Abstract
Housing tenure is an important aspect to determine health. However, even though renters tend to have more socioeconomic disadvantages than homeowners, mortality risk between private and public renters compared with homeowners remains unclear. Japanese public rented housing, such as the Urban Renaissance Agency, has been developed for supplying an adequate living environment since 1950s. This study aimed to examine the mortality risk among older Japanese residents living in private and public rented houses compared with those living in owner-occupied houses using 9-year follow-up data. This study drew upon a 9-year follow-up of participants in the Japan Gerontological Evaluation Study, a population-based cohort study of Japanese independent adults aged ≥ 65 years. Mortality from 2010 to 2019 was analyzed for 44,007 respondents. Housing tenure was defined by a questionnaire. Cox regression models were used for calculating the hazard ratio for mortality. Bonferroni correction was used to account for multiple testing between rental houses. Overall, 10,638 deaths occurred during the follow-up period. Compared with housing owners, all rental housing groups had a significantly higher risk of mortality. Among renters, participants who lived in public rental housing had the lowest risk of mortality even after adjusting for sociodemographic characteristics, health status, social status, and environmental status. Multiple testing among renters with Bonferroni correction showed that public renters had 0.80 times (95% CI 0.72–0.89) lower mortality risk than private renters. Although Japanese older adults living in public rental housing had a higher mortality risk than homeowners, this risk was lower than that among private renters. A positive neighborhood environment based on well-planned urban development may have contributed to this result. The results suggest that planned urban development lowers the risk of mortality in older renters in Japan.
Similar content being viewed by others
Introduction
Population aging has been considered a challenging issue worldwide. Approximately 30% of Japan’s population are aged ≥ 60 years, which is the highest number globally1. Additionally, older adults in Japan are known for their long lifespans2. One of the eight age-friendly city topics is housing, which is essential for safety and well-being3. A previous study reported that preschool children and retired people spend around 90% of their time at home4. Several studies have focused on housing tenure and health from different aspects. For instance, the census longitudinal study conducted by Filakti and Fox5 noted that housing tenure is associated with morbidity and mortality. Furthermore, Ellaway and Macintyre6 revealed that housing stressors were associated with anxiety and depression. In a study by Macintyre et al.7 on 2867 adults in the UK, it was found that the characteristics of the dwelling and its surroundings may help explain the association between housing tenure and health. Another study by Park et al.8 using country-level panel data showed that housing cost burden can be associated with population health. Moreover, Park et al.9 also investigated 881,220 older adults using population-based linked dataset and revealed that housing assets and income were associated with mortality. Furthermore, Laaksonen et al.10 found that subsidized renters had a higher risk of mortality than private renters and owner-occupiers. A recent study from Graetz et al.11 using longitudinal data represented that high costs of rent and evictions were associated with mortality. Therefore, a familiar environment, such as housing, can be considered an important health factor in older adults. However, some of those studies did not include factors that contribute to health, such as educational history, work status, and social activities, in their analysis, which may require further analysis. Further research is needed to determine the definition of the housing indicator and the mechanism for preventing adverse health effects.
Although housing is often described as a proxy measure of socioeconomic status (SES), it may also affect health independent of SES. For example, in a study by Macintyre et al.12 on 6500 adults in the UK, it was observed that four material asset indicators, i.e., tenure car access, social class, and income, may affect an individual’s health. A study by Do and Kim13 on 17,214 older adults in Korea using 2-year follow-up data revealed that individuals in short-term rental houses showed a higher risk of falls and activity limitation due to fear of falling than homeowners did. Furthermore, Pledger et al.14 studied 15,626 older adults in New Zealand using pooled data from 2013 to 2016 and revealed that individuals who were in rental tenure were associated with poor health. A study by Morales and Robert15 on 1064 older adults in the United States using longitudinal data from 2015 to 2017 revealed that housing cost burden was associated with activity of daily living (ADL)/instrumental ADL limitation over time. A longitudinal study has also investigated the association between housing cost burden and poor psychological well-being16. Dalstra et al.17, using the national health survey from 10 European countries, demonstrated that even after adjusting for education and income, health differences according to housing tenure were observed and that the difference varies between countries. However, the factors that cause these differences were not determined. Pledger et al. reported that differences in the housing market and public policy may also have an influence14. Additionally, urban planning, such as the environment around houses, could also be an important factor.
Rental housing, such as private and public rental housing, can also have an influence on health, and has a different effect depending on the type of rental housing. For example, a study by Digenis-Bury et al.18 on 2919 participants showed that public housing residents are more likely diagnosed with several medical conditions, including hypertension, obesity, current asthma, disability, loss of six or more teeth, and feelings of depression, and have poorer health status than other city residents. Furthermore, Windle et al.19 interviewed 423 older individuals and revealed that individuals who lived in public rented properties experienced more health problems than those living in owner-occupied and private rented properties. A report showed that private rental houses have poorer quality than public housing and owner-occupied homes in New Zealand, thus having the possibility of different effects on health and well-being20,21. A cross-sectional study by Tomioka et al.22 on Japanese adults revealed that private renters had poorer self-rated health than other tenure. According to a Japanese White Paper in 2021 of households headed by a married couple with a person aged ≥ 65 years, 87.4% of Japanese older adults were homeowners, 5.5% lived in public rented houses, and 6.9% lived in private rented houses23. Another Japanese study showed that older adults living in rental houses are more socially isolated, specifically among private renters but not public renters24. Although renters tend to have more socioeconomic disadvantages than homeowners, mortality risk between public and private renters compared with that among homeowners has not been investigated, and only a few studies have compared the mortality between public and private renters5,8,9,10. Thus, considering that most studies have not clearly distinguished the effects between public and private rental housing, further research is needed.
In Japan, two agencies supply public housing, and differences exist in the backgrounds behind their establishment. One is the local government (municipality or prefecture level). The main purpose of publicly owned housing operated at the municipal or prefectural level is to provide rental housing to low-income individuals who are struggling to find adequate housing. Another is an independent administrative agency, called the Urban Renaissance Agency (UR), which supplies public housing called Koudan housing (housing complexes) mainly in urban or suburban areas. The Japan Housing Corporation (JHC), UR’s predecessor organization, was founded in 1955. During the 1950s, 1960s, and 1970s, the JHC built many Koudan housing in suburban areas to offset the increasing housing demand during the post-World War II economic boom and later baby boom. The UR is a semi-private, independent administrative agency responsible for housing in Japan other than public housing. As the agency responsible for housing in Japan, it provides housing at market prices, but without the fees (key money or renewal fees) and guarantor requirements common in private rentals in Japan. Public housing developed by the UR refers to the implementation of Perry’s Neighborhood Unit Theory, which involves the deliberate placement of open spaces, commercial facilities, public facilities, and internal streets25 (Fig. 1). According to the Ministry of Land, Infrastructure, Transport and Tourism’s 2022 housing economic data, the total number of housing in Japan was 53,616,300, of which 1,922,300 were public rental housing and 747,200 were UR apartments. Furthermore, another report from the Ministry of Land Infrastructure Transport and Tourism showed the distribution of rental housing managed by the UR throughout Japan. According to the report, as of 2012, of all apartment complexes (1732 apartment complexes) managed by the UR, the total for Tokyo, Kanagawa, Chiba, Saitama, and Ibaraki was 911 (52.6%). Furthermore, 124 (7.2%) complexes were located in the Aichi Prefecture; 422 (24.4%) in Osaka, Hyogo, Kyoto, and Nara; 162 (9.4%) in Fukuoka; and 113 (6.5%) in others26,27. These data also showed that public housing operated by the UR was concentrated in urban or suburban areas. The average size of UR houses is 46.6–51.9 m228. Moreover, as of March 31, 2015, the company announced that it had built 2029 apartment complexes with 883,038 apartments29. Based on this data, it has been estimated that each apartment complex has approximately 435 apartments. Several application requirements for UR apartments have been established, such as income requirements and visa (for foreign residents)30. The income criterion dictates that the applicant must have an income of four times the rent, thus indicating that not necessarily only low-income families reside in the area30.
Example of a large public housing complex (including the participants of this analysis): Naruko Housing Complex in Midori Ward, Nagoya City, Aichi Prefecture. The area within the dashed lines is the Naruko Housing Complex. The complex was completed in 1964, with many residential buildings being five-story tall. The main street, which curves to match the terrain, serves as the axis for the area, with a primary school, park, shops, banks, post office, and other facilities located in the center of the complex. The complex also features abundant open spaces with lush greenery between the residential buildings, reflecting the influence of the theory of “the neighboring unit.” During its development, 2196 apartments were built and the planned population was approximately 8000 individuals. Aerial photographs were provided by the Geospatial Information Authority of Japan in 2007.
Public rental housing, such as the UR in Japan, is often larger than private rental housing and is built under planned urban development. If differences in health effects are found between the two, this could clarify some conditions for age-friendly housing. A previous study also revealed that the definition of housing tenure may differ by contextual features, such as historical period, society or region, and culture7. Thus, further studies on this topic with different populations and locations are needed. Therefore, this study aimed to examine the risk of mortality among older Japanese residents living in private and public rental houses compared with those living in owner-occupied houses using large-scale 9-year follow-up data. We hypothesized that those who lived in owned houses had the lowest risk of mortality and those who lived in public rental houses had a lower risk of mortality than those who lived in private rental houses. By examining the association between housing tenure and mortality among Japanese older adults, this study can be expected to contribute to creating pieces of evidence for urban planning for healthy older adults.
Methods
Study design and participants
The Japan Gerontological Evaluation Study (JAGES) collected baseline data using a mail survey in August 2010 among independent older adults who are ineligible for benefits from the long-term care insurance system in Japan from 11 municipalities31. The baseline survey was conducted from August 2010 to December 2011. Self-administered questionnaires were distributed by mail to individuals aged ≥ 65 years who were physically and cognitively independent. The survey was conducted using random sampling in large municipalities and was administered to all eligible residents in small municipalities. Hence, the study participants were independent and relatively healthy older adults. In total, 46,144 have been linked to a long-term care insurance database. These analyses were performed using data from 44,007 participants. We excluded those with missing data, including home address (n = 80), and those whose ADL was not independent or missing (n = 2057). The flow chart of study participants is represented in Fig. 2.
Mortality outcome
The vital status during the follow-up period from 2010 to 2019 (mean: 3087 days; range: 8–3775 days) was determined by linking data of the self-administered questionnaire to mortality records in the long-term care insurance database. In total, 10,638 deaths occurred in the analytical sample (cumulative mortality = 10,638/44,007; 24.2%). This study examined all-cause mortality instead of cause-specific mortality because death certificate data were unavailable.
Housing tenure
Housing tenure was defined using a questionnaire. The participants were asked “What type of residence do you live in?” and answers were (1) Owned house; (2) Private rental house; (3) Public rental house; (4) Company housing or dormitories, and (5) Others. Because the participants who answered “living in company housing or dormitories” were few (n = 87), we combined answers (4) and (5) to form the “Others” group. Then, we used these four categories in the analysis.
Covariates
Based on previous studies on housing status or mortality, we selected demographic factors, health status, social activities, and environmental factors as covariates. For the demographic factors, sex (men or women), age (65–69, 70–74, 75–79, 80–84, or ≥ 85 years), marital status (married, widowed, divorced, unmarried, or others), educational attainment (≤ 9 or ≥ 10 years), equivalent income (low, ≤ ¥1,999,999; middle, ¥2,000,000–3,999,999; or high, ≥ ¥4,000,000), living status (living alone, with family members, or other facilities), longest job held (professional/technical, administrative, clerical, sales/service, skilled/labor, agriculture/forestry/fishery, others, and no occupation), and employment status (worker, retired, or never worked) were selected6,9,32. The equivalent income was calculated by dividing the total household income by the square root of the number of household members33. Cut-off of the category was followed by a previous report of JAGES34,35. For health status, Geriatric Depression Scale (GDS) score, hypertension (yes or no), stroke (yes or no), diabetes mellitus (yes or no), hearing disorder (yes or no), heart disease (yes or no), respiratory disease (yes or no), cancer (yes or no), and body mass index (BMI) were selected32,36,37. For social activities, the participation for sports or hobby groups (none of them, one of them, or both of them) and tertile of the total score of social support from family or friends (low, 0–4; middle, 5–7; or high, 8–24) were selected38. For social support, four dimensions were used to scale as follows: (1) receiving emotional support, (2) providing emotional support, (3) receiving instrumental support, and (4) giving instrumental support39. For the environmental factors, population density as tertile (low, 430–3791 individuals per km2; middle, 3818–6549 individuals per km2; or high, 6550–27,781 individuals per km2) and duration of residence (< 5, 10–19, 20–29, 30–39, 40–49, and > 50 years) were selected40.
Statistical analysis
Descriptive analysis was performed to summarize the characteristics of the participants. Furthermore, owing to the lack of some variables in this analysis, multiple imputations were performed. Twenty multiple imputed datasets, including all measurement variables, were created using the multivariate normal imputation method under a “missing at random” assumption, after which the estimated parameters were combined using Rubin’s combination methods. Cox proportional-hazards model was performed to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for mortality. We have set three models after the crude. In Model 1, sociodemographic factors (sex, age, marital status, educational attainment, equivalent income, living status, longest job held, and employment status) were added. In Model 2, health status (GDS score, hypertension, stroke, diabetes mellitus, hearing disorder, and BMI) was added. In Model 3, social status (social participation in sports and hobby groups, and social support) was added. In Model 4, environment status (population density and duration of residence) was added. Bonferroni correction was used to account for post hoc multiple testing other than owned house, which is private rental house versus public rental house, private rental house versus others, and public rental house versus others. All statistical analyses were performed using Stata 16/IC (StataCorp, College Station, TX, USA).
Ethics approval
This study was reviewed and approved by the Ethics Committee of Chiba University (3442) and the Research Ethics Committee involving Human Participants of Nihon Fukushi University (10-05). The study was conducted according to the principles of the Declaration of Helsinki and its later amendments. The JAGES participants were informed that participation in the study was voluntary, and the completion and return of the questionnaire by mail constituted consent to participate in the study. All participants provided written informed consent when they returned a questionnaire.
Results
Table 1 shows the characteristics of the 44,007 respondents. Of all participants, 37,761 were living in owned houses, 2280 were living in private rental houses, 2490 were living in public rental houses, and 569 were others. Furthermore, the number of participants whose income was low was similar in public rental housing (56.3%) and private rental housing (61.5%), whereas they were higher than participants living in owned houses (38.6%). Moreover, the percentage of participants living alone was also similar in public rental housing (32.1%) and private rental housing (28.6%).
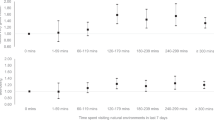
Table 2 presents the HRs with 95% CIs for the association between housing tenure and the risk of mortality. After adjusting for potential confounders in Model 4, participants who lived in private rental houses had 1.45 times (95% CI 1.34–158) higher, those who lived in public rental houses had 1.17 times (95% CI 1.07–1.27) higher, and those who lived in others had 1.21 times (95% CI 1.05–1.40) higher risk of mortality than those who lived in owned houses. The results of post hoc multiple testing among non-home owners indicated a significant difference between private and public renters. Public renters have 0.80 times (95% CI 0.72–0.89) lower risk of mortality than private renters (p = 0.0001). The results from other post hoc multiple testing did not indicate significant differences.
Discussion
To the best of our knowledge, this was the first study to investigate the association between housing tenure particularly between residents living in private and public rental housing and mortality risk with four different models. We found that the risk of mortality was the lowest among older adults living in owned houses. Furthermore, the mortality risk was lower in those living in public rental houses than in those living in other types of rental houses.
In this study, even after adjusting for SES, older adults living in owned houses had the lowest risk of mortality. One of the reasons could be that SES is not fully adjusted. Educational attainment, income, and employment status were added as SES in this analysis; however, we did not add other attributes that older individuals may have, such as wealth. Another example of a possible effect from not fully adjusted SES could be the ability to maintain the quality of house. For instance, individuals with higher SES can easily maintain room temperature. In their housing and health guidelines, the World Health Organization strongly recommends controlling indoor cold and heat41. Room temperature should be well-balanced indoor temperature to protect health during cold seasons in countries with cold seasons, such as Japan. Older adults with high SES possibly have more capacity to maintain room temperature through, for instance, renovations to maintain room temperature, purchasing a heater or air conditioner, and constantly paying utility bills.
Possibility of a lower risk of mortality among participants living in public rental housing compared with private rental housing is a richer neighborhood environment around public housing that can enhance physical activities and social participation42. In Japan, a quantitative supply of houses after World War II28 enabled a planned design of the surrounding environment around public rental housing, such as parks, sidewalks, and greenery. Having places suitable for exercise in the community has been associated with a lower risk of heart disease in older men43. One of the previous studies revealed that people who are living in a social rented dwelling setup were more likely to be exposed to environmental factors that negatively affect their health, such as noise, crime, and vandalism7. The study discusses the issue of low availability of health-promoting environments, such as gardens and community amenities. Another study revealed that lower frailty of older adults was also associated with the accessibility of parks and sidewalks44. Lack of grocery stores in the neighborhood increases the risk of death, dementia, and need for long-term care and reduces fresh food intake32,35,45,46. Moreover, living in a neighborhood with a higher rate of sidewalk installation was associated with a low risk of dementia in urban areas47. Another study revealed that living in a higher subjective neighborhood walkability is associated with lower knee and lower back pain48. Hence, living in a positive neighborhood environment, which promotes healthy behaviors, may be associated with a lower risk of mortality.
Another possible mechanism is the positive effect from well-planned environments, such as greenspaces. As previously mentioned, Japanese public houses are well-developed such that all necessities, including green areas, are distributed around the residence28. A cross-sectional study by Nishigaki et al. on 126,878 older adults in Japan revealed that living in greener neighborhoods was shown to be associated with lower risk of depression in urban areas. This could be due to the fact that green spaces in an artificial environment may enhance their impression according to the Attention Restoration Theory49. Furthermore, the effect of greenness supports reducing the heat island phenomenon, mitigating noise, or improving the air quality50. The health benefits of green spaces are also summarized in the meta-analysis51.
Moreover, the social dimension may also be a key factor, such as social cohesion. In this study, we added social status (i.e., social participation and support) in Model 3, and the HR decreased by 0.02 after adjusting for social status. A study showed that owning a home is seen as having achieved the “American Dream” and may contribute to maintaining a high subjective sense of well-being52. Living in a Koudan house represented the “Japanese dream” during the rapid economic growth period (during the 1950s and 1970s) in Japan28. Because some individuals continue to live in public houses since their working age, they may have stronger social cohesion or networks than those living in other housing tenures. In some studies, it has been reported that social cohesion increases subjective well-being and reduces the risks of all-cause and cause-specific mortality53,54. Moreover, Nishina and Oh55 studied 897 older adults in Japan using cross-sectional data and showed that older adults who live in public housing have more social life variety than those living in owned houses. While private rental houses in this study may contain various characteristics, such as building age (new to old) and accessibility to necessities for life (located convenient area to inconvenient area), Japanese public rental houses may have homogeneous characteristics, such as location or access to necessities. Hence, stronger social cohesion may be a reason for our results.
Key strengths of this study were its novelty that the association between housing tenure and the risk of mortality was investigated using cohort data and that participants living in private and public rented houses were compared. Several limitations should be mentioned. First, our analysis was limited to all-cause mortality. Future studies should examine cause-specific mortality to investigate the association between housing tenure and mortality in more detail to determine the impact of environment, such as neighborhood walkability and cardiovascular death. Second, we did not account for the quality of houses. The US Department of Housing and Urban Development outlines eight things to maintain a healthy home: Keep it dry, clean, safe, well-ventilated, pest-free, contaminant-free, well-maintained, and thermally controlled56. Japanese old houses tend to be ill thermally controlled, and insulation is inadequate even though it has been stated as a strong recommendation in the housing and health guidelines by the World Health Organization41. Japanese census reveals that 59.5% of houses in Japan were built before 200057. Third, we have not analyzed the mechanism of the association; therefore, this association must be further examined. Future analysis should be conducted using data designed to elucidate these issues. Fourth, we have not included the designs of rental housing. It can be imagined that some buildings are designed to promote social interaction in both private and public rental housing complexes; however, such considerations were not considered in this analysis. Fifth, it was impossible to distinguish whether public housing is operated by the local government or the UR. However, according to our JAGES 2019 survey data that allowed us to distinguish them, 55.3% of residents lived in buildings operated by the UR, 33.2% did not, and 11.5% of the data were missing. Sixth, selection bias may be present for residents who want to live in houses operated by the UR because the UR provided housing, particularly for low- to middle-income individuals. Therefore, it is possible that the residents of public housing targeted in this study are not necessarily only from low-income households. Despite the aforementioned limitations, this study discussed important perspectives regarding the association between housing tenure and the risk of mortality.
Conclusion
In this study, we examined the risk of mortality among older Japanese residents living in private and public rented houses compared with that among those living in owner-occupied houses using 9-year follow-up data. We found that the risk of mortality was lower in those living in public rental houses than in those living in private rented houses and other types of rental houses. As aging leads to frailty, the housing environment may directly affect older individuals. Therefore, rental housing may also be important to consider during planned development, including the neighborhood. Investigating factors related to their living conditions among older populations is important to suggest healthy urban development.
Data availability
Data is made available for academic purposes upon request. People can request from the following web page: https://www.jages.net/contact/.
Abbreviations
- ADL:
-
Activity of daily living
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- GDS:
-
Geriatric Depression Scale
- HR:
-
Hazard ratios
- JAGES:
-
Japan Gerontological Evaluation Study
- JHC:
-
Japan Housing Corporation
- UR:
-
Urban Renaissance
References
World Health Organization. World Report on Ageing and Health (WHO, 2015).
Horie, S. The secret of Japanese longevity. J. Men’s Health 8, S4. https://doi.org/10.1016/S1875-6867(11)60009-2 (2011).
World Health Organization. Global Age-friendly Cities: A Guide. World Health Organization. http://www.who.int/ageing/publications/Global_age_friendly_cities_Guide_English.pdf (2007).
Baker, M., Keall, M., Au, E. L. & Howden-Chapman, P. Home is where the heart is—Most of the time. N. Z. Med. J. 120, 1–5 (2007).
Filakti, H. & Fox, J. Differences in mortality by housing tenure and by car access from the OPCS Longitudinal Study. Popul. Trends 81, 27–30 (1995).
Ellaway, A. & Macintyre, S. Does housing tenure predict health in the UK because it exposes people to different levels of housing related hazards in the home or its surroundings?. Health Place 4, 141–150 (1998).
Macintyre, S. et al. What features of the home and the area might help to explain observed relationships between housing tenure and health? Evidence from the west of Scotland. Health Place 9, 207–218 (2003).
Park, G. R., Grignon, M., Young, M. & Dunn, J. R. The association between housing cost burden and avoidable mortality in wealthy countries: Cross-national analysis of social and housing policies, 2000–2017. J. Epidemiol. Community Health 77, 65–73 (2022).
Park, G. R., Grignon, M., Young, M. & Dunn, J. R. How do housing asset and income relate to mortality? A population-based cohort study of 881220 older adults in Canada. Soc. Sci. Med. 314, 115429. https://doi.org/10.1016/j.socscimed.2022.115429 (2022).
Laaksonen, M., Tarkiainen, L. & Martikainen, P. Housing wealth and mortality: A register linkage study of the Finnish population. Soc. Sci. Med. 69, 754–760 (2009).
Graetz, N. et al. The impacts of rent burden and eviction on mortality in the United States, 2000–2019. Soc. Sci. Med. 340, 116398. https://doi.org/10.1016/j.socscimed.2023.116398 (2024).
Macintyre, S., Ellaway, A., Der, G., Ford, G. & Hunt, K. Do housing tenure and car access predict health because they are simply markers of income or self esteem? A Scottish study. J. Epidemiol. Community Health 52, 657–664 (1998).
Do, Y. K. & Kim, C. S. Home ownership and fall-related outcomes among older adults in South Korea. Geriatr. Gerontol. Int. 13, 867–873 (2013).
Pledger, M., McDonald, J., Dunn, P., Cumming, J. & Saville-Smith, K. The health of older New Zealanders in relation to housing tenure: Analysis of pooled data from three consecutive, annual New Zealand Health Surveys. Aust. N. Z. J. Public Health 43, 182–189 (2019).
Meghan, J. M. & Robert, S. A. Housing cost burden and health decline among low- and moderate-income older renters. J. Gerontol. Ser. 77, 1–18 (2021).
Szabo, A., Allen, J., Alpass, F. & Stephens, C. Longitudinal trajectories of quality of life and depression by housing tenure status. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 73, e165–e174 (2018).
Dalstra, J. A. A., Kunst, A. E. & Mackenbach, J. P. A comparative appraisal of the relationship of education, income and housing tenure with less than good health among the elderly in Europe. Soc. Sci. Med. 62, 2046–2060 (2006).
Digenis-Bury, E. C., Brooks, D. R., Chen, L., Ostrem, M. & Horsburgh, C. R. Use of a population-based survey to describe the health of Boston public housing residents. Am. J. Public Health 98, 85–91 (2008).
Windle, G. S., Burholt, V. & Edwards, R. T. Housing related difficulties, housing tenure and variations in health status: Evidence from older people in Wales. Health Place 12, 267–278 (2006).
Alan, J., Philippa, H.-C. & Shamubeel, E. A stocktake of New Zealand’s housing. http://www.beehive.govt.nz/sites/default/files/2018-02/AStocktakeOfNewZealand%27sHousing.pdf (2018).
Howden-Chapman, P. & Pierse, N. Commentary on housing, health, and well-being in Aotearoa/New Zealand. Health Educ. Behav. 47, 802–804 (2020).
Tomioka, K., Kurumatani, N. & Saeki, K. Association between housing tenure and self-rated health in Japan: Findings from a nationwide cross-sectional survey. PLoS ONE 14, 1–13 (2019).
Cabinet Office. 令和3年版高齢社会白書 (全体版) (Japanese). https://www8.cao.go.jp/kourei/whitepaper/w-2021/zenbun/03pdf_index.html (2021).
Koike, T. et al. Social isolation of the elderly living in housing complexes from a comparative analysis on residence statuses. Jpn. J. Gerontol. 36, 303–312 (2014).
Perry, C. The Neighborhood Unit (Routledge, 1998).
The Urban Renaissance Agency. Overview of Urban Renaissance Agency’s Role and Initiatives (Japanese) (2013).
Shimizu, S., Kikuchi, Y. & Sakurai, Y. The Study on The Actual State of Public Rental Housing’s Distribution. Mem. Grad. Eng. Univ. Fukui 57 (2009).
Kobayashi, M. The housing market and housing policies in Japan. SSRN Electron. J. (2016).
The Urban Renaissance Agency. 数字で見るUR都市機構の60年 (Japanese). https://www.ur-net.go.jp/aboutus/publication/web-urpress43/special2.html (2023).
The Urban Renaissance Agency. Application Requirements (Japanese), 2–3. https://www.ur-net.go.jp/chintai/rent/requirements/ (2024).
Kondo, K. & Rosenberg, M. National Center for Geriatrics and Gerontology. Advancing universal health coverage through knowledge translation for healthy ageing. World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO., editor. World Health Organization. Licence: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/handle/10665/279010 (2018).
Tani, Y. et al. Neighborhood food environment and mortality among older Japanese adults: Results from the JAGES cohort study. Int. J. Behav. Nutr. Phys. Act. 15, 1–12 (2018).
OECD. Divided We Stand WHY INWQUALITY KEEPS RISING (2011).
Koga, C., Tsuji, T., Hanazato, M., Takasugi, T. & Kondo, K. Types of elder abuse and dementia onset among older adults in Japan: A 6-year longitudinal study from the Japan Gerontological Evaluation Study. Arch. Gerontol. Geriatr. 100, 104656. https://doi.org/10.1016/j.archger.2022.104656 (2022).
Tani, Y., Suzuki, N., Fujiwara, T., Hanazato, M. & Kondo, K. Neighborhood food environment and dementia incidence: The Japan Gerontological Evaluation Study Cohort Survey. Am. J. Prev. Med. 56, 383–392 (2019).
Burke, W. J., Roccaforte, W. H. & Wengel, S. P. The short form of the Geriatric Depression Scale: A comparison with the 30-item form. J. Geriatr. Psychiatry Neurol. 4, 173–178 (1991).
Schreiner, A. S., Hayakawa, H., Morimoto, T. & Kakuma, T. Screening for late life depression: Cut-off scores for the Geriatric Depression Scale and the Cornell Scale for Depression in Dementia among Japanese subjects. Int. J. Geriatr. Psychiatry 18, 498–505 (2003).
Kondo, K. Achievements and challenges of social epidemiology research aiming to reduce health inequality: A revised English version of Japanese in the Journal of the Japan Medical Association 2020;149 (9):1626-30. JMA J. 5, 9–16 (2020).
Tsuboi, H., Hirai, H. & Kondo, K. Giving social support to outside family may be a desirable buffer against depressive symptoms in community-dwelling older adults: Japan gerontological evaluation study. Biopsychosoc. Med. 10, 1–11. https://doi.org/10.1186/s13030-016-0064-6 (2016).
Nishida, M., Hanazato, M., Koga, C. & Kondo, K. Association between proximity of the elementary school and depression in Japanese older adults: A cross-sectional study from the jages 2016 survey. Int. J. Environ. Res. Public Health 18, 1–13 (2021).
World Health Organization. WHO Housing and Health Guidelines. https://www.who.int/publications/i/item/9789241550376 (2018).
Hanibuchi, T., Kawachi, I., Nakaya, T., Hirai, H. & Kondo, K. Neighborhood built environment and physical activity of Japanese older adults: Results from the Aichi Gerontological Evaluation Study (AGES). BMC Public Health 11, 1–12 (2011).
Inoue, Y. et al. Neighborhood characteristics and cardiovascular risk among older people in Japan: Findings from the JAGES project. PLoS ONE 11, 1–16 (2016).
Mori, Y. et al. Built environments and frailty in older adults: A three-year longitudinal JAGES study. Arch. Gerontol. Geriatr. 103, 104773. https://doi.org/10.1016/j.archger.2022.104773 (2022).
Momosaki, R. et al. Association between food store availability and the incidence of functional disability among community-dwelling older adults: Results from the Japanese Gerontological Evaluation Cohort Study. Nutrients 11, 1–10 (2019).
Yamaguchi, M. et al. Community social capital and depressive symptoms among older people in Japan: A multilevel longitudinal study. J. Epidemiol. 29, 363–369 (2019).
Tani, Y., Hanazato, M., Fujiwara, T., Suzuki, N. & Kondo, K. Neighborhood sidewalk environment and incidence of dementia in older Japanese adults. Am. J. Epidemiol. 190, 1270–1280 (2021).
Okabe, D. et al. Neighborhood walkability in relation to knee and low back pain in older people: A multilevel cross-sectional study from the Jages. Int. J. Environ. Res. Public Health 16, 1–13 (2019).
Nishigaki, M., Hanazato, M., Koga, C. & Kondo, K. What types of greenspaces are associated with depression in urban and rural older adults? A multilevel cross-sectional study from JAGES. Int. J. Environ. Res. Public Health 17, 9276 (2020).
Nieuwenhuijsen, M. J., Khreis, H., Triguero-Mas, M., Gascon, M. & Dadvand, P. Fifty shades of green. Epidemiology 28, 63–71 (2017).
Twohig-Bennett, C. & Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 166, 628–637. https://doi.org/10.1016/j.envres.2018.06.030 (2018).
Miranda, P. Y. et al. Reports of self-rated health by citizenship and homeownership, United States 2000–2010. Prev. Med. (Baltim.) 100, 3–9. https://doi.org/10.1016/j.ypmed.2017.03.006 (2017).
Cramm, J. M. & Nieboer, A. P. Social cohesion and belonging predict the well-being of community-dwelling older people. BMC Geriatr. 15, 1–10 (2015).
Inoue, S., Yorifuji, T., Takao, S., Doi, H. & Kawachi, I. Social cohesion and mortality: A survival analysis of older adults in Japan. Am. J. Public Health 103, 60–66 (2013).
Nishina, N. & Oh, S. A study on the characteristics and issues of social relationships of the elderly living in Suburban Public Housing: A comparative study of both public housing and surrounding areas. Jpn. J. Soc. Welf. 54, 42–54 (2013).
U.S. Department of Housing and Urban Development. Health @ Home High-Performance Housing Rehabilitation Guidelines (2021).
Japanese Government Statistics. Housing and Land Survey, 2008 Basic Tabulation on Housing and Households (e-Stat). https://www.e-stat.go.jp/dbview?sid=0003355546.
Acknowledgements
We are extremely grateful to all study participants for the use of their personal data. We express our deepest gratitude to everyone who participated and cooperated in the study.
Funding
This study used data from the JAGES. This study was supported by Grant-in-Aid for Scientific Research (15H01972, 15H04781, 15H05059, 15K03417, 15K03982, 15K16181, 15K17232, 15K18174, 15K19241, 15K21266, 15KT0007, 15KT0097, 16H05556, 16K09122, 16K00913, 16K02025, 16K12964, 16K13443, 16K16295, 16K16595, 16K16633, 16K17256, 16K17281, 16K19247, 16K19267, 16K21461, 16K21465, 16KT0014, 17K04305, 17K04306, 25253052, 25713027, 26285138, 26460828, 26780328, 18H03018, 18H04071, 18H03047, 18H00953, 18H00955, 18KK0057, 19H03901, 19H03915, 19H03860, 19K04785, 19K10641, 19K11657, 19K19818, 19K19455, 19K24060, 19K20909, 20H00557, 20K13721, 21K19635, 21H03153, and 22K04450) from the Japan Society for the Promotion of Science; Health Labor Sciences Research Grants (H26-Choju-Ippan-006, H27-Ninchisyou-Ippan-001 H28Choju-Ippan-002, H28Ninchisyou-Ippan-002, H30-Kenki-Ippan-006,H29-Chikyukibo-Ippan-001, H30-Jyunkankinado-Ippan-004, 19FA1012, 19FA2001, 21FA1012, 22FA2001, 22FA1010), research project on health and welfare promotion for the elderly from the Ministry of Health, Labor and Welfare, Japan; the Research and Development Grants for Longevity Science from Japan Agency for Medical Research and Development (AMED) (JP18dk0110027, JP18ls0110002, JP18le0110009, JP20dk0110034, JP21lk0310073, JP21dk0110037, and JP22lk0310087), the Research Funding for Longevity Sciences from National Center for Geriatrics and Gerontology (24-17, 24-23, 29-42, 30-30, 30-22, 20-19, 21-20); Open Innovation Platform with Enterprises, Research Institute and Academia (OPERA, JPMJOP1831) from the Japan Science and Technology (JST); a grant from the Japan Foundation For Aging And Health (J09KF00804), a grant from Innovative Research Program on Suicide Countermeasures (1-4), a grant from Sasakawa Sports Foundation, a grant from Japan Health Promotion & Fitness Foundation, a grant from Chiba Foundation for Health Promotion & Disease Prevention, the 8020 Research Grant for fiscal 2019 from the 8020 Promotion Foundation (adopted number: 19-2-06), and grants from Meiji Yasuda Life Foundation of Health and Welfare. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the respective funding organizations.
Author information
Authors and Affiliations
Contributions
T.S. and T.O. had basic ideas for this research. N.K., M.S., K.K, and M.H had carefully reviewed manuscript. M.H. created the figure for the article. C.K. analyzised data and wrote the main manusxript text.
Corresponding author
Ethics declarations
Competing interests
One of the co-authors, Masamichi Hanazato, was collaborating with the UR Urban Renaissance Agency for three years starting in 2019 and has received joint research funding. Other authors does not have any conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koga, C., Saito, T., Hanazato, M. et al. Living in public rental housing is healthier than private rental housing a 9-year cohort study from Japan Gerontological Evaluation Study. Sci Rep 14, 7547 (2024). https://doi.org/10.1038/s41598-024-58244-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58244-y
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.