Abstract
Intimate partner Violence (IPV) can affect any woman, irrespective of their economic status, religion, or culture. This is a human-rights issue and due to its prevalence and adverse effects on pregnancy and birth, it must be given greater attention. Further, there is a lack of data in the Tigray region about adverse birth outcomes due to intimate partner violence during pregnancy. The aim of this study was to assess intimate partner violence during pregnancy and its association with low birth weight and preterm birth in Tigray region. Across-sectional study design was used. 647 women were involved in the study. Simple random sampling techniques were employed to select health facilities and systematic sampling was used to select study participants. Data were entered using Epi info version 3.5.1 and was analyzed using SPSSversion 20. Logistic regression analysis was conducted to assess the association between exposure to intimate partner violence during pregnancy and preterm birth and low birth weight while adjusting for possible confounders. The prevalence of intimate partner violence during pregnancy was 7.3% and the prevalence of low birth weight and preterm birth were 18.5% and 10.8% respectively. There was a statistically significant association between exposure to intimate partner violence during pregnancy and low birth weight. After adjustment for socioeconomic status, women’s habits and obstetric factors, the pregnant women who were exposed to intimate partner violence during pregnancy were two times more likely to have a child with a low birth weight (2.39 (95% CI: 1.26–4.55)). The prevalence of intimate partner violence during pregnancy, low birth weight, and preterm birth in this study was high. Women who experienced intimate partner violence during pregnancy had an increased risk of low birth weight. These findings justify a call to the federal minster of health to take measures aimed at avoiding intimate partner violence during pregnancy to reduce adverse birth outcomes.
Similar content being viewed by others
Introduction
Intimate partner Violence (IPV) can occur in all groups of women irrespective of economic status, religion, or culture1. Currently it is a human rights issue, and due to its prevalence and adverse effects on birth outcomes, attention has been given to this topic worldwide2. Globally, 35% of women have experienced physical and or sexual intimate partner violence or non-partner sexual violence3. In Ethiopia, women experiencing IPV ranged from 23% experiencing physical violence to 10% experiencing sexual violence, with 4% of pregnant women facing physical violence4. Clinical studies from Africa have also reported that 3% of women experienced sexual violence and 49% experienced psychological violence during pregnancy2.
Women who were physically or sexually violated by their partner have a greater than 16% risk of giving birth to a low birth weight baby and have twice risk of abortion and depression, compared to their counterparts3. Low birth weight and preterm birth are the main predictors of neonatal mortality and morbidity. Globally, 15–20% of babies are born at a low birth weight, which represents 20 million birth per year5. An analysis across thirty studies from Ethiopia indicated that 17.3% of babies are delivered with low birth weight6. As consequences of low birth weight, newborn exposed to mental retardation, hypothermia, physical problem and hypoglycemia6.
More than 10% of babies are born preterm worldwide7. More than one million children die each year secondary to preterm birth7 and it is the main cause of mortality in the under-fives8 and the burden is more found in less developed countries and also affected both the life of mother and children9. Similarly in Ethiopia, from the total number of babies delivered, 10% of them are premature9.
Studies have shown that experiencing IPV during pregnancy increases the risk of low birth weight10,11,12. Similarly, some studies have indicated that IPV during pregnancy has a significant association with preterm birth11,12, while other studies have shown no such association13. There is lack of data on describing the rates of IPV during pregnancy in Ethiopia as a whole, and no studies have been reported in the Tigray region. Moreover, the association between IPV and the rates of low birth weight and preterm birth has not been investigated in the study area, and this study aims to fill this gap. The findings from this study may also be used as baseline for further study in the area.
Since violence is a problem globally, and low birth weight and preterm birth are the leading causes of neonatal mortality and morbidity, this study aimed to address the research gap by characterizing the rate of IPV during pregnancy and quantifying its association with low birth weight and preterm birth.
Methods
Study setting and design
The Tigray region is located 783 km from Addis Ababa, capital city of Ethiopia. According to the 2007 census, the population was estimated to be 4,316,988. Women of childbearing age (15–49) comprised 251,650 of this population. According to the 2015 Tigray regional health bureau annual report, the area hosts a total of one specialized hospital, 15 general hospitals, 22 primary hospitals, 204 health centers, 712 health posts, and three private hospitals. There are 51 special doctors, 87 general practitioners, 3092 nurses, and 792 midwives in the region. This study utilized an institution-based cross-sectional design. The study was conducted from February-June 2018.
Inclusion and exclusion criteria
Women who gave birth in selected hospitals of the Tigray region and who were present during the data collection period were included in the study. Babies with visible congenital anomalies and unknown gestational age were excluded from the study.
Study participants
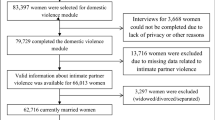
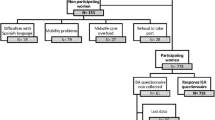
Participants were postpartum women that gave birth in Tigray region healthcare institutions, together with their newborn babies. The sample size was calculated based on a previous study. A study from Ethiopia reported the rate of intimate partner violence during pregnancy to be 25.8%14. Based on this figure, together with a 95% confidence interval, a 5% margin of error, a design effect of 2, and an expected non-response rate of 10%, the required sample size was calculated to be 648. Within the Tigray area, there are 41 hospitals that provide a delivery service, comprising 1 specialized hospital, 15 general hospitals, 22 primary hospitals, and 3 private hospitals. Healthcare facilities were stratified into private and public hospitals, and 1 private hospital and 8 public hospitals were selected using a simple random sampling technique. Participants from each selected healthcare facility were selected using systematic sampling, whereby every third postpartum woman would be included in the sample until the required sample size has been reached. If the selected woman was not eligible to be a participant, the next woman would be considered. The required number of facilities and rate of recruitment was estimated by considering the average numbers of clients expected to deliver daily during the data collection period, i.e., the previous daily client flow of each unit was obtained by referring to the client registration book/record for a month prior to data collection. It was estimated that three months' recruitment at the average client load as measured proceeding the data collection period would be sufficient, and this was used to allocate the sample size proportionally to each of the selected healthcare facilities.
Data collection tool
A structured questionnaire was prepared in English by reviewing the published literature. The English questionnaire was translated to Tigrigna (local language) by a language expert and back translated to English to maintain internal consistency. Data collection was conducted through interviewer-administered techniques. To ensure the validity of the questionnaire expert review was made.
Outcomes of interest for this analysis pertained directly to neonatal outcomes, which were obtained by a chart review within 48 h of delivery. Birth weight (g) and gestational age (weeks) were taken directly from the chart.
Operational definition
Low birth weight was assigned if the neonate weighed < 2500 g, and preterm birth was assigned if the neonate was born at < 37 completed weeks of gestation. Gestational age was determined by the date of the last normal menstrual period and by early ultrasound. Ultrasound performed in the first trimester is considered to provide a more reliable estimate, i.e., plus or minus one week, and mothers who did not know the date of their last menstrual period and had no reliable early ultrasound were excluded from the study15. Newborn babies were weighed on a beam balance with a 30 g accuracy within 6 h of delivery.
Maternal exposure to IPV was determined through the question: ‘‘when you were pregnant for this child did your current partner or boyfriend do any of the following things to you?” With a list of potential offences as follows:
-
Physical violence: slapped, pushed or shoved, hit with fist or something else that could hurt, beaten abdomen, choked or burnt on purpose, used or threatened to use a knife, gun or another weapon.
-
Emotional violence: insulted, humiliated, intimidated on purpose, threatened.
-
Sexual violence: forced into sexual intercourse when you did not want it, had sexual intercourse when you did not want to because of being afraid of what the partner might do, forced to do something sexual that could be found degrading or humiliating.
If the pregnant women had experienced one or more of the above forms of violence during their current pregnancy, they were considered as having been exposed to IPV during pregnancy15.
Analysis
Double data entry was conducted using EPI Info 2008. Data were exported to SPSS version 20 for analysis. A bivariate logistic regression was conducted to identify covariates with associations that were significant to a level of p ≤ 0.2. Variables meeting the criterion of p ≤ 0.2 were taken forward to the multiple logistic regression stage. Odds ratios, 95% confidence intervals and p-values were computed to identify the factors associated and to determine the strength of the association. Significance at a level of p < 0.05 was considered statistically significant for the final model.
Ethical considerations
Ethical approval was obtained from Mekelle University; College of Health Science health research ethics review committee (ethical approval number ERC 1364/2018). Next, an official letter was submitted to the Tigray Regional Health bureau and to each healthcare facility, and permission was obtained from the regional health bureau and each participating healthcare facility. Written informed consent was obtained from each study participant prior to data collection. Each participant was informed about the objectives of the study and that the study findings would contribute necessary information for policymakers and other concerned bodies. Participants were also informed that all data obtained from them would be kept confidential and all data were collected in a private area. Study participants were also informed of their full right to refuse, or withdraw from, any part or all of the study.
Ethics approval and consent
Ethical clearance was secured from Mekelle University Institutional Review Board (IRB). The study participants provided written informed consent to participate in the study after receiving information about the purpose of the study, risks and benefits, and their rights.
Ethics declarations
The study was conducted in accordance to relevant guidelines and regulations.
Results
Socio-demographic characteristics
Six hundred and forty seven participants were enrolled with a response rate of 99.8%. Out of the total participants, 458 (70.78%) of them were urban residents. A majority of the participants 530 (81.9%), were aged between 20 and 35 years although a few were younger. Most participants (N = 610; 94.28%) were married. Nearly half the participants were housewives (N = 301; 46.5%) (Table 1).
Obstetrics characteristics of the participants
Of the 647 women, 155 (24%) were delivered via cesarean section. Around one fourth (162; 25%) of the women had premature rapture of membranes (PROM), 66 (10.2%) women had hypertension during their pregnancy, and 35 (5.4%) women had antepartum hemorrhage (APH). Of all women delivered in the study hospitals, 611 (94.4%) had ante natal care (ANC) follow-up for their last baby. Forty-two (6.5%) women reported the pregnancy as being unwanted. Seventy (10.8%) women delivered before term and 120 (18.5) babies were of low birth weight. The number of stillbirths in this study was 23 (3.6%). From the total neonates delivered, 82 (12.7%) had a low APGAR (Appearance, Pulse, Grimace response, Activity, and Respiration) score (less than 7) (Table 2).
Habits of women
Of the sample, 288 (44.5%) women, had consumed alcohol sometimes during their pregnancy, 10 (1.6%) had chewed chat, and three (0.5%) women smoked.
Regarding the habits of the father of the baby, 19 (2.9%) had drunk alcohol throughout the pregnancy and 362 (56%) had drunk sometimes. 31 (4.8%) men chat chewed sometimes, 4 (0.6%) had chewed throughout. Concerning smoking, 22 (3.4%) men smoked sometimes and 3 (0.5%) men had smoked throughout.
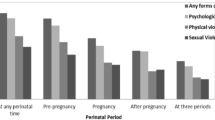
Types of intimate partner violence
Of the total study participants 47 (7.3%) had experienced intimate partner violence during their pregnancy. Of these forty-seven who had experienced intimated partner violence, 22 (46.8%) had experienced physical violence, 8 (17%) psychological violence, and 39 (60%) sexual violence.
Factors associated with low birth weight and preterm birth
Factors exhibiting associations with preterm birth (p ≤ 0.2) in the bivariate regression were hypertension, area of residence, APH, PROM, and ANC follow-up. These factors were exported to the multivariate regression. In the multivariate regression, APH, PROM, and ANC follow-up had significant associations (p < 0.05).
Factors exhibiting associations (p ≤ 0.2) in the bivariate regression with low birth weight were whether the pregnancy was wanted, ANC follow-up, and IPV during pregnancy, and these factors were exported to the multivariate regression. In the multivariate regression, only IPV during pregnancy was significantly associated with low birth weight (p ≤ 0.05).
Women who had had experienced intimate partner violence during pregnancy had 2.39 (95% CI: 1.26–4.55) times the risk of delivering a low-birth-weight baby compared to women who had not experienced violence. Women who had no ANC follow-up, APH, or PROM were significantly more likely to have a preterm birth. Women who had no ANC follow up had 3.9 (95% CI: 1.8–8.6) times the risk of preterm birth compared to their counterparts. Similarly, women who had PROM had 1.86 (95% CI: 1.09–3.18) times the risk of preterm birth, and women who had APH had 2.6 (95% CI: 1.1–6.1) times the risk of preterm birth compared to women who had no APH (Table 3).
Discussion
This study aimed to determine whether intimate partner violence during pregnancy was associated with preterm birth and low birth weight. Intimate partner violence during pregnancy was not found to be significantly associated with preterm birth, but there was a significant association with low birth weight.
The prevalence of intimate partner violence during pregnancy was 7.3%. The findings of this study are supported by the findings of a previous data analysis conducted across 19 countries, that reported the prevalence of intimate partner violence to range from 4 to 13.5%16. The present study reports a higher prevalence than that of a study (3.7%) conducted in New York City17. The difference may be attributable to New York having a better level of gender equality than that present in Ethiopia. It has been reported that if there is gender equality, intimate partner violence will be less. However, the prevalence of intimate partner violence reported in the present study is lower than that reported in Tanzania (30%), Vietnam (32.5%), and Ethiopia Hosanna (23%)11,12,13. This might due to recent measures taken by the Ethiopia government in their second Growth and Transformational Plan, that prioritized ending violence against women4. The disparities between the present study and those conducted in Vietnam and Tanzania are likely due to differences in the study methodologies used in Tanzania and Vietnam, as the present study used a cohort study design.
In this study, the prevalence of preterm birth was 10.8% and the prevalence of low birth weight was 18.5%. A study from Kenya reported a higher rate of preterm birth (18.3%) compared to this study18. Conversely, a study conducted in Vietnam reported a 6.2% prevalence of preterm birth and a 4.9% prevalence of low birth weight11. A study conducted in Baltimore, Maryland, reported a prevalence of low birth weight of 21%19. These variations could be due to the prevalence of preterm birth and low birth weight varying with different environments, healthcare systems, and advice given during pregnancy, all of which are likely to be associated with increased or decreased risk of preterm birth and low birth weight.
This study found that IPV during pregnancy had a significant association with low birth weight. This finding is in line with a study conducted in Vietnam, which reported that experiencing physical violence was associated with an increased the risk of low birth weight11. Similarly, in a study from Tanzania, women exposed to physical violence were found to be three times more likely to give birth to a baby with low birth weight12. A further study conducted in low income women has shown IPV during pregnancy to be associated with a four-fold increase in low birth weights10.
These findings also agree with a study conducted in Ethiopia, where the findings indicated that women experiencing IPV during pregnancy had an increased risk of low birth weight13,14.
Multiple studies have demonstrated IPV to have a significant association with low birth weight. This may be due to the effect of IPV on the woman having both physical and mental components, and as such, low birth weights can occur either by direct or indirect mechanisms.
In this study, IPV had no association with preterm birth. However, women who had no ANC follow up, PROM, or APH did have a significantly higher risk of preterm birth. Similar findings have shown that women without ANC follow up have four times the risk of preterm birth as compared to their counterparts20. Research conducted in Tanzania has shown that women who lacked ANC follow up had five times the risk factor for delivering prematurely21. This finding may be related to ANC including valuable counseling, covering health education about nutrition and disease prevention and health promotion. It is likely that receiving this counseling may be contributed to the prevention of preterm birth.
Again, women with PROM have nearly twice the risk of preterm birth. A study conducted in Iran provides further confidence in this result, whereby women who experienced PROM had three times the risk factor for preterm birth22. Similarly, research findings from Kenya reported that women with PROM were at a fivefold risk for preterm birth18. These findings may be associated with a common need for the induction of labor secondary to chorioamnionitis. Microorganisms that cause bacterial vaginitis can simply ascend and cause intrauterine infections. It is assumed that subclinical chorioamnionitis may trigger the release of inflammatory mediators which lead to release of prostaglandins from the uterine decidua that ultimately induce preterm labor.
Finally, APH increased the risk of preterm birth by a factor of nearly three. This finding is supported by research conducted in Iran, whereby women with bleeding during pregnancy had double the risk factor for preterm birth22, and research conducted in Kenya showed that having APH increased the risk of preterm birth four-fold18. The causes for vaginal bleeding during the first half of pregnancy are unknown. However, much of the time, bleeding during the second or third trimester of pregnancy is attributed to placenta previa or placenta abruption. Vaginal bleeding may lead to emergency treatment for the fetus or mother and may in turn induce preterm birth.
Limitation of the study
This study did not assess the frequency of intimate partner violence experienced by each participant, and therefore associations with the frequency and severity of violence could not be addressed.
Conclusion
This study demonstrated that intimate violence during pregnancy is high and that intimate partner violence during pregnancy significantly associated with an increased risk of low birth weight.
Recommendation and policy implication
The federal minster of health should introduce measures to prevent intimate partner violence during pregnancy to reduce adverse birth outcomes.
Intimate partner violence screening should be involved at ANC.
Researchers should conduct a case–control study to see if there is a measurable cause and effect between intimate partner violence during pregnancy and low birth weight / preterm birth.
Data availability
The data supporting the findings of this article can be made available on request.
References
Of, F. & Partner, I. Understanding and addressing violence against women Intimate partner violence 1–12 (Springer, 2022).
World Health Organization, Intimate Partner Violence During Pregnancy, 23 November, (2011).
The World Bank, Gender-Based Violence (Violence Against Women and Girls), September 25, (2019).
Survey, H. Ethiopia (Springer, 2016).
Asia, S. Low Birth Weight Policy Brief 1–8 (Springer, 2012).
Endalamaw, A., Engeda, E. H., Ekubagewargies, D. T. & Belay, G. M. Low birth weight and its associated factors in Ethiopia: A systematic review and meta- analysis. Ital. J. Pediatr. 6, 1–12 (2018).
Messages, H. Executive Summary 1–7 (Springer, 2022).
United Nations Inter-agency Group for Child Mortality Estimation (UN IGME), ‘Levels & Trends in Child Mortality: Report 2018, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’. (United Nations Children’s Fund, New York, 2018).
State, O. R. Journal of Women ™ s health care prevalence of preterm birth and its associated factors among mothers delivered in Jimma University specialized teaching and referral hospital. Jimma Zone 6(1), 1–10 (2017).
Alhusen, J. L. et al. Intimate partner violence during pregnancy and adverse neonatal outcomes in low-income women. J. Women’s Heal. 23(11), 920–926. https://doi.org/10.1089/jwh.2014.4862 (2014).
Hoang, T. N. et al. Association between intimate partner violence during pregnancy and adverse pregnancy outcomes in Vietnam: A prospective cohort study. PLoS One 11, 9 (2016).
Sigalla, G. N. et al. Intimate partner violence during pregnancy and its association with preterm birth and low birth weight in Tanzania: A prospective cohort study. PLoS ONE 12(2), 1–14 (2017).
Laelago, T., Belachew, T. & Tamrat, M. Effect of intimate partner violence on birth outcomes. Afr. Health Sci. 17(3), 681–689 (2017).
Demelash, H., Nigatu, D. & Gashaw, K. A case-control study on intimate partner violence during pregnancy and low birth weight, Southeast Ethiopia. Obstetr. Gynecol. Int. 2015, 152 (2015).
Gebreslasie, K. Preterm birth and associated factors among mothers who gave birth in gondar town health institutions. Hindawi 2016, 5 (2016).
Garcia-moreno, C. Intimate partner violence during pregnancy: Analysis of prevalence data from 19 countries. Reprod. Health Matters 18(36), 158–170 (2010).
Lane, S. D., Koumans, E. H. & Wojtowycs, M. Effects of intimate partner violence on pregnancy trauma and placental abruption. J. Women Health 19(8), 1501–1509 (2010).
Wagura, P. M. Prevalence and factors associated with preterm birth at Kenyatta national hospital. BMC Pregnancy Childbirth 2014, 2–9 (2014).
Alhusen, J. L., Lucea, M. B., Bullock, L. & Sharps, P. Intimate partner violence, substance use, and adverse neonatal outcomes among urban women. J. Pediatr. 163(2), 471–476. https://doi.org/10.1016/j.jpeds.2013.01.036 (2013).
Woday, A., Muluneh, M. D. & Sherif, S. Determinants of preterm birth among mothers who gave birth at public hospitals in theAmhara region, Ethiopia: A case-control study. PLoS ONE 14(11), e0225060. https://doi.org/10.1371/journal.pone.0225060 (2019).
Mahapula, F. A., Kumpuni, K., Mlay, J. P. & Mrema, T. F. Risk factors associated with pre-term birth in Dar es Salaam, Tanzania: A case-control study. Tanzan J. Health Res. 18(1), 1–8 (2016).
Alijahan, R., Hazrati, S., Mirzarahimi, M., Pourfarzi, F. & Hadi, P. A. Prevalence and risk factors associated with preterm birth in Ardabil, Iran. Iran. J. Reprod. Med. 12 (1), 47–56 (2014). http://www.ijrm.ir/index.php/ijrm/article/view/857/649.
Acknowledgements
The authors thank Mekelle University for helping conduct this research.
Author information
Authors and Affiliations
Contributions
All authors were involved in the proposal development. K.Z.G. was the principal investigator for the study and wrote the manuscript. G.G., S.W., D.Z., M.M., A.B. and G.S.D. were co-investigators and participated in data analysis, and writing the manuscript. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gebreslasie, K.Z., Weldemariam, S., Gebre, G. et al. Intimate partner violence during pregnancy and risks of low birth weight and preterm birth in hospitals of Tigray, Northern Ethiopia. Sci Rep 14, 1363 (2024). https://doi.org/10.1038/s41598-024-51569-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-51569-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.