Abstract
The predictive power of B-type natriuretic peptide (BNP) and left ventricular ejection fraction (LVEF) is limited by its low specificity in patients with heart failure (HF). Discovery of more novel biomarkers for HF better diagnosis is necessary and urgent. ELABELA, an early endogenous ligand for the G protein-coupled receptor APJ (Apelin peptide jejunum, Apelin receptor), exhibits cardioprotective actions. However, the relationship between plasma ELABELA and cardiac function in HF patients is unclear. To evaluate plasma ELABELA level and its diagnostic value in HF patients, a total of 335 patients with or without HF were recruited for our monocentric observational study. Plasma ELABELA and Apelin levels were detected by immunoassay in all patients. Spearman correlation analysis was used to analyze the correlation between plasma ELABELA or Apelin levels and study variables. The receiver operating characteristic curves were used to access the predictive power of plasma ELABELA or Apelin levels. Plasma ELABELA levels were lower, while plasma Apelin levels were higher in HF patients than in non-HF patients. Plasma ELABELA levels were gradually decreased with increasing New York Heart Association grade or decreasing LVEF. Plasma ELABELA levels were negatively correlated with BNP, left atrial diameter, left ventricular end-diastolic diameter, left ventricular end-systolic diameter, and left ventricular posterior wall thickness and positively correlated with LVEF in HF patients. In contrast, the correlation between plasma Apelin levels and these parameters is utterly opposite to ELABELA. The diagnostic value of ELABELA, Apelin, and LVEF for all HF patients was 0.835, 0.673, and 0.612; the sensitivity was 62.52, 66.20, and 32.97%; and the specificity was 95.92, 67.23, and 87.49%, respectively. All these parameters in HF patients with preserved ejection fraction were comparable to those in total HF patients. Overall, plasma ELABELA levels were significantly reduced and negatively correlated with cardiac function in HF patients. Decreased plasma ELABELA levels may function as a novel screening biomarker for HF. A combined assessment of BNP and ELABELA may be a good choice to increase the accuracy of the diagnosis of HF.
Similar content being viewed by others
Introduction
Heart failure (HF) is recognized as a major clinical and global public health concern that affected nearly 64.3 million people worldwide in 20171. In particular, HF has been a leading cause of the high mortality and morbidity of cardiovascular diseases with an average annual mortality of 25–40% worldwide2. HF not only affects the elderly but also burdens the young population (< 50 years old) with a continuous rise in incidence3,4. It is vital to achieve early diagnosis and effective risk stratification to improve the management of HF patients. B-type natriuretic peptide (BNP) and left ventricular ejection fraction (LVEF) have been widely used in the diagnosis and prognosis of HF5. However, their predictive power was limited by their low specificity in clinical applications6,7. A combined assessment of BNP and other factors can improve HF diagnosis8. Thus, it is necessary and urgent to discover more novel biomarkers for HF diagnosis.
The Apelinergic system consists of a G protein-coupled receptor APJ (Apelin peptide jejunum, Apelin receptor, encoded by Aplnr)9 and two endogenous peptide ligands ELABELA (encoded by Apela, also called Toddler)10,11 and Apelin (encoded by Apln)12. The Apelinergic system significantly regulates cardiovascular homeostasis and functions as a potential therapeutic target of cardiovascular diseases13,14. Notably, the Apelin peptide could ameliorate acute HF by inhibiting endoplasmic reticulum stress15, ELABELA could protect against hypertensive-induced cardiac damage by inhibiting FoxM1/ACE signaling16 and improve left ventricular filling in cecal ligation puncture rats17. These results indicated the participation of Apelin and ELABELA in preventing HF. However, studies have indicated that ELABELA may be more efficient than Apelin18.
Accumulating evidence showed that Apelin and ELABELA exert similar important bioeffects, including cardiorenal protective action, anti-hypertension action, and positive inotropic effect14,18,19. As reported, the status of the plasma Apelin levels in HF patients is still controversial. Many studies have demonstrated decreased plasma Apelin levels20,21,22,23,24,25,26, while several other studies have indicated increased or unchanged plasma Apelin levels in HF patients27,28,29,30. Similarly, plasma ELABELA levels were markedly elevated in patients with myocardial infarction31,32 and complete atrioventricular block33 but reduced significantly in patients with congenital heart disease34 and atrial fibrillation35,36. Plasma ELABELA levels were also decreased in patients with hypertension37 and renal impairment38. Of note, hypertension and renal impairment are two independent risk factors for HF progression39,40, implying the potential biomarker function of ELABELA for HF. However, only one small cohort study indirectly demonstrated the correlation between plasma ELABELA and cardiac function in HF patients41. The levels of plasma ELABELA were significantly decreased in hypertensive patients with HF compared to those in hypertensive patients without HF41. In the present study, with the maximum exclusion of interference from other complications, we further evaluated the plasma ELABELA and Apelin levels and investigate the association between plasma ELABELA or Apelin levels and cardiac function in HF patients. Additionally, we also compared the diagnostic value of ELABELA, Apelin, and LVEF in HF patients.
Methods
Study population
The studies involving human participants were reviewed and approved by the Ethics Committee of the Affiliated Hospital of the Jiangxi University of Chinese Medicine (JZFYLL20230208002) and performed in accordance with the World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. All individual patients/participants provided their written informed consent and clinical characteristics to participate in this study at enrollment. All subjects were recruited in the Department of Cardiology, Affiliated Hospital of Jiangxi University of Chinese Medicine, between December 2022 and July 2023 and divided into Non-HF and HF groups. All the laboratory assessments, except plasma ELABELA and Apelin levels, were conducted in the clinical laboratory center according to the standard protocols. Inclusion criteria for diagnosis and classification of HF, including (1) typical signs (i.e., dyspnea), (2) typical symptoms (i.e., pulmonary rales), (3) increased plasma brain natriuretic peptide (BNP) concentrations [> 95 pg/ml according to the New York Heart Association (NYHA) functional classification.], (4) ultrasound cardiogram report (impaired cardiac function evaluated by echocardiography), and (5) X-ray examination (i.e., enlarged heart shadow) were based on the 2021 ESC Guidelines for the diagnosis and treatment of HF5. Heart failure with preserved EF (HFpEF), mid-range EF (HFmrEF), and reduced ejection fraction (HFrEF) was defined as EF ≥ 50%, > 40 but < 50, and ≤ 40%, respectively5. The exclusion criteria were: (1) heart diseases (i.e., atrial fibrillation, congenital heart disease, acute myocardial infarction, cardiomyopathy), (2) severe renal dysfunction (grade 4 or higher), (3) malignant tumor, (4) inferior airway diseases (i.e., acute pulmonary embolism, severe disease of lung parenchyma), (5) autoimmune related diseases (i.e., severe infection, autoimmune disease, autoimmune deficiency disease), and (6) acute stroke. In this regard, on the premise of following the inclusion and exclusion criteria, patients from the Department of Cardiology with plasma BNP concentrations ≥ 95 pg/ml were included in the HF group and patients without symptoms and signs of HF with plasma BNP concentrations < 95 pg/ml were included in the Non-HF group. All of the patients/participants did not receive the optimized treatment before collecting blood samples.
ELISA assays for plasma ELABELA and Apelin
All the fasting blood samples were collected from a peripheral vein of all patients within 24 h of admission. Upon collection, blood samples were immediately centrifuged for 5 min at 4 °C and 3000 rpm to separate plasma. The plasma samples were stored at − 80 °C for ELABELA and Apelin analysis by ELISA using the commercialized human ELABELA ELISA Kit (S-1508, Peninsula Laboratories International, Inc. USA) and Apelin ELISA kit (E01T0015, Bluegene Tech Inc., Shanghai, China) according to the manufacturers’ instructions, respectively. For the measurement of plasma ELABELA, the plasma samples were appropriately extracted.
Statistical analysis
Continuous data were expressed as mean ± standard deviation (SD) for normally distributed data, median and interquartile range (IQR) for non-normally distributed data, and categorical variables as number and percentage. Student’s t-test was used for intergroup differences in continuous normally distributed variables between two groups, one-way analysis of variance followed by Bonferroni comparisons and unpaired tests was used for continuous normally distributed variables among more than two groups. Spearman correlation analysis was used to correlate plasma ELABELA or Apelin levels and study variables. The clinical characteristics associated with HF were analyzed through univariate and multivariate logistic regression in all subjects. The diagnostic value of plasma ELABELA, Apelin, and LVEF was assessed by determining the area under the receiver operating characteristic (ROC) curves (AUC) using the DeLong test. All tests were two-sided, and P < 0.05 was considered statistically significant. The statistical analyses were performed using MedCalc Version 22.017 (MedCalc Software Ltd, Ostend, Belgium).
Ethics approval
The studies involving human participants were reviewed and approved by the Affiliated Hospital of the Jiangxi University of Chinese Medicine (JZFYLL20230208002). The patients/participants provided written informed consent to participate in this study.
New and noteworthy
The predictive power of BNP and LVEF is limited by its low specificity in patients with HF. We reported that plasma ELABELA was significantly reduced and negatively correlated with cardiac function in HF patients, utterly opposite to the changes in plasma BNP and Apelin. Plasma ELABELA might be superior to Apelin and LVEF for the diagnosis and prognosis of HF, at least in patients with HFpEF. Combined assessment of BNP and ELABELA may provide potential benefits for the diagnosis of HF.
Results
The baseline characteristics of patients
A total of 335 participants with and without HF were enrolled in the Non-HF group (n = 119, 68.4 ± 12.2 years) and the HF group (n = 216, 69.6 ± 11.6 years, p = 0.176 vs. Non-HF group), respectively; the other baseline clinical characteristics are shown in Table 1. There were no significant differences in sex, body mass index (BMI), comorbidities, or blood pressure between the two groups. For complications, the incidence of coronary heart disease was higher in the HF than in the Non-HF group (22.2 vs. 16.8%, p = 0.047). Data from laboratory examinations revealed that plasma BNP, creatinine, urea nitrogen, uric acid, and low-density lipoprotein cholesterol (LDL-c) levels were all higher in the HF group compared to the non-HF group (P < 0.05). In contrast, the plasma total cholesterol and triglyceride levels were lower in the HF group compared to the non-HF group (P < 0.05). Compared to the non-HF group, the HF group showed lower left ventricular ejection fraction (LVEF) and higher left atrial diameter (LAD), left ventricular end-diastolic diameter (LVEDd), left ventricular end-systolic diameter (LVEDs), and left ventricular posterior wall (LVPW) thickness (p < 0.05), with no significant difference in interventricular septum thickness (IVST) and right ventricular internal dimension diameter (RVIDd) between non-HF and HF groups.
Plasma BNP levels in patients with HF and without HF
Plasma BNP levels were higher in HF patients than in non-HF groups (Table 1). We further divided the 216 HF patients into four subgroups [NYHA I (57/216), II (32/216), III (39/216), and IV (88/216)] according to the classification of NYHA, or HFpEF (191/216), HFmrEF (15/216), and HFrEF (10/216) groups determined by LVEF. Plasma BNP levels were further increased with severity stratified by NYHA grade (Table 2) and the continuous reduction of LVEF (Table 3), and a similar gradient reduction of LVEF was observed in patients in both classification models.
Plasma ELABELA levels in patients with HF and without HF
The levels of plasma ELABELA in HF patients were significantly lower than those in non-HF groups (7.3 ± 3.9 vs. 13.7 ± 3.0 ng/ml, p < 0.001, Fig. 1A). They were further significantly reduced with severity stratified by NYHA grade (NYHA I 12.3 ± 3.5 vs. NYHA II 9.9 ± 2.8 vs. NYHA III 7.7 ± 4.0 vs. NYHA IV 5.6 ± 3.9 ng/ml) (Table 2). Interestingly, the mean plasma ELABELA levels of the HFpEF, HFmrEF, and HFrEF groups were significantly lower than in the non-HF group. The plasma ELABELA levels in HFpEF (8.8 ± 4.5 ng/ml), HFmrEF (6.3 ± 4.7 ng/ml), and HFrEF (4.6 ± 3.0 ng/ml) groups were decreased sequentially with statistical significance (Table 3).
Plasma Apelin levels in patients with HF and without HF
Plasma Apelin levels were higher in HF patients than in non-HF groups (116.5 ± 16.8 vs. 27.2 ± 11.3 ng/ml, p < 0.001, Fig. 1B) and in HF patients with NYHA II, III, and IV grade than in non-HF groups with no significant difference between non-HF and NYHA I patients (Table 2). The severity stratified by NYHA grade (Table 2) or LVEF levels (Table 3) did not affect the plasma levels of Apelin in HF patients.
Correlation between ELABELA or Apelin and study variables
We further analyzed the correlation between ELABELA or Apelin and study variables in all subjects (Table 4). BNP levels (r = − 0.704, p < 0.001), creatine levels (r = − 0.235, p < 0.001), urea nitrogen levels (r = − 0.284, p < 0.001), uric acid levels (r = − 0.110, p = 0.045), LAD (r = -0.265, p < 0.001), LVEDd (r = − 0.231, p < 0.001), LVEDs (r = − 0.223, p < 0.001), LVPW (r = − 0.167, p = 0.002), NYHA function grade (r = − 0.700, p < 0.001) were negatively related to plasma ELABELA levels. In contrast, diastolic blood pressure (r = 0.164, p = 0.003), mean arterial pressure (r = 0.117, p = 0.033), LDL-c levels (r = 0.134, p = 0.014), HDL-c levels (r = 0.126, p = 0.021), total cholesterol levels (r = 0.207, p < 0.001), total cholesterol levels (r = 0.207, p < 0.001), triglyceride levels (r = 0.164, p = 0.003) and LVEF (r = 0.183, p = 0.001) positively correlated to plasma ELABELA levels (Table 4).
In contrast, coronary artery disease (r = 0.175, p = 0.001), BNP levels (r = 0.336, p < 0.001), urea nitrogen levels (r = 0.138, p = 0.011), LAD (r = 0.295, p < 0.001), LVEDd (r = 0.213, p < 0.001), LVEDs (r = 0.187, p = 0.001), IVST (r = 0.135, p = 0.013), LVPW (r = 0.108, p = 0.048), NYHA function grade (r = 0.365, p < 0.001) were positively related to plasma Apelin levels, while LVEF (r = − 0.144, p = 0.037) negatively correlated to plasma Apelin levels (Table 4). Furthermore, plasma ELABELA levels were negatively correlated to plasma Apelin levels (r = − 0.229, p < 0.001).
Furthermore, multiple linear regression analyses in all the participants were performed to determine the relationship between plasma ELABELA levels and plasma Apelin levels and clinical characteristics associated with HF (Table 5). We found a significant association between plasma ELABELA levels and diastolic blood pressure (β = 0.096, t = 2.611, p = 0.009), plasma BNP levels (β = − 0.001, t = − 8.127, p < 0.001), and LAD (β = − 0.096, t = − 2.521, p = 0.012), while plasma Apelin levels were only associated with LAD (β = 5.775, t = 2.653, p = 0.008).
Baseline clinical characteristics of patients with different levels of ELABELA or Apelin
We further divided all the HF patients into two groups, the high-ELABELA-level group, and the low-ELABELA-level group, or the high-Apelin-level group and the low-Apelin-level group (Table 6). The low-ELABELA-level group exhibited more male patients (56.4 vs. 43.5%, p = 0.006), lower diastolic blood pressure (73.4 ± 9.6 vs. 77.8 ± 10.0 mmHg, p = 0.001), lower mean arterial pressure (91.2 ± 11.3 vs. 95.3 ± 11.3 mmHg, p = 0.009), higher BNP levels [2745.7 (127.0, 27,753.0) vs. 830.7 (96.2, 10,362.0) pg/ml, p < 0.001], lower creatine levels [67.2 (57.8,82.4) vs. 69.6 (56.2, 81.5) μmol/l, p = 0.001], higher urea nitrogen levels [9.4 (3.0, 47.9) vs. 7.0 (2.9, 69.2) μmol/l, p = 0.010], and lower ELABELA levels (4.7 ± 2.4 vs. 12.1 ± 2.9 ng/ml, p < 0.001) than those in the high-ELABELA-level group. Echocardiographic data indicated that the low-ELABELA-level group had lower LVEF (58.6 ± 9.8 vs. 62.4 ± 6.9%, p = 0.001) and longer LAD (38.1 ± 8.4 vs. 34.3 ± 5.1 mm, p < 0.001), LVEDd (48.6 ± 8.2 vs. 45.4 ± 4.7 mm, p < 0.001), LVEDs (33.2 ± 8.3 vs. 29.9 ± 4.0 mm, p < 0.001), and LVPW (9.8 ± 1.3 vs. 9.4 ± 1.3 mm, p < 0.001) than the high-ELABELA-level group, indicating the worse left ventricular systolic function and larger atrial and ventricular chambers in the low-ELABELA-level group. Moreover, the low-ELABELA-level group had fewer NYHA I patients (2.8 vs. 50.0%, p < 0.001) and more NYHA III (24.1 vs. 12.0%, p < 0.001) and NYHA IV (62.0 vs. 19.4%, p < 0.001) patients than the high-ELABELA-level group.
In contrast, Low-Apelin-level group exhibited lower heart rate (75.6 ± 8.3 vs. 79.2 ± 9.0 bpm, p = 0.002), higher ELABELA levels (9.2 ± 4.5 vs 7.6 ± 4.5 ng/ml, p = 0.010), and lower Apelin levels (26.7 ± 9.0 vs. 278.8 ± 36.2 pg/ml, p < 0.001) than those in high-Apelin-level group. Echocardiographic data indicated that the low-Apelin-level group had higher LVEF (62.3 ± 6.5 vs. 58.8%, p = 0.003) and shorter LAD (34.4 ± 5.3 vs. 38.1 ± 8.3 mm, p < 0.001), LVEDd (45.5 ± 5.0 vs. 48.5 ± 8.1 mm, p < 0.001), LVEDs (30.0 ± 4.3 vs. 33.1 ± 8.2 mm, p < 0.001), IVST (9.7 ± 0.9 vs. 10.0 ± 1.3 mm, p = 0.045), and LVPW (9.4 ± 1.0 vs. 9.8 ± 1.5 mm, p = 0.006) than the high-Apelin-level group, indicating the worse left ventricular systolic function and larger atrial and ventricular chambers in the high-Apelin-level group. Moreover, the low-Apelin-level group had more NYHA I patients (37.0 vs. 15.7%, p < 0.001) and fewer NYHA III (12.0 vs. 24.1%, p < 0.001) and NYHA IV (34.3 vs. 47.2%, p = 0.006) patients than the high-Apelin-level group.
Diagnostic value of ELABELA and Apelin level for HF
Using univariate logistic regression analysis and multivariate logistic regression analysis, we further investigated the clinical characteristics associated with HF, which may be the underlying risk factor for HF development (Table 7). In univariate analysis, plasma BNP levels (OR 1.023, 95% CI 1.004–1.025, P = 0.003), plasma Apelin levels (OR 1.005, 95% CI 1.002–1.009, P = 0.004), plasma ELABELA levels (OR 0.731, 95% CI 0.666–0.801, P < 0.001), and LAD (OR 1.088, 95% CI 1.011–1.172, P = 0.025) were closely associated with the occurrence of HF. In multivariate analysis, plasma BNP levels (OR 1.008, 95% CI 1.006–1.012, P = 0.002), plasma Apelin levels (OR 1.015, 95% CI 1.003–1.017, P = 0.001), plasma ELABELA levels (OR 0.722, 95% CI 0.658–0.791, P < 0.001), and LAD (OR 1.098, 95% CI 1.021–1.181, P = 0.012) were associated with the occurrence of HF. These results indicated that reduced ELABELA or increased Apelin levels may be an underlying risk factor for HF progression.
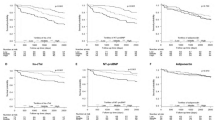
To analyze the diagnostic value of ELABELA and Apelin, ROC curves were plotted for data for all Non-HF and HF patients (Table 8 and Fig. 2), and a pairwise comparison of ROC curves was performed by using the DeLong test (Table 9). For the total HF patients (Fig. 2A), the AUC area of ELABELA, Apelin, and LVEF was 0.835 ± 0.021 (95% CI 0.790–0.873), 0.673 ± 0.030 (95% CI 0.620–0.723), and 0.612 ± 0.031 (95% CI 0.557–0.664). The optimal cut-off point was 9.87 ng/ml (sensitivity 62.50%, specificity 94.96%), 36.75 pg/ml (sensitivity 66.20%, specificity 67.23%), and 59% (sensitivity 32.87%, specificity 87.39%), respectively. Using the DeLong test, there is a significant difference between the AUC values of ELABELA and that of both LVEF (∆AUC 0.223 ± 0.036, 95% CI 0.151–0.294, P < 0.001) and Apelin (∆AUC 0.162 ± 0.037, 95% CI 0.089–0.234, P < 0.001). For the HFpEF patients (Fig. 2B), the AUC area of ELABELA, Apelin, and LVEF was 0.817 ± 0.023 (95% CI 0.772–0.863), 0.653 ± 0.032 (95% CI 0.591–0.715), and 0.561 ± 0.033 (95% CI 0.497–0.626). The optimal cut-off point was 9.86 ng/ml (sensitivity 59.22%, specificity 95.82%), 36.81 pg/ml (sensitivity 62.84%, specificity 67.22%), and 59.52% (sensitivity 24.18%, specificity 87.40%), respectively. However, there is a significant difference between the AUC values of ELABELA and that of both LVEF (∆AUC 0.256 ± 0.040, 95% CI 0.177–0.335, P < 0.001) and Apelin (∆AUC 0.165 ± 0.039, 95% CI 0.088–0.242, P < 0.001) in the HFpEF patients. Thus, the diagnostic values of ELABELA were significantly higher than that of Apelin or LVEF, while there is no difference between the diagnostic values of Apelin and that of LVEF in the total or HFpEF patients.
For the NYHA I patients (Fig. 2C), the AUC area of ELABELA, Apelin, and LVEF was 0.639 ± 0.045 (95% CI 0.563–0.709), 0.527 ± 0.048 (95% CI 0.451–0.603), and 0.531 ± 0.047 (95% CI 0.454–0.606). The optimal cut-off point was 12.72 ng/ml (sensitivity 68.42%, specificity 58.82%), 65.66 pg/ml (sensitivity 31.68%, specificity 78.25%), and 63.69% (sensitivity 50.98%, specificity 57.14%), respectively. However, there is no significant difference between the AUC values of ELABELA and that of both LVEF (∆AUC 0.108 ± 0.064, 95% CI − 0.017–0.233, P = 0.090) and Apelin (∆AUC 0.111 ± 0.067, 95% CI 0.021–0.243, P = 0.099) in the NYHA I patients. For the NYHA II patients (Fig. 2D), the AUC area of ELABELA, Apelin, and LVEF was 0.822 ± 0.046 (95% CI 0.751–0.879), 0.636 ± 0.060 (95% CI 0.554–0.712), and 0.531 ± 0.063 (95% CI 0.449–0.613), and the optimal cut-off point was 10.11 ng/ml (sensitivity 65.62%, specificity 89.92%), 30.08 pg/ml (sensitivity 68.85%, specificity 60.50%), and 59.52% (sensitivity 28.12%, specificity 87.49%), respectively. A significant difference was found between the AUC values of ELABELA and that of both LVEF (∆AUC 0.290 ± 0.078, 95% CI 0.138–0.442, P < 0.001) and Apelin (∆AUC 0.186 ± 0.082, 95% CI 0.025–0.347, P = 0.024) in the NYHA II patients. For the NYHA III patients (Fig. 2E), the AUC area of ELABELA, Apelin, and LVEF was 0.871 ± 0.040 (95% CI 0.809–0.919), 0.766 ± 0.047 (95% CI 0.693–0.830), and 0.643 ± 0.055 (95% CI 0.563–0.717), and the optimal cut-off point was 20.96 ng/ml (sensitivity 79.57%, specificity 85.76%), 39.29 pg/ml (sensitivity 84.62%, specificity 68.17%), and 59.52% (sensitivity 38.56%, specificity 87.49%), respectively. There is a significant difference between the AUC values of ELABELA and that of LVEF (∆AUC 0.228 ± 0.065, 95% CI 0.101–0.356, P = 0.001) but not Apelin (∆AUC 0.105 ± 0.064, 95% CI − 0.021–0.231, P = 0.103) in the NYHA III patients. For the NYHA IV patients (Fig. 2F), the AUC area of ELABELA, Apelin, and LVEF was 0.950 ± 0.017 (95% CI 0.911–0.975), 0.741 ± 0.036 (95% CI 0.676–0.799), and 0.680 ± 0.039 (95% CI 0.612–0.743). The optimal cut-off point of ELABELA, Apelin, and LVEF was 9.88 ng/ml (sensitivity 82.19%, specificity 95.48%), 39.40 pg/ml (sensitivity 79.57%, specificity 68.13%), and 59.52% (sensitivity 41.03%, specificity 87.49%), respectively. A significant difference was also detected between the AUC values of ELABELA and that of both LVEF (∆AUC 0.270 ± 0.043, 95% CI 0.186–0.353, P < 0.001) and Apelin (∆AUC 0.209 ± 0.038, 95% CI 0.135–0.284, P = 0.024) in the NYHA IV patients. In contrast with ELABELA, no significant difference was detected between the AUC values of Apelin and that of LVEF in HF patients regardless of the severity stratified by NYHA grade. Additionally, A significant difference was found between the AUC values of Apelin and that of ELABELA only in the NYHA II and NYHA IV patients. Thus, the diagnostic values of ELABELA, Apelin, and LVEF were associated with the classification of NYHA. In particular, the diagnostic values of ELABELA were increased with the severity stratified by NYHA grade and higher than that of Apelin and LVEF.
Discussion
The present study aimed to investigate the potential diagnostic value of plasma ELABELA in HF patients compared to LVEF and Apelin. Our data have demonstrated that plasma ELABELA was significantly reduced and correlated with increasing NYHA grade or decreasing LVEF, utterly opposite to the changes in plasma BNP. On the contrary, plasma Apelin was significantly elevated but was not affected by the severity stratified by NYHA grade, the reduction of LVEF, or the sustained increase of plasma BNP in HF patients. We found that the levels of plasma ELABELA were negatively associated with LAD, LVEDd, LVEDs, LVPW, and plasma BNP and positively correlated with LVEF. In contrast, the correlation between plasma Apelin levels and these parameters was utterly opposite to that of plasma ELABELA. Moreover, although the differences in sensitivity between ELABELA and Apelin or LVEF for the diagnosis of HF depend on the specific NYHA grade, the diagnostic values and specificity of plasma ELABELA level for HF were higher than those of plasma Apelin and LVEF. Thus, reduced plasma ELABELA level may be a novel promising diagnostic indicator for HF patients. These findings may guide the use of ELABELA as a screening indicator for HF patients and call for further preclinical and clinical evaluation of the cardioprotective property of ELABELA in the setting of HF and the underlying mechanisms.
Although several studies have demonstrated an increase in plasma Apelin levels in NYHA II and III HF patients27,42, some other studies have reported a significant downregulation in plasma Apelin levels in HF21,22,24,43 and atrial fibrillation (AF)44 patients. Here we also found an elevated plasma Apelin level in HF patients. The reasons for these discrepancies are unclear but could be related to the difference in the study population and/or the testing methods (especially the differences in Apelin ELISA kits). Nevertheless, these studies implied a close correlation between plasma Apelin and the pathogenesis of HF. Indeed, Apelin exhibited a cardioprotective action in dilated cardiomyopathy45 and HF15,46 in animals. Due to the similar bioeffects with Apelin, ELABELA also exhibited similar cardiovascular-protective actions18,19. The current study demonstrated that plasma ELABELA levels were significantly reduced with the severity stratified by NYHA grade or decreasing LVEF in HF patients compared with non-HF patients. Although a previous study by Ma et al. has demonstrated the declined plasma ELABELA levels in hypertensive patients with HF41, preliminary indicating the status of plasma ELABELA in HF patients. However, they cannot rule out the interference from other complications, including hypertension and renal impairment. What's more, previous reports have already shown that plasma ELABELA concentrations were increased in patients with coronary heart diseases31,32,33 but reduced in patients with congenital heart disease34, renal impairment38, hypertension37, and AF35, indicating the independent impact of these complications on plasma ELABELA levels. As an extension, our study excluded the influence of the above complications and demonstrated the association of the declined plasma ELABELA levels with a high risk of HF progression. In this regard, patients with lower circulating ELABELA exhibited more severe cardiac dysfunction than those with higher circulating ELABELA. In addition, our study also showed that ELABELA was also positively related to, while Apelin had a negative correlation with (no significant statistical significance) plasma LDL-c, HDL-c, cholesterol, and triglyceride. These results indicated that ELABELA might be similar to Apelin in participating in metabolic regulation or metabolic related diseases such as atherosclerosis47,48,49. Recently, a small cohort study has shown that plasma ELABELA levels were negatively associated with carotid intima-media thickness in hypertensive patients, indicating the potential involvement of reduced ELABELA in the pathogenesis of hypertension-associated subclinical atherosclerosis50. It is important to note that atherosclerosis is considered to be the main cause of most cardiovascular diseases worldwide, with ischemic heart disease as its main clinical manifestation51. Thus, these pieces of evidence further support the potential importance of the declined circulating ELABELA in HF pathophysiology. However, the relationship between ELABELA and the progression of atherosclerosis needs to be further clarified.
We further compared plasma levels of ELABELA versus Apelin in different types of HF. Interestingly, plasma levels of ELABELA gradually decreased with increasing NYHA grade. In contrast, plasma Apelin levels were initially elevated in NYHA II patients compared to non-HF and NYHA I patients and then slightly decreased in NYHA III and IV patients compared to NYHA II patients with no statistical significance. Similarly, plasma ELABELA levels in the HF patients with HFpEF, HFrEF, or HFmrEF were sequentially decreased and lower than that in the non-HF patients. In contrary, The HF patients with HFpEF, HFrEF, or HFmrEF had higher plasma Apelin levels than non-HF patients. Interestingly, neither plasma Apelin levels between the HFpEF and HFmrEF or HFrEF group nor between HFmrEF and HFrEF group showed notable differences. These results indicated that decreased ELABELA level is more closely associated with impaired left ventricular systolic function than Apelin. There is no relationship between plasma Apelin levels and cardiac function. Notably, worsened heart function has been known as an independent risk factor for adverse events in HF patients52. Thus, the reduced plasma ELABELA levels rather than elevated plasma Apelin levels may be connected to adverse events in HF patients. Although studies have reported the positive inotropic effects and anti-myocardial fibrosis actions of ELABELA and Apelin14,16,17,53, ELABELA exhibited more effectively improving left ventricular filling in rats with cecal ligation puncture-induced sepsis17, achieve pronounced effects on cardiac contractions54, and reduce blood pressure and improve cardiorenal dysfunctions in spontaneously hypertensive rats55. The positive inotropic effect of Apelin was not matched to the elevated plasma Apelin levels in patients with HF. The reasons for this are not yet clear. However, we speculate that the increased plasma Apelin levels may be a compensation to the reduced plasma ELABELA levels and contribute to the alleviation of HF. This is supported by the observation that plasma Apelin levels were negatively correlated to plasma ELABELA levels in HF patients in our study.
HFpEF is recognized as a heterogeneous clinical syndrome and accounts for at least 50% of all HF patients56. However, the diagnosis of HFpEF is still challenging. In this regard, the European Society of Cardiology (ESC) has offered a complex definition of HFpEF which includes the symptoms and signs of HF, with evidence of structural and/or functional cardiac abnormalities and/or raised natriuretic peptides, and with an LVEF more than 50%57. Similarly, clinicians in clinical practice have adopted another definition of HFpEF which includes an LVEF more than 40%, an elevated N-terminal pro-BNP (NT-proBNP) level, and a structural cardiac abnormality on echocardiography57. Of note, approximately 20% of HFpEF patients with have normal natriuretic peptide levels58 and guidelines use the combination of LVEF ≥ 50% with functional abnormality assessment with tissue Doppler imaging to diagnose HFpEF57. Thus, the diagnosis of HFpEF is more difficult than that of HFmrEF or HFrEF and there is still no simpler definition specifying the use of a combination of imaging or natriuretic peptides in the diagnosis of HFpEF. In the present study, the great majority of the HF patients were diagnosed with HFpEF (88.43%), the percentages of the HFmrEF and HFrEF patients were only 6.94% and 4.62%, respectively. The diagnostic value and specificity of plasma ELABELA in patients with HFpEF were comparable with that in All HF patients and significantly higher than those of Apelin or LVEF. This may suggest the diagnostic potential of the decreased ELABELA level when combined with an elevated BNP level and LVEF ≥ 50% for HFpEF patients. Although it is clear that ventricular diastolic dysfunction plays a key role in HFpEF progression59, diastolic dysfunction is not synonymous with HFpEF but considered as a part of the normal again process56. In this case, the benchmarking to LVEF is not used for the diagnosis of HFpEF in a meaningful manner. The determination of the diagnosis value of plasma ELABELA on HFpEF may be compensate for the shortcomings of LVEF. In addition, multiple non-diastolic abnormalities including diabetes, obesity, chronic kidney disease, and hypertension are risk factors for HFpEF56. However, the occurrence of diabetes, obesity, chronic kidney disease, and hypertension was very low in the present cohort. This may be related to the specific subtypes of HFpEF. Indeed, a clinical phenotypic classification of HFpEF has already reported, mainly including (1) Vascular–related HFpEF; (2) Cardiomyopathy-related HFpEF; (3) Right heart- and pulmonary-related HFpEF; (4) Valvular- and rhythm-related HFpEF; and (5) Extracardiac disease-related HFpEF60. Along this line, our data may indicate that the HFpEF patients in the cohort mainly belong to cardiomyopathy-related HFpEF or valvular- and rhythm-related HFpEF. Briefly, patients with HFpEF in the present cohort may be mainly caused by valvular heart disease and old myocardial infarction.
The various bioeffects of ELABELA or Apelin display important roles in HF development. We found that plasma ELABELA levels rather than Apelin levels were positively correlated with diastolic blood pressure and negatively correlated with plasma creatine and urea nitrogen. Chronic kidney disease and hypertension are closely associated with HF and are known as independent risk factors for HF progression 39,40,61. Hypertension or chronic kidney disease interacts with HF, which jointly deteriorates the patient’s physical condition. Increasing animal studies have demonstrated that peripheral ELABELA administration exhibits an antagonistic actions on multiple cardiovascular-related diseases including hypertension62,63 and kidney injury64,65. Moreover, the levels of plasma ELABELA were remarkably lower and significantly negatively correlated with albuminuria, systolic and diastolic blood pressure in patients with type 2 diabetes38 or essential hypertension37. Therefore, reduced circulating ELABELA levels might cause the elevation of the incidence of HF progression through hypertension or renal dysfunction. Along this line, ELABELA may be a potential therapeutic target/drug for HF. This assumption may be supported by the evidence from multiple animal studies that have already demonstrated the protective actions of peripheral ELABELA application on cardiac injury including ischemia/reperfusion injury, oxidative stress injury, hypertensive injury, and myocardial infarction18. However, there is currently a lack of direct clinical evidence for the therapeutic efficacy of ELABELA for HF patients, which awaits future clinical evaluation.
NT-proBNP and BNP, known as diagnostic indicators of HF66,67, were associated with the severity and mortality of HF68 and important predictors for adverse events in HF patients69. Plasma ELABELA was significantly negatively associated with plasma BNP, while plasma Apelin was markedly positively related to plasma BNP in the present study. The negative relationship between ELABELA and BNP suggested that ELABELA protects against HF, possibly via its positive inotropic effect and attenuating cardiac remodeling. While the positive correlation between Apelin and BNP may be a compensatory outcome of reduced plasma ELABELA that enhances inotropic action and abolishes cardiac remodeling, thus exerting an anti-HF effect. Along this line, we found that the correlations between plasma ELABELA and cardiac function-related parameters (LVEF, LAD, LVEDd, LVEDs, IVST, LVPW, and RVIDd assessed by electrocardiography) were opposite to that between plasma Apelin and the above indexes. Unfortunately, both BNP and LVEF have poor predictive power for HF due to their low specificity6,7. Our results indicated that decreased ELABELA level might be a novel promising screening indicator for HF. In the present study, multivariate linear regression analysis revealed that plasma BNP only exhibited a significant negative impact on plasma ELABELA levels but not plasma Apelin levels. Thus, declined ELABELA plasma levels might be an underlying risk factor for HF progression and a potential predictor of a worse prognosis for HF. This concept can be supported by the multiple protective effects of ELABELA, including antihypertensive, cardioprotective, and renoprotective effects18,19. Similar to previous reports27,41, compared to ELABELA, the LVEF had a lower diagnostic value for HF with a lower predictive sensitivity and a comparable predictive specificity. Notably, although the predictive sensitivity of plasma ELABELA for the diagnosis of HF is comparable to that of plasma Apelin, plasma ELABELA had a higher diagnostic value and predictive specificity than plasma Apelin. Therefore, ELABELA might be superior to Apelin and LVEF for the diagnosis and prognosis of HF. Combined assessment of BNP and ELABELA may provide potential benefits for the diagnosis of HF.
The present study has several limitations. First, the current study population included only subjects from a single center. Thus, our findings may not be suitable for all ordinary populations due to the sample selection bias, including population and region bias. However, our findings are at least applicable to Chinese patients. Second, the sample size was small, which may reduce the reliability of the subgroup analysis. Third, the data was only dependent on the ELABELA/Apelin ELISA assay, the method is limited by the specificity of the antibody used in the ELISA kit. Fourth, patients in HF and non-HF groups were included based on typical signs, symptoms, and plasma BNP concentrations, with a lacking of a healthy control group or an HF group of different origins, such as patients with ischemic HF. It is still unclear whether there are differences in the levels of plasma ELABELA between healthy individuals and HF patients of matched age or HF of different origins. Lastly, follow-up studies were not conducted and outcome data are not available. The correlation between ELABELA and major outcomes including hospitalization, readmission, and all-cause mortality due to HF in our cohort is unclear. Therefore, future longitudinal multicenter clinical studies with a larger sample size and a healthy control cohort or an HF cohort of different origins are necessary to further verify the effectiveness of ELABELA in clinical diagnostic practice.
Data availability
The raw data supporting the conclusions of this article will be made available by Dr. Chuanming Xu without undue reservation.
References
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392: 1789–1858, (2018).
Ezekowitz, J. A., Kaul, P., Bakal, J. A., Quan, H. & McAlister, F. A. Trends in heart failure care: has the incident diagnosis of heart failure shifted from the hospital to the emergency department and outpatient clinics?. Eur. J. Heart Fail. 13, 142–147 (2011).
Groenewegen, A., Rutten, F. H., Mosterd, A. & Hoes, A. W. Epidemiology of heart failure. Eur. J. Heart Fail. 22, 1342–1356 (2020).
Lecoeur, E., Domeng, O., Fayol, A., Jannot, A. S. & Hulot, J. S. Epidemiology of heart failure in young adults: A French nationwide cohort study. Eur. Heart J. 44, 383–392 (2023).
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A, ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC). With the special contribution of the heart failure association (HFA) of the ESC. Eur. J. Heart Fail. 24, 4–131 (2022).
Oremus, M. et al. A systematic review of BNP and NT-proBNP in the management of heart failure: Overview and methods. Heart Fail. Rev. 19, 413–419 (2014).
Shiraishi, Y. et al. Improved prediction of sudden cardiac death in patients with heart failure through digital processing of electrocardiography. Europace 25, 922–930 (2023).
Han, L. et al. Combined assessment of relaxin and B-type natriuretic peptide improves diagnostic value in patients with congestive heart failure. Am. J. Med. Sci. 354, 480–485 (2017).
O’Dowd, B. F. et al. A human gene that shows identity with the gene encoding the angiotensin receptor is located on chromosome 11. Gene 136, 355–360 (1993).
Chng, S. C., Ho, L., Tian, J. & Reversade, B. ELABELA: A hormone essential for heart development signals via the apelin receptor. Dev. Cell 27, 672–680 (2013).
Pauli, A. et al. Toddler: an embryonic signal that promotes cell movement via Apelin receptors. Science 343, 1248636 (2014).
Tatemoto, K. et al. Isolation and characterization of a novel endogenous peptide ligand for the human APJ receptor. Biochem. Biophys. Res. Commun. 251, 471–476 (1998).
Shin, K., Kenward, C. & Rainey, J. K. Apelinergic system structure and function. Compr. Physiol. 8, 407–450 (2017).
Yamaleyeva, L. M., Shaltout, H. A. & Varagic, J. Apelin-13 in blood pressure regulation and cardiovascular disease. Curr. Opin. Nephrol. Hypertens. 25, 396–403 (2016).
Li, Y. et al. Apelin ameliorated acute heart failure via inhibiting endoplasmic reticulum stress in rabbits. Amino Acids 53, 417–427 (2021).
Sato, T. et al. ELABELA-APJ axis protects from pressure overload heart failure and angiotensin II-induced cardiac damage. Cardiovasc. Res. 113, 760–769 (2017).
Coquerel, D. et al. ELABELA improves cardio-renal outcome in fatal experimental septic shock. Crit. Care Med. 45, e1139–e1148 (2017).
Xu, C. Cardiovascular aspects of ELABELA: A potential diagnostic biomarker and therapeutic target. Vascul. Pharmacol. 151, 107193 (2023).
Xu, C. The Elabela in hypertension, cardiovascular disease, renal disease, and preeclampsia: An update. J. Hypertens. 39, 12–22 (2021).
Goetze, J. P. et al. Apelin: A new plasma marker of cardiopulmonary disease. Regul. Pept. 133, 134–138 (2006).
Chong, K. S., Gardner, R. S., Morton, J. J., Ashley, E. A. & McDonagh, T. A. Plasma concentrations of the novel peptide apelin are decreased in patients with chronic heart failure. Eur. J. Heart Fail. 8, 355–360 (2006).
Francia, P. et al. Cardiac resynchronization therapy increases plasma levels of the endogenous inotrope apelin. Eur. J. Heart Fail. 9, 306–309 (2007).
Gao, L. R. et al. Increased apelin following bone marrow mononuclear cell transplantation contributes to the improvement of cardiac function in patients with severe heart failure. Cell Transplant. 18, 1311–1318 (2009).
Chandrasekaran, B. et al. Myocardial apelin production is reduced in humans with left ventricular systolic dysfunction. J. Card Fail. 16, 556–561 (2010).
Przewlocka-Kosmala, M., Kotwica, T., Mysiak, A. & Kosmala, W. Reduced circulating apelin in essential hypertension and its association with cardiac dysfunction. J. Hypertens. 29, 971–979 (2011).
El Amrousy, D. & El-Mahdy, H. Prognostic value of serum Apelin level in children with heart failure secondary to congenital heart disease. Pediatr. Cardiol. 39, 1188–1193 (2018).
Han, L. et al. Increased plasma level of apelin with NYHA grade II and III but not IV. Amino. Acids 52, 823–829 (2020).
Helske, S., Kovanen, P. T., Lommi, J., Turto, H. & Kupari, M. Transcardiac gradients of circulating apelin: extraction by normal hearts vs release by hearts failing due to pressure overload. J. Appl. Physiol. (1985) 109, 1744–1748 (2010).
Miettinen, K. H. et al. Utility of plasma apelin and other indices of cardiac dysfunction in the clinical assessment of patients with dilated cardiomyopathy. Regul. Pept. 140, 178–184 (2007).
van Kimmenade, R. R. et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J. Am. Coll. Cardiol. 48, 1217–1224 (2006).
Dönmez, Y. & Acele, A. Increased Elabela levels in the acute ST segment elevation myocardial infarction patients. Medicine 98, e17645 (2019).
Tian, Q. P. et al. Plasma level of Elabela in patients with coronary heart disease and its correlation with the disease classification. Int. Heart J. 62, 752–755 (2021).
Acele, A., Bulut, A., Donmez, Y. & Koc, M. Serum Elabela level significantly increased in patients with complete heart block. Braz. J. Cardiovasc. Surg. 35, 683–688 (2020).
Wang, J. et al. Elabela: A novel biomarker for right ventricular pressure overload in children with pulmonary stenosis or pulmonary atresia with intact ventricular septum. Front. Cardiovasc. Med. 7, 581848 (2020).
Cui, C., Zhou, H. & Xu, J. ELABELA acts as a protective biomarker in patients with atrial fibrillation. J. Thorac. Dis. 13, 6876–6884 (2021).
Ma, Z., Zhao, L., Zhang, Y. P., Zhong, J. C. & Yang, X. C. Declined ELABELA plasma levels in hypertension patients with atrial fibrillation: A case control study. BMC Cardiovasc. Disord. 21, 390 (2021).
Li, Y. et al. Declined circulating Elabela levels in patients with essential hypertension and its association with impaired vascular function: A preliminary study. Clin. Exp. Hypertens. 42, 239–243 (2020).
Zhang, H. et al. Serum Elabela/toddler levels are associated with albuminuria in patients with type 2 diabetes. Cell. Physiol. Biochem. 48, 1347–1354 (2018).
Aguilar, D. et al. American heart association heart failure and transplantation committee of the council on clinical cardiology; council on cardiovascular surgery and anesthesia; council on cardiovascular and stroke nursing; council on hypertension; and council on quality and outcomes research. contributory risk and management of comorbidities of hypertension, obesity, diabetes mellitus, hyperlipidemia, and metabolic syndrome in chronic heart failure: A scientific statement from the american heart association. Circulation 134, e535–e578 (2016).
Selvaraj, S. et al. Prognostic value of albuminuria and influence of spironolactone in heart failure with preserved ejection fraction. Circ. Heart Fail. 11, e005288 (2018).
Ma, Z. et al. Lower plasma Elabela levels in hypertensive patients with heart failure predict the occurrence of major adverse cardiac events: A preliminary study. Front. Cardiovasc. Med. 8, 638468 (2021).
Ferdinal, F., Limanan, D., Rini, R. D., Alexsandro, R. & Helmi, R. Elevated levels of Apelin-36 in heart failure due to chronic Systemic hypoxia. Int. J. Angiol. 28, 194–199 (2019).
Földes, G. et al. Circulating and cardiac levels of apelin, the novel ligand of the orphan receptor APJ, in patients with heart failure. Biochem. Biophys. Res. Commun. 308, 480–485 (2003).
Bezak, B. et al. Plasmatic apelin shows a promising potential as a screening biomarker for atrial fibrillation. Bratisl. Lek. Listy. 124, 368–372 (2023).
El Mathari, B. et al. Apelin improves cardiac function mainly through peripheral vasodilation in a mouse model of dilated cardiomyopathy. Peptides 142, 170568 (2021).
Zhong, S. et al. Apelin-13 alleviated cardiac fibrosis via inhibiting the PI3K/Akt pathway to attenuate oxidative stress in rats with myocardial infarction-induced heart failure. Biosci. Rep. 40, BSR20200040 (2020).
Fraga-Silva, R. A. et al. Apelin-13 treatment enhances the stability of atherosclerotic plaques. Eur. J. Clin. Invest. 48, e12891 (2018).
Gunter, S. et al. Apelin concentrations are associated with altered atherosclerotic plaque stability mediator levels and atherosclerosis in rheumatoid arthritis. Atherosclerosis 256, 75–81 (2017).
Zhang, X. et al. Apelin-13 inhibits lipoprotein lipase expression via the APJ/PKCα/miR-361-5p signaling pathway in THP-1 macrophage-derived foam cells. Acta Biochim. Biophys. Sin. 49, 530–540 (2017).
Hendrianus, Adiarto S, Prakoso R, Firdaus I, Indriani S, Rudiktyo E, Widyantoro B, Taofan, Ambari AM, Sukmawan R. A novel peptide elabela is associated with hypertension-related subclinical atherosclerosis. High Blood Press Cardiovasc Prev. 30: 37–44, (2023).
Herrington, W., Lacey, B., Sherliker, P., Armitage, J. & Lewington, S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ. Res. 118, 535–546 (2016).
Bonsu, K. O., Owusu, I. K., Buabeng, K. O., Reidpath, D. D. & Kadirvelu, A. Clinical characteristics and prognosis of patients admitted for heart failure: A 5-year retrospective study of African patients. Int. J. Cardiol. 238, 128–135 (2017).
Murza, A. et al. Discovery and Structure-activity relationship of a bioactive fragment of ELABELA that modulates vascular and cardiac functions. J. Med. Chem. 59, 2962–2972 (2016).
Yang, P. et al. Elabela/toddler is an endogenous agonist of the Apelin APJ receptor in the adult cardiovascular system, and exogenous administration of the peptide compensates for the downregulation of its expression in pulmonary arterial hypertension. Circulation 135, 1160–1173 (2017).
Sainsily, X. et al. Elabela protects spontaneously hypertensive rats from hypertension and cardiorenal dysfunctions exacerbated by dietary high-salt intake. Front. Pharmacol. 12, 709467 (2021).
Campbell, P., Rutten, F. H., Lee, M. M., Hawkins, N. M. & Petrie, M. C. Heart failure with preserved ejection fraction: Everything the clinician needs to know. Lancet 403, 1083–1092 (2024).
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Skibelund AK, ESC Scientific Document Group. Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 44(3627–3639), 2023 (2023).
Pieske, B. et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: A consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. Heart J. 40, 3297–3317 (2019).
Borlaug, B. A., Kane, G. C., Melenovsky, V. & Olson, T. P. Abnormal right ventricular-pulmonary artery coupling with exercise in heart failure with preserved ejection fraction. Eur. Heart J. 37, 3293–3302 (2016).
Ge, J. Coding proposal on phenotyping heart failure with preserved ejection fraction: A practical tool for facilitating etiology-oriented therapy. Cardiol. J. 27, 97–98 (2020).
Coiro, S. et al. Association of diabetes and kidney function according to age and systolic function with the incidence of sudden cardiac death and non-sudden cardiac death in myocardial infarction survivors with heart failure. Eur. J. Heart Fail 21, 1248–1258 (2019).
Xu, C. et al. ELABELA antagonizes intrarenal renin-angiotensin system to lower blood pressure and protects against renal injury. Am. J. Physiol. Renal. Physiol. 318, F1122–F1135 (2020).
Chen, Z. et al. ELABELA attenuates deoxycorticosterone acetate/salt-induced hypertension and renal injury by inhibition of NADPH oxidase/ROS/NLRP3 inflammasome pathway. Cell Death Dis. 11, 698 (2020).
Chen, H. et al. ELABELA and an ELABELA fragment protect against AKI. J. Am. Soc. Nephrol. 28, 2694–2707 (2017).
Zhang, Y. et al. Elabela protects against podocyte injury in mice with streptozocin-induced diabetes by associating with the PI3K/Akt/mTOR pathway. Peptides 114, 29–37 (2019).
Redfors, B. et al. B-type natriuretic peptide assessment in patients undergoing revascularization for left main coronary artery disease: Analysis from the EXCEL trial. Circulation 138, 469–478 (2018).
Zhang, C. et al. Implications of N-terminal pro-B-type natriuretic peptide in patients with three-vessel disease. Eur. Heart J. 40, 3397–3405 (2019).
Rahimi, K. et al. Risk prediction in patients with heart failure: A systematic review and analysis. JACC Heart Fail 2, 440–446 (2014).
Omar, H. R. & Guglin, M. Discharge BNP is a stronger predictor of 6-month mortality in acute heart failure compared with baseline BNP and admission-to-discharge percentage BNP reduction. Int. J. Cardiol. 221, 1116–1122 (2016).
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 82160051 and 32100908), the Jiangxi Provincial Natural Science Foundation (No. 20232BAB206018), the science and technology research project in Education Department of Jiangxi Province (No. GJJ2200904), Jiangxi “Double Thousand Plan” (No. jxsq2020101074), the Ph.D. Start-up Research Fund in Jiangxi University of Chinese Medicine (No. 2020BSZR009), the science and technology research project in Health Commission of Jiangxi Province (No. 202311143), the Scientific and Technological Innovation Team grant of the Jiangxi University of Chinese Medicine (No. CXTD22014).
Author information
Authors and Affiliations
Contributions
Conceptualization, C.X.; methodology, C.X., C.L., J.X., X.Yi., S.S., H.Y., W.T., X.Y., and L.Z.; validation, C.X., C.L., J.X., X.Yi., S.S., H.Y., W.T., X.Y., and L.Z.; formal analysis and interpretation, C.X., C.L., J.X., X.Yi., S.S., H.Y., W.T., X.Y., L.Z., and J.Y.; investigation, C.X., C.L., J.X., X.Yi., S.S., H.Y., W.T., X.Y., and L.Z.; data curation, C.X., C.L., J.X., X.Yi., S.S., H.Y., W.T., X.Y., and L.Z.; writing—original draft preparation, C.X., C.L., J.X., X.Yi., S.S., and H.Y.; writing—review and editing, C.X. and J.Y.; supervision, C.X.; project administration, C.X.; funding acquisition, C.X. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, C., Xiong, J., Yi, X. et al. Decreased plasma ELABELA level as a novel screening indicator for heart failure: a cohort and observational study. Sci Rep 14, 11333 (2024). https://doi.org/10.1038/s41598-024-61480-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61480-x
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.