Abstract
This study determined the prevalence and the associated factors with meeting the recommended amount of physical activity among type 2 diabetes mellitus (T2DM) patients receiving care in resource-limited settings of the West Bank of Palestine. Physical activity was assessed using the World Health Organization’s Global Physical Activity Questionnaire. Associations were examined using multivariate logistic regression. Of the 302 patients included, 117 (38.7%) met the recommended amount of physical activity. Being younger than 58 years [aOR = 2.1 (95% CI 1.0–4.3], were employed [aOR = 2.3 (95% CI 1.1–4.9)], had high income [aOR = 3.9 (95% CI 1.3–11.9)], had thought that physical activity was crucial for T2DM patients [aOR = 32.7 (95% CI 3.9–275.5)], did not have comorbidities [aOR = 2.2 (95% CI 1.1–4.4)], had normal weight [aOR = 2.8 (95% CI 1.3–6.0)], and those who were overweight [aOR = 2.6 (95% CI 1.1–6.0)] were more likely to meet the recommended amount of physical activity compared to the patients who were 58 years or older, had low income, did not think that physical activity was crucial for T2DM patients, had comorbidities, and were obese, respectively. There is a need to increase physical activity among T2DM patients in resource limited settings.
Similar content being viewed by others
Introduction
Globally, physical inactivity is considered a major cause of significant mortality and morbidity1,2. It is well-established that physical inactivity is causally associated with a wide range of negative health outcomes that include cardiovascular diseases, type 2 diabetes mellitus (T2DM), and obesity3. According to some estimates, physical inactivity caused 5.3 million deaths globally which accounted for about 9% of all premature mortality in 20084.
The World Health Organization (WHO) has defined physical inactivity as engaging in less than 600 metabolic equivalent tasks (METs) minutes per week5. In 2016, the global age-standardized prevalence of physical inactivity was 27.5% (95% uncertainty interval 25.0–32.2) based on 358 studies that were conducted in 168 countries and included a total of 1.9 million participants6. The level of physical inactivity can be affected by age, gender, sociodemographic, cultural, health conditions/disabilities, and personal factors7,8. It has been estimated that 7.2% of all all-cause mortality among T2DM patients can be attributed to physical inactivity4.
Physical inactivity is a modifiable risk factor for metabolic diseases including T2DM. In addition, being physically active was shown to be associated with multiple health benefits9. Therefore, many health organizations and professional bodies including the WHO and the World Health Assembly (WHA) have called for higher levels of physical activity and launched initiatives to reduce levels of physical inactivity10. The WHO’s revised Global Recommendations on Physical Activity for Health offer fresh guidelines to decrease levels of physical inactivity, emphasizing the message that engaging in any amount of physical activity is preferable to none, and increasing physical activity levels can lead to better health outcomes10,11.
Accumulating evidence has shown that T2DM patients can achieve adequate glycemic control using pharmacologic and nonpharmacologic approaches12,13. In addition to diet, physical activity is one of the most commonly used nonpharmacological approaches to help achieve adequate glycemic control among T2DM patients. Systematic reviews of different studies showed that T2DM patients, breast cancer, ischemic heart disease, and chronic obstructive pulmonary disease who engaged in higher levels of physical activity after their diagnosis have lower mortality rates12,14,15,16. Additionally, higher levels of physical activity were shown to improve body composition, muscular strength, bone health, cardiorespiratory functions, psychological health, and the quality of life of the patients12.
Even though physical activity is a cornerstone in the management of T2DM, several studies have reported suboptimal levels of physical activity among T2DM patients 12,17,18,19. It has been argued that the likelihood of meeting the recommended amount of physical activity among T2DM patients can be influenced by sociodemographic, economic, health-related, and psychological factors. The patients who are old, have other comorbid conditions, and high body mass index often face physical and/or health-related limitations to engage in physical activity20. Similarly, employed patients may have limited leisure time that can be used for physical activity, especially when their job is more sedentary21. Moreover, patients who live in rural areas and refugee camps and those with low income have limited access to recreational and sports facilities22,23. Although married patients could have social support from their spouses to engage in physical activity, they can also enjoy less autonomy in scheduling their physical activities. It has been argued that education can improve health awareness and knowledge of the benefits of physical activity for T2DM patients24. A few studies were conducted to assess the prevalence of physical inactivity among Palestinians with T2DM. These studies were conducted in the Gaza Strip25,26,27. Physical inactivity levels were high among T2DM patients in the Gaza Strip. However, little is known about the prevalence of physical inactivity among T2DM patients in the West Bank, notably those receiving care in resource-limited settings28. We hypothesized that similar to the data reported from the Gaza Strip, the prevalence of physical inactivity among T2DM patients in the West Bank was also high. There was a need to determine the associations between the sociodemographic and clinical factors of the patients and meeting the recommended amount of physical activity. Therefore, this study was conducted to assess the prevalence of T2DM patients meeting the recommended amount of physical activity and to determine the associations between different sociodemographic and clinical factors and meeting the recommended amount of physical activity among T2DM patients who received care in resource-limited settings in the West Bank of Palestine.
Methods
Study area
This study was conducted in the resource-limited primary healthcare clinics distributed across the different governorates in the West Bank including those in the refugee camps. Figure 1 shows a map of the West Bank with the different governorates.
Map of the West Bank showing the governorates (the map was modified from Wikimedia Commons: www.commons.wikimedia.org/wiki).
Study design and participants
The study was carried out using a cross-sectional approach. The study adhered to the guidelines of the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement29.
The participants in this study were T2DM patients who received care in the Palestinian healthcare system. The necessary sample size was determined based on the number of individuals in Palestine with T2DM, as reported by the Palestinian Ministry of Health. At the time of the research, the number of individuals with diabetes mellitus in Palestine was 270,465, with 95.3% of those having T2DM. An online calculator (Raosoft, Raosoft, Inc.) was used to calculate the appropriate sample size with a 95% confidence level and a margin of error of 5% using physical activity data (time spent in moderate to vigorous physical activity) reported in previous studies among T2DM patients8,30,31,32,33,34,35,36,37. The calculated sample size was 384 patients. In this study, we decided to invite 400 T2DM patients.
The patients were included in this study using a convenience sampling approach when they met the following inclusion criteria: (1) being 18 years and older, (2) having been diagnosed with T2DM, (3) received healthcare services in the Palestinian healthcare system, (4) willing to respond to items in a questionnaire, and (5) providing written informed consent. Patients who had a record of mental and cognitive impairments or as diagnosed by physicians were excluded from this study.
Physical activity outcome
The total physical activity time and METs were the dependent outcomes measured in this study. It is noteworthy mentioning that physical activity time and METs are related concepts. However, the two concepts differ in measuring physical exertion and energy expenditure33,34,35. While physical activity refers to any bodily movement that requires expenditure of energy, METs are a measure of the energy expenditure while performing the different forms of physical activity. One MET is defined as the energy expenditure while resting. This is equivalent to the amount of energy expenditure while sitting quietly. The different forms of physical activity performed are assigned MET values based on their intensity relative to the metabolic rate at resting. For instance, running or performing a vigorous exercise has a higher MET value compared to walking at a moderate pace.
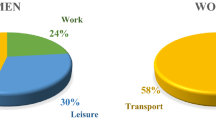
The total physical activity time and MET-minutes/week were measured using the WHO’s Global Physical Activity Questionnaire (GPAQ)33. Using 16 items, the GPAQ measured the physical activity time and MET-minutes/week performed at work, traveling to and from places, and during recreational activities. The GPAQ was shown to be valid and reliable in measuring the amount of physical activity time and MET-minutes/week in different populations and countries34,35. As guided by the GPAQ analysis manual, the patients were classified into MET classes as: (1) low: < 3 METs (< 600 MET-minutes/week), (2) moderate: 3–6 METs (600–3000 MET-minutes/week), and (3) high: > 6 METs (> 3000 MET-minutes/week)34. According to the WHO, one should expend at least 600 MET-minutes/week to meet the recommended amount of physical activity5.
Compared to other tools that can be used to measure physical activity and energy expenditure, the WHO’s GPAQ was preferred because it was more often used to assess physical activity levels in low- and middle-income countries38,39,40.
Independent variables
For this research, a questionnaire specifically designed for the study was utilized. Previous studies that assessed physical activity levels in individuals with diabetes were consulted while developing of the questionnaire8,36,37. While developing the questionnaire, the literature was searched for the factors that could affect meeting the recommended amount of physical activity. Meeting the recommended amount of physical activity was influenced by sociodemographic and illness-related factors34,35,38,39,40. To determine the associations between the different sociodemographic and clinical factors and meeting the recommended amount of physical activity among T2DM patients in this study, variables like age, marital status, employment status, place of residence, educational attainment, monthly household income, medical insurance status, and type of medical insurance were collected. The patients were also asked to indicate whether they have participated in an awareness program related to T2DM, received education about the importance of physical activity in T2DM management, were physically active before being diagnosed with T2DM, and whether they thought that physical activity was beneficial for T2DM patients. In addition, the patients were asked to report if they had hyperlipidemia, hypertension, or other chronic health conditions, and the time elapsed since they received their diagnosis with T2DM. The body mass index of the patients was calculated based on their weight and height. The last glycosylated hemoglobin (HbA1c), fasting plasma glucose, and postprandial plasma glucose levels were obtained from their medical records.
Statistical analysis
The data were analyzed using IBM SPSS v. 21.0 (IBM Inc., Armonk, NY). The collected data were tested for normal distribution using the Shapiro–Wilk test, which revealed that the data did not conform to a normal distribution. Therefore, medians with the corresponding interquartile range [IQR = first (Q1) and third (Q3) quartiles] were employed. Differences in the physical activity time and MET-minutes/week as continuous variables were assessed using the Mann–Whitney U and Kruskal–Wallis tests. The correlations between the continuous variables were assessed using Spearman's rank correlations. Low, moderate, and high METs classes were described using frequencies (n) and percentages (n). The associations between demographic and clinical variables of the patients with the three METs classes (low, moderate, and high) were investigated using Chi-square tests. Because meeting the recommended amount of physical activity was indicated by expending 600 or more MET-minutes/week5, the patients were categorized into two groups: those who did not meet the recommended amount of physical activity (< 3 METs (< 600 MET-minutes/week)) and those who met the recommended amount of physical activity ((≥ 3METs (≥ 600 MET-minutes/week). The continuous variables like age, HbA1c, fasting plasma glucose level, and postprandial plasma glucose level were categorized around their medians. The body mass index was categorized as: normal weight < 25 kg/m2, overweight: 25–29.9 kg/m2, or obese: ≥ 30 kg/m2. The household income was categorized as: low (< US$ 800), medium (US$ 800–1350), or high (> US$ 1350) based on the reports of the Palestinian Central Bureau of Statistics. The associations between demographic and clinical variables of the patients with meeting or not meeting the recommended amount of physical activity were investigated using Chi-square tests. A multivariate logistic regression model was used to calculate the adjusted odds ratios (aOR) for meeting the recommended amount of physical activity. All independent variables were retained in the multivariate logistic regression model. A p-value of < 0.05 indicated statistical significance.
Ethical approvals
This study adhered to both local and international ethical principles governing scientific research involving human subjects. The research received approval from the Institutional Review Board (IRB) of An-Najah National University and also obtained consent from the Health Education Office of the Ministry of Health. Written informed consent was provided by all patients, and hospital and clinic managers approved the researchers' access to the patient's medical records. The data collected were coded and analyzed anonymously to protect the patients' privacy.
Results
Of the 400 invited patients, 302 completed the questionnaire, giving a response rate of 75.5%. The median age of the patients was 58.0 [IQR = 50.0, 67.0] years and a median time since diagnosis of 9.0 [IQR = 5.0, 15.0] years. The median body mass index was 28.1 [IQR = 24.9, 33.1] kg/m2, while the median fasting plasma glucose level was 170.0 [IQR = 130.0, 230.0] mg/dL, the median postprandial plasma glucose level was 220.0 [IQR = 170.0, 300.0] mg/dL, and the median HbA1c was 8.0% [IQR = 7.0%, 10.0%]. The detailed information on the patient's sociodemographic and clinical characteristics are shown in Table 1.
Responses of the patients on the global physical activity questionnaire items
In this study, many patients reported low levels of physical activity at work, during travel to and from places, and during recreational activities. The detailed responses of the patients on the items in the Global Physical Activity Questionnaire are shown in Supplementary Table S1.
Associations between physical activity outcome and the independent variables
The median physical activity was 480.0 [IQR = 69.0, 1440.0] min and the median MET-min/week was 100.0 [IQR = 0.0, 272.5]. The total physical activity and MET were significantly higher for patients who were younger than 58 years, employed, had a university degree, had median or high income, had participated in an awareness program related to T2DM, had received education about the importance of physical activity in T2DM management, were physically active before being diagnosed with T2DM, thought that physical activity was crucial for T2DM patients, did not have hyperlipidemia, hypertension, or other health conditions, was diagnosed with T2DM less than 10 years ago, had normal body weight, had HbA1c less than 7%, had a fasting plasma glucose level less than 130 mg/dL, and had a postprandial plasma glucose level less than 180 mg/dL. Details of the differences in total physical activity and MET in relation to the demographic and disease variables of the patients are shown in Supplementary Table S2.
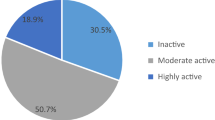
When the patients were stratified into MET classes, 185 (61.3%) of the patients reported low physical activity and 11.9% reported high physical activity. Significantly more patients were in the high MET class when they were younger than 58 years, employed, had a university education, had medium or higher income, had participated in an awareness program related to T2DM, had received education about the importance of physical activity in T2DM management, were physically active before being diagnosed with T2DM, thought that physical activity was crucial for T2DM patients, did not have hyperlipidemia, hypertension, or other health conditions, was diagnosed with T2DM less than 10 years ago, had normal body weight, had HbA1c less than 7%, had a fasting plasma glucose level less than 130 mg/dL, and had a postprandial plasma glucose level less than 180 mg/dL. Details of the associations are shown in Supplementary Table S3.
When the patients were stratified into meeting or not meeting the recommended amount of physical activity, 117 (38.7%) patients met the recommended amount of physical activity. Chi-square tests showed that meeting the recommended amount of physical activity was significantly associated with younger age, being employed, having a university degree, and having higher income (Table 2). In addition, having participated in an awareness program, having received education about the importance of physical activity in T2DM management, being physically active before diagnosis with T2DM, and thinking that physical activity was crucial for T2DM patients were also associated with meeting the recommended amount of physical activity. Moreover, patients who did not have hyperlipidemia, hypertension, or other health conditions, were diagnosed with T2DM less than 10 years ago, had normal body weight, had HbA1c less than 7%, had a fasting plasma glucose level less than 130 mg/dL, and had a postprandial plasma glucose level less than 180 mg/dL were more likely to meet the recommended amount of physical activity. Details of the associations are shown in Table 2.
The multivariate logistic regression model showed that the odds of the patients who were younger than 58 years were 2.1-fold (95% CI 1.0–4.3) more likely to meet the recommended amount of physical activity compared to the patients who were 58 years or older (Table 2). The odds for the patients who were employed were 2.3-fold (95% CI 1.1–4.9) more likely to meet the recommended amount of physical activity compared to the patients who unemployed. The odds for the patients who had high household income were 3.9-fold (95% CI 1.3–11.9) more likely to meet the recommended amount of physical activity compared to the patients who had low household income. The odds for the patients who had thought that physical activity was crucial for T2DM patients were 32.7-fold (95% CI 3.9–275.5) more likely to meet the recommended amount of physical activity compared to the patients who did not think that physical activity was crucial for T2DM patients. The odds for the patients who did not have comorbidities were 2.2-fold (95% CI 1.1–4.4) more likely to meet the recommended amount of physical activity compared to the patients who had comorbidities. The odds for the patients who had normal weight and those who were overweight were 2.8-fold (95% CI 1.3–6.0) and 2.6-fold (95% CI 1.1–6.0) more likely to meet the recommended amount of physical activity compared to the patients who were obese, respectively. Details of the multivariate logistic regression model are shown in Table 2.
There was a significant negative correlation between total physical activity and MET with age, the time elapsed since diagnosis, body mass index, fasting plasma glucose level, postprandial plasma glucose level, and HbA1c. The correlation matrix is shown in Supplementary Table S4.
Discussion
Evidence of the benefits of physical activity for T2DM patients is well-established. Adherence to the recommended amount of physical activity was shown to improve insulin sensitivity, help achieve glycemic control, improve cardiorespiratory fitness, blood pressure control, weight loss, lipid profile, psychological health, and quality of life of the patients12. For the first time, levels of physical activity were assessed among T2DM patients in the West Bank. Additionally, the factors associated with meeting the recommended amount of physical activity were also investigated. The findings reported in this study would be informative to decision and policymakers who might be interested in designing appropriate measures to increase physical activity and reduce physical inactivity among T2DM patients.
In this study, the majority (61.3%) of the T2DM patients reported low physical activity. Moreover, only 38.7% of the patients met the recommended amount of physical activity. The findings reported in this study were consistent with those reported in the Arab region8,25,26,41,42. Additionally, the findings were also consistent with those reported in the Western world including the US in which more than 60% of T2DM patients were reportedly inactive43. Given the increasing consumption of energy-rich diets and adopting sedentary lifestyles, countries in the Middle East and North Africa (MENA) are expected to have a 96% increase in the number of patients with diabetes by the year 203544. Taken together these findings indicate that there is a pressing need to design effective measures to increase physical activity and reduce sedentary lifestyles among T2DM patients.
Although 27.2% of the patients reported no physical activity in this study, this percentage was lower than those reported in previous studies like in Oman (60.3%) and the US8,45. Similar to previous studies, the patients who reported low physical activity had higher HbA1c, fasting plasma glucose, and postprandial plasma glucose levels. These findings were not surprising as the benefits of physical activity in helping patients achieve glycemic control were well-established12.
The findings of this study showed that higher physical activity was associated with younger age, employment, high income, positive attitudes toward physical activity, reporting the absence of comorbidities, and not being obese. Similarly, higher recreational inactivity was also reported among patients who lacked financial resources34. The results reported in this study were consistent with those reported in other countries including Arab countries8,25,26,34,41,42,46,47,48,49. Old age and high body mass index were predictors of physical inactivity. It was estimated that travel inactivity increased by 6% for every increased unit of body mass index. Younger patients without existing chronic comorbidities would likely face fewer barriers to performing physical activities compared to older patients with chronic diseases8. Probably, those patients would find it easier to travel and practice recreational activities compared to older patients who have other chronic comorbidities50. Healthcare providers should consider providing more comprehensive healthcare services to T2DM patients in the primary healthcare clinics. In addition, T2DM patients should be assessed and monitored for complications. Moreover, comorbidities, HbA1c, body mass index, blood pressure, and lipid profile should be periodically assessed and appropriate recommendations should be made. Probably, healthcare providers should consider counseling older patients on the importance of physical activity and maintaining a healthy weight. Suitable physical activity programs should be developed and tailored to the needs of the individual patients. Physical activity programs might consider avoiding the use of expensive exercise equipment. These programs might include walking, gardening, and home-based exercise programs that require minimal or no equipment. Moreover, the patients who expressed positive attitudes toward physical activity were more likely to report higher physical activity. These findings might indicate that education, awareness, and attitude changing interventions might be effective in increasing physical activity and decreasing physical inactivity. These findings indicate that decision- and policymakers should consider intensifying campaigns and initiatives that target patients who are older, obese, have comorbidities, and have negative attitudes toward the benefits of physical activity for T2DM patients.
The findings reported in this study are consideration worthy as the Palestinian healthcare system is complex and highly fragmented. T2DM patients receive healthcare services in healthcare clinics that belong to the governmental sector, the non-governmental organizations, the Palestinian Military Medical Services, the United Nations Relief and Work Agency, and the private sector51. It is noteworthy to mention that none of these sectors provide comprehensive healthcare services. The Palestinian Ministry of Health provides primary healthcare services to T2DM patients through primary healthcare clinics that are distributed throughout the West Bank of Palestine51,52. The healthcare professionals providing services through these clinics reported lack of training on the care guidelines52. In addition, the clinics lacked essential equipment to assess for diabetic complications including ophthalmoscopes, visual acuity charts, electrocardiogram machines, tuning forks, and foot-care equipment. Moreover, weight and height measurements, calculation of body mass index, and measurement of blood pressure were often neglected. Many clinics do not offer monofilament, microalbumin, and glycated hemoglobin A1c (HbA1c) tests. Similarly, nutrition and physical activity specialists are not available in many of these clinics. The consultations with physicians and nurses are often short, not individualized, or recorded. The appointment system and protocols for periodic monitoring are often not used. Decision-makers in the healthcare authorities might use the findings reported in this study to improve the care services provided to T2DM patients in these clinics.
Strengths and limitations
The findings of this study should be interpreted in light of the following strengths and limitations. First, this was the first study in the West Bank to determine the level of physical activity among T2DM patients. The factors associated with low, moderate, and high physical activity were also determined. The findings of this study could be informative to decision and policymakers in the Palestinian healthcare authorities and similar healthcare systems. Second, the study was conducted using a robust tool that was previously validated and tested for reliability in different settings and countries. The use of this robust, valid, and reliable tool should have promoted comparability of the findings with those reported in other studies. Third, the sample of patients who were included in this study was diversified in terms of demographic and disease variables. This diversity should have improved the representativeness of the entire population of T2DM patients and should have improved the external validity of the findings reported in this study.
On the other hand, the findings of this study should also be interpreted after considering the following limitations. First, the study was conducted in a cross-sectional design. Cross-sectional studies are not suitable to study causalities. Second, many of the data collected in this study were self-reported. Therefore, social desirability and recall bias cannot be excluded. Third, the sample size used in this study was not very large compared to previous studies. A larger sample size could have allowed a more solid conclusion.
Conclusion
T2DM patients who were included in this study reported low physical activity as determined by the WHO’s GPAQ. Higher physical activity was associated with younger age, high income, positive attitudes toward physical activity, absence of comorbidities, and not being obese. Decision and policymakers in healthcare authorities need to consider designing effective interventions to increase physical activity and reduce physical inactivity among T2DM patients in resource limited settings. More studies are still needed to determine which interventions are superior in increasing physical activity among T2DM patients.
Data availability
All data relevant to this study were included in the “Results” section of this manuscript.
References
Kohl, H. W. 3rd. et al. The pandemic of physical inactivity: Global action for public health. Lancet 380, 294–305 (2012).
ArochaRodulfo, J. I. Sedentary lifestyle a disease from xxi century. Clin. Investig. Arterioscler. 31, 233–240 (2019).
Cleven, L., Krell-Roesch, J., Nigg, C. R. & Woll, A. The association between physical activity with incident obesity, coronary heart disease, diabetes and hypertension in adults: A systematic review of longitudinal studies published after 2012. BMC Public Health 20, 726 (2020).
Lee, I. M. et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 380, 219–229 (2012).
Organization, W.H. (World Health Organization, Geneva, Switzerland; 2010).
Guthold, R., Stevens, G. A., Riley, L. M. & Bull, F. C. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 6, e1077–e1086 (2018).
Hafner, M. et al. Estimating the global economic benefits of physically active populations over 30 years (2020–2050). Br. J. Sports Med. 54, 1482–1487 (2020).
Alghafri, T. S. et al. Correlates of physical activity and sitting time in adults with type 2 diabetes attending primary health care in Oman. BMC Public Health 18, 85 (2017).
Chan, J. S. Y. et al. Special issue-therapeutic benefits of physical activity for mood: A systematic review on the effects of exercise intensity duration, and modality. J. Psychol. 153, 102–125 (2019).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462 (2020).
Organization, W. H. Global action plan on physical activity 2018–2030: More active people for a healthier world (World Health Organization, Geneva, Switzerland, 2019).
Shawahna, R., Batta, A., Asa’ad, M., Jomaah, M. & Abdelhaq, I. Exercise as a complementary medicine intervention in type 2 diabetes mellitus: A systematic review with narrative and qualitative synthesis of evidence. Diabetes Metab. Syndr. 15, 273–286 (2021).
Wang, X., Kang, J., Liu, Q., Tong, T. & Quan, H. Fighting diabetes mellitus: Pharmacological and non-pharmacological approaches. Curr. Pharm. Des. 26, 4992–5001 (2020).
Geidl, W., Schlesinger, S., Mino, E., Miranda, L. & Pfeifer, K. Dose-response relationship between physical activity and mortality in adults with noncommunicable diseases: A systematic review and meta-analysis of prospective observational studies. Int. J. Behav. Nutr. Phys. Act 17, 109 (2020).
Carbone, S., Del Buono, M. G., Ozemek, C. & Lavie, C. J. Obesity, risk of diabetes and role of physical activity, exercise training and cardiorespiratory fitness. Prog. Cardiovasc. Dis. 62, 327–333 (2019).
Singh, R., Pattisapu, A. & Emery, M. S. US physical activity guidelines: Current state, impact and future directions. Trends Cardiovasc. Med. 30, 407–412 (2020).
Bullard, T. et al. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: Cancer, cardiovascular disease, and diabetes. BMC Public Health 19, 636 (2019).
Joseph, J. J. et al. Physical activity, sedentary behaviors and the incidence of type 2 diabetes mellitus: The multi-ethnic study of atherosclerosis (MESA). BMJ Open Diabetes Res. Care 4, e000185 (2016).
Plotnikoff, R. C. et al. Factors associated with physical activity in Canadian adults with diabetes. Med. Sci. Sports Exerc. 38, 1526–1534 (2006).
Wang, Q. et al. Physical activity patterns and risk of type 2 diabetes and metabolic syndrome in middle-aged and elderly northern Chinese adults. J. Diabetes Res. 2018, 7198274 (2018).
Kim, K. S. et al. Association of self-reported sedentary time with insulin resistance among Korean adults without diabetes mellitus: A cross-sectional study. BMC Public Health 18, 1335 (2018).
Mondal, R., Banik, P. C. & Zaman, M. M. Low physical activity among middle-aged type-2 diabetic outpatients of two peripheral hospitals in Bangladesh. PLoS One 18, e0284392 (2023).
Lee, E. B. et al. Association between domain-specific physical activity and diabetes in Korean adults. Sci. Rep. 11, 13066 (2021).
Chirdkiatisak, M., Sranacharoenpong, K., Churak, P. & Praditsorn, P. Thai diabetes prevention education program: development and validation of the Thai physical activity questionnaire for at-risk people. J. Public Health 27, 659–667 (2019).
El Bilbeisi, A. H., Hosseini, S. & Djafarian, K. The association between physical activity and the metabolic syndrome among type 2 diabetes patients in Gaza strip, Palestine. Ethiop. J. Health Sci. 27, 273–282 (2017).
Ellulu, M. S. Obesity, hypertension, and type-2 diabetes mellitus: The interrelationships and the determinants among adults in Gaza city, Palestine. Osong. Public Health Res. Perspect. 9, 289–298 (2018).
Ellulu, M. S. & Samouda, H. Clinical and biological risk factors associated with inflammation in patients with type 2 diabetes mellitus. BMC Endocr. Disord. 22, 16 (2022).
Shawahna, R., Samaro, S. & Ahmad, Z. Knowledge, attitude, and practice of patients with type 2 diabetes mellitus with regard to their disease: A cross-sectional study among Palestinians of the West Bank. BMC Public Health 21, 472 (2021).
Vandenbroucke, J. P. et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. PLoS Med. 4, e297 (2007).
Çolak, T. K. et al. Association between the physical activity level and the quality of life of patients with type 2 diabetes mellitus. J. Phys. Ther. Sci. 28, 142–147 (2016).
Praidou, A., Harris, M., Niakas, D. & Labiris, G. Physical activity and its correlation to diabetic retinopathy. J. Diabetes Complicat. 31, 456–461 (2017).
Duarte, C. K., Almeida, J. C., Merker, A. J., de Brauer, F. O. & da Rodrigues, T. C. Physical activity level and exercise in patients with diabetes mellitus. Rev. Assoc. Med. Bras. 58, 215–221 (2012).
Armstrong, T. & Bull, F. Development of the world health organization global physical activity questionnaire (GPAQ). J. Public Health 14, 66–70 (2006).
Bull, F. C., Maslin, T. S. & Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act. Health 6, 790–804 (2009).
Keating, X. D. et al. Reliability and concurrent validity of global physical activity questionnaire (GPAQ): A systematic review. Int. J. Environ. Res. Public Health 16, 4128 (2019).
Rastogi, A., Hiteshi, P. & Bhansali, A. Improved glycemic control amongst people with long-standing diabetes during COVID-19 lockdown: A prospective, observational, nested cohort study. Int. J. Diabetes Dev. Ctries. 40, 476–481 (2020).
Patnaik, L. et al. Effectiveness of mobile application for promotion of physical activity among newly diagnosed patients of type II diabetes–a randomized controlled trial. Int. J. Prev. Med. 13, 54 (2022).
Moniruzzaman, M., Ahmed, M. S. & Zaman, M. M. Physical activity levels and associated socio-demographic factors in Bangladeshi adults: A cross-sectional study. BMC Public Health 17, 59 (2017).
Mengesha, M. M., Roba, H. S., Ayele, B. H. & Beyene, A. S. Level of physical activity among urban adults and the socio-demographic correlates: A population-based cross-sectional study using the global physical activity questionnaire. BMC Public Health 19, 1160 (2019).
Gaskin, C. J. & Orellana, L. Factors associated with physical activity and sedentary behavior in older adults from six low- and middle-income countries. Int. J. Environ. Res. Public Health 15, 908 (2018).
Mabry, R. M., Reeves, M. M., Eakin, E. G. & Owen, N. Gender differences in prevalence of the metabolic syndrome in gulf cooperation council countries: A systematic review. Diabet. Med. 27, 593–597 (2010).
Al Riyami, A. et al. Oman world health survey: Part 1-methodology, sociodemographic profile and epidemiology of non-communicable diseases in oman. Oman Med. J. 27, 425–443 (2012).
Heath, G. W. et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet 380, 272–281 (2012).
da Rocha Fernandes, J. et al. IDF diabetes atlas estimates of 2014 global health expenditures on diabetes. Diabetes Res. Clin. Pract. 117, 48–54 (2016).
Hays, L. M. & Clark, D. O. Correlates of physical activity in a sample of older adults with type 2 diabetes. Diabetes Care 22, 706–712 (1999).
Al-Otaibi, H. H. Measuring stages of change, perceived barriers and self efficacy for physical activity in Saudi Arabia. Asian Pac. J. Cancer Prev. 14, 1009–1016 (2013).
Mabry, R. M., Reeves, M. M., Eakin, E. G. & Owen, N. Evidence of physical activity participation among men and women in the countries of the Gulf cooperation council: A review. Obes. Rev. 11, 457–464 (2010).
Mabry, R. M., Winkler, E. A., Reeves, M. M., Eakin, E. G. & Owen, N. Correlates of Omani adults’ physical inactivity and sitting time. Public Health Nutr. 16, 65–72 (2013).
Sibai, A. M., Costanian, C., Tohme, R., Assaad, S. & Hwalla, N. Physical activity in adults with and without diabetes: from the “high-risk” approach to the “population-based” approach of prevention. BMC Public Health 13, 1002 (2013).
Amin, T. T., Suleman, W., Ali, A., Gamal, A. & Al Wehedy, A. Pattern, prevalence, and perceived personal barriers toward physical activity among adult Saudis in Al-Hassa. KSA. J. Phys. Act Health 8, 775–784 (2011).
El Sharif, N. & Imam, A. in Handbook of Healthcare in the Arab World. (ed. I. Laher) 1–29 (Springer International Publishing, Cham; 2019).
Mikki, N., Shoaibi, A., Khatib, R. & Husseini, A. Assessment of services for diabetes mellitus in clinics in Ramallah, west bank, occupied Palestinian territory: An evaluation study. Lancet 380, S39–S40 (2012).
Acknowledgements
The authors would like to thank the patients who participated in the study. An-Najah National University is acknowledged for making this study possible.
Funding
This study did not receive any specific funding.
Author information
Authors and Affiliations
Contributions
R.S., and M.J. were involved in the conception and design of the work, analysis, and interpretation of data, drafting, and final approval of the manuscript. A.Z. and S.K. were involved in the data acquisition, analysis, drafting of the work and final approval of the version to be published. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shawahna, R., Jaber, M., Zmiro, A. et al. Factors associated with physical inactivity among Palestinians with type 2 diabetes mellitus treated in resource-limited settings. Sci Rep 14, 11256 (2024). https://doi.org/10.1038/s41598-024-60876-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-60876-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.