Abstract
Neurodegenerative diseases (NDDs) are characterized by neuronal damage and progressive loss of neuron function. Microbiome-based interventions, such as dietary interventions, biotics, and fecal microbiome transplant, have been proposed as a novel approach to managing symptoms and modulating disease progression. Emerging clinical trials have investigated the efficacy of interventions modulating the GM in alleviating or reversing disease progression, yet no comprehensive synthesis have been done. A systematic review of the literature was therefore conducted to investigate the efficacy of microbiome-modulating methods. The search yielded 4051 articles, with 15 clinical trials included. The overall risk of bias was moderate in most studies. Most microbiome-modulating interventions changed the GM composition. Despite inconsistent changes in GM composition, the meta-analysis showed that microbiome-modulating interventions improved disease burden (SMD, − 0.57; 95% CI − 0.93 to − 0.21; I2 = 42%; P = 0.002) with a qualitative trend of improvement in constipation. However, current studies have high methodological heterogeneity and small sample sizes, requiring more well-designed and controlled studies to elucidate the complex linkage between microbiome, microbiome-modulating interventions, and NDDs.
Similar content being viewed by others
Introduction
Neurodegenerative diseases (NDDs) are a diverse spectrum of disorders characterized by the progressive loss of neurons and deterioration in the central or peripheral nervous system, resulting in long-term motor and nonmotor impairments1. NDDs include Parkinson’s disease (PD), Alzheimer’s disease (AD), frontotemporal dementia and its variants, amyotrophic lateral sclerosis (ALS), and multiple sclerosis (MS). As the population ages, the incidence rate and prevalence of NDDs increase modestly, as demonstrated by an incidence estimated annual percentage changes of 0.52 for PD and 0.13 in men and 0.06 in women for AD2,3. Affecting millions of people worldwide, NDDs are a major public health concern; yet, despite decades of research effort, no effective treatments for curing or reversing their progression have been realized3. The exact pathophysiology of NDDs is also not fully elucidated owing to the heterogeneity and complexity of these diseases4,5,6. However, emerging evidence suggests that the gut microbiome (GM), the collection of microorganisms that inhabit the gastrointestinal (GI) tract, may play a role in modulating the risk and severity of NDDs.
GM, often called the second brain, harbors nearly 100 trillion bacteria, yeast, and other microorganisms, functioning symbiotically in day-to-day activities7. Host genetics, lifestyle, and environmental factors, such as diet, chemical exposure, infection, and host comorbidity, shape GM through the modulation of gut motility and secretion, which in turn affects various aspects of the host physiology, including immunomodulation, metabolic activity, and neuronal development and function. The connection between GM and metabolic and immune-related diseases is well established8. For example, obesity, as a complex metabolic disorder, is associated with decreased diversity and richness and altered composition in GM9. Wells et al. also identified that Prevotella correlates with the genetic risk and anticitrullinated protein antibody level of rheumatoid arthritis, suggesting the role of Prevotella as a potential mediator in disease progression10.
A growing body of evidence has suggested that GM also communicates bidirectionally via multiple pathways, which collectively is described by the gut–brain axis. The brain communicates with the gut through neuronal and hormonal pathways, including the hypothalamic pituitary adrenal axis (HPA) and sympathoadrenal axis11. The vagal nerves relay most signals from the brain to the gut12 and coordinate stress and anti-inflammatory activities with HPA to regulate gut motility, intestinal permeability, and mucosal immune activity13. At the same time, GM can affect the brain by producing and releasing various molecules, such as metabolites, neurotransmitters, and cytokines; these molecules can reach the brain through multiple pathways and may be a key modulator in NDDs14.
Disruption of GM balance caused by host and environmental factors may lead to diseases or disorders15. Romano et al. performed a meta-analysis of 21 case–control studies to compare the GM composition of 1083 PD patients and 1213 healthy controls and revealed a lower abundance of Prevotellaceae and Lachnospiraceae families and higher abundance of Enterobacteriaceae and Akkermansiaceae families in patients than in controls16. Similarly, patterns of dysbiosis in other NDDs, including AD, MS, and ALS, have been reported in recent systematic review and meta-analysis17,18,19. Sampson et al. reported the requisite involvement of gut microbiota to elicit synucleinopathies in a PD model using wild-type and Thy1-α-synuclein genotype mice, in which the germ-free Thy1-α-synuclein genotype demonstrated limited motor and GI dysfunction compared with specific pathogen-free counterparts20. These findings suggest that GM may play a key role in the pathophysiology of NDDs, and modulating GM may be a potential strategy for preventing or treating NDDs.
However, many challenges and limitations remain in this research field. For example, most animal studies rely on germ-free or genetic models of NDDs, which may not fully recapitulate the human disease phenotypes or etiologies21. Standardized methods for assessing and manipulating GM across different studies are also lacking. Meanwhile, human studies, are mostly observational and cross-sectional, which cannot establish causality or directionality between GM and NDDs22.
In the recent decade, clinical trials have been conducted to investigate the efficacy of interventions modulating GM in alleviating or reversing disease progression. Yet, comprehensive synthesis of the available evidence in understanding microbiome-modulating methods is lacking. Therefore, this systematic review aims to summarize and critically appraise the current evidence regarding the effects of microbiome-modulating interventions on NDD-related clinical outcomes and to discuss the translatability and implementation potentials for future research and clinical application.
Methods
Inclusion criteria and search strategy
This protocol-based systematic review (PROSPERO ID: CRD42023437490) was conducted and reported in accordance with the Cochrane Handbook for Systematic Reviews of Interventions23 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement24. Studies were selected in accordance with predefined inclusion and exclusion criteria. Randomized controlled trials (RCTs), quasi-experimental studies, single-arm studies, and pilot studies with microbiome-modulating intervention were included if studies (1) were conducted in adults (age > 18 years) with a diagnosis of NDDs, such as AD, PD, MS, and ALS, and (2) reported any microbiome outcomes. Microbiome-modulating intervention is defined as any treatment or intervention that alters the composition, diversity, or functionality of GM. The intervention can be, but not limited to, changes in diet or lifestyle, use of biotics, fecal microbiota transplantation (FMT), or other medications. The methods of microbiome analysis are not restricted, which may include, but not limited to, 16S ribosomal (r) RNA sequencing, shotgun metagenomic sequencing, and fluorescence in situ hybridization. Studies were excluded if they were not published in English.
PubMed, Ovid-Embase, and Web of Science were searched from inception to January 11, 2023. The search strategy was summarized as follows: [neurodegenerative diseases] AND [microbiome assessment] AND [microbiome-modulating methods: (diet) OR (supplement or biotics) OR (FMT)]. Online Resource 1 presents the full search strategy. Duplicate records were removed with EndNote and manually.
Data extraction and quality assessment
Two independent reviewers (ZSW Chui and EWH Zhang) extracted data from each trial using a pre-specific, standardized form and evaluated the risk of bias via the Cochrane Risk-of-Bias Tool 2 for RCTs25 and the Risk Of Bias In Nonrandomized Studies of Interventions (ROBINS-I) for non-RCTs26. Discrepancies were identified and resolved by consensus with a third reviewer (LML Chan) and the supervisor (JYY Kwok).
Synthesis
A narrative synthesis was conducted for all trials to describe study design, country and setting of study, characteristics of participants and interventions, assessment time points, microbiota sequencing technique, main microbiota, and clinical outcomes (Table 1). Meta-analyses were performed among microbiota and clinical outcomes if they were reported by at least three studies. In view of wide variations in instruments used between trials to assess the primary outcomes, pooled effects were summarized as standardized mean differences (SMDs). SMD is a summary statistic used to report intervention effects in standardized units, rather than the original units of measurement for each scale. The total sample size, mean with standard deviation (SD) or median, and interquartile range of disease progression pre- and post-intervention were extracted to calculate SMD and SD. Twenty-five individual study results were corrected for directionality when appropriate. Considering the substantial variations in microbiome-modulating interventions and study design, we utilized a random-effect model to conduct the analysis using RevMan 5.427,28. All significance tests were 2-tailed, and P value of < 0.05 was considered statistically significant. The heterogeneity among studies was assessed using I2 statistic.
Results
Study selection
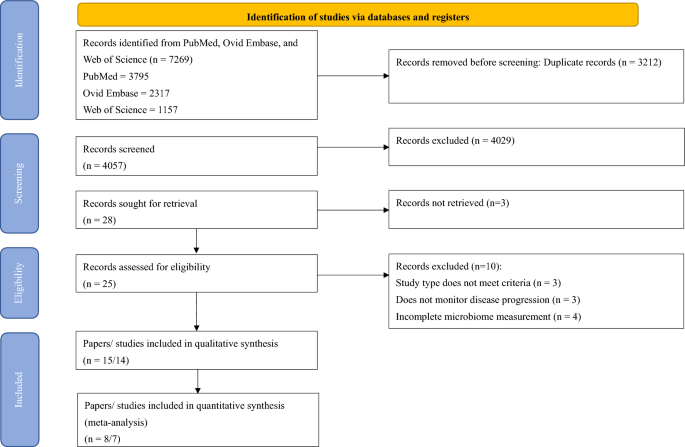
The PRIMSA 2020 flow diagram (Fig. 1) shows the flow of the study selection process. A total of 7269 unique records identified from the search, of which 25 were deemed eligible for full review. Fourteen trials were included for qualitative synthesis. Seven trials were included in the meta-analyses.
Study characteristics
Table 1 shows a systematic presentation of information regarding the study characteristics. Fifteen articles comprised 14 trials that involved 445 patients: 5 trials/6 articles on sclerosis (n = 112), 6 trials on PD (n = 235), and 3 trials on AD and related disorders (n = 98). Of the 14 trials, 6 studies adopted single-arm design, 5 studies were RCT, and 3 were non-RCT.
Quality assessment
The quality of the methodology and risk of bias of the 15 articles were assessed in accordance with Cochrane RoB2 for randomized trials and ROBINS-I for nonrandomized trials25,26 (Table 2 and 3).
Bias in the selection of reports is a common concern among studies; here, three out of five RCTs and seven out of nine non-RCTs were of moderate-to-high risk in the concerning domain owing to multiple measurements of disease progression. In general, RCTs had a lower risk of bias, in which no high-risk RCTs were included. The RCT performed by Al et al. was terminated early because of the sudden death of the principal investigator22; nevertheless, results were analyzed in such a way that no directional bias toward or against the intervention exists, and this RCT was therefore assessed to have a moderate risk.
For non-RCTs, 66.78% of the studies were of serious risk of bias, and the remaining were of moderate risk29,34,36,39,40,42. Apart from reporting bias (D7), major concerns of bias included confounding bias (D1), selection bias (D2), and bias in data measurement (D6). Serious confounding bias mainly contributed to the lack of control of diet, which can affect the microbiome composition, leading to less conclusive results. In addition, many of the non-RCTs relied on self-reporting, while the participants were aware of the interventions. Becker et al. conducted an open-label study to modify GM in PD patients with resistance starch and collected subject-reported nonmotor data; consequently, the measurement could be inaccurate owing to subjective reporting34. Poor selection of participants and missing data were also common among nonrandomized clinical trials.
MS and amyotrophic lateral sclerosis
Five studies focusing on MS22,29,30,31,32 and one study specifically on ALS33 were included. These studies comprised three RCTs22,32,33 and two single-arm studies29,30,31. The sample sizes of MS studies were small, ranging from 922 to 2230,31, whereas the study on ALS recruited 50 samples33. The study durations varied from 1 week29 to 1 year22. A spectrum of microbiome-modulating interventions were used, ranging from probiotic supplementation30,31,33, dietary intervention (intermittent fasting)32, FMT22, and a multidimensional program consisting of dietary intervention and physical activities29. All studies used 16 s rRNA sequencing to analyze microbiome composition, covering V3 and/ or V4 regions. In addition to V3 and V4 regions, V13 region was also covered by Cignarella et al. to distinguish specific species of Lactobacillus, as well as V1 and V2 regions32.
MS is characterized with chronic inflammatory response in the central nervous system, which leads to pronounced Th1/Th17-mediated inflammation and increased proinflammatory cytokine concentration43,44. Therefore, improvement in MS progression can be evaluated by measuring inflammatory response and clinical functional and nonfunctional outcomes. Three out of four studies focusing on MS reported reduced inflammatory response or improved autoimmune response29,30,31,32, while the remaining underpowered study showed insignificant difference post-modulation22.
All of the studies had diverse microbiome patterns. The two studies on probiotic supplementation showed time-related changes in microbiome composition but had different microbiota outcomes despite using similar bacterial families, that is, Di Gioia et al. used Streptococcaceae and Lactobacillaceae families, while Tankou et al. used Bifidobacteriaceae family in addition to Streptococcaceae and Lactobacillaceae families30,31,33. Di Gioia et al. found no significant alterations in microbiota and probiotic supplementation, except for Rikenellaceae and trends of increase in Bateroidaceae and decrease in Prevotellaceae and Clostridiales, and no clinical improvement in ALS33. Tankou et al. reported enrichment of Lactobacillaceae, Streptococcaceae, and Bifidobacteriaceae and reduction of Akkermansia, Blautia, and Dorea, which were enriched in MS patients at baseline. They also observed reduced intermediate monocytes, increased effector memory CD8 T cells, and anti-inflammatory gene expression, with some association with microbiome changes, therefore suggesting an implication of synergistic effect with current therapies30,31.
Dietary interventions significantly improved disease progression and inflammatory tone in both studies29,32. Cignarella et al. reported increased Faecalibacterium, Lachnospiracea incertae sedis, and Blautia, improved Expanded Disability Status Scale (EDSS), and reduced serum leptin and peripheral blood leukocyte profile changes after 15 days of intermittent fasting in conjunction with corticosteroid treatment32. However, the difference in improvement of EDSS between the ad libitum control group and the intermittent fasting group was insignificant, and the MS Functional Composite was insignificantly different from the baseline in both groups, possibly due to the short intervention duration32. Barone et al. conducted a 1-week multidimensional program involving Mediterranean diet, neuromotor rehabilitation, and mindfulness29. They reported partial recovery of gut dysbiosis with reduced Collinsella, Actinobacteria, and Ruminococcus and increased Bacteroidetes and some short-chain fatty acid (SCFA) producers. They also observed reduced inflammatory tone and serum lipopolysaccharide, increased anti-inflammatory gene expression, and some associations with microbiome changes. Considering the significant improvement in the total score in the Modified Fatigue Impact Scale, the author concluded that the multidimensional approach may be effective in mitigating MS progression.
Al et al. conducted an RCT on FMT, in which they randomized participants into early (received FMT with 6-month follow-up, n = 4) or late intervention group (6-month observation, substantiated by FMT and 1-month follow-up, n = 5); however, the study was terminated early and underpowered because of the unexpected death of the principal investigator22. Preliminary results showed that FMT was well-tolerated without serious adverse events. Microbiome changes recapitulated the microbiome composition of the donor and had the potential to improve elevated intestinal permeability. Insignificant clinical changes were noted on disease severity measured by EDSS, without new MRI activity, and the inflammatory levels in terms of serum cytokines showed insignificant changes.
PD
We identified six articles that fulfilled all criteria34,35,36,37,38,39. They included one RCT38, two non-RCT34,36, and three single-arm studies35,37,39, which used diversified microbiome-modulating methods, including prebiotics, FMT, dietary interventions, and probiotics. The sample size was in the range of 8–11 for non-RCTs and single-arm studies and 87–100 for RCTs. The study lasted 7 weeks to 1 year.
Two of the studies investigated GM with metagenomic sequencing34,38, while others used 16 s rRNA sequencing, despite sequencing different variable regions. Although different interventions were used, the alpha and beta diversities did not differ significantly in all studies. No consensus existed in terms of the change in a particular family, genus, or species.
Despite using different microbiome-modulating strategies, these studies showed a significant impact on alleviating disease burden. Motor functions, as measured by Unified PD Rating Scale (UPDRS), were significantly improved in four of the six studies that used FMT, probiotics, ovo-lacto diet, ovo-lacto diet with enema, and Mediterranean diet35,36,38,39, while others did not measure motor function. Apart from the study that used resistant starch34, constipation and GI-related symptoms were also improved in the three studies that used probiotics, FMT, and Mediterranean diet35,37,38. Other nonmotor symptoms, including anxiety and depression, were improved34,35,38, and inflammatory and PD-related fecal markers decreased34,39.
Sun et al. provided the only RCT that measured motor, nonmotor, and constipation symptoms, as well as microbiome-related metabolites38. Their study evaluated the synergistic effects of probiotics with conventional PD treatment (benserazide and dopamine agonist) by comparing it with a placebo group (placebo with conventional regimen) for 3 months. The probiotics led to increased Bifidobacterium animalis, Ruminococcaceae, and Lachnospira and decreased Lactobacillus fermentum and Klebsiella oxytoca, which might be related to changes in microbiome-related metabolites and neurotransmitter, consequently leading to a beneficial effect in PD patients.
AD
Three included studies focused on AD or mild cognitive impairment, and the study designs were diversified: one single-arm42, RCT41, and non-RCT40. Changes in microbiome were measured by qPCR of designated microbial targets42, 16 s rRNA41, and histology and urease test of Helicobacter pyroli40. Given that the focus of the studies varied, they also modified GM with different approaches, including probiotic supplementation42, dietary treatment41, and antibiotic treatment40. The sample sizes ranged from 1741 to 6140, and the studies lasted for 4 weeks42 to 2 years40.
Leblhuber et al. investigated the effects of probiotic supplementation on immune activation42. They found that 4-week probiotic supplementation led to increased Faecalibacterium prausnitzii and altered tryptophan metabolites, yet no significant improvement in cognition was observed. Nagpal et al.41 was the only cross-over study to compare the effects of Mediterranean-keto diet (MMKD) on AD markers. They found increased abundance of several bacterial families and genera, such as Enterobacteriaceae, Akkermansia, and Slackia, after modified MMKD compared with that after American Heart Association Diet (AHAD), which also altered the SCFA profile and was in association with CSF biomarkers, such as Ab40 and Ab42. Kountouras et al. focused on the impact of eradication of H. pylori in infected AD patients45. AD patients were significantly more susceptible to H. pylori infection, and the eradication therapy led to improved cognitive and functional status upon the 2-year clinical endpoint compared with infected patients. These studies suggested that modulating GM may alter AD progression via modifying SCFA and immune profile, leading to reduced AD marker and possibly improved status.
SCFA producers and fecal/serum SCFAs
Several included studies have explored the relationship between SCFA producers or fecal/serum SCFA concentration in NDDs. Of the eight studies that reported changes in SCFA producers or SCFA concentration, six reported improved outcomes, as measured by inflammatory tone, functional outcome, or GI symptoms, yet showed inconsistent changes in SCFA producers and SCFA concentration (Table 4).
Tankou et al. and Rusch et al. reported decreased Blautia after probiotic supplementation and Mediterranean diet, respectively30,31,37. Barone et al. reported a stable level of Blautia after multidimensional rehabilitation29. Kuai et al. and Cignarella et al. reported increased Blautia after FMT and intermittent fasting32,35. All of them, except Cignarella et al., reported improved clinical outcomes. Faecalibacterium was reported to have increased significantly in three studies after intermittent fasting, FMT, and probiotic supplementation. Sun et al. reported increased diversity of SGBs involved in SCFA synthesis after probiotic supplementation, in which the acetate and dopamine concentrations increased significantly, whereas the glutamine and tryptophan concentrations decreased38. The patients also exhibited improved clinical outcomes.
Meta-analysis: effect of microbiome modulation on clinical outcomes
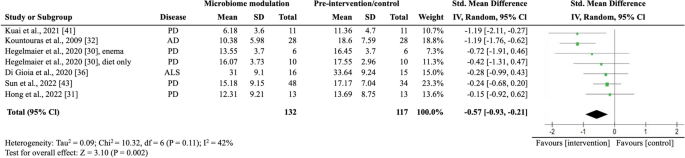
We pooled all clinical trials to investigate the overall effectiveness of modulating the microbiome on motor symptom progression in NDD. Of the eight studies that assessed motor symptom progression, five (62.5%) reported statistically significantly improvements in motor symptom progression. We pulled all studies that reported motor symptom progression quantitatively before and after intervention and extracted the mean, interquartile range, or SD to calculate the standard mean differences of the studies, resulting in six studies. We did not include Al et al.’s study in meta-analysis, despite the reported EDSS, due to the study’s early termination, which resulted in incomplete and varied treatment conditions in the two groups22. Additionally, we excluded the study conducted by Cignarella et al. as it did not report numerical data for EDSS32. In the meta-analysis involving six studies with seven intervention groups (n = 249), microbiome-modulating interventions were significantly associated with a lower motor symptom burden (SMD, − 0.57; 95% CI − 0.93 to − 0.21; I2 = 42%; P = 0.002; Fig. 2). They used different strategies, such as probiotics, antibiotics, FMT, and dietary changes, to alter the gut microbiota33,35,36,38,39,40. Four out of the six studies included patients with PD30,31,35,36,39, and the remaining involved patients with ALS33 and AD40. The primary outcome measures were UPDRS for PD, ALS Functional Rating Scale-Revised for ALS, and Functional Rating Scale for Symptoms of Dementia for AD. Hegelmaier et al. compared the clinical outcomes of PD patients receiving ovo-lacto diet, with a subgroup receiving additional enema36. Considering that the aim of this meta-analysis was to study the pooled effect of microbiome-modulating methods, we compared the clinical outcomes before and after interventions and segregate the enema subgroup. We did not include studies on MS because they did not report numerical results on functional outcomes or were underpowered.
Random-effects meta-analysis of trials on the association between microbiome modulating intervention and clinical outcomes. AD Alzheimer’s disease; ALS amyotrophic lateral sclerosis; IV inverse variance; PD Parkinson’s disease; error bars represent 95% CIs; size of the shaded square indicates study weight; diamond represents pooled standardized mean difference and 95% CI.
Constipation and GI symptoms
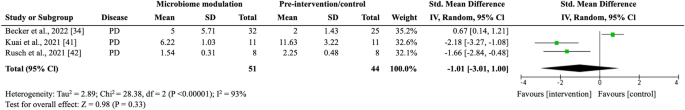
Of the four trials that assessed constipation and GI-related symptoms33,34,35,37, three studies reported significant improvement compared with the baseline or placebo, whereas the remaining reported insignificant changes in bowel habits. The meta-analysis did not include Hegelmaier et al.’s study because they used the Bristol stool scale, a noncontinuous scale, in measuring constipation syndrome36. In the meta-analysis involving three trials (n = 76), microbiome-modulating interventions were insignificantly associated with improving constipation (SMD, − 1.01; 95% CI − 3.01 to 1.00; I2 = 93%; P = 0.33; Fig. 3). The primary outcome measures included the Constipation Scoring System34, Wexner35, and GI Symptom Rating Scale37 constipation scores.
Random-effects meta-analysis of trials on the association between microbiome modulating intervention and constipation symptoms. IV inverse variance; PD Parkinson’s disease; error bars represent 95% CIs; size of the shaded square indicates study weight; diamond represents pooled standardized mean difference and 95% CI.
Discussion
This study is the first systematic review and meta-analysis to date synthesizing the current evidence from clinical trials that examined the effects of microbiome-modulating interventions on the disease burden of NDDs. Our meta-analysis demonstrated that microbiome-modulating interventions are significantly associated with reduction in motor symptom burden in NDDs, including PD, ALS, and AD. Findings from qualitative synthesis also suggested that microbiome-modulating interventions may reduce inflammation and alleviate GI symptoms, including constipation. Despite the promising effects of microbiome-modulating interventions, the relationships and mechanisms underpinning GM modulation and clinical outcomes remain inconclusive owing to the lack of high-quality clinical trials, the heterogeneity in study design, and the diverse nature of interventions among the included studies.
Microbiome modulation may improve motor symptoms and inflammatory tone
Our meta-analysis revealed that microbiome-modulating interventions can generally lower motor symptom burden in patients with NDDs. In addition, qualitative findings showed that inflammatory tone was generally improved in different NDDs by various microbiome-modulating interventions. NDDs are characterized by chronic inflammation, leaky gut, and decreased production of neuroactive substances, in which the degeneration and loss of neurons lead to long-term motor and nonmotor impairment45,46. The effect on alleviation on symptom burden might be explained by the restoration of GM to reduce inflammation47, re-establish intestinal permeability22,37,48, and enhance neuroactivity through the production of neurotransmitters49.
Xiang et al. performed systematic review and meta-analysis on the use of probiotics in AD and PD and suggested that probiotics improve AD possibly through anti-inflammatory pathways, as demonstrated by a decrease in the GSH level after probiotic supplementation50. In line with our study findings, microbiome modulation, not limited to probiotic supplementation, was found to reduce inflammation and thereby disease burden, which also applies to other NDDs including MS and ALS22,29,30,31,32,33,39.
Restoration of gut dysbiosis can reduce inflammation by multiple pathways, with many of the modulation methods focusing on increasing SCFA-producing bacteria, such as Roseburia spp., Blautia, and Prevotella spp., to increase serum or fecal SCFAs30,31,34,38,42 or on reducing pathogenic bacteria, such as H. pyroli39,40. SCFAs, including butyrate, propionate, and acetate, exert anti-inflammatory effects by inhibiting the activation of nuclear factor-kappa B and the production of proinflammatory cytokines, such as tumor necrosis factor alpha and interleukin-651,52. They can also promote the differentiation of regulatory T cells (Tregs) and suppress that of Th17 cells53. Apart from indirect homeostasis through SCFAs, some bacteria in the microbiome, such as Bacteroides fragilis, can directly induce Treg differentiation to maintain immune intolerance and prevent autoimmunity.
Along with consistent findings of decreased Lactobacillus in MS, Tankou et al. reported an enrichment of SCFA producers, including Akkermansia, Blautia, and Dorea, in MS patients at baseline. After probiotic supplementation, these SCFA producers decreased, but the expression of proinflammatory genes, such as HLA.DPA1 and MS risk allele HLA.DQA1, also decreased30,31. Our qualitative finding also showed that no consistency was established in the changes in SCFA producers or SCFA concentration, but clinical outcomes were improved in general (Table 4). In particular, while some studies suggested that certain species of Blautia and Dorea were associated with decreased levels of inflammatory markers54,55, others indicated that they had proinflammatory effects56,57. The activity of SCFA producers can vary depending on several factors and contribute differently in terms of SCFA production in the gut58,59. Given the complex nature of GM, additional studies are needed to elucidate other factors that influence its interactions with the immune system, such as its abundance, diversity, metabolites, or co-occurrence with other bacteria.
Microbiome modulation may alleviate constipation and GI symptoms
Constipation is common in NDDs and can affect the quality of life of patients. Constipation can be caused by the accumulation of pathological proteins in the GI tract, such as amyloid beta in AD, α-synuclein in PD, or myelin basic protein in MS, which induce dysfunction of the enteric nervous system (ENS) to affect gut motility and barrier59,60. Our study found that, qualitatively, microbiome-modulating interventions may also alleviate constipation. A reduction in constipation might be explained by the enhancement in the integrity and permeability of the intestinal barrier through restoring the microbiome61,62. In addition, SCFAs produced by bacteria can modulate intestinal peristalsis and upregulate the expression of tight junction proteins to strengthen the integrity of the gut barrier63. Secretion of neurotransmitters to stimulate ENS may also play a role in constipation64. However, available evidence remains inadequate, and the results have not reached statistical significance because of the lack of high-quality studies, which should ideally be blinded RCTs with appropriate sample size and statistical power.
Microbiome-modulating interventions and related GM changes
Although all of the included studies reported some degree of changes in GM composition, no consistent changes in GM were found in relation to the overall improvement in clinical outcomes. The inconsistency might be explained by the heterogeneity in interventions and disease nature, while other systematic reviews also observed diverging GM patterns65,66. In terms of studies that involved the use of probiotics, Lactobacillus and Bifidobacterium were commonly used, yet they resulted in different GM changes: one reported increased Lactobacillus and Bifidobacterium30,31, one reported increased B. animalis but decreased Lactobacillus fermentum38, and one reported an increase in F. prausnitzii only42. These observations are in line with other probiotic systematic reviews67. The exact relationship between GM and NDDs remains unknown, and further studies are needed to understand the impact of individual bacteria, the co-occurrence, and the molecular pathway in GM and diseases.
Strengths and limitations
This is the first comprehensive systematic review that examined the effects of a broad spectrum of microbiome-modulating interventions on NDDs, including MS, ALS, PD, and AD. NDDs represent a broad spectrum of disorders, and clinical microbiome trials remain lacking for some diseases, such as the Huntington disease. In addition, most included studies could only be synthesized qualitatively, and heterogeneity regarding the intervention type, outcome measures, and methodological differences was noted. Therefore, we adopted a random-effect model to account for the statistical heterogeneity among studies. Publication bias assessment was not possible given the limited number of available trials for quantitative synthesis, which may also result in minimal but statistically significant overestimation of effects68. Most of the included clinical trials had a small sample size and were of moderate risk of bias mainly subject to the selection of reported results. We also included nonrandomized and single-arm clinical trials, which might have a high risk of bias owing to the lack of comparison group. Studies should include a control group when possible and report the complete effect estimate on the basis of the P value, magnitude, or direction of results69, such as fold change in microbiome changes. When evaluating microbiome diversity, using multiple indices can provide a comprehensive and nuanced understanding of the microbiota diversity and composition70, yet all results of the chosen indices should be listed and interpreted to prevent reporting bias. The findings indicate that the relationship between microbiome-modulating interventions, GM composition, and clinical outcomes of NDDs has been poorly studied and skewed to certain NDDs, namely, PD.
A spectrum of microbiome-modulating components was identified, ranging from probiotic supplement to multidimensional lifestyle interventions consisting of diet modification, mindfulness, and physical activities. Owing to the large variation in methodology across the included studies, definitive conclusions on how microbiome-modulating interventions modulate the GM composition and clinical outcomes and affect the progression of NDDs were impossible to draw.
Most of the studies did not report on significant confounders, such as comorbidities, medication use, and lifestyle, which could affect microbial and clinical outcomes and thus might limit the transferability of our findings. Control conditions also differed between the studies, given that some control interventions comprised AHAD41, a placebo group that received conventional treatments32,38, or a group that received placebo for the first 3 months and probiotics for the next 3 months33, restricting the generalizability of our study findings.
Conclusions and implications
Microbiome-modulating interventions are likely to improve symptom burden, possibly through reducing inflammatory tone in NDD patients via increasing SCFA producers and reducing proinflammatory bacteria. However, the exact relationship remains unknown because no consistent changes in GM composition were identified. High-quality evidence of microbiome-modulating interventions for NDDs is still missing. This review underscores the need for rigorous large-scale studies to examine the effects of microbiome-modulating methods on NDDs.
Future clinical trials of microbiome-modulating methods on NDDs should (1) evaluate the changes in GM through microbiome modulation in terms of alpha and beta diversities and specific phylum, family, and species; (2) assess motor and nonmotor clinical outcomes and incorporate objective data in addition to self-reporting questionnaire; (3) account for confounding factors, including diet, age, medication record, lifestyle, and disease progression. Regarding the diverse methodology of existing GM modulation research, a standardized approach to GM evaluation, such as the STORMS checklist71, is necessary to understand the complex mechanisms and relationships between GM-modulating interventions, GM composition, and NDDs further.
Data availability
The dataset analyzed in this study is available from the corresponding author upon reasonable request.
References
Brettschneider, J. et al. Spreading of pathology in neurodegenerative diseases: A focus on human studies. Nat. Rev. Neurosci. 16(2), 109–120 (2015).
Ou, Z. et al. Global trends in the incidence, prevalence, and years lived with disability of Parkinson’s disease in 204 countries/territories from 1990 to 2019. Front. Public Health 9, 776847 (2021).
Li, X. et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2019. Front. Aging Neurosci. 14, 937486 (2022).
Young, A. L. et al. Uncovering the heterogeneity and temporal complexity of neurodegenerative diseases with Subtype and Stage Inference. Nat. Commun. 9(1), 4273 (2018).
Twohig, D. & Nielsen, H. M. alpha-synuclein in the pathophysiology of Alzheimer’s disease. Mol. Neurodegener. 14(1), 23 (2019).
Behl, T. et al. Multifaceted role of matrix metalloproteinases in neurodegenerative diseases: Pathophysiological and therapeutic perspectives. Int. J. Mol. Sci. 22(3), 1413 (2021).
Backhed, F. et al. Host-bacterial mutualism in the human intestine. Science 307(5717), 1915–1920 (2005).
Fan, Y. & Pedersen, O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 19(1), 55–71 (2021).
Liu, B. N. et al. Gut microbiota in obesity. World J. Gastroenterol. 27(25), 3837–3850 (2021).
Wells, P. M. et al. Associations between gut microbiota and genetic risk for rheumatoid arthritis in the absence of disease: A cross-sectional study. Lancet Rheumatol. 2(7), e418–e427 (2020).
Carabotti, M. S. A., Maselli, M. A. & Severi, C. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 28(2), 203 (2015).
Fulling, C., Dinan, T. G. & Cryan, J. F. Gut microbe to brain signaling: What happens in Vagus. Neuron 101(6), 998–1002 (2019).
Peterson, C. T. Dysfunction of the microbiota-gut-brain axis in neurodegenerative disease: The promise of therapeutic modulation with prebiotics, medicinal herbs, probiotics, and synbiotics. J. Evid. Based Integr. Med. 25, 251569020X957225 (2020).
Wu, S. et al. Roles and mechanisms of gut microbiota in patients with Alzheimer’s disease. Front. Aging Neurosci. 13, 650047 (2021).
Chen, Y., Xu, J. & Chen, Y. Regulation of neurotransmitters by the gut microbiota and effects on cognition in neurological disorders. Nutrients 13(6), 2099 (2021).
Romano, S. et al. Meta-analysis of the Parkinson’s disease gut microbiome suggests alterations linked to intestinal inflammation. NPJ Parkinsons Dis. 7(1), 27 (2021).
Paley, E. L. Discovery of gut bacteria specific to Alzheimer’s associated diseases is a clue to understanding disease Etiology: Meta-analysis of population-based data on human gut metagenomics and metabolomics. J. Alzheimers Dis. 72(1), 319–355 (2019).
Sun, J. et al. Gut microbiome and amyotrophic lateral sclerosis: A systematic review of current evidence. J. Intern. Med. 290(4), 758–788 (2021).
Mirza, A. et al. The multiple sclerosis gut microbiota: A systematic review. Mult .Scler Relat. Disord. 37, 101427 (2020).
Sampson, T. R. et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease. Cell 167(6), 1469–1480 (2016).
Warner, B. B. The contribution of the gut microbiome to neurodevelopment and neuropsychiatric disorders. Pediatr. Res. 85(2), 216–224 (2019).
Al, K. F. et al. Fecal microbiota transplantation is safe and tolerable in patients with multiple sclerosis: A pilot randomized controlled trial. Mult. Scler. J. Exp. Transl. Clin. 8(2), 20552173221086664 (2022).
JPT, H., et al., Cochrane Handbook for Systematic Reviews of Interventions version 6.3 Cochrane, 2022.
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Sterne, J. A. C. et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366, 14898 (2019).
Sterne, J. A. et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355, i4919 (2016).
Hackenberger, B. K. Bayesian meta-analysis now - let’s do it. Croat Med. J. 61(6), 564–568 (2020).
Team, J., JASP (Version 0.17.1)[Computer Software]. 2023.
Barone, M. et al. Influence of a high-impact multidimensional rehabilitation program on the gut microbiota of patients with multiple sclerosis. Int. J. Mol. Sci. 22(13), 7173 (2021).
Tankou, S. K. et al. Investigation of probiotics in multiple sclerosis. Mult. Scler. 24(1), 58–63 (2018).
Tankou, S. K. et al. A probiotic modulates the microbiome and immunity in multiple sclerosis. Ann. Neurol. 83(6), 1147–1161 (2018).
Cignarella, F. et al. Intermittent fasting confers protection in CNS autoimmunity by altering the gut microbiota. Cell Metab. 27(6), 1222–1235 (2018).
Di Gioia, D. et al. A prospective longitudinal study on the microbiota composition in amyotrophic lateral sclerosis. BMC Med. 18(1), 153 (2020).
Becker, A. et al. Effects of resistant starch on symptoms, fecal markers, and gut microbiota in Parkinson’s disease: The RESISTA-PD Trial. Genomics Proteomics Bioinform. 20(2), 274–287 (2022).
Kuai, X. Y. et al. Evaluation of fecal microbiota transplantation in Parkinson’s disease patients with constipation. Microb. Cell Fact. 20(1), 98 (2021).
Hegelmaier, T. et al. Interventional influence of the intestinal microbiome through dietary intervention and bowel cleansing might improve motor symptoms in Parkinson’s disease. Cells 9(2), 376 (2020).
Rusch, C. et al. Mediterranean diet adherence in people with Parkinson’s disease reduces constipation symptoms and changes fecal microbiota after a 5-week single-arm pilot study. Front. Neurol. 12, 794640 (2021).
Sun, H. et al. Probiotics synergized with conventional regimen in managing Parkinson’s disease. NPJ Parkinsons Dis. 8(1), 62 (2022).
Hong, C. T. et al. Rifaximin modifies gut microbiota and attenuates inflammation in Parkinson’s disease: Preclinical and clinical studies. Cells 11(21), 3468 (2022).
Kountouras, J. et al. Eradication of Helicobacter pylori may be beneficial in the management of Alzheimer’s disease. J. Neurol. 256(5), 758–767 (2009).
Nagpal, R. et al. Modified Mediterranean-ketogenic diet modulates gut microbiome and short-chain fatty acids in association with Alzheimer’s disease markers in subjects with mild cognitive impairment. EBioMedicine 47, 529–542 (2019).
Leblhuber, F. et al. Probiotic supplementation in patients with Alzheimer’s dementia: An explorative intervention study. Curr. Alzheimer Res. 15(12), 1106–1113 (2018).
Bai, Z. et al. Cerebrospinal fluid and blood cytokines as biomarkers for multiple sclerosis: A systematic review and meta-analysis of 226 studies with 13,526 multiple sclerosis patients. Front Neurosci. 13, 1026 (2019).
Lassmann, H. Multiple sclerosis pathology. Cold Spring Harb. Perspect. Med. 8(3), e028936 (2018).
Gwak, M. G. & Chang, S. Y. Gut-brain connection: Microbiome, gut barrier, and environmental sensors. Immune Netw. 21(3), e20 (2021).
Bhatt, A. P. et al. Nonsteroidal anti-inflammatory drug-induced leaky gut modeled using polarized monolayers of primary human intestinal epithelial cells. ACS Infect. Dis. 4(1), 46–52 (2018).
Dixit, K. et al. Restoration of dysbiotic human gut microbiome for homeostasis. Life Sci. 278, 119622 (2021).
Kowalski, K. & Mulak, A. Brain-gut-microbiota axis in Alzheimer’s disease. J. Neurogastroenterol. Motil. 25(1), 48–60 (2019).
Zhang, H. et al. Implications of gut microbiota in neurodegenerative diseases. Front Immunol. 13, 785644 (2022).
Xiang, S. et al. Efficacy and safety of probiotics for the treatment of Alzheimer’s disease, mild cognitive impairment, and parkinson’s disease: A systematic review and meta-analysis. Front. Aging Neurosci. 14, 730036 (2022).
Omenetti, S. & Pizarro, T. T. The Treg/Th17 axis: A dynamic balance regulated by the gut microbiome. Front. Immunol. 6, 639 (2015).
Cheng, H. et al. The Th17/Treg cell balance: A gut microbiota-modulated story. Microorganisms 7(12), 583 (2019).
Zhou, W. et al. The gut microbe Bacteroides fragilis ameliorates renal fibrosis in mice. Nat. Commun. 13(1), 6081 (2022).
Tillett, B. J. & Hamilton-Williams, E. E. Microbiota derived factors as drivers of type 1 diabetes. Prog. Mol. Biol. Transl. Sci. 171, 215–235 (2020).
Liu, X. et al. Blautia-a new functional genus with potential probiotic properties?. Gut Microbes 13(1), 1–21 (2021).
Bolte, L. A. et al. Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut 70(7), 1287–1298 (2021).
Vacca, M. et al. The controversial role of human gut lachnospiraceae. Microorganisms 8(4), 573 (2020).
Morrison, D. J. & Preston, T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes 7(3), 189–200 (2016).
Warnecke, T. et al. Gastrointestinal involvement in Parkinson’s disease: Pathophysiology, diagnosis, and management. NPJ Parkinsons Dis. 8(1), 31 (2022).
Brudek, T. Inflammatory bowel diseases and Parkinson’s disease. J. Parkinsons Dis. 9(s2), S331–S344 (2019).
Ohkusa, T. et al. Gut microbiota and chronic constipation: A review and update. Front Med. (Lausanne) 6, 19 (2019).
Takiishi, T., Fenero, C. I. M. & Camara, N. O. S. Intestinal barrier and gut microbiota: Shaping our immune responses throughout life. Tissue Barriers 5(4), e1373208 (2017).
Saleri, R. et al. Effects of different short-chain fatty acids (SCFA) on gene expression of proteins involved in barrier function in IPEC-J2. Porcine Health Manag. 8(1), 21 (2022).
Nezami, B. G. & Srinivasan, S. Enteric nervous system in the small intestine: Pathophysiology and clinical implications. Curr. Gastroenterol. Rep. 12(5), 358–365 (2010).
Attaye, I. et al. A systematic review and meta-analysis of dietary interventions modulating gut microbiota and cardiometabolic diseases-striving for new standards in microbiome studies. Gastroenterology 162(7), 1911–1932 (2022).
Zhao, X. et al. Therapeutic and improving function of lactobacilli in the prevention and treatment of cardiovascular-related diseases: A novel perspective from gut microbiota. Front Nutr. 8, 693412 (2021).
Alexander, G. E. Biology of Parkinson’s disease: Pathogenesis and pathophysiology of a multisystem neurodegenerative disorder. Dialogues Clin. Neurosci. 6(3), 259–280 (2004).
van Aert, R. C. M., Wicherts, J. M. & van Assen, M. Publication bias examined in meta-analyses from psychology and medicine: A meta-meta-analysis. PLoS One 14(4), e0215052 (2019).
Page, M. J. & Higgins, J. P. Rethinking the assessment of risk of bias due to selective reporting: A cross-sectional study. Syst. Rev. 5(1), 108 (2016).
Risely, A. et al. Phylogeny- and abundance-based metrics allow for the consistent comparison of core gut microbiome diversity indices across host species. Front Microbiol. 12, 659918 (2021).
Mirzayi, C. et al. Reporting guidelines for human microbiome research: The STORMS checklist. Nat. Med. 27(11), 1885–1892 (2021).
Acknowledgements
We would like to acknowledge the matching and support received from the Research Platform Hong Kong Student Association of Neuroscience (HKSAN) programme. Dr Jojo Kwok served as the mentor for the programme, while Ms. Zara Chui and Ms. Esther Zhang were the elite students matched from the programme.
Author information
Authors and Affiliations
Contributions
Z.C.: Conceptualization (equal); data curation (lead); methodology (equal); writing—original draft preparation (lead); writing—review & editing (equal). L.C.: Conceptualization (equal); methodology (equal); writing— review & editing (equal). E.Z.: methodology (equal); data curation (equal). Suisha Liang: writing—review & editing (equal). E.C.: writing—review & editing (equal). K.L.: writing—review & editing (equal). J.K.: Writing—conceptualization (lead); methodology (equal); writing—review & editing (equal); supervision (lead). H.T.: Writing—review & editing (equal); supervision (equal).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chui, Z.S.W., Chan, L.M.L., Zhang, E.W.H. et al. Effects of microbiome-based interventions on neurodegenerative diseases: a systematic review and meta-analysis. Sci Rep 14, 9558 (2024). https://doi.org/10.1038/s41598-024-59250-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59250-w
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.