarction can be very extensive.
References
Peter L Williams (ed). Nervous system, Arterial blood supply of the Spinal Cord. In: Gray's Anatomy, 38th edn. Churchill Livingston: New York, 1995, pp 1218–1219.
Giovanni DiChiro MD, John Doppman MD, Ommaya A . Selective arteriography of arteriovenous aneurysms of spinal cord. Radiology 1967; 88: 1065–1077.
Djindjian R . Arteriography of the spinal cord. Am J Roentgenol 1969; 107: 461–478.
Maliszewski M et al. Occlusion of radicular arteries-reasons, consequences and anastomotic substitution pathways. Spinal Cord 1999; 37: 710–716.
Longmore M, Wilkinson I, Torok E . Oxford Handbook of Clinical Medicine, 5th edn. Oxford University Press: Oxford: 2001, p 341.
Kumar P, Clark M (eds). Clinical Medicine, 4th edn. W.B. Saunders: Edinburgh, 1998 Chapter 18, Table 18.47.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ram, S., Osman, A., Cassar-Pullicino, V. et al. Spinal cord infarction secondary to intervertebral foraminal disease. Spinal Cord 42, 481–484 (2004). https://doi.org/10.1038/sj.sc.3101583
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101583
Keywords
This article is cited by
-
Neurotoxicity Biomarkers as Potential Indicators of Spinal Cord Ischemia
Neuroscience and Behavioral Physiology (2019)
-
Spinal cord injury complicating a thoracolumbar selective nerve root block in a deformed spine: neurological and functional outcome
Spinal Cord (2015)
-
Relevance of the anatomical location of the Adamkiewicz artery in spine surgery
Surgical and Radiologic Anatomy (2011)
-
Spinal Cord Infarction with Multiple Etiologic Factors
Journal of General Internal Medicine (2007)