Abstract
We developed the Navigate intervention to improve survival among vulnerable lung cancer patients. In this intervention-only study, we examined feasibility in terms of recruitment, retention, attendance, adherence, and acceptability to specify adjustments to study procedures and intervention components prior to a randomized trial. The Navigate intervention includes nurse navigation, patient-reported outcomes, and physical exercise. Patients ≥ 18 years old, diagnosed with non-small cell lung cancer at any stage, with performance status ≤ 2, eligible for cancer treatment and vulnerable according to a screening instrument were included. The recruitment goal of eligible patients was 40% while the retention goal was 85%. The predefined cut-offs for sufficient attendance and adherence were ≥ 75%. Acceptability was evaluated by semi-structured interviews with participants, nurse navigators, and physiotherapists. Seventeen (56%) out of 30 screened patients were considered vulnerable and eligible for the study, 14 (82%) accepted participation, and 3 (21%) were subsequently excluded due to ineligibility, leaving 11 patients. Four patients dropped out (36%) and four patients died (36%) during follow-up and 3 (27%) were retained. All 11 patients participated in nurse sessions (mean 16, range 1–36) with 88% attendance and dialogue tools being applied in 68% of sessions. Ninety-one percent of patients responded to PROs (mean of 9 PROs, range 1–24) with 76% of the PRO questionnaires used (attendance) and 100% adherence (completion of all questions in PRO questionnaires), and 55% participated in exercise sessions with 58% attendance and 85% adherence. We identified important barriers primarily related to transportation, but overall acceptability was high. The Navigate intervention was feasible with high participation, acceptability and satisfactory adherence. Retention and exercise attendance were low, which resulted in adjustments.
Trial registration: The feasibility study was initiated prior to the multicenter randomized controlled trial registered by ClinicalTrials.gov (number: NCT05053997; date 23/09/2021).
Similar content being viewed by others
Introduction
Social disparities exist both in lung cancer incidence, survival1,2,3 and receipt of first-line guideline-recommended treatment2,4,5. Adverse health behavior such as smoking, high alcohol consumption and limited physical activity, poor physical condition and limited psychosocial resources6,7 may influence both treatment decisions and inhibit the patient’s ability to adhere to treatment. Other contributing factors may include inadequate time in consultations with patients and knowledge of how to communicate with vulnerable patients among healthcare professionals8,9 and lack of resources in the healthcare system10. The social gradient in both patient-near and system-related factors may result in lower levels of emotional support, participatory dialogue, involvement in treatment decisions and treatment information for patients with fewer resources8,9,11,12. No previous interventions have aimed to improve treatment and rehabilitation adherence13,14 among lung cancer patients at risk of non-adherence to treatment and follow-up. We developed the Navigate intervention15 including nurse navigation16,17,18, use of patient-reported outcomes (PROs)19,20,21 and physical exercise22,23 to improve survival for lung cancer patients who are vulnerable in terms of social, behavioral and disease factors.
To ensure high-quality trials, it is of key importance to assess the feasibility of interventions especially when the patient group has not previously been included in clinical trials. While measures of adherence may inform the delivered dose of interventions and the understanding of trial results, acceptability from the perspective of both healthcare professionals and patients may help identify intervention characteristics crucial to adherence24,25. Few previous studies have described feasibility aspects of nurse navigation26, use of PROs20,27,28 and physical exercise23,29,30 among lung cancer patients, and none systematically included patients who were socially, behaviourally, and physically vulnerable. Only one previous randomized controlled trial (RCT) tested a tailored supportive care intervention among 108 inoperable lung cancer patients and reported high adherence (87%)26. However, the intervention was brief with only two consultations. Two feasibility studies of web-based PRO monitoring in unselected patients with lung cancer found high adherence rates (93% and 94%)27,28 and one of these studies reported high acceptability for both patients and healthcare professionals28. Previous feasibility studies of 6–8 weeks exercise interventions among lung cancer patients achieved between 44 and 87% attendance rates for supervised exercise sessions31,32,33,34, while the attendance was low for home-based exercise programs31,32. Two of these studies evaluated aspects of acceptability from the patients’ perspective showing high acceptability of hospital-based exercise programs32,33 and low acceptability for a walking and relaxation program in home-based settings with key barriers being lack of self-discipline and doubts concerning the effects32.
In preparation for the ongoing multicenter RCT, the current study aimed to determine the feasibility and acceptability of the Navigate intervention in order to identify needed adjustments of the intervention components and study procedures including questionnaires and evaluate the expected goals for recruitment, retention, attendance and adherence.
Methods
Design and setting
The study was conducted as an one-armed, intervention-only feasibility study of the Navigate intervention targeting vulnerable lung cancer patients. Recruitment took place between October 2021 and January 2022 at the Department of Clinical Oncology and Palliative Care, Zealand University Hospital, Roskilde and patients were followed until January 2023. The Consolidated Standards of Reporting Trials (CONSORT) statement for feasibility and pilot studies was used35 (Supplementary Table 1). The Ethics Committee, Region Zealand (SJ-884/EMN-2020-37380) and the Data Protection Agency in Region Zealand (REG-080-2021) approved the study, participants provided written informed consent and all methods were performed in accordance with relevant guidelines and regulations.
Eligibility criteria
All patients diagnosed with non-small cell lung cancer at any stage, with an Eastern Cooperative Oncology Group performance score up to two36, above 18 years, eligible for cancer treatment and screened vulnerable according to a screening instrument within 1 week of diagnosis were eligible for the study. The screening instrument was developed through literature review and with feedback from clinical experts and lung cancer patients15 to identify patients, who were vulnerable in terms of social, behavioral and health (both cancer and non-cancer) factors and at risk for not adhering to treatment guidelines and follow-up. Patients were screened vulnerable if they met three or more of the following nine criteria: (1) stage IIIB-IV (diagnosed with large tumours that have spread to nearby lymph nodes or other areas of the body), (2) comorbidity (somatic disease, e.g. heart disease or mental disease, e.g. depression) with impact on treatment or comorbidity resulting in hospitalization within last three years, (3) above 80 years, (4) performance status of two (and not above two as this is an exclusion criterion), as well as self-reported measures of (5) difficulties in activities of daily living, (6) low social support from social network, (7) low health literacy, (8) transportation-related barriers for treatment or (9) alcohol abuse. Patients were excluded if they were not able to read and understand Danish or had a severe untreated psychiatric disorder or cognitive problems preventing them from giving informed consent.
Intervention program
The development and content of the Navigate intervention have previously been described in detail15. Briefly, the one-year intervention included three components: nurse navigation based on Motivational Interviewing (MI)37, use of PROs and physical exercise.
The manualized nurse navigation sessions were structured with the aim to (1) optimize symptom management, (2) increase treatment initiation and adherence and (3) support patients in health behavior changes and psychosocial needs. Face-to-face or telephone (by patient’s preference) nurse sessions were offered by the following intervals: weekly during the exercise program, bi-weekly while still receiving treatment and monthly after end of treatment.
The aim of systematically collecting PROs was to initiate timely medical treatment or self-management strategies to lower the symptom burden, increase health-related quality of life and treatment adherence. PRO screening for symptoms was monitored bi-weekly throughout the one-year intervention either electronically or through telephone interviews with the nurse-navigator, as per patients’ preference. Patients reported on twelve physical symptoms adapted from the European Organization for Research and Treatment of Cancer (EORTC)21,38. The nurse-navigator followed pre-defined recommended actions according to each elevated symptom, e.g., appointment with an oncologist or self-management strategies.
The manualized exercise program aimed to prevent a decline in physical function and enhance the level of physical activity to improve eligibility for cancer treatment and treatment adherence. The program included 24 exercise sessions (twice weekly) supervised by physiotherapists over the first three months of the intervention targeting cardiorespiratory fitness (15 min of aerobic exercise such as walking or cycling with intensity level 14–15 on the BORG scale) as well as muscle strength and endurance including 25 min of pull-to-chest, sit-to-stand, shoulder press and abdominal crunch with three sets of 15 repetitions in a sitting position with elastic bands in different strengths. Tailoring was possible through manualized criteria for the progression or regression of the intensity level. The first eight exercise sessions were supervised at the hospital to ensure participants could perform the program at home if needed. Any home-based sessions were supported by an online video-based exercise guide available at the study’s webpage and the physiotherapists guided patients by telephone if they needed help with the web browser or any of the exercises. Patients were instructed to fill out an exercise diary to support and document their training at home and to monitor any minor or severe adverse advents occurring in connection with the exercises: ‘Did you feel any discomfort or changed the exercise?’. Physiotherapists were instructed to follow up on the patient’s diary each week to document the exercises or any adverse events occurring in connection with the exercise program in Redcap.
Data collecting by questionnaires and physical testing
Patients filled in questionnaires (demographics (baseline only), health-related quality of life (The European Organisation for Research and Treatment of Cancer Quality-of-life Questionnaire Core 30, Quality-of-life Questionnaire Lung Cancer 13 and European Quality of life Questionnaire-5 Dimensions-5 Levels), health behaviour (alcohol, smoking and physical activity measured by single-item questions), self-activation/self-efficacy (single items from Patient Activation Measure and Health Education Impact Questionnaire) and rehabilitation services (measured by a single question) at baseline and after 3, 6 and 12 months either electronically, on paper or via telephone as per the patients’ preference. Students in medical sciences were trained to perform the questionnaire interview by telephone and probe to support patients through the questions.
To assess and motivate physical activity, patients were monitored with pedometers over 7 days handed out at the baseline physical tests including a prepaid envelope to return the pedometer after 7 days.
Physical fitness was evaluated at baseline, at the end of the exercise program and at 12 months follow-up. Cardiorespiratory fitness was assessed using the Ekblom-Bak test39, endurance and walking ability were assessed using the six-minute walk test (6MWT)40, muscular strength using the 30-s chair stand test41 as well as using a handgrip dynamometer (Jamar) test42. The Ekblom-Bak test was conducted on a cycle ergometer where patients were instructed to pedal at a low work rate of 0.5 kiloponds with a pedal frequency of 60 revolutions per minute (RPM) during the first 4 min followed by 4 min on a higher individually chosen work rate corresponding to 14 on the BORG scale43. The 6MWT was performed in a 20-m undisturbed hallway while the 30-s chair stand test was performed with the patient seated on a 44–47 cm highchair having a straight back, feet approximately shoulder-width apart and placed on the floor with arms crossed over the chest. The patients were encouraged to complete as many full stands as possible within a 30-s time limit. The handgrip test was performed with three measurements on each hand using the best test result from each hand. The physiotherapists were trained to perform the testing procedure.
Feasibility evaluation
Feasibility was examined in terms of recruitment, retention, attendance and adherence to evaluate the expected goals for the ongoing multicenter RCT, while acceptance was evaluated among patients, nurses and physiotherapists to examine whether study procedures or intervention components required any adjustments.
Recruitment and retention
Based on previous trials among lung cancer patients23,26, the expected recruitment goal was 40% while the retention goal at 12 months follow-up was 85%. We evaluated the recruitment goal as the number of patients agreeing to participate in the Navigate pilot study out of all eligible and approached patients. The retention goal was evaluated as the number of patients alive and remaining in the study at 12 months follow-up out of the number of patients recruited into the study.
Attendance and adherence
The predefined cut-offs for sufficient attendance and adherence were ≥ 75%. We calculated attendance for each intervention component according to the individual patient’s follow-up time, e.g., the number of exercise sessions divided by the number of possible sessions until dropout. Adherence to the nurse manual was calculated as the number of nurse sessions using manual dialogue tools out of the total number of nurse sessions. We calculated adherence to PRO questionnaires as the average number of questions completed by the participants out of the total number of 14 questions in the PRO questionnaires. Finally, adherence to the exercise program was calculated as the average minutes of aerobic exercises out of the total of 15 min of exercise and average repetitions per set of strength exercises out of the total of 15 repetitions, as well as the average intensity out of the prescribed amount (15 on the BORG scale and 6 on the OMNI scale).
Acceptability
We evaluated acceptability by semi-structured face-to-face interviews with participants after 3 months and with nurse navigators and physiotherapists after 12 months applying seven constructs of the Theoretical Framework of Acceptability (TFA)25. Interviews were transcribed verbatim and data extraction and condensation were done including familiarization with the interview, using deductive coding and summarizing data according to the seven constructs of TFA25,44. Moreover, patient-reported acceptability on a Likert scale (single items) was obtained after 12 months from questionnaires. We defined high satisfaction with the intervention as a minimum of 75% of patients rating each intervention component as either very relevant or relevant and highly beneficial for them.
Feasibility of study procedures
We evaluated the feasibility of self-reported questionnaires (electronic, paper or telephone) at baseline and after 3, 6 and 12 months through patient interviews. The feasibility of the physical tests was evaluated at baseline in terms of acceptance and adherence by feedback from the physiotherapists.
Statistics
As this is a feasibility study, a sample size calculation was not performed. We had originally planned to include 20 participants, but this was revised to 15 participants as this was expected to be sufficient to reach information saturation regarding feasibility aspects for the ongoing RCT45. Descriptive statistics was performed to estimate the frequencies, means and SD of the baseline patient, clinical and treatment characteristics. We estimated the rates of recruitment, retention, attendance and adherence in numbers and percentages.
Ethics statement
Ethics Committee, Region Zealand (SJ-884/EMN-2020-37380) and the Data Protection Agency in Region Zealand (REG-080-2021) approved the feasibility study. Participants provided written informed consent.
Results
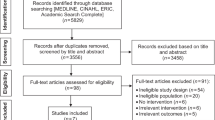
From October 2021 to January 2022, we screened 30 lung cancer patients for vulnerability with 56% (N = 17) considered vulnerable and eligible for the study. Out of the 17 eligible patients, 14 patients (82%) agreed to participate (Fig. 1) with the last follow-up in January 2023. Three patients were subsequently excluded due to ineligibility (too cognitively impaired to participate or rapid disease progression resulting in a performance status of 3) and did not receive the intervention leaving 11 patients in total (7 males and 4 females; mean age 73 years, SD 6). Baseline characteristics for the 11 patients are shown in Table 1. Most patients were screened as vulnerable due to an advanced disease stage (Table 2). Moreover, approximately one-third reported having no help with practicalities at home and difficulties filling in forms or reaching the hospital due to lack of transportation or long travel distance (Table 2). Four patients dropped out (36%) and four patients died (36%) during follow-up and retention at 12 months was 27% (3 out of 11 patients). The primary reasons for dropout were no energy or being too sick to participate. In general, the patients were satisfied with the intervention describing positive attitudes regarding each intervention component (Table 3) and considered nurse sessions and the exercise program as relevant (100% and 68%, respectively) and the intervention as highly beneficial for them (68%).
Nurse sessions
All 11 patients participated in nurse sessions (mean 16 sessions, range 1–36) with an attendance rate of 88% (Table 4). Most sessions were by telephone (87%) primarily due to transportation barriers. Nurse navigators used dialogue tools from the manual in 68% of the nurse sessions (Table 4). The most frequently used dialogue tool was asking the patients what is most important for them and setting an agenda as well as a dialogue tool to support patients in talking about difficult issues related to their disease. Nurse sessions lasted approximately 1 h (range 15–75 min). In total, nurses made 24 referrals, primarily to oncologists, social workers or psychologists. Patients experienced trust and acceptance from the nurse, which made them share difficult things in their life (Table 3). The nurses also expressed positive attitudes towards the intervention, e.g., that their support was highly beneficial, especially among the most vulnerable patients, but also challenges related to the work conditions, professional skills and the extensive intervention manual (Table 3). Supervision meetings were essential to support nurses in their new role as nurse navigators and enabled them to develop their MI skills.
PRO questionnaires
Ninety-one percent of patients (10 out of 11 patients) responded to the PRO questionnaires (mean of 9 PROs, range 1–24) with 106 out of 139 possible PRO questionnaires used until dropout due to death or withdrawal (76% attendance) (Table 4). All PRO questions in the 106 questionnaires were completed (100% adherence) by telephone and dyspnoea and fatigue were the most reported symptoms. Responding to the PRO questionnaire provided patients with knowledge on their disease, the nurse’s guidance enabled patients to better cope with their symptoms, and patients only had difficulties in relating to one question concerning whether they were depressed (Table 3). Nurses made six referrals to an oncologist and three acute referrals as a result of reported symptoms in PROs.
Exercise program
Fifty-five percent of patients (6 out of 11 patients) participated in the exercise program (mean 5 sessions, range 4–24) and five did not participate due to early dropout (N = 3) or treatment complications resulting in severely impaired physical function (N = 2). The six patients attended 70 exercise sessions (58%) out of 120 maximum possible exercise sessions until drop-out due to death or withdrawal (Table 4). As patients had transportation barriers, the majority performed the exercise sessions at home (78%). The primary reasons for non-attendance were treatment-related fatigue or other burdensome symptoms. Adherence to the prescribed aerobic and strength exercises and intensity level among the six patients who participated in the exercise program was good (85–100%) (Table 4). The primary reasons for non-adherence were exhaustion. No severe adverse events during exercise sessions were reported, but minor issues related to muscle soreness (n = 4 patients) and lactic acid in legs (n = 1 patient) did occur. Overall, physiotherapists and patients reported high acceptability of the exercise program and found the volume of time, intensity and type of exercise well-suited. The bodily experience of successfully performing physical exercise was linked to an enhancement in the patient’s self-efficacy (Table 3).
Feasibility of study procedures
Patients found several physical assessments and study procedures challenging. Firstly, the use of pedometers to assess and motivate physical activity over 7 days was too demanding, as patients either forgot to use them or did not return them. Secondly, none of the patients were able to complete the Ekblom-Bak test at baseline, primarily due to poor physical condition and severe dyspnoea. Finally, most patients were not able to attend the baseline physical tests primarily due to transportation barriers prolonging the inclusion of patients up to 1.5 months from the day of recruitment. Conversely, the possibility for patients to select a questionnaire format (electronic, paper version, or telephone-based) that matched their preference reduced the patient burden.
Discussion
This feasibility study of the first intervention targeting vulnerable patients with lung cancer illustrated a high participation rate, adherence, acceptability, and thus relevance of the intervention. However, several intervention components and study procedures required tailoring. Moreover, since retention was low (27%) and only approximately half of the participants attended the exercise program these goals needed adjustment for the ongoing multicentre RCT.
The high inclusion rate of 82% was expected due to the intervention-only study design. However, 21% were subsequently judged ineligible primarily because of rapid disease progression to a terminal phase, which resulted in a discussion of more careful procedures for evaluating eligibility. Moreover, as also recognised in previous studies once recruited into the study, retaining this vulnerable patient group in the intervention was a challenge as they had limited mental and physical resources, e.g. due to treatment complication-related hospital admissions46. Our ongoing RCT should expect lower recruitment rates due to the randomized study design, exclusions due to ineligibility and low retention rates for this vulnerable patient group. It is important to note that the proportion of low retention due to death (36%) will not limit analyses of the primary outcome of survival, but the analyses of the secondary outcomes. To evaluate potential consequences of low recruitment and retention rates for the statistical power and to potentially adapt sample size, we plan to conduct interim analyses 2 years after start of inclusion.
Nurse sessions
Patients had high nurse session attendance (88%) and due to transportation barriers, in-person meetings were scheduled adjacent to planned hospital appointments and the manual requirement that the first nurse session should be in-person was dropped. The frequency of nurse sessions was quite extensive compared with a previous RCT among 108 inoperable lung cancer patients testing a tailored supportive care intervention with only two consultations26. Nevertheless, the attendance rate in our study (88%) was comparable with the brief intervention (87%)26 indicating that the nurse navigator support was acceptable for both patients and nurses. However, nurses also identified burdens related to the work conditions, professional skills and the extensive intervention manual. Organizational support at each participating site will be enhanced through continuous engagement of leaders during meetings and project presentations. Moreover, supervision concerning the use of MI techniques and support in manual use and study procedures will be continued throughout the RCT study period.
PRO questionnaires
In agreement with our study, high adherence rates (93% and 94%) have been reported previously in studies of web-based PRO monitoring among patients with lung cancer27,28 as well as high acceptability for both patients and health care professionals28. Overall, the PRO questionnaire gave patients more disease insight and the nurses’ guidance enabled patients to manage their symptoms. As some patients had difficulties in relating to one question concerning whether they were depressed, this was replaced by a question concerning distress.
Exercise program
Consistent with our findings, two RCTs of exercise interventions similar in frequency and timing (twice weekly sessions for 8–12 weeks), but with higher intensity levels have reported low attendance rates of 44% and drop-out rates of 32%–37%23,34. To provide the highest flexibility also for future implementation, we will allow patients in the RCT to decline participation in the exercise intervention component without being excluded from the study, even though this may dilute the intervention effect.
Previous studies have shown that lung cancer patients can adhere to the prescribed volume of exercise47,48, which is in line with our findings. Therefore, the adherence goal of 75% for the RCT seems realistic for patients attending the exercise program. The high acceptability of the exercise program in our study corroborates previous findings perhaps due to experiencing the effects of exercise in combination with support from a healthcare professional has positive effects on lung cancer patients’ attitudes towards exercise32,49,50,51. In line with our findings, transportation to the exercise facility has previously been identified as the most burdensome aspect of participating in supervised physical exercise51. Therefore, we will reduce the requirement of at least eight supervised sessions at the hospital to a minimum of one supervised session. We will address previous findings of low attendance in home-based exercise programs31,32 by a weekly follow-up on exercise sessions by the nurse navigator to reinforce motivation and thus attendance. This method provided positive results for some patients (Table 4).
Planned analyses in the RCT
In addition to intention-to-treat (ITT) analyses in the RCT, we will also perform per protocol analyses exploring the potential full effect of the intervention by including only participants who meet the definition for sufficient attendance and adherence. Sufficient attendance will be defined as participating in 75% of PRO questionnaires (20 out of 26) and exercise sessions (18 out of 24) according to the manual. As nurse sessions are offered on a need basis, we are unable to define a sufficient proportion of sessions. Sufficient adherence will be defined as completing 75% of each intervention component according to the manual: (1) use of dialogue tools during nurse sessions, (2) all PRO questions in a minimum of 20 questionnaires and (3) aerobic and muscle strength exercises during minimum 18 sessions (aerobic exercise: time and intensity, muscle strength exercises: repetitions and intensity). This was the case for one-third of the participants in the feasibility study. In addition, since retention was low, we will perform an interim analysis in March 2024 to determine a sufficient sample size to evaluate survival in the RCT considering low retention rates.
Feasibility of study procedures
Consistent with previous studies conducted on supportive care interventions for lung cancer patients46, we identified several research procedures that were challenging for the participants to comply with and that prompted changes for the RCT. Pedometers will not be used to assess and motivate physical activity and the Ekblom-Bak test will not be used to assess cardiorespiratory fitness. To reduce the inclusion duration, we will increase flexibility by allowing the baseline physical assessment to be performed after randomization to shorten the enrolment period. The impact of knowledge of group allocation on patients’ performance during the baseline physical test is expected to be minimal. To ensure that baseline odds of survival are the same for both groups in the RCT, patients will fill out questionnaires at baseline before randomization as soon as possible and within 1.5 months after being invited into the study15. With transportation as a key barrier, we will cover the costs related to transportation to the hospital.
The strength of this study was the exploration of both feasibility goals and acceptability of a complex intervention enabling the identification of key aspects to improve expected goals and study procedures for the ongoing RCT. The relatively low number of participating patients was a limitation of this study with key participation barriers being transportation, long distance to the hospital or limited mental or physical resources to comply with the requirements of participating in a research project. Moreover, since retention was low and mortality was high only three patients completed follow-up after 12 months.
Conclusions
We explored the feasibility of the first intervention targeting vulnerable lung cancer patients. The results illustrate a high participation rate and high acceptability and thus the relevance of the intervention, but low retention, exercise attendance and barriers were identified leading to an adjustment of study procedures to meet the complex needs of the study population. The Navigate intervention is currently being evaluated in a multicenter RCT with recruitment start March 1st, 2022.
Data availability
Due to the EU regulation, the General Data Policy Regulation, we cannot share data with external parties without prior consent of the participants. Collaboration projects will however be possible by contacting Co-PI Pernille Bidstrup: pernille@cancer.dk.
References
Dalton, S. O., Steding-Jessen, M., Engholm, G., Schuz, J. & Olsen, J. H. Social inequality and incidence of and survival from lung cancer in a population-based study in Denmark, 1994–2003. Eur. J. Cancer 44(14), 1989–1995 (2008).
Dalton, S. O. et al. Socioeconomic position and survival after lung cancer: Influence of stage, treatment and comorbidity among Danish patients with lung cancer diagnosed in 2004–2010. Acta oncologica 54(5), 797–804 (2015).
Sidorchuk, A. et al. Socioeconomic differences in lung cancer incidence: A systematic review and meta-analysis. Cancer Causes Control 20(4), 459–471 (2009).
Kaergaard Starr, L. et al. Socioeconomic position and surgery for early-stage non-small-cell lung cancer: A population-based study in Denmark. Lung Cancer. 79(3), 262–269 (2013).
Forrest, L. F., Adams, J., Wareham, H., Rubin, G. & White, M. Socioeconomic inequalities in lung cancer treatment: Systematic review and meta-analysis. PLoS Med. 10(2), e1001376 (2013).
Diderichsen, F. et al. Health inequality–determinants and policies. Scand. J. Public Health. 40(8 Suppl), 12–105 (2012).
Halgren, M. O., Kjær, T. K. & Dalton, S. O. Hvidbog-Social ulighed i kræft i Danmark. (2019).
Dencker, A., Tjørnhøj-Thomsen, T. & Pedersen, P. V. A qualitative study of mechanisms influencing social inequality in cancer communication. Psycho-oncology. 30(11), 1965–1972 (2021).
Verlinde, E., De Laender, N., De Maesschalck, S., Deveugele, M. & Willems, S. The social gradient in doctor-patient communication. Int. J. Equity Health. 11, 12 (2012).
Johannes, B., Graaf, D., Blatt, B., George, D. & Gonzalo, J. D. A multi-site exploration of barriers faced by vulnerable patient populations: A qualitative analysis exploring the needs of patients for targeted interventions in new models of care delivery. Prim. Health Care Res. Dev. 20, e61 (2018).
Siminoff, L. A., Graham, G. C. & Gordon, N. H. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors. Patient Educ. Counsel. 62(3), 355–360 (2006).
Smith, S. K., Dixon, A., Trevena, L., Nutbeam, D. & McCaffery, K. J. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc. Sci. Med. 69(12), 1805–1812 (2009).
Sampedro Pilegaard, M. et al. Rehabilitation and palliative care for socioeconomically disadvantaged patients with advanced cancer: A scoping review. Acta Oncol. 60(1), 112–123 (2021).
Ruiz-Pérez, I., Rodríguez-Gómez, M., Pastor-Moreno, G., Escribá-Agüir, V. & Petrova, D. Effectiveness of interventions to improve cancer treatment and follow-up care in socially disadvantaged groups. Psycho-oncology. 28(4), 665–674 (2019).
Langballe, R. et al. NAVIGATE: Improving survival in vulnerable patients with lung cancer through nurse navigation, symptom monitoring and exercise—Study protocol for a multicentre randomised controlled trial. BMJ Open. 12(10), e060242 (2022).
Budde, H., Williams, G. A., Winkelmann, J., Pfirter, L. & Maier, C. B. The role of patient navigators in ambulatory care: Overview of systematic reviews. BMC Health Serv. Res. 21(1), 1166 (2021).
Freund, K. M. et al. Impact of patient navigation on timely cancer care: The Patient Navigation Research Program. J. Natl. Cancer Inst. 106(6), dju115 (2014).
Rodday, A. M. et al. Impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 121(22), 4025–4034 (2015).
Kotronoulas, G. et al. What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J. Clin. Oncol. 32(14), 1480–1501 (2014).
Basch, E. et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J. Clin. Oncol. 34(6), 557–565 (2016).
Denis, F. et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J. Natl. Cancer Inst. https://doi.org/10.1093/jnci/djx029 (2017).
Peddle-McIntyre, C. J. et al. Exercise training for advanced lung cancer. Cochrane Database Syst. Rev. 2, CD012685 (2019).
Quist, M. et al. Effects of an exercise intervention for patients with advanced inoperable lung cancer undergoing chemotherapy: A randomized clinical trial. Lung Cancer. 145, 76–82 (2020).
Sekhon, M., Cartwright, M. & Francis, J. J. Development of a theory-informed questionnaire to assess the acceptability of healthcare interventions. BMC Health Serv. Res. 22(1), 279 (2022).
Sekhon, M., Cartwright, M. & Francis, J. J. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 17(1), 88 (2017).
Schofield, P. et al. A tailored, supportive care intervention using systematic assessment designed for people with inoperable lung cancer: A randomised controlled trial. Psycho-oncology. 22(11), 2445–2453 (2013).
Denis, F. et al. Detection of lung cancer relapse using self-reported symptoms transmitted via an internet web-application: Pilot study of the sentinel follow-up. Support. Care Cancer 22(6), 1467–1473 (2014).
Friis, R. B., Hjollund, N. H., Mejdahl, C. T., Pappot, H. & Skuladottir, H. Electronic symptom monitoring in patients with metastatic lung cancer: A feasibility study. BMJ Open. 10(6), e035673 (2020).
Dhillon, H. M. et al. Impact of physical activity on fatigue and quality of life in people with advanced lung cancer: A randomized controlled trial. Ann. Oncol. 28(8), 1889–1897 (2017).
Chen, H. M., Tsai, C. M., Wu, Y. C., Lin, K. C. & Lin, C. C. Randomised controlled trial on the effectiveness of home-based walking exercise on anxiety, depression and cancer-related symptoms in patients with lung cancer. Br. J. Cancer. 112(3), 438–445 (2015).
Quist, M. et al. Safety and feasibility of a combined exercise intervention for inoperable lung cancer patients undergoing chemotherapy: A pilot study. Lung Cancer. 75(2), 203–208 (2012).
Adamsen, L., Stage, M., Laursen, J., Rørth, M. & Quist, M. Exercise and relaxation intervention for patients with advanced lung cancer: A qualitative feasibility study. Scand. J. Med. Sci. Sports. 22(6), 804–815 (2012).
Peddle-McIntyre, C. J., Bell, G., Fenton, D., McCargar, L. & Courneya, K. S. Feasibility and preliminary efficacy of progressive resistance exercise training in lung cancer survivors. Lung Cancer. 75(1), 126–132 (2012).
Temel, J. S. et al. A structured exercise program for patients with advanced non-small cell lung cancer. J. Thorac. Oncol. 4(5), 595–601 (2009).
Eldridge, S. M. et al. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 355, i5239 (2016).
Oken, M. M. et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 5(6), 649–655 (1982).
Spencer, J. C. & Wheeler, S. B. A systematic review of motivational interviewing interventions in cancer patients and survivors. Patient Educ. Counsel. 99(7), 1099–1105 (2016).
Basch, E. et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J. Clin. Oncol. 34, 557–565 (2016).
Ekblom-Bak, E., Bjorkman, F., Hellenius, M. L. & Ekblom, B. A new submaximal cycle ergometer test for prediction of VO2max. Scand. J. Med. Sci. Sports. 24(2), 319–326 (2014).
Troosters, T., Gosselink, R. & Decramer, M. Six minute walking distance in healthy elderly subjects. Eur. Respir. J. 14(2), 270–274 (1999).
Jones, C. J., Rikli, R. E. & Beam, W. C. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res. Q. Exerc. Sport. 70(2), 113–119 (1999).
Yorke, A. M., Curtis, A. B., Shoemaker, M. & Vangsnes, E. Grip strength values stratified by age, gender, and chronic disease status in adults aged 50 years and older. J. Geriatr. Phys. Ther. 38(3), 115–121 (2015).
Borg, G. A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 14(5), 377–381 (1982).
Gale, N. K., Heath, G., Cameron, E., Rashid, S. & Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 13, 117 (2013).
Julious, S. Sample size of 12 per group rule ofthumb for a pilot study. Pharm. Stat. 4, 287–291 (2005).
Schofield, P. et al. Lung cancer: Challenges and solutions for supportive care intervention research. Palliat. Support. Care. 6, 281–287 (2008).
Edvardsen, E. et al. High-intensity training following lung cancer surgery: A randomised controlled trial. Thorax. 70(3), 244–250 (2015).
Quist, M. et al. The impact of a multidimensional exercise intervention on physical and functional capacity, anxiety, and depression in patients with advanced-stage lung cancer undergoing chemotherapy. Integr. Cancer Ther. 14(4), 341–349 (2015).
Chang, P. H. et al. Exercise experiences in patients with metastatic lung cancer: A qualitative approach. PLoS ONE. 15(4), e0230188 (2020).
Cheville, A. L., Dose, A. M., Basford, J. R. & Rhudy, L. M. Insights into the reluctance of patients with late-stage cancer to adopt exercise as a means to reduce their symptoms and improve their function. J. Pain Symptom Manag. 44(1), 84–94 (2012).
Granger, C. L. et al. Understanding factors influencing physical activity and exercise in lung cancer: A systematic review. Support Care Cancer 25(3), 983–999 (2017).
Acknowledgements
We would like to thank all the participating patients and the dedicated healthcare professionals including nurse navigators Lizette Lykke Mehr and Lene Duus and physiotherapist Katrine Kærgaard Christiansen for their valuable feedback on study procedures and intervention components. Moreover, we would like to thank nurse navigator Lizette Lykke Mehr for conducting interviews with patients who provided valuable feedback on study components and procedures.
Funding
This work is conducted as part of research activities in the Danish Research Center for Equality in Cancer, COMPAS and was supported by The Danish Cancer Society ‘Knæk Cancer’ (grant no. R223-A13094-18-S68), The Novo Nordisk Foundation (grant no. NNF20OC0064570), The Independent Research Fond (grant no. 1030-00414B), Danish Research Center for Lung Cancer, Region Southern Denmark and Region Zealand Research Fond and the Danish Comprehensive Cancer Center. Neither the funders nor the study sponsor had no part in the design of the feasibility study nor the trial and will not have any role in its execution, analyses, interpretation of results, or decision related to reports of the results. The funders did not have any role in this feasibility study or the ongoing trial other than to provide funding.
Author information
Authors and Affiliations
Contributions
P.E.B., S.D., E.J., R.V.K., L.B.J. and S.T.S. and R.L. contributed substantially to the concept and design of the feasibility study. R.L., R.V.K. and P.E.B. developed manuals for recruitment, assessment, and nurse navigation. L.B.J., S.T.S., R.L. and P.E.B. developed manual for the physical tests and exercise program. P.E.B., R.V.K. and RL developed written information for participants. R.L., P.E.B. and S.D. contributed with applications for grants, and approval assignments. P.E.B., R.V.K. and R.L. introduced and supervised the recruitment, assessment, and intervention concepts and procedures to physiotherapists and nurses and headed the data collection. L.P.S. and R.L. conducted interviews with physiotherapists and nurse navigators, respectively. L.P.S. transcribed the interviews and L.P.S. and R.L. performed data extraction and condensation. R.L. and P.E.B. drafted the manuscript. All authors provided intellectual feedback to the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Langballe, R., Svendsen, L., Jakobsen, E. et al. Nurse navigation, symptom monitoring and exercise in vulnerable patients with lung cancer: feasibility of the NAVIGATE intervention. Sci Rep 13, 22744 (2023). https://doi.org/10.1038/s41598-023-50161-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50161-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.