Abstract
Cognitive dysfunction, especially memory impairment, is a typical clinical feature of long-term symptoms caused by repetitive mild traumatic brain injury (rmTBI). The current study aims to investigate the relationship between regional brain atrophy and cognitive impairments in retired athletes with a long history of rmTBI. Overall, 27 retired athletes with a history of rmTBI (18 boxers, 3 kickboxers, 2 wrestlers, and 4 others; rmTBI group) and 23 age/sex-matched healthy participants (control group) were enrolled. MPRAGE on 3 T MRI was acquired and segmented. The TBV and TBV–adjusted regional brain volumes were compared between groups, and the relationship between the neuropsychological test scores and the regional brain volumes were evaluated. Total brain volume (TBV) and regional brain volumes of the mammillary bodies (MBs), hippocampi, amygdalae, thalami, caudate nuclei, and corpus callosum (CC) were estimated using the SPM12 and ITK–SNAP tools. In the rmTBI group, the regional brain volume/TBV ratio (rmTBI vs. control group, Mann–Whitney U test, p < 0.05) underwent partial correlation analysis, adjusting for age and sex, to assess its connection with neuropsychological test results. Compared with the control group, the rmTBI group showed significantly lower the MBs volume/TBV ratio (0.13 ± 0.05 vs. 0.19 ± 0.03 × 10−3, p < 0.001). The MBs volume/TBV ratio correlated with visual memory, as assessed, respectively, by the Rey–Osterrieth Complex Figure test delayed recall (ρ = 0.62, p < 0.001). In conclusion, retired athletes with rmTBI have MB atrophy, potentially contributing to memory impairment linked to the Papez circuit disconnection.
Similar content being viewed by others
Introduction
Contact-sport athletes who receive repetitive concussive and subconcussive blows to the brain can develop cognitive and behavioral impairments after retirement; these were formerly described as punch–drunk syndrome or dementia pugilistica1,2. Repetitive mild traumatic brain injury (rmTBI) differs from single moderate or severe TBI in its clinical characteristics from acute to chronic phase, the pattern of recovery, and long-term sequelae, and is a risk factor for late-onset and long-lasting neurocognitive disturbances3 that often persist throughout life. Among the diverse cognitive impairments that follow rmTBI, the most frequently observed symptom is memory impairment, which leads to a reduced quality of life for retired athletes2. However, the underlying mechanisms linking rmTBI exposure through contact sports to persistent memory impairment is poorly understood (e.g., white matter dysfunction, inflammation, aging effects, and neurodegenerative changes)4
Previous neuroimaging modalities, such as computed tomography (CT) and conventional magnetic resonance imaging (MRI), have shown ventricular enlargement, cavum septum pellucidum, and cavum vergae5,6, which have been suggested to be signs indicating past exposure to rmTBI. However, the sensitivity of sports-related brain imaging findings is not sufficient for diagnosis due to a large amount of diversity in the neuropathological changes caused by rmTBI and the interindividual variability in severity7. In addition, in some contact sports, there are no substantial structural abnormalities on MRI8,9. Therefore, it may be suggested that consistent findings related to rmTBI are not fully available. Furthermore, there is no clear relationship between these findings and cognitive testing scores10,11. These problems make the diagnosis of long-term cognitive dysfunction due to rmTBI extremely difficult.
A typical delayed-onset condition caused by rmTBI is chronic traumatic encephalopathy (CTE). McKee et al. reported that postmortem CTE brains manifest broad and various macroscopic features, including ventricular enlargement, cavum septum pellucidum or cavum vergae, frontal and temporal atrophy, thinning of the hypothalamic floor and corpus callosum (CC), and shrinkage of mammillary bodies (MBs)12,13. The MBs transmit information from the hippocampus to the anterior thalamic nuclei through the mammillothalamic tract. The CC is anatomically located between the fornix and the cingulate gyrus. These are vital links in the memory system within the Papez circuit14. Prior concussion is a risk factor for increased hippocampal atrophy and the development of mild cognitive impairment in former National Football League athletes, with an average age in their late 50 s15. However, there have been no reports on whether memory impairment in retired athletes with rmTBI is associated with atrophy of brain regions comprising the Papez circuit such as MBs and CC.
The purpose of this study was to identify changes in the regional brain volume related to long-term exposure to rmTBI in retired athletes. This study also evaluated whether changes in regional brain volumes are associated with neurocognitive dysfunction.
Methods
Approval
This study was approved by the Institutional Review Board of the National Institute of Radiological Sciences, Chiba, Japan. The study was registered with the University Hospital Medical Information Network Clinical Trials Registry (UMIN 000013517 and UMIN 000030248). All research was performed in accordance with relevant guidelines/ regulations and the Declaration of Helsinki. Written informed consent was obtained from each participant after providing a complete explanation of the study.
Participants
Participants with rmTBI were recruited from hospitals affiliated to the Keio University School of Medicine and other general hospitals in the metropolitan Tokyo area. Those enrolled in this study fulfilled the following criteria4: (i) had a history of head injury, engaged in contact sports for > 2 years, and received multiple concussions; (ii) age ≥ 20 years; (iii) absence of any neuropsychiatric or neurological disorders before or within 1 year of the head injury; and (iv) absence of severe physical diseases. The exclusion criteria included a history of other neurological diseases, an inability to obtain adequate images due to artifacts, and MRI abnormalities. Thus, we excluded one participant with rmTBI due to inadequate image quality. None of the rmTBI participants displayed chronic trauma-related lesions (e.g., cerebral contusions, traumatic subdural hematoma, or microbleeds) on conventional T2-weighted imaging (T2WI), fluid-attenuated inversion recovery (FLAIR), or susceptibility-weighted imaging (SWI), and no participants were excluded due to MRI abnormalities. Age- and sex-matched healthy control participants without a history of TBI or other neurological/psychiatric diseases were recruited from the volunteer association of the National Institutes for Quantum Science and Technology. All healthy control (HC) participants had normal results on conventional imaging.
Image acquisition
All studies were performed using a 3 T MRI system (MAGNETOM Verio 3 T, Siemens Healthcare; Erlangen, Germany) equipped with a 32-channel head coil. T1-weighted three-dimensional (3D) magnetization-prepared rapid acquisition gradient echo (MPRAGE) scans were acquired using the following parameters: field of view = 250 mm, TR/TE = 2300/2 ms, 512 × 512 matrix, slice thickness = 1 mm, acquisition time = 4 min 33 s.
Quantitative volumetric analysis
Two readers (Reader 1: 17, Reader 2: 13 years of experience in diagnostic neuroradiology) blinded to the participants’ information conducted manual 3D segmentation of the MPRAGE using ITK–SNAP (Insight segmentation and registration toolkit–Snake automatic partitioning; Penn Image Computing and Science Laboratory, University of Pennsylvania, Philadelphia, PA)16. The DICOM datasets were imported into the ITK–SNAP and presented in sagittal, coronal, and axial slices. The open-source medical imaging program ITK–SNAP is based on geodesic active-contour and region competition methods; it provides manual and semi-automatic tools to measure the volumes of anatomical regions of interest16. The program has been validated previously for volumetric and morphometric analyses of the caudate nucleus17. The programs computed the volume of the lesions in cubic millimeters. Two readers independently measured the following volumes as brain structures reported abnormalities in the CTE pathology13: the MBs, caudate nucleus, putamina, globus pallidus, talus, hippocampus, amygdala, and CC (Fig. 1). Total brain volume (TBV) was estimated using SPM12 (Wellcome Department of Cognitive Neurology, Institute of Neurology; London, United Kingdom), which is available online at https://www.fil.ion.ucl.ac.uk/spm/).
Cognitive assessments
The cognitive function of the rmTBI group was assessed using the following neuropsychological tests described in our previous report4: the Mini-Mental State Examination for global cognitive function; the logical memory in the Wechsler Memory Scale–revised test (LM; immediate and delayed recall) for verbal memory; the Rey–Osterrieth Complex Figure Test (ROCFT; copy and delayed recall) for visual memory; the digit span (forward and backward) for attentional function; and the verbal fluency test (category and initial letter), Wisconsin Card Sorting Test (WCST, Keio Version), and Stroop Test (I, II, and III) for executive function. Data from the Stroop Test were missing for one participant.
Statistical analysis
The characteristics of the participants are presented as the mean ± standard deviation (range) for each item. The Mann–Whitney U test was used to compare the TBV, regional brain volumes, and ratio of the regional brain volume to the TBV (the regional brain volume/TBV ratio) between the rmTBI and HC groups. In the rmTBI group, the regional brain volume/TBV ratio, which was p < 0.05 by the Mann–Whitney U test, was subjected to partial correlation analysis using age and sex as covariates to evaluate its relationship with cognitive assessment test results, and sex as covariate with other clinical parameters. The Bonferroni-corrected significance was set at p < 0.006 for comparison analysis and p < 0.005 for correlation analysis to account for multiple testing, and a lenient threshold p < 0.05 was considered to suggest a causal relationship. Interobserver repeatability between the two readers for quantitative assessment was evaluated using the intraclass correlation coefficient (ICCs) calculation mode l—a single rater, absolute agreement, two-way random-effects model. Values less than 0.5 indicate poor reliability, values between 0.5 and 0.75 suggest moderate reliability, values between 0.75 and 0.9 indicate good reliability, and values greater than 0.90 indicate excellent reliability18. All statistical analyses were performed using the IBM Statistical Package for Social Sciences (SPSS) Statistics (version 29) software (SPSS Inc., Chicago, IL, USA).
Results
There were 27 rmTBI participants, with a mean age of 43.9 ± 10.9 (31–69) years and 13.7 ± 2.4 (9–18) years of education; of these, 24 (88.9%) were male. Their sports professions were boxing (n = 18, 66.7%), kickboxing (n = 3, 11.1%), wrestling (n = 2, 7.4%), snowmobiling (n = 1, 3.7%), rugby (n = 1, 3.7%), ice hockey (n = 1, 3.7%), and American football (n = 1, 3.7%). The mean duration since the first injury was 24.0 ± 9.5 (9–47) years, and duration of exposure to rmTBI 15.4 ± 9.4 (12–25) years. No rmTBI participants had a history of severe and moderate TBI, family history of hereditary neurodegenerative disease. Three of rmTBI particiants were diagnosed with an alcohol use disorder, but none had a history of other substance use disorders. The HC group included 23 participants with a mean age of 45.1 ± 14.0 (23–69) years; of these, 20 (87.0%) were male. The data for the characteristics of the rmTBI and control participants are summarized in Table 1.
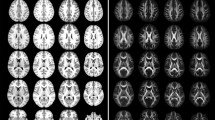
Table 2 shows the comparison results between the rmTBI and HC groups. There was no significant between-group difference in TBV (rmTBI vs. HC: 1.12 ± 0.13 vs. 1.17 ± 0.12 × 103 cm3). However, the regional brain volumes of the MBs and CC were significantly smaller in the rmTBI group than in the HC group (rmTBI vs. HC: 0.14 ± 0.05 vs. 0.22 ± 0.03 cm3 for the MBs and 13.9 ± 1.77 vs. 15.9 ± 2.32 cm3 for CC; p < 0.001), and that of the thalami were causally smaller in the rmTBI group, as assessed by Reader 1 (13.6 ± 2.08 vs. 14.9 ± 2.01 cm3; p = 0.04, not significant after Bonferroni correction) (Fig. 2). The other regional brain volumes showed no significant difference. The ratio of the MBs /TBV was significantly smaller in the rmTBI group than that in the HC group (0.13 ± 0.05 vs. 0.19 ± 0.03 × 10–3; p < 0.001), and the CC/TBV was smaller in the rmTBI group, as assessed by Reader 1 (12.5 ± 1.63 vs. 13.6 ± 1.81 × 10–3; p = 0.03). The other regional volume-to-TBV ratios showed no significant difference. See the result of Reader 2 to the Supplemental Table 1.
Comparison of the mammillary bodies (MBs) and the corpus callosum (CC) on sagittal (a–c) and coronal (d–f) images. (a,d) A control participant in their 40 s. (b,e) A professional kickboxer in their 40 s with mild atrophy of the MBs and the CC. (c,f) A professional boxer in their 40 s with severe atrophy of the MBs and the CC.
The cognitive scores of the rmTBI group are shown in Table 3. In partial correlation analysis, the ratio of the MBs volume/TBV was positively correlated with the results of the ROCFT delayed recall (r = 0.62, p < 0.001) (Fig. 3), and was a trend of correlation with LM for delayed recall (r = 0.51; p = 0.01, not significant after Bonferroni correction); it was not correlated with clinical parameters or other cognitive assessment results. The CC volume/TBV ratio was not correlated with any clinical data or any cognitive assessment results (p > 0.05).
The ICCs and 95% confidence intervals for the regions were MBs: 0.96 (0.93–0.97), putamina: 0.94 (0.80–0.97), globus pallida: 0.86 (0.79–0.90), caudate nuclei: 0.96 (0.95–0.98), thalami: 0.97 (0.97–0.99), hippocampi: 0.96 (0.94–0.97), amygdalae: 0.94 (0.91–0.96), and CC: 0.96 (0.92–0.98). The interobserver reproducibility between the two reviewers for measurements demonstrated good agreement for the globus pallida and excellent agreement for the other evaluated brain regions. See the result of Reader 2 to the Supplemental Table 2.
Discussion
This study evaluated regional brain volumes in retired athletes with a history of rmTBI and found that TBV-adjusted brain volumes of the MBs and CC were lower than those in HCs. In addition, the TBV-adjusted MB volume correlated with scores of the ROCFT delayed recall, and the TBV-adjusted CC volume did not correlate with any cognitive assessment results in rmTBI participants. Furthermore, the good or excellent interobserver agreement suggested that MRI-based evaluation methods for regional brain volumes using ITK–SNAP are applicable for individualized assessment of rmTBI. To the best of our knowledge, this is the first report to demonstrate MB atrophy and its association with the severity of memory impairment on an individual basis in rmTBI participants.
The MBs form a vital link in a putative memory system, comprising projections from the hippocampus to the MBs, connecting to the anterior thalamic nuclei14 through the mammillothalamic tract. Recent studies describing the role of the MBs in memory emphasize the importance of the hippocampal inputs to the region; the MBs are often referred to as part of an “extended hippocampal system”14. The presence of MB atrophy has been reported in various conditions, including Korsakoff’s syndrome19, postresection of colloid cysts in the third ventricle20, Alzheimer’s disease (AD)21, schizophrenia22, heart failure23, and sleep apnea24. Furthermore, recent evidence suggests that the MBs are important for memory highlights the memory problems associated with these conditions and the need to accommodate such problems25.
CTE is a persistent condition caused by rmTBI. The gross pathological findings of CTE include ventricular enlargement, cavum septum pellucidum or cavum vergae, frontal and temporal atrophy, thinning of the hypothalamic floor and the CC, and shrinkage of the MBs12,13. Particularly, shrinkage of the MBs is a characteristic finding for CTE and is one of the supportive neuropathological findings in the consensus criteria26. Furthermore, MB dysfunction is suggested to play a significant role in producing memory loss, cognitive impairment, and eventual dementia27. However, the exact mechanism underlying MB shrinkage in CTE is unknown.
One hypothesis for the cause of MB atrophy in rmTBI is a direct traumatic injury to the hypothalamus, including the MBs. The hypothalamus is one of the brain regions vulnerable to injury from head trauma. A report based on 15 cases of severe TBI identified four anatomical lesions by examining serial histological sections of the hypothalamus: (1) lesions of the supraoptic and paraventricular nuclei, (2) lesions of the infundibulum, (3) lesions in and around the third ventricle, and (4) lesions of the MBs. Lesions in all four areas were consistently found in all TBI patients28. Furthermore, infarction and hemorrhage were less frequently observed in the MBs, but gliosis and loss of neurons were observed, especially in longstanding cases28. In previous MR imaging analyses, detected disruption of fornical fibers after TBI, including the MBs, using diffusion tensor imaging with anisotropy measures and tractography29,30,31. In addition, a reduction in the volume of the fornix and atrophy elsewhere, including the CC and hippocampus, were observed in a long-term course after TBI32,33. These neuropathological and neuroimaging results may help explain the cause of the rmTBI-related MB atrophy in our study.
Another potential mechanism for MB atrophy in rmTBI participants is neurodegeneration. Axonal injury and rmTBI might trigger molecular pathways that result in the aggregation of proteins prone to pathological accumulation in neurodegenerative disease, including phosphorylated tau (p-tau), TAR DNA-binding protein 43 kDa, α-synuclein, and amyloid-ß, thereby increasing the likelihood of frontotemporal lobar degeneration, Lewy body disease, or AD27,29. Multiple epidemiological studies have shown that trauma is a risk factor for dementia, especially AD29. Among neuropathological findings in patients with early-stage AD, only 60% of the patients had senile plaques and/or NF neurofibrillary tangles in the MBs20. In addition, age and dementia are accompanied by a loss of MB volume without neuronal loss30 or neuronal atrophy31. Furthermore, abnormal p-tau immunoreactive neuronal and astrocytic aggregates in subcortical nuclei, including the MBs, are a supportive neuropathological feature in the Preliminary National Institute of Neurological Disorders and Stroke criteria for the pathologic diagnosis of CTE27. However, not a single study to date has succeeded in demonstrating that MB atrophy is directly linked to TBI-induced tau accumulation or other TBI-related neurodegenerative changes. Thus, these data suggest that MB atrophy in rmTBI may not only be affected by neurodegenerative disease but may also be produced by direct traumatic injury or by lesions coexisting in other memory-related areas, such as the medial thalamus, mammillothalamic tract, descending columns of the fornix, amygdalofugal pathways, or by other neuronal pathologies.
The current study showed that, in rmTBI participants, MB atrophy occurs, and the MBs volume/TBV ratio correlates with the ROCFT delayed recall. To the best of our knowledge, this is the first study to quantitatively evaluate the relationship between the MBs volume and memory performance in rmTBI participants. Our findings suggest that MB atrophy may serve as an index for the severity of visual memory impairment in rmTBI participants. Furthermore, memory impairment may be attributed to a disconnection between the MBs and the anterior nuclei of the thalamus, which are a part of the Papez circuit. Previous reports on retired National Football League (NFL) players with a history of concussions demonstrated significant reductions in hippocampal volumes and deficits in episodic memory15. In addition, after the late 50 s, atrophy of the hippocampus was more pronounced in the players than in HCs15. In our study, 85% of the rmTBI participants were aged < 55 years; the hippocampal volume was not significantly different from that of the HC group in the NFL study15. It should be noted that our results suggest that the MB atrophy in rmTBI precedes the volume reduction of the hippocampus and may be related to memory impairment in the early stage.
The present study also revealed atrophy of the CC in rmTBI participants, The present study also demonstrated the CC/TBV was smaller in the rmTBI group but not significant after multiple comparisons, as measured by volumetric analysis. The CC is particularly vulnerable to shearing forces or rotation of the brain due to trauma32. Our results are consistent with those of previous studies on CC injury in concussion or mild TBI33. The CC is crucial for the normal interhemispheric transfer of sensory, motor, attentional, and executive information34. Anterior callosal regions, such as the genu, contain fibers from the prefrontal cortex, whereas the body (proceeding from front to back) contains fibers from the premotor, motor, somatosensory, parietal, and temporal cortices35. Previous studies suggested that trauma-induced atrophy of the CC likely occurs as a consequence of complex neuropathological features. Another report suggested that active boxers had an average yearly rate of decline in the volumes of the central corpus callosum, but retired boxers did not show progression of atrophy in the CC36. These features involve both direct trauma to the CC37 and secondary Wallerian degeneration occurring because of diffuse damage elsewhere in the brain, disrupting the integrity of white matter tracts38. Other studies have reported an association between white matter alterations (e.g., volume and microstructure) and cognitive function in TBI39. Our study showed that the CC volume/TBV ratio was not correlated with age, duration since the first injury, or any cognitive assessment results. This result may reflect the heterogeneity of CC damage and widespread white matter alternation in rmTBI participants.
This study had some limitations. First, the relatively small sample size of this study requires caution in interpreting the results, and the study should be conducted with a larger sample. Second, only Japanese participants were evaluated; thus, the results should be interpreted cautiously because post-TBI outcomes differ according to genetic associations among Caucasians, African-Americans, Hispanic, and Asians40. In addition, racial variations in physique may contribute to the extent of brain trauma. Third, the sports professions varied. A previous study found differences in impact velocity and head injury criteria between boxing and American football41. Therefore, differences in MB or CC atrophy in rmTBI should be examined by sport. Future research should investigate the longitudinal associations between MB atrophy and the prognosis of behavioral or cognitive impairment in rmTBI to determine whether MB atrophy can be used as an imaging marker. Fourth, previous reports have indicated that mild TBI often remains undiagnosed and untreated42, and rmTBI patients with severe post-injury symptoms exhibit stronger recall bias43. Therefore, an exact number of rmTBI is difficult to estimate using self-reported information and the number of confirmed diagnoses by a physician. Fifth, the lack of neuropsychological test data from healthy controls makes clinical interpretation of cognitive dysfunction in rmTBI participants difficult. Sixth, although no participants showed abnormal findings on conventional T2WI, FLAIR, or SWI, the possibility that diffuse axonal injury without microbleeds affected the current results couldn’t be ruled out. Finally, there were limitations in controlling for lifestyle, genetic background, and environmental factors of the participants to demonstrate the association between rmTBI and MB atrophy.
In conclusion, retired athletes with a long history of rmTBI have MB atrophy, and this may be related to memory impairment associated with disconnection of the MBs from the Papez circuit.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the anonymity of the patients but are available from the corresponding author on reasonable request.
References
Critchley, M. et al. Medical aspects of boxing, particularly from a neurological standpoint. Br. Med. J. 1, 357–362 (1957).
Asken, B. M. et al. Factors influencing clinical correlates of chronic traumatic encephalopathy (CTE): A review. Neuropsychol. Rev. 26, 340–363 (2016).
Klein, M. et al. Long-term persisting cognitive sequelae of traumatic brain injury and the effect of age. J. Nerv. Ment. Dis. 184, 459–467 (1996).
Takahata, K. et al. PET-detectable tau pathology correlates with long-term neuropsychiatric outcomes in patients with traumatic brain injury. Brain 142, 3265–3279 (2019).
Bodensteiner, J. B. et al. Dementia pugilistica and cavum septi pellucidi: Born to box?. Sports Med. 24, 361–365 (1997).
Koerte, I. K. et al. Cavum septi pellucidi in symptomatic former professional football players. J. Neurotrauma 33, 346–353 (2016).
Shenton, M. E. et al. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 6, 137–192 (2012).
Koerte, I. K. et al. White matter integrity in the brains of professional soccer players without a symptomatic concussion. JAMA 308, 1859–1861 (2012).
Zhang, L. et al. Diffusion anisotropy changes in the brains of professional boxers. AJNR Am. J. Neuroradiol. 27, 2000–2004 (2006).
Wilson, J. T. The relationship between neuropsychological function and brain damage detected by neuroimaging after closed head injury. Brain Inj. 4, 349–363 (1990).
Levin, H. S. et al. Serial MRI and neurobehavioural findings after mild to moderate closed head injury. J. Neurol. Neurosurg. Psychiatry 55, 255–262 (1992).
Iverson, G. L. et al. Chronic traumatic encephalopathy neuropathology might not be inexorably progressive or unique to repetitive neurotrauma. Brain 142, 3672–3693 (2019).
McKee, A. C. et al. The neuropathology of chronic traumatic encephalopathy. Brain Pathol. 25, 350–364 (2015).
Aggleton, J. P. et al. Episodic memory, amnesia, and the hippocampal-anterior thalamic axis. Behav. Brain Sci. 22, 425–444 (1999).
Strain, J. F. et al. Imaging correlates of memory and concussion history in retired national football league athletes. JAMA Neurol. 72, 773–780 (2015).
Yushkevich, P. A. et al. User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 31, 1116–1128 (2006).
Vallaeys, K. et al. 3D dento-maxillary osteolytic lesion and active contour segmentation pilot study in CBCT: Semi-automatic vs manual methods. Dentomaxillofac. Radiol. 44, 20150079 (2015).
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15, 155–163 (2016).
Kopelman, M. D. The Korsakoff syndrome. Br. J. Psychiatry 166, 154–173 (1995).
Denby, C. E. et al. The frequency and extent of mammillary body atrophy associated with surgical removal of a colloid cyst. AJNR Am. J. Neuroradiol. 30, 736–743 (2009).
Grossi, D. et al. Mamillary bodies in Alzheimer’s disease. Acta Neurol. Scand. 80, 41–45 (1989).
Briess, D. et al. Mamillary body abnormalities in schizophrenia. Lancet 352, 789–790 (1998).
Kumar, R. et al. Mammillary bodies and fornix fibers are injured in heart failure. Neurobiol. Dis. 33, 236–242 (2009).
Kumar, R. et al. Reduced mammillary body volume in patients with obstructive sleep apnea. Neurosci. Lett. 438, 330–334 (2008).
Vann, S. D. et al. The mammillary bodies: Two memory systems in one?. Nat. Rev. Neurosci. 5, 35–44 (2004).
McKee, A. C. et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 131, 75–86 (2016).
McKee, A. C. et al. The spectrum of disease in chronic traumatic encephalopathy. Brain 136, 43–64 (2013).
Treip, C. S. Hypothalamic and pituitary injury. J. Clin. Pathol. Suppl. (R Coll Pathol) 4, 178–186 (1970).
Plassman, B. L. et al. Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology 55, 1158–1166 (2000).
Wilkinson, A. et al. The influence of age and dementia of the neurone population of the mammillary bodies. Age Ageing 7, 151–160 (1978).
Ishunina, T. A. et al. Changes in metabolic activity and estrogen receptors in the human medial mamillary nucleus: Relation to sex, aging and Alzheimer’s disease. Neurobiol. Aging 24, 817–828 (2003).
Gentry, L. R. et al. Prospective comparative study of intermediate-field MR and CT in the evaluation of closed head trauma. AJR Am. J. Roentgenol. 150, 673–682 (1988).
Kim, D. S. et al. Radiologic determination of corpus callosum injury in patients with mild traumatic brain injury and associated clinical characteristics. J. Korean Neurosurg. Soc. 58, 131–136 (2015).
Gazzaniga, M. S. Cerebral specialization and interhemispheric communication: Does the corpus callosum enable the human condition?. Brain 123, 1293–1326 (2000).
Witelson, S. F. Hand and sex differences in the isthmus and genu of the human corpus callosum. A postmortem morphological study. Brain 112, 799–835 (1989).
Bernick, C. et al. Longitudinal change in regional brain volumes with exposure to repetitive head impacts. Neurology 94, 232–240 (2020).
Mac Donald, C. L. et al. Detection of traumatic axonal injury with diffusion tensor imaging in a mouse model of traumatic brain injury. Exp. Neurol. 205, 116–213 (2007).
Wu, T. C. et al. Longitudinal changes in the corpus callosum following pediatric traumatic brain injury. Dev. Neurosci. 32, 361–373 (2010).
Spitz, G. et al. White matter integrity following traumatic brain injury: the association with severity of injury and cognitive functioning. Brain Topogr. 26, 648–660 (2013).
Arango-Lasprilla, J. C. et al. Race/ethnicity differences in satisfaction with life among persons with traumatic brain injury. NeuroRehabilitation 24, 5–14 (2009).
Viano, D. C. et al. Concussion in professional football: comparison with boxing head impacts–part 10. Neurosurgery 57, 1154–1172 (2005).
Meehan, W. P. 3rd. et al. The prevalence of undiagnosed concussions in athletes. Clin. J. Sport. Med. 23, 339–342 (2013).
Silverberg, N. D. et al. The Nature and Clinical Significance of Preinjury Recall Bias Following Mild Traumatic Brain Injury. J. Head Trauma Rehabil. 31, 388–396 (2016).
Acknowledgements
We gratefully acknowledge the support of many colleagues in the study, including members of the National Institutes for Quantum Science and Technology, Keio University School of Medicine, and Juntendo University School of Medicine. We also thank Katsuyuki Tanimoto, Takamasa Maeda, and the members of the Translational Team for their support with MRI scans, and we thank Shizuko Kawakami and Haruka Yamashita for their assistance as clinical coordinators.
Funding
Japan Society for the Promotion of Science,22K07727,20K07935,21H02805,22H02998,General Insurance Association of Japan,2019–2020,Health and Labour Sciences Research,20GC1018 and 22GC1004,Celgene,Japan Agency for Medical Research and Development,P18dm0207018,JP19dm0207072,JP18dk0207026,and JP19dk0207049
Author information
Authors and Affiliations
Contributions
M.Miy., K.Tak., M.Mim. and M.H. planned and designed the study and wrote the manuscript. K.Tak. and M.Mim. recruited the patients. Y.S., Y.Y., S.K., H.E., K.Tag., M.O., K.H. and F.S. helped with implementation. M.K. and K.M. analyzed data. K.K. and S.A. developed the methodology and gave technological support. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
This work was supported in part by grants from the Celgene Corporation through the MDS Foundation. It was also supported by grants-in-aid from the Japan Agency for Medical Research and Development under grant numbers JP18dm0207018, JP19dm0207072, JP18dk0207026, and JP19dk0207049 to MH, Japan Society for the Promotion of Science (JSPS) KAKENHI 22K07727 to Mari Miyata (managed at Juntendo University), JSPS KAKENHI 20K07935, 21H02805 and the General Insurance Association of Japan (2019–2020) to KTak, JSPS KAKENHI 22H02998 to KM, and Health and Labour Sciences Research Grant 20GC1018 and 22GC1004 to MMim.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miyata, M., Takahata, K., Sano, Y. et al. Association between mammillary body atrophy and memory impairment in retired athletes with a history of repetitive mild traumatic brain injury. Sci Rep 14, 7129 (2024). https://doi.org/10.1038/s41598-024-57383-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57383-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.