Abstract
Extracorporeal cardiopulmonary resuscitation (ECPR) is increasingly performed as an adjunct to conventional cardiopulmonary resuscitation (CCPR) for refractory out-of-hospital cardiac arrest (OHCA). However, the specific benefits of ECPR concerning survival with favorable neurological outcomes remain uncertain. This study aimed to investigate the potential advantages of ECPR in the management of refractory OHCA. We conducted a retrospective cohort study involved OHCA patients between January 2016 and May 2021. Patients were categorized into ECPR or CCPR groups. The primary endpoint assessed was survival with favorable neurological outcomes, and the secondary outcome was survival rate. Multivariate logistic regression analyses, with and without 1:2 propensity score matching, were employed to assess ECPR’s effect. In total, 1193 patients were included: 85underwent ECPR, and 1108 received CCPR. Compared to the CCPR group, the ECPR group exhibited notably higher survival rate (29.4% vs. 2.4%; p < 0.001). The ECPR group also exhibited a higher proportion of survival with favorable neurological outcome than CCPR group (17.6% vs. 0.7%; p < 0.001). Multivariate logistic regression analysis demonstrated that ECPR correlated with increased odds of survival with favorable neurological outcome (adjusted odds ratio: 13.57; 95% confidence interval (CI) 4.60–40.06). Following propensity score matching, the ECPR group showed significantly elevated odds of survival with favorable neurological outcomes (adjusted odds ratio: 13.31; 95% CI 1.61–109.9). This study demonstrated that in comparison to CCPR, ECPR may provide survival benefit and increase the odds of favorable neurological outcomes in selected OHCA patients.
Similar content being viewed by others
Introduction
Out-of-hospital cardiac arrest (OHCA) is the leading cause of death and disability worldwide1. Despite advancements in the chain of survival and improvements in cardiopulmonary resuscitation (CPR), the post-OHCA prognosis remains unsatisfactory. For patients receiving conventional CPR (CCPR), statistics reveal a return of spontaneous circulation (ROSC) at 29.7%, survival to hospital admission at 22.0%, and survival to hospital discharge at 8.8%2. In Taiwan, post-resuscitation, only 24.9% exhibited ROSC, 7.8% survived to discharge, with only 3.7% achieve a favorable neurological outcome, with a mere 1% of CPR recipients experiencing a Cerebral Performance Category (CPC) score of 1 or 2 after enduring CPR for more than 35 minutes3.
Extracorporeal CPR (ECPR) through oxygenation and pumping units was initially proposed in 1976 for cardiac arrest patients4. It has increasingly been adopted as an adjunct to CCPR for refractory cardiac arrest5. Observational studies highlight survival benefits associated with ECPR6,7, particularly among OHCA patients with short low-flow duration, shockable rhythms, higher arterial pH value, and lower serum lactate levels8. However, a 2020 Paris registry study reported no discernible difference in post-OHCA survival rates between ECPR and CCPR9. The 2020 ARREST trial, the first randomized controlled trial assessing ECPR, demonstrated that early extracorporeal membrane oxygenation (ECMO)–facilitated resuscitation for OHCA patients with refractory ventricular fibrillation significantly improved survival to hospital discharge compared to standard advanced life support treatment10. Recent meta-analyses have also supported ECPR’s potential to enhance survival and long-term favorable neurologic outcomes in OHCA patients11,12. Nevertheless, subsequent randomized controlled trials reported no significant disparities between CCPR and ECPR in terms of survival with favorable neurological outcomes13,14.
These varying findings suggest that while a subset of patients with refractory arrest benefit from ECPR, unnecessary ECPR engagement may lead to avoidable complications and heightened medical costs. Given the substantial uncertainty in relevant evidence, the 2021 European Resuscitation Guidelines only weakly recommend ECPR in the case of unsuccessful CCPR15. Consequently, this present study aims to investigate the potential advantages of ECPR in achieving favorable outcomes among patients who experienced refractory OHCA.
Methods
Study design and setting
This retrospective cohort study involved individuals admitted to China Medical University Hospital (CMUH) in Taichung, Taiwan, subsequent to experiencing OHCA. CMUH serves as an urban tertiary medical center, witnessing an annual influx of 140,000–160,000 emergency department (ED) visits, with over 400 cases involving OHCA patients receiving CPR. In Taiwan, emergency medical service (EMS) personnel provide prehospital resuscitation, encompassing chest compressions, airway management using bag–valve–mask ventilation or laryngeal mask airway, and defibrillation with automated external defibrillators16. Upon arrival at CMUH’s ED, OHCA patients receive advanced life support adhering to international guidelines17,18, inclusive of endotracheal intubation, CPR, epinephrine administration, and electrical defibrillation. Patients suspected of cardiac causes triggering cardiac arrest, such as shockable rhythms during CPR or ST-elevation myocardial infarction post-ROSC on electrocardiogram, undergo percutaneous coronary intervention. Target temperature management is contemplated for patients achieving ROSC exhibiting impaired consciousness (Glasgow Coma Scale score: < 9) or inability to follow commands.
Ethical declarations
This retrospective study was reviewed and approved by the Research Ethics Committee, China Medical University & Hospital, Taichung, Taiwan (CMUH REC No.: CMUH109-REC2-182). The need for informed consent from study participants was waived by the Research Ethics Committee due to the retrospective nature of the study and the use of de-identified data, ensuring participant anonymity and confidentiality. All procedures were executed in accordance with ethical standards outlined in the Helsinki Declaration of 1975.
Patient selection
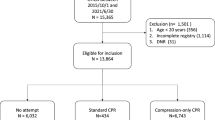
Patients included in the study were those experiencing cardiac arrest and receiving resuscitation at CMUH’s ED between January 2016 and May 2021. Exclusions comprised individuals aged < 20 years, cases of cardiac arrest attributable to circumstantial causes such as trauma, hanging, drowning, intoxication or asphyxia, transferred from other hospitals, and patients without CPR attempted at the ED. Additionally, patients who achieved sustained ROSC within 15 min of advanced life support at the ED were also excluded from this study.
ECPR and relevant variables
OHCA patients were categorized into ECPR and CCPR groups based on whether they received adjunct ECPR. ECPR initiation was activated by an emergency physician and performed by cardiovascular surgeons after verification. Although definitive criteria were absent, consideration for ECPR typically involved patients aged < 65 years, suspected to have arrest from cardiac causes (e.g., acute myocardial infarction and pulmonary embolism), receipt of bystander CPR after collapsing, presentation with shockable rhythms, and an estimated collapse-to-ECMO time of < 100 min.
The Taichung Sudden Cardiac Arrest Registry prospectively registers all OHCA patients following an Utstein-style template19,20,21. The database encompassed demographic details (age and sex; personal medical history), prehospital variables (witness of collapse, location, bystander CPR, and time record of prehospital EMS resuscitation), initial rhythm (shockable or non-shockable rhythm), in-hospital resuscitation parameters (arrival time, initial rhythm, CPR duration, ROSC time), and post-resuscitation care data (target temperature management, percutaneous coronary intervention).
Study outcomes and statistical analysis
The primary outcome assessed was survival with a favorable neurological outcome, defined as a CPC score of 1 or 2 (CPC of 3–5 was defined as unfavorable neurological outcome)22. The secondary outcome was survival rate, defined as survival to hospital discharge (including those transferred to a rehabilitation facility or extended care facility and those requiring home nursing services) or survival for > 30 days23..
Statistical analyses were performed using SAS (version 9.4; SAS Institute, Cary, NC, USA). Significance was set at p value of < 0.05. Categorical variables are presented in terms of numbers and percentages and were compared using the chi-square test. Continuous variables are presented in terms of the median and interquartile range values and were analyzed with Mann–Whitney U test. For the primary outcome, bivariate analysis with the chi-square and Mann–Whitney U tests were performed to identify factors associated with favorable outcome. Factors present before the decision to activate ECPR and those that might influence post-OHCA prognosis were selected for multivariate analysis. A multivariate logistic regression model adjusted for age, OHCA location, bystander CPR, witness of collapse, and initial shockable rhythm was used to evaluate the effect of ECPR on outcomes after OHCA. Propensity score matching was performed for the ECPR and CCPR groups (at a 1:2 ratio) by adjusting for the factors present before the decision of ECPR activation; these factors included age, sex, location, bystander CPR, witness, and shockable rhythms. Propensity score matching was performed using the nearest neighbor method, with the caliper width set at 0.2. After matching, the standardized mean difference was calculated to assess the balance between the ECPR and CCPR groups regarding the covariates. Additionally, the C-statistic was calculated to evaluate the performance of the propensity score matching model. Conditional logistic regression without further adjustment was performed to investigate the effect of ECPR on favorable neurological outcomes after OHCA. Patients were further stratified based on potential prognostic factors following OHCA. Subgroup analyses were conducted using conditional logistic regression for the matched cohort and depicted in a forest plot.
Results
From January 2016 to May 2021, a total of 2613 OHCA patients were admitted to CMUH’s ED. Of these, 1420patients were excluded due to age < 18 years (n = 42), cardiac arrest due to circumstantial causes (n = 172), no CPR attempted at ED (n = 535), transferred from another hospital (n = 72) or achieving sustained ROSC within 15 min at ED (n = 599). The final cohort comprised 1193 patients, with 85 undergoing ECPR and 1108 receiving CCPR. Among them, 104 patients (8.72%) achieved sustained ROSC, and 23 (1.93%) had a favorable neurological outcome (Fig. 1).
Baseline characteristics
Table 1 displays patients’ baseline characteristics. The ECPR group exhibited a younger age (56.0 vs. 71.0 years, p < 0.001), male sex (83.5% vs. 62.5%, p < 0.001) and a higher frequency of OHCA occurrence in public locations (40.0% vs. 14.0%, p < 0.001). Additionally, a higher proportion of patients in the ECPR group experienced witnessed arrests and initial shockable rhythms. Compared to the CCPR group, the ECPR cohort displayed significantly higher rates of sustained ROSC (100.0% vs. 10.4%, p < 0.001), higher proportion of survival (29.4% vs. 2.4%, p < 0.001) and survival with a favorable neurological outcome (17.6% vs. 0.7%, p < 0.001).
Factors associated with favorable outcome
Table 2 presents bivariate analysis for factors potentially associated with favorable neurological outcomes. Patients with refractory OHCA who survived with favorable neurological function were younger, had a higher proportion of witnessed arrests, and presented with initial shockable rhythms. Patients who received ECMO and TTM also had a higher likelihood of achieving favorable outcomes.
Propensity score matching and conditional logistic regression
Following 1:2 propensity score matching, the ECPR and CCPR groups included 77 and 154 patients, respectively, with a C-statics of 0.88. After matching, the ECPR group exhibited higher rates of survival (28.6% vs. 7.8%), and survival with a favorable neurological outcome (18.2% vs. 5.2%) compared to the CCPR group (Table 1).
Multivariate analysis for outcome after refractory OHCA
Multivariate logistic regression for prognosis after refractory OHCA is presented in Table 3. In the original cohort, the ECPR group demonstrated a better chance of survival (adjusted odds ratio [aOR]: 7.84; 95% confidence interval [CI]: 3.83–16.04) as well as favorable neurological outcomes (aOR: 13.57; 95% CI: 4.60–40.06). Following propensity score matching, the ECPR group continued to exhibit a higher proportion of favorable neurological outcomes (aOR: 13.31; 95% CI: 1.61–109.9) and survival rates (aOR: 6.02; 95% CI: 2.19–16.52) in the conditional logistic regression analysis. Figure 2 summarized the comparison of primary outcome between the ECPR and CCPR groups.
Survival with a favorable neurological outcome among patients with refractory out-of-hospital cardiac arrest receiving extracorporeal or conventional CPR. Among 1193 patients with out-of-hospital cardiac arrest, 85 received extracorporeal CPR. These patients demonstrated a higher proportion of survival with a favorable neurological outcome than those receiving conventional CPR. CPR, cardiopulmonary resuscitation.
Factors affecting neurological outcome in ECPR patients
Table 4 illustrates factors influencing a favorable neurological outcome in ECPR patients. Younger age (48.0 vs. 58.5 years, p = 0.001), CPR duration (37.0 vs. 51.0 min, p = 0.006) and collapse to ECMO flow initiation time (76.0vs. 98.0 min, p = 0.031) were associated with higher rates of a favorable neurological outcome.
Subgroup analysis
The effect of ECPR on favorable neurological outcomes after propensity score matching was illustrated in Fig. 3. A greater likelihood of achieving a favorable outcome was observed in the ECPR group among patients aged < 65 years, males, and those with an initial shockable rhythm. However, there was no significant difference in prognosis between ECPR and CCPR for patients with witnessed arrest, those who received bystander CPR, or those who experienced arrest in public places. Conversely, the ECPR group demonstrated improved outcomes among patients without a witnessed arrest, those who did not receive bystander CPR, and those whose arrest occurred in non-public locations.
Forrest plot of subgroup analysis for favorable neurological outcome. Shown are the analysis of primary outcome (survival with a favorable neurological function) in prespecified subgroups. The forest plot shows the adjusted odds ratio derived from the multivariate logistic regression. The horizonal bar represent 95% confidence intervals. ECPR, extracorporeal cardiopulmonary resuscitation; CCPR, conventional cardiopulmonary resuscitation. ECPR, extracorporeal cardiopulmonary resuscitation; CCPR, conventional cardiopulmonary resuscitation.
Discussion
Our investigation revealed higher survival rate and a greater probability of survival with a favorable neurological outcome in refractory OHCA patients who underwent ECPR compared to those receiving CCPR. This study represents a relatively large single-center inquiry into the efficacy of ECPR in treating refractory OHCA patients and is among the few to use propensity score matching. Even after propensity score matching, the distinction in prognosis between the CCPR and ECPR groups persisted significantly in the multivariate analysis.
Evidence suggests that patients with refractory OHCA can benefit from ECPR. Retrospective studies utilizing propensity score matching suggested that OHCA patients undergoing ECPR have more favorable prognosis than those who are treated with CCPR7,24,25. A recent meta-analysis of randomized and propensity score matching studies revealed that 14% of all patients in the ECPR group survived with a favorable neurological outcome compared with only 7.8% in the CCPR group12. Consistent with these findings, our results from this single-center observational study, utilizing propensity score matching, indicated that ECPR can improve post-OHCA prognosis. Despite the limitations of a single-center study with a relative smaller sample size, it advantages lie in standard care protocols, complete patient data, consistent medical care quality, precise timing, and definitive diagnosis. These factors were considered in our propensity score matching, which facilitated an objective comparison of the ECPR and CCPR groups in terms of outcomes.
The ARREST trial reported a higher survival to hospital discharge rate in ECPR group compared to the CCPR group10. However, subsequent randomized controlled trials such as the Prague trial26 and the INCEPTION trial14 indicated no discernible differences in neurological recovery between the two groups. This discrepancy may be due to the differences in the time from collapse to ECMO flow, which was 59 min in the ARREST trial but 62 and 74 min in the Prague and INCEPTION trials, respectively. In our study, this duration was notably longer at 92 min, much longer than these trials as well as that reported in a Korean nationwide registry study27. This was primarily because of the longer time from ECMO team activation to the start of ECMO flow in our study than in the other studies; this delay is caused mainly by our protocol of surgeon verification for ECMO implantation, which involves discussion with the patient’s family, rather than direct activation. Although our findings revealed substantial benefits of ECPR, survival rate and favorable neurological outcomes were lower in our study than in the ARREST and Prague trials. Thus, a prepared ECMO team and protocolized team activation process may be beneficial.
Divergence among previous studies could also arise from discrepancies in the inclusion criteria for ECPR activation. For instance, the ARREST trial included only patients with ventricular arrhythmia failing to achieve ROSC after three defibrillation attempts10. The INCEPTION trial also included patients with ventricular arrhythmia but enrolled those who experienced refractory cardiac arrest despite 15 min of advanced life support14. On the other hand, the Prague trial enrolled both patients with ventricular arrhythmia and those without it, defining refractory arrest as failure to achieve ROSC after 5 min of advanced life support26. In current study, we included patients without sustained ROSC after 15 min of advanced life support and demonstrated the benefit of ECPR on favorable after OHCA, especially in patients younger than 65 years old, male sex and presenting with initial shockable rhythms. However, among patients with witnessed arrest, bystander CPR, and arrest at a public location, the proportions of surviving with favorable neurological outcome were comparable between the CCPR and ECPR groups This could be due to the influence of various factors on patient outcomes, such as the quality of chest compressions, duration of no-flow and low-flow time, early defibrillation, and the cause of cardiac arrest.28,29,30. Additionally, the ECPR activation was at the discretion of physicians, prioritizing patients with a relatively high likelihood of achieving a favorable outcome. This decision-making process may also confound the effect of ECPR on neurological outcomes. Collectively, findings from the Prague trial, INCEPTION trial, Paris registry study, and our investigation suggest that activation of ECPR may provide benefit for selected patient of refractory OHCA.
We also identified factors predictive of neurological recovery in ECPR patients. Consistent with previous study31, the median CPR duration in our study was significantly shorter among patients with a favorable neurological outcome (37.0 min) than among those with an unfavorable neurological outcome (51.0 min). Furthermore, we observed younger age, and shorter collapse to ECMO flow initiation, were associated with favorable neurological outcomes, consistent with the results of previous study32. Age emerged as a crucial prognostic factor across all OHCA patients19. We observed that in the ECPR group, patients exhibiting neurological recovery tended to be younger than those not exhibiting neurological recovery.
Nonetheless, our study presents several limitations. Being retrospective, the study lacked stringent criteria for ECPR activation, leading to varied demographic characteristics, comorbidities, and prognostic parameters between the ECPR and CCPR groups. The decision-making process regarding whether to activate ECPR, the presence of signs of life, and the level of end-tidal carbon dioxide were not documented in the electronic medical records. Despite propensity score matching, potential selection bias cannot be completely rule out. Moreover, due to the limited ECPR cases, statistical analysis might have lacked sufficient power to discern differences in prognostic factors within the ECPR group. The longer time from collapse to ECMO flow in our study compared to previous studies might also impact the outcomes. At our institute, the consensus time window for ECPR is < 100 min from collapse to ECMO flow. A nationwide multicenter study from Denmark, which also used the consensus criteria for ECPR with a similar median low-flow time of 105 min, reported a high survival rate with favorable neurological outcome34; this finding is consistent with ours. The present study may serve as a valuable reference for institutes without strict activation criteria and for patients with OHCA requiring transportation for ECMO. Lastly, despite the advantage of consistency in resuscitation and postresuscitation care, the use of a single-center registry limits the generalizability of our results. Future larger-scale multicenter studies or those using nationwide databases are warranted.
Conclusions
Base on the current propensity score–matched analysis, ECPR may enhance the odds of survival with favorable neurological outcome in selected patients with refractory OHCA. Additional investigation is required to determine optimal criteria for identifying appropriate candidates for ECPR.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Berdowski, J., Berg, R. A., Tijssen, J. G. & Koster, R. W. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 81, 1479–1487 (2010).
Yan, S. et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit. Care (Lond., Engl.) 24, 61. https://doi.org/10.1186/s13054-020-2773-2 (2020).
Lin, H.-Y. et al. Outcomes of out-of-hospital cardiac arrests after a decade of system-wide initiatives optimising community chain of survival in Taipei city. Resuscitation 172, 149–158 (2022).
Mattox, K. L. & Beall, A. C. Resuscitation of the moribund patient using portable cardiopulmonary bypass. Ann. Thoracic Surg. 22, 436–442. https://doi.org/10.1016/s0003-4975(10)64452-9 (1976).
Richardson, A. S. et al. ECMO cardio-pulmonary resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation 112, 34–40. https://doi.org/10.1016/j.resuscitation.2016.12.009 (2017).
Maekawa, K., Tanno, K., Hase, M., Mori, K. & Asai, Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit. Care Med. 41, 1186–1196. https://doi.org/10.1097/CCM.0b013e31827ca4c8 (2013).
Patricio, D. et al. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: a retrospective propensity score matched study. Crit. Care 23, 27. https://doi.org/10.1186/s13054-019-2320-1 (2019).
Debaty, G. et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation 112, 1–10. https://doi.org/10.1016/j.resuscitation.2016.12.011 (2017).
Bougouin, W. et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur. Heart J. 41, 1961–1971. https://doi.org/10.1093/eurheartj/ehz753 (2020).
Yannopoulos, D. et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet 396, 1807–1816. https://doi.org/10.1016/S0140-6736(20)32338-2 (2020).
Alfalasi, R. et al. A comparison between conventional and extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: A systematic review and meta-analysis. Healthcare https://doi.org/10.3390/healthcare10030591 (2022).
Scquizzato, T. et al. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: A systematic review and meta-analysis of randomized and propensity score-matched studies. Artif. Organs 46, 755–762 (2022).
Belohlavek, J. et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest a randomized clinical trial. JAMA 327, 737–747. https://doi.org/10.1001/jama.2022.1025 (2022).
Suverein, M. M. et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N Engl J Med 388, 299–309. https://doi.org/10.1056/NEJMoa2204511 (2023).
Lott, C. et al. European resuscitation council guidelines 2021: Cardiac arrest in special circumstances. Resuscitation 161, 152–219. https://doi.org/10.1016/j.resuscitation.2021.02.011 (2021).
Huang, T.-L. et al. Emergency medical services in Taiwan: Past, present, and future. J Acute Med 13, 91–103 (2023).
Panchal, A. R. et al. Part 3: Adult basic and advanced life support: 2020 American Heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 142, S366–S468. https://doi.org/10.1161/CIR.0000000000000916 (2020).
Link, M. S. et al. Part 7: Adult advanced cardiovascular life support: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132, S444-464. https://doi.org/10.1161/CIR.0000000000000261 (2015).
Shih, H. M. et al. Derivation and validation of the SWAP score for very early prediction of neurologic outcome in patients with out-of-hospital cardiac arrest. Ann. Emerg. Med. 73, 578–588. https://doi.org/10.1016/j.annemergmed.2019.01.017 (2019).
Huang, S. K. et al. Dispatcher-assisted cardiopulmonary resuscitation: Differential effects of landline, Mobile, and transferred calls. Resuscitation 146, 96–102. https://doi.org/10.1016/j.resuscitation.2019.11.008 (2020).
Cummins, R. O. et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 84, 960–975 (1991).
Raina, K. D., Callaway, C., Rittenberger, J. C. & Holm, M. B. Neurological and functional status following cardiac arrest: method and tool utility. Resuscitation 79, 249–256. https://doi.org/10.1016/j.resuscitation.2008.06.005 (2008).
Tsai, M. F., Yu, S. H., Sie, J. S., Huang, F. W. & Shih, H. M. Prognostic value of early and late spontaneous conversion into a shockable rhythm for patients with out-of-hospital cardiac arrest. Am. J. Emerg. Med. 61, 192–198. https://doi.org/10.1016/j.ajem.2022.09.025 (2022).
Kim, S. J. et al. Association between extracorporeal membrane oxygenation (ECMO) and mortality in the patients with cardiac arrest: A nation-wide population-based study with propensity score matched analysis. J. Clin. Med. https://doi.org/10.3390/jcm9113703 (2020).
Choi, D. S. et al. Extracorporeal life support and survival after out-of-hospital cardiac arrest in a nationwide registry: A propensity score-matched analysis. Resuscitation 99, 26–32. https://doi.org/10.1016/j.resuscitation.2015.11.013 (2016).
Belohlavek, J. et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: A randomized clinical trial. Jama 327, 737–747. https://doi.org/10.1001/jama.2022.1025 (2022).
Choi, Y. et al. Extracorporeal cardiopulmonary resuscitation for adult out-of-hospital cardiac arrest patients: Time-dependent propensity score-sequential matching analysis from a nationwide population-based registry. Crit. Care 27, 87. https://doi.org/10.1186/s13054-023-04384-y (2023).
Martinell, L. et al. Early predictors of poor outcome after out-of-hospital cardiac arrest. Crit. Care 21, 96. https://doi.org/10.1186/s13054-017-1677-2 (2017).
Maupain, C. et al. The CAHP (Cardiac Arrest Hospital Prognosis) score: A tool for risk stratification after out-of-hospital cardiac arrest. Eur. Heart J. 37, 3222–3228. https://doi.org/10.1093/eurheartj/ehv556 (2016).
Adrie, C. et al. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: the OHCA score. Eur. Heart J. 27, 2840–2845. https://doi.org/10.1093/eurheartj/ehl335 (2006).
Wengenmayer, T. et al. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit. Care 21, 157. https://doi.org/10.1186/s13054-017-1744-8 (2017).
Bertic, M. et al. Predictors of survival and favorable neurologic outcome in patients treated with eCPR: A systematic review and meta-analysis. J. Cardiovasc. Transl. Res. 15, 279–290. https://doi.org/10.1007/s12265-021-10195-9 (2022).
Debaty, G. et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation 112, 1–10. https://doi.org/10.1016/j.resuscitation.2016.12.011 (2017).
Mork, S. R. et al. Mechanical circulatory support for refractory out-of-hospital cardiac arrest: a Danish nationwide multicenter study. Crit. Care 25, 174. https://doi.org/10.1186/s13054-021-03606-5 (2021).
Acknowledgements
We would like to express our appreciation for all the efforts and contributions to the study support from the Taichung Sudden Cardiac Arrest Registry and Taichung Fire Department.
Funding
This work was supported by the grant from Taiwan’s Ministry of Science and Technology (MOST 111–2314-B-039–071) and China Medical University Hospital (DMR-112–069). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
H-M. S. Performed statistical analysis, wrote manuscript, tables, and figures. W-J. L. Wrote manuscript and re-checked the data prior to the analysis. Y-C. L. Provided resources and methodology. K-C. C. Provided formal analysis and validation. S–S. C. Contributed to the conceptualization and investigation. S–H. Y. Contributed to the review and editing, Resources, Methodology, Conceptualization, Project administration, and Funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shih, HM., Lin, WJ., Lin, YC. et al. Extracorporeal cardiopulmonary resuscitation for patients with refractory out-of-hospital cardiac arrest: a propensity score matching, observational study. Sci Rep 14, 9912 (2024). https://doi.org/10.1038/s41598-024-60620-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-60620-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.