Abstract
To investigate the risk factors for new renal scarring (NRS) in children with vesicoureteral reflux (VUR) receiving continuous antibiotic prophylaxis (CAP). This was a single-center cohort study. The clinical data of 140 children with grade I–V VUR receiving CAP were analyzed. In this study, exposure variables were sex, younger age at the initial diagnosis of UTI ≤ 12 months, the occurrence of breakthrough urinary tract infection (BT-UTI), high-grade VUR, bilateral VUR, etiology, presence of renal scarring at the initial diagnosis and ultrasound abnormalities. The outcome was NRS. A total of 140 children were included in the risk factor analysis of NRS, 73 of whom experienced NRS, an incidence rate of 52.14%. Multivariate Cox regression suggested that the presence of renal function impairment after the initial diagnosis of UTI (OR 3.411, 95% CI 1.5751–6.646) and the occurrence of BT-UTI while receiving CAP (OR 1.995, 95% CI 1.089–2.958) were independent risk factors for NRS. Multivariate Cox regression showed that high-grade VUR had no significant effects on NRS (OR 0.940, 95% CI 0.462–1.912, P = 0.864). No significant difference was identified in multivariate Cox regression analysis in the IV–V group (vs I–III group) (OR 0.960, 95% CI 0.565–1.633, P = 0.960). Renal function impairment after the initial diagnosis of UTI and the occurrence of BT-UTI while receiving CAP were independent risk factors for NRS. Neither univariate analysis nor multivariate analysis found a correlation between VUR grade and NRS.
Similar content being viewed by others
Introduction
Vesicoureteral reflux (VUR) is a disease involving the reflux of urine from the bladder to the ureter or pelvis; VUR is one of the most common congenital kidney and urinary tract malformations in children, and children with VUR are at high risk for breakthrough urinary tract infection (BT-UTI), and 5‒10% of will experience decreased glomerular filtration rates. This leads to reflux nephropathy, which eventually leads to hypertension, albuminuria, chronic renal impairment, and even renal failure in some children1,2,3,4. Reflux nephropathy usually has no obvious clinical manifestations in the early stage, and its pathology is characterized by patchy interstitial scarring, tubular atrophy, and nephron atrophy. The mechanism of VUR-induced regurgitant nephropathy is not well understood. Repeated urinary tract infections and immune impairment are thought to contribute to regurgitant nephropathy5,6. Current therapeutic strategies for VUR are aimed at reducing the occurrence of new BT-UTIs and kidney function impairment7,8. Recurrent BT-UTI in VUR children is prone to new renal scarring, which can also affect their long-term prognosis, with the potential risk of developing hypertension, albuminuria, renal impairment, and even renal failure6. This study aimed to analyze the clinical data of children receiving CAP treatment for VUR in our hospital from 2016 to 2019, with the purpose of summarizing the risk factors for new kidney scarring in children with VUR.
Patients and methods
This is a retrospective cohort study included 213 children with vesicoureteral reflux (VUR) receiving CAP study. Children seeking treatment due to febrile UTI at the outpatient clinic or inpatient ward of the Department of Nephrology, Children's Hospital of Xiamen, between January 2016 and June 2019 were enrolled in the study. These children were diagnosed with VUR by micturating cystourethrography (MCU) and received CAP intervention. They all receiving regular CAP and following-up by specialist every month through phone or outpatient service. The exclusion criteria were as follows: no follow-up DMSA scan, secondary VUR (neuropathic bladder, posterior urethral valve, congenital tethered cord syndrome), stage 5 chronic kidney disease, genital malformations (urethro-rectal fistula, recto-vesical fistula), and congenital immunodeficiency. A total of 140 children were included in the analysis of risk factors for NRS (Fig. 1). This cohort study was approved by the medical ethics committee of Children's Hospital of Xiamen. We confirmed that all methods were performed in accordance with the relevant guidelines and regulations. The diagnosis and grading were based on the VUR classification (grade I–V) developed by the International Reflux Study Committee9. The classification of bilateral VUR was determined according to the side with a higher reflux grade. After the diagnosis of VUR, all patients received CAP. CAP was given in a single oral dose per night (one-quarter to one-third of a daily dose). Antibiotics (nitrofurantoin enteric-coated tablets, sulfamethoxazole tablets, etc.) were selected according to the bacterial susceptibility and were orally administered. The treatment was individualized for each child, CAP is empirically recommended until age of toilet training. The diagnostic criteria of BT-UTI included: (1) body temperature higher than 38 ℃; cloudy, foul-smelling urine or symptoms such as urinary urgency, dysuria, and back pain; (2) abnormal midstream clean-catch urine laboratory values: leukocytes > 5/high-power field and positive urinary leukocyte esterase; (3) urine culture: bacterial growth in midstream urine > 105 colony-forming units (CFU)/mL5. In our study, obtaining urine samples for non-toilet-trained children include clean catch, bag, in–out catheterisation.
DMSA scan
Kidney dimercaptosuccinic acid (DMSA) scan interpretation: 99mTc-DMSA renal static imaging was performed. After receiving an intravenous injection of 22.2–185.0 MBq imaging agent (1.85 MBq/kg body weight) for 3–4 h, children were placed in the supine position, and static imaging in the anteroposterior view was performed using a low-energy high-resolution parallel-hole collimator with a field of view that included both kidneys and the bladder, energy peak 140 keV, window width 20%, matrix 512 × 512, magnification 2.19, and radioactivity count 1.8 × 106. The 99mTc-DMSA renal imaging protocol and result assessment followed the clinical guideline of the Society of Nuclear Medicine and Molecular Imaging10,11. The time between index UTI and first DMSA was 1 (0.6) months. New renal scarring was assessed by DMSA performed minimally 12 months after the treatment of UTI, and median time was 16 (12,27)months. The interpretations of the DMSA was made by experienced nuclear medicine consultants and experienced radiologists. Normal imaging was considered to be a normal location, morphology, and contour of both kidneys and a uniform distribution of radioactivity in the renal parenchyma. The percentage of renal function on each side (differential renal function) was calculated by delineating the kidney regions of interest and background using computer, and a differential renal function greater than 10% was considered renal impairment. One or more focal radioactivity reductions or defects in the renal cortex, with contraction or volume reduction of the affected cortex, or wedge-shaped defects denoted renal scarring11. NRS was defined as the occurrence of new renal scarring or aggravation of existing renal scarring on a DMSA re-scan while receiving CAP11 (Fig. 2).
Study design
The VUR children were divided into an NRS group and an NRS-free group based on the presence or absence of renal scarring observed during the follow-up DMSA scan. The risk factors that were analyzed were were sex, age, pathogens (Escherichia coli and non-E. coli) at the initial diagnosis of UTI, VUR grade, unilateral or bilateral VUR, presence or absence of renal scarring on a DMSA scan after the initial diagnosis of UTI, presence or absence of renal function impairment diagnosed by DMSA after the initial diagnosis of UTI, and ultrasound abnormalities.
Statistical analysis
Measurement data are expressed as means ± standard deviation, and count data are presented as percentages (%). Univariate analysis was performed using the Kaplan–Meier analysis test for comparisons between groups. Cox regression was used to evaluate individual variables as independent risk factors for NRS. P < 0.05 was considered statistically significant. Data analysis was performed with SPSS 22.0 software.
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by Ethical committee of Children Hospital of Xiamen (XMSETYY-2020-123). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Results
General information
A total of 140 children were included in this study, including 72 males and 68 females, with a median age of 5 months (range from 1 to 56 months). The median follow-up time was 18.3 months. None of the male patients had been circumcised. All VUR children received MCU after being diagnosed with febrile UTI. Of these patients, 70 had unilateral VUR, 70 had bilateral VUR, and VUR was present in a total of 210 ureters. There were 8 children with grade I VUR (5.71%), 14 with grade II (10%), 59 with grade III (42.14.%), 39 with grade IV (27.86%), and 20 with grade V (14.29%) ( Table 1).
Baseline demographic and clinical characteristics
The 140 children who underwent DMSA re-scanning were divided into an NRS group and a non-NRS group for risk factor analysis. Chi-squared tests were used to compare the normal distribution between groups. The NRS group was found the presence of renal function improvement after the initial diagnosis of UTI and the presence of renal scaling at the initial diagnosis, with statistically significant differences between the groups (P < 0.05); There was no statistically significant difference between the other groups (P > 0.05) (Table 2).
Risk factors for NRS
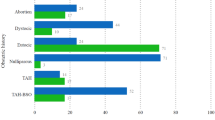
Among the 140 children who received CAP, 73 experienced NRS, for an incidence rate of 52.14%. 53 children were detected one new scar, 15 were detected two new scars and 6 were detected three or more new scars. Univariate analysis showed that younger age at the initial diagnosis of UTI (≤ 12 months), the presence of renal function impairment after the initial diagnosis of UTI, BT-UTI and the presence of renal scarring at the initial diagnosis were correlated with NRS (P < 0.05). Multivariate Cox regression included the correlated factors with P < 0.05 in the univariate analysis and VUR grade. The results suggested that the presence of renal function impairment after the initial diagnosis of UTI (OR 3.411, 95% CI 1.751–6.646, P = 0.001) and the presence of BT-UTI while receiving CAP were independent risk factors for NRS (OR 1.995, 95% CI 1.089–2.958, P = 0.000). The 140 children were divided into a high VUR-grade group (III–V) and a low VUR-grade group (I–II).
Univariate analysis showed that high-grade VUR had no significant effects on NRS (P = 0.032). Multivariate Cox regression was also conducted, and no significant effect was identified (OR 0.940, 95% CI 0.462–1.912, P = 0.864). When the VUR children were divided into grade IV–V and grade I–III VUR groups, univariate analysis showed that children in the IV–V group also showed no significant differences in terms of NRS (P = 0.571). No significant difference was identified in multivariate Cox regression analysis (OR 0.960, 95% CI 0.565–1.633, P = 0.960) (Table 3).
Discussion
In this study, the clinical data of 140 children with grade I–V VUR receiving CAP at the Department of Nephrology, Children's Hospital of Xiamen were analyzed. Children were grouped based on the presence or absence of NRS while receiving CAP. Children with renal function impairment on a DMSA scan after the initial diagnosis of UTI and who had BT-UTI while receiving CAP were more prone to NRS.
In this study, the time between index UTI and first DMSA was 1(0.6) months. Loukogeorgakis et al.12 performed a retrospective analysis on 61 VUR children found that renal scarring is the most significant risk factor for breakthrough UTI in primary VUR patients and could be used to determine those at risk of symptomatic VUR persistence. Harper et al. also found that abnormal post-UTI DMSA scan is associated with a higher risk of recurrence of UTI at 24 months13. So a DMSA scan for VUR children after the first urinary tract infection is necessary.
In this study, children with VUR receiving regular CAP and specialist follow-up still had renal scarring. 140 children underwent a follow-up DMSA scan, and 73 children had NRS, including 41 males and 32 females, an incidence of 52.14%. Even when active clinical intervention is given to children with VUR, 30–50% of children still experience renal scarring, which is consistent with the findings14,15. In some recent randomized studies, the number of cases reported with renal scarring in children with VUR correlated with patient sex. Studies with more males reported significantly more cases of renal scarring, which is more likely to be congenital than acquired RN16,17. For girls, the risk of BT-UTI remains higher overall and the new scars were acquired and found to be related to severe inflammatory processes, while in boys the renal damage was often congenital18.
Univariate and multivariate analyses showed that in VUR children received CAP, the recurrence of BT-UTI was independent risk factor for NRS. Sevgi et al.19 performed a retrospective analysis on 90 VUR children receiving CAP and found that BT-UTI was a risk factor for renal scarring. Previous studies have suggested that renal parenchymal infection is a prerequisite for renal scarring20,21. This study showed that the rate of renal scarring in children with BT-UTI was 1.995 times that in children without BT-UTI recurrence, indicating that renal parenchymal infection is an important condition for renal scarring. But Morello et al.22 performed a investigator-initiated, randomized, open-label trial analysis on 292 grade IV or V VUR children receiving CAP and found that the number of new lesions was independent of the occurrence of UTIs during the trial period. They also founded that new defects were identified in 27 of 144 participants (18.8%) who had no UTI and in 11 of 57 (19%) who had at least one UTI (rate ratio, 0.97; 95% CI 0.52 to 1.83)22. Some studies have suggested that VUR children older than 2 years at the initial diagnosis of UTI have a greater likelihood of renal scarring, which may be related to the lack of timely treatment due to their late diagnosis of UTI23,24. In the RIVUR study, children with a second UTI had significantly more renal scars when compared with those with a single UTI16. A post hoc analysis of the RIVUR and CUTIE (Careful Urinary Tract Infection Evaluation) studies revealed that the odds of renal scarring after a second febrile UTI were 11.8 times higher and after 3 or more febrile UTIs were 13.7 times greater than after a single febrile infection25.
Previous studies have found that in children with VUR who use CAP intervention, high-level VUR, especially IV-V grade VUR, is an independent risk factor for NRS26. Mattoo et al.5 found in a prospective randomized controlled clinical study (RIVUR) that children with IV-V grade VUR were more likely to develop BT-UTI and renal scars, 24.2 and 1.88 times higher than those with I–III grade VUR, respectively. Sitarah Mathias et al.27 also found that patients with high-grade VUR patients were more likely than those with low-grade VUR patients to have renal scarring (75% vs. 49%, p < 0.01), low eGFR (23% vs. 13%, p Z 0.04) and significant hypertension (26% vs. 13%, p Z 0.02). In our study, neither the univariate nor multivariate analysis found a correlation between VUR grade and NRS. This result may be related to the high proportion of high-grade VUR children included in this cohort (84.28% of III–V grade VUR children and 42.14% of IV-V grade VUR children).
This study has some limitations. First, the study was a single-center, small cohort study. Second, although the children were regularly followed up in our hospital, there was no quantitative standard for CAP compliance. In addition, there were some data defects during data acquisition, such as the lack of etiology during the initial diagnosis of UTI. These factors may have led to biased results. Multicenter, prospective clinical studies are needed to confirm the reliability of our results.
Conclusion
Renal function impairment after the initial diagnosis of UTI and the occurrence of BT-UTI while receiving CAP were independent risk factors for NRS. All of these factors require attention in clinical diagnosis and treatment.
Data availability
All data generated or analysed during this study are included in this published article.
References
Signorelli, M., Cerri, V., Taddei, F., Groli, C. & Bianchi, U. A. Prenatal diagnosis and management of mild fetal pyelectasis: Implications for neonatal outcome and follow-up. Eur. J. Obstet. Gynecol. Reprod. Biol. 118(2), 154–159 (2005).
Peters, C. A. et al. Summary of the AUA guideline on management of primary vesicoureteral reflux in children. J. Urol. 184(3), 1134–1144 (2010).
Austin, P. F. et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children’s Continence Society. Neurourol. Urodyn. 35(4), 471–481 (2016).
Meena, J. et al. Prevalence of bladder and bowel dysfunction in toilet-trained children with urinary tract infection and/or primary vesicoureteral reflux: A systematic review and meta-analysis. Front. Pediatr. 8, 84 (2020).
Mattoo, T. K. & Mohammad, D. Primary vesicoureteral reflux and renal scarring. Pediatr. Clin. North Am. 69(6), 1115–1129 (2022).
Mathias, S. et al. Risk factors for renal scarring and clinical morbidity in children with high-grade and low-grade primary vesicoureteral reflux. J. Pediatr. Urol. 18(2), 225 (2022).
Keren, R. et al. Risk factors for recurrent urinary tract infection and renal scarring. Pediatrics 136(1), e13-21 (2015).
Johnston, A. W. et al. Immune expression in children with vesicoureteral reflux: A pilot study. Urology 148, 254–259 (2021).
International Reflux Study Committee. Medical versus surgical treatment of primary vesicoureteral reflux: Report of the International Reflux Study Committee. Pediatrics. 67(3), 392–400 (1981).
Kawai, S., Kanai, T. & Hyuga, T. Top-down approach is possible strategy for predicting breakthrough fUTIs and renal scars in infants. Pediatr. Int. 59(7), 781–785. https://doi.org/10.1111/ped.13279 (2017).
Aboutaleb, H. et al. Correlation of renal scarring to urinary tract infections and vesicoureteral reflux in children. Adv. Urol. 2022, 9697931 (2022).
Loukogeorgakis, S. P. et al. Renal scarring is the most significant predictor of breakthrough febrile urinary tract infection in patients with simplex and duplex primary vesico-ureteral reflux. J. Pediatr. Urol. 16(2), 189.e1-189.e7 (2020).
Harper, L. et al. Children with abnormal DMSA nuclear scan present a higher risk of recurrent febrile urinary tract infections. World J. Pediatr. 15(2), 204–205 (2019).
Jodal, U., Smellie, J. M., Lax, H. & Hoyer, P. F. Ten-year results of randomized treatment of children with severe vesicoureteral reflux. Final report of the International Reflux Study in Children. Pediatr. Nephrol. 21(6), 785–792 (2006).
Zaki, M., Badawi, M., Al Mutari, G., Ramadan, D. & Adul, R. M. Acute pyelonephritis and renal scarring in Kuwaiti children: A follow-up study using 99mTc DMSA renal scintigraphy. Pediatr. Nephrol. 20(8), 1116–1119 (2005).
Mattoo, T. K. Vesicoureteral reflux and reflux nephropathy. Adv Chronic Kidney Dis. 18(5), 348–354 (2011).
Mattoo, T. K. et al. RIVUR Trial Investigators. Renal scarring in the randomized intervention for children with vesicoureteral Reflux (RIVUR) Trial. Clin. J. Am. Soc. Nephrol. 11(1), 54–61 (2016).
Swerkersson, S. et al. Relationship among vesicoureteral reflux, urinary tract infection and renal damage in children. J. Urol. 178(2), 647–651 (2007).
Al-Mendalawi, M. D. Risk factors for renal scarring in children with primary vesicoureteral reflux disease. Saudi J. Kidney Dis. Transpl. 24(3), 600–601. https://doi.org/10.4103/1319-2442.111082 (2013).
Garin, E. H., Orta-Sibu, N. & Campos, A. Primary vesicoureteral reflux in childhood. Adv Pediatr. 49, 341–357 (2002).
Polito, C. et al. High incidence of a generally small kidney and primary vesicoureteral reflux. J. Urol. 164(2), 479–482 (2000).
Morello, W. et al. PREDICT Study Group. Antibiotic prophylaxis in infants with grade III, IV, or V vesicoureteral reflux. N. Engl. J. Med. 389(11), 987–997 (2023).
Pirker, M. E. et al. Familial vesicoureteral reflux: Influence of sex on prevalence and expression. J. Urol. 176, 1776–1780 (2006).
Chiou, Y. Y., Wang, S. T., Tang, M. J., Lee, B. F. & Chiu, N. T. Renal fibrosis: Prediction from acutepyelonephritis focus volume measured at 99mTcdimercaptosuccinic acid SPECT. Radiology 221, 366–370 (2001).
Shaikh, N., Haralam, M. A., Kurs-Lasky, M. & Hoberman, A. Association of renal scarring with number of febrile urinary tract infections in children. JAMA Pediatr. 173(10), 949–952 (2019).
Shaikh, N., Ewing, A. L., Bhatnagar, S. & Hoberman, A. Risk of renal scarring in children with a first urinary tract infection: A systematic review. Pediatrics 126(6), 1084–1091 (2010).
Mathias, S. et al. Risk factors for renal scarring and clinical morbidity in children with high-grade and low-grade primary vesicoureteral reflux. J. Pediatr. Urol. 18(2), 225.e1-225.e8 (2022).
Funding
This study was supported by Xiamen City Health Guidance Project [Grant No.3502Z2021ZD1247].
Author information
Authors and Affiliations
Contributions
S.D. and Z.Z. contributed to the data analysis and drafted the manuscript. S.D. and H.H.L. contributed to the study design and critically revised the manuscript for important intellectual content. S.D., Z.Z., H.H. and Y.M. contributed to the patient follow-up and data collection. All authors have approved the final version of the manuscript to be published. Each author participated sufficiently in the work to be responsible for the content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Su, D., Zhuo, Z., Zhang, J. et al. Risk factors for new renal scarring in children with vesicoureteral reflux receiving continuous antibiotic prophylaxis. Sci Rep 14, 1784 (2024). https://doi.org/10.1038/s41598-024-52161-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52161-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.