Abstract
Serum 25-hydroxyvitamin D concentrations deficiency is a growing health problem that affects a significant part of the world’s population, with particularly negative consequences in children and older adults. Public health has prioritized healthy aging; thus, an investigation of the social determinants related to deficient and insufficient Serum 25-hydroxyvitamin D concentrations in older adults is needed to contribute to the implementation of comprehensive social programs focused on addressing those conditions adversely affecting the health of this group. This study was conducted using a sample of older adults (age ≥ 65 years, n = 1283) from the National Health Survey (NHS 2016–2017). The Average Marginal Effects of the social determinants of Serum 25-hydroxyvitamin D concentrations deficiency in older adults were predicted using a probit model in which the outcome variable assumed two values (deficiency or not deficiency), taking as independent variables those reported in previous studies. The model showed an adequate goodness of fit, Count R2 = 0.65, and the independent variables explained between 11% (Cox-Snell) and 14% (Nagelkerke) of the variance of the outcome variable. The social determinants associated with a greater likelihood of Serum 25-hydroxyvitamin D concentrations deficiency are the following conditions: women, people of native origin, urban dwellers, shorter sunlight exposure, and greater geographical latitude. Implications are discussed, and limitations are considered. Promotion and prevention programs should preferentially target older adults in the southernmost regions who live in urban areas, with a special focus on women. Due to the country’s characteristics (17°–57° south latitude), it is necessary to review in future research the three zones shown in this study as relevant social determinants for the older adults living in them to generate inputs in formulating public health policies. The authorities must define the cut-off points for considering the difference between the country’s ranges of Serum 25-hydroxyvitamin D concentrations insufficiency and deficiency.
Similar content being viewed by others
Introduction
Serum 25-hydroxyvitamin D [25(OH)D] concentrations belong to the family of fat-soluble vitamins, although it is also proposed as a prohormone1. Its function is intimately related to bone health in children and adults2,3,4; it also participates in cell proliferation and differentiation as well as mental health2. Deficient levels of this vitamin are also associated with an increased risk of cardiovascular pathologies, cancer, diabetes, and autoimmune and infectious diseases, COVID-19, among others5,6,7,8,9,10,11. The main mechanism by which an organism obtains 25(OH)D is through exposure to sunlight, which triggers its synthesis in the skin cells thanks to the absorption of photons from UV rays14. It can also be obtained, although to a lesser extent, through dietary intake4,13,14. Thus, people with 25(OH)D deficiency mainly have less sun exposure and lower intake15. Some factors influencing 25(OH)D concentrations are geographical latitude, season, and ethnicity16.
25(OH)D deficiency is a growing health problem that affects a significant part of the world population16,17,18, with negative consequences in children, ill people, and older people3,15,19,20. As for the last group, the natural aging process is associated with a decrease in 25(OH)D synthesis because seven dehydrocholesterol levels in older skin are reduced21,22, which can be reflected in adverse health outcomes such as sarcopenia, respiratory problems, osteomalacia, bone loss, osteoporotic fractures, and muscle problems2,6,23,24. Along this line, public health has made older adults a priority focus of interest to generate knowledge and promote public policies for healthy aging25. Considering that environmental and personal factors may be involved in older adults’ lower 25(OH)D concentrations, research has begun to study the social determinants of deficient and insufficient 25(OH)D levels in this group20,26,27. Knowing the social conditions underlying people’s negative health results, called “the social causes of disease”28, can contribute to the implementation of social programs focused on addressing those adverse conditions29. Research on older adults has observed a lower concentration of 25(OH)D in women20,26, those who skip breakfast, are more sedentary, have less sun exposure, have darker skin, have disabilities, live alone, and are older20,26,27,30,31,32; especially relevant are factors such as not taking medications or vitamin supplements, smoking, the winter season, and obesity30,32. Likewise, protective factors negatively related to 25(OH)D deficits are intense physical activity, sleeping more than nine hours, and having more schooling and income26,30. On the other hand, living in rural or urban areas yields mixed results; in some cases, there is a greater deficit associated with large cities23, while in others, the result is the opposite30.
More research is also needed from Latin America and middle- and low-income countries18,20,34. In this regard, Chile has unique characteristics. Geographically, it is located between approximately 17° and 57° degrees south latitude, with the driest desert in the world beginning in the north (Atacama Desert) and extending to Patagonia in the south; its longitude is similar to that from southern Algeria to the north of the United Kingdom. It also possesses ethnic and lifestyle diversity and a mixture of public and private health systems that are characteristic of the Latin American reality35. Chilean authorities have consistently called for studies on 25(OH)D conditions in the country due to the paucity of information on specific groups. They also aim to have input to establish clear cut-off points concerning assessing 25(OH)D36. The present work seeks to identify the social determinants related to older adults with deficient 25(OH)D concentrations in Chile. In this context, knowledge of the social determinants can help public policymakers, health professionals, and researchers develop interventions that promote good health outcomes among the Chilean older adult population. This study considers the data provided by the National Health Survey 2016–201737 and weighs a single cut-off point to define the condition of “deficiency,” based on the indications of experts from the Chilean Ministry of Health, who established the cut-off point at 20 ng/mL of 25(OH)D “to make population-based analyses that allow public policy proposals”36. A probit model will be run to determine the average marginal effects of each social determinant reviewed.
Methods
Source of information
The data used in this study are from the third version of the National Health Survey (NHS 2016–2017) commissioned by the Department of Epidemiology of the Chilean Ministry of Health37. Its purpose is to identify the diseases suffered by and treatments provided to men and women aged 15 years and older living in Chile. It is a cross-sectional, randomized, population-based survey stratified by cluster and applied in 15 regions of Chile in both urban and rural areas. The NHS 2016–2017 consists of three sections. The first is a questionnaire with 576 general questions (including a diagnostic interview to measure mental disorders); the second includes anthropometric measurements; and the third corresponds to laboratory tests (including measurement of 25-hydroxyvitamin concentrations). The NHS 2016–2017 database is for public use and was obtained from the Ministry of Health. All population-based surveys are conducted under Law Nº19.628 on protecting citizens' privacy, and consequently, they do not require approval by an Ethics Committee. All participants voluntarily participated. The NHS 2016–2017 is used in research as a secondary data source27. The total population surveyed amounted to 6,233 people. However, for the specific case of 25(OH)D, its measurement was incorporated in only two population subsamples: women of childbearing age (15 to 49 years) and the elderly (65 years and older). In this study, we will only work with the second group, composed of 1,283 older adults representative of the national level.
Outcome variable: 25(OH)D deficiency in adults over 65 years of age
The criterion defining deficiency or not deficiency categories is the cut-off point of 20 ng/mL of 25(OH)D13,38. Thus, the outcome variable is dichotomous and takes the value 1 in the “25(OH)D deficiency” range (below the cut-off point) and the value 0 in the range above the cut-off point (no deficiency).
Independent variables
The independent variables were considered according to previously reviewed literature and were present in NHS 2016–2017. They are sex, belonging or direct descent from native peoples, rural or urban areas, exposure to sunlight, and regions of the country (see Table 1). All independent variables are dichotomous, assuming the value 1 (belongs to the category) or 0 (does not belong). It should be noted that the geographic area taken as a base is the metropolitan region (located approximately between 32 and 34 degrees south latitude).
Plan of analysis
Data statistical analysis was performed with Stata software13. A probabilistic nonlinear model was performed with a dichotomous response (people ≥ 65 years having or not having 25(OH)D deficiency), and a regressor that refers to a probit model. Average marginal effects were calculated for each interaction, and likelihoods were predicted. The model specification is:
where F(.) corresponds to the cumulative distribution function assumed to be probit, which is a link between the determinants and the probability of presenting 25(OH)D deficiency; thus, the probit model to be estimated corresponds to:
Goodness of fit
The model was estimated based on 1,283 observations. The log-likelihood is -800.16, χ2 (18) = 143.24, p < 0.0001. The goodness of fit, Count R2 = 0.65, indicates good explanatory power of the model. The independent variables explain between 11% (Cox-Snell) and 14% (Nagelkerke) of the variance of the outcome variable.
Results
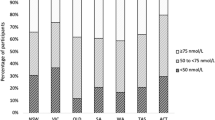
Of the total number of older adults (n = 1,283) included in the present study, 59% had levels below 20.0 ng/mL of 25(OH)D, referred to as deficiency. Of the sample, 64% were women (65% had 25(OH)D deficiency), 68% reported little sunlight exposure, 20% lived in rural areas, and 7% belonged to native peoples. Moreover, 15% of older adults in the sample live in the metropolitan region (which includes the capital of Chile), 34% live in the regions located to the north, and 51% live to the south of the metropolitan region. Out of those with 25(OH)D deficiency, 16% live in the metropolitan region, 31% live in the north, and 53% live in the south of the metropolitan region. When stratified by sex and region of the country, women living in the first three regions of the north have a considerably higher 25(OH)D deficiency than men (61% vs. 25%). However, in the last three regions of the south, deficiency increases in both sexes and is close to each other (77% vs. 75%, women and men, respectively). Also, 60% of people with 25(OH)D deficiency have less than eight years of schooling or no schooling, and 59% have public health insurance (National Health Fund, called FONASA). It should be noted that according to Casen 2017, 44% of older people are within the first two quintiles, with the lowest income. Both schooling and type of health insurance were incorporated as a proxy for income level; however, their relationships with 25(OH)D deficiency were not statistically significant for a 95% confidence interval.
Next, variables with statistical significance within the model will be presented. The demographic results indicate that women are 15% more likely to have 25(OH)D deficiency than men (see Table 2). Older people with low exposure to sunlight are more likely (8%) to have 25(OH)D deficiency than those exposed to more sunlight. Also, those living in rural areas have a lower probability (-24%) of having 25(OH)D deficiency than those living in urban areas. People of native origin are 11% more likely to have 25(OH)D deficiency.
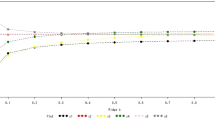
The regions from north to south follow each other from the lowest to greatest latitude (see Fig. 1). Older people living in the northern part of the country (regions 1, 2, and 4 closer to the Equator) are less likely to have 25(OH)D deficiency than those in the metropolitan region. At the same time, people living in the country’s extreme south (regions 13, 14, and 15, closer to Antarctica) are more likely to have 25(OH)D deficiency than people living in the metropolitan region. The other regions of the country show no significant results.
Average Marginal Effects (AMEs) of Older adults 25(OH)D deficiency, by Chilean regions. Note. Regions from north to south follow each other in order: Arica and Parinacota (1); Tarapacá (2); Antofagasta (3); Atacama (4); Coquimbo (5); Valparaíso (6); Metropolitan (7); O’Higgins (8); Maule (9); Biobío (10); Araucanía (11); Los Ríos (12); Los Lagos (13); Aysen (14), and Magallanes (15).
Discussion
Using the NHS 2016–2017, our results on 25(OH)D deficiency in Chilean older adults converge with findings reported in other countries and also render important comparative information, all of which allows us to contribute to understanding this critical issue for public health that has implications for the wellbeing and quality of life of older people in the country and the world.
Regarding demographic variables, it is observed that older women have higher 25(OH)D deficiency, an issue that has been consistently reported in previous studies20,26. However, multiple factors could be related to these sex differences, including, for example, differences in vitamin D intake between men and women, sun exposure, skin synthesis capabilities, age, and being overweight39. Without a definitive answer, differences in synthesis capabilities derived from different skin pigmentation could be ruled out since Chilean women tend to have a lighter skin tone than men40. In addition, men tend to withdraw fewer dietary supplements than women41 that are fortified with vitamin D. Likewise, there is no difference in age by sex in the sample (Males average = 73.8 years vs. Females average = 74.2 years), t(1283) = -1.00, p = 0.31, and men agree the most to be exposed to more sunlight than women (Males average = 1.43 vs. Females average = 1.26), t(851) = 6.35, p < 0.001. However, a factor that might explain this difference is that Chilean women are overweight at higher levels than men42, a condition consistently related to lower 25(OH)D status43,44. In our sample, their body mass index (BMI) ratio is higher than that of men (Males = 0.59 vs. Females = 0.63), t(1058) = -8.05, p < 0.001.
The main mechanism for obtaining 25(OH)D is through exposure to sunlight12. Previous studies have consistently found higher 25(OH)D concentrations in the summer months30,31,32; thus, it is not surprising that in this study, those older adults who reported greater exposure to sunlight had higher 25(OH)D levels.
Latitude is also a predominant factor in 25(OH)D levels due to greater solar exposure closer to the Equator16,32. In our results, older adults from the northernmost regions (Arica and Parinacota, and Tarapacá), located between 17° 30′ and 21° 38′ south latitude, have the lowest likelihood of presenting 25(OH)D deficiency. The metropolitan region, which is taken as a base, does not differ from the regions located from 21° 38′ to 40° 33′ south latitude, while the areas located from that point to 56° 30′ south latitude (Los Lagos, Aysen, and Magallanes) are where older adults deliver the highest probabilities of showing 25(OH)D deficiency. Therefore, 25(OH)D in the country is associated with the geographical location north to south (north closest to the Equator). A comparison of mean 25(OH)D levels among older adults in these three geographic zones yields significant differences among them: Great North Zone (Mean = 22), from Little North to South (Mean = 19), and Austral Zone (Mean = 16), F (2, 1283) = 24.22, ps < 0.01, with insufficiencies of 37.2%, 57.8%, and 74.3%, respectively. In comparative terms, using the same cut-off point, the rates of deficiency move in different ranges in the world, for example, from 21.6% in Ecuador34 and 23.5% in Brazil20 to 62.1% in Korea26 and 67.2% in Portugal30. Thus, using the only cut-off point suggested by the authorities for public health research (20 ng/mL)36, the country presents three differentiated realities that require further study to serve as input for the development of public health policies. For example, considering the Austral zone, there is evidence in Ireland, which has a similar latitude (51º-55º North), that 25(OH)D synthesis in older adults occurs preferentially in the summer months, making it necessary to provide vitamin D through intake during the winter months32.
Older adults living in rural areas are less likely to have 25(OH)D deficiency, a finding that is consistent with some precedents33 but differs from others30. These differences may be due, in part, to the greater pollution in large cities in developing countries46, which impedes adequate 25(OH)D synthesis. It has also been observed that people in rural environments tend to have greater solar exposure than people in cities47. It should be noted that Santos and collaborators30 emphasized that their results are probably due to a confounding variable since the metropolitan area of Lisbon is where more people with higher incomes live, which is a protective factor against 25(OH)D deficiency.
In contrast, Indigenous peoples’ older adults in Latin America have shown lower levels of 25(OH)D compared with the rest of their country’s population34. It is possible that, in the case of Chile, the combination of native people’s darker skin pigmentation40 and a higher proportion of them living in the central and southern regions of the country (i.e., at a higher southern latitude) may contribute to understanding this finding. In addition, Indigenous populations tend to use clothing to protect themselves from the climate, which reduces sun exposure (e.g., shawls and hats). Clothing that covers more of the body has been observed as a factor associated with lower 25(OH)D levels45.
One of the limitations of this work is that the NHS 2016–2017 is the first national survey that addresses the measurement of 25(OH)D levels in some specific groups, so there are no antecedents with which to contrast results. Second, the descriptive variables were taken based on self-reports, and their responses could be biased, such as the time of sun exposure and ethnicity. Third, as indicated, no cut-off point is defined by the Chilean authorities to distinguish between deficient and insufficient levels. The only suggested cut-off point for the categories referred to in this study as “deficiency” and “no deficiency” were used. Also, BMI was not included as an independent variable. Finally, sampling was carried out over several months, passing through different seasons of the year (part of the winter and the entire spring and summer), which could generate some distortion in the measurement.
It is worth noting that this research used information from the Health Surveys for epidemiological surveillance of the Undersecretariat of Public Health. The authors thank the Ministry of Health of Chile for making the database available. All the results obtained from this research are the responsibility of the authors and in no way compromise that institution.
Conclusions
The social determinants related to deficient 25(OH)D concentrations in older adults in Chile are mainly associated with lower sun exposure related to variables such as having an urban residence, living in the southernmost areas of the country, and reporting low exposure to sunlight; consistently, residing in the northern part of the country, closer to the Equator, is a protective factor. Other variables, such as being female and belonging to native peoples, also have a negative effect. Our results suggest three differentiated zones within the country regarding latitude (and, thus, sun exposure), which require further attention and study to contribute as input for generating public health policies.
Data availability
The National Health Survey database is available in MINSAL webpage, http://epi.minsal.cl/encuesta-nacional-de-salud-2015-2016/.
References
Courbebaisse, M. & Cavalier, E. Vitamin D in 2020: An old pro-hormone with potential effects beyond mineral metabolism. Nutrients 12(11), 3378. https://doi.org/10.3390/nu12113378 (2020).
Bouillon, R. et al. Skeletal and extraskeletal actions of vitamin D: Current evidence and outstanding questions. Endocr. Rev. 40(4), 1109–1151. https://doi.org/10.1210/er.2018-00126 (2019).
Chanchlani, R. et al. An overview of rickets in children. Kidney Int. Rep. 5(7), 980–990. https://doi.org/10.1016/j.ekir.2020.03.025 (2020).
Charoenngam, N., Shirvani, A. & Holick, M. F. Vitamin D for skeletal and non-skeletal health: What we should know. J. Clin. Orthop. Trauma. 10(6), 1082–1093. https://doi.org/10.1016/j.jcot.2019.07.004 (2019).
Charoenngam, N. & Holick, M. F. Immunologic effects of vitamin D on human health and disease. Nutrients. 12(7), 2097. https://doi.org/10.3390/nu12072097 (2020).
Hahn, J. et al. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ. 376, e066452. https://doi.org/10.1136/bmj-2021-066452 (2022).
Pittas, A. G. et al. Vitamin D and risk for type 2 diabetes in people with prediabetes: A systematic review and meta-analysis of individual participant data from 3 randomized clinical trials. Ann. Intern. Med. 176(3), 355–363. https://doi.org/10.7326/M22-3018 (2023).
Acharya, P. et al. The Effects of Vitamin D Supplementation and 25-Hydroxyvitamin D Levels on the Risk of Myocardial Infarction and Mortality [published correction appears in J Endocr Soc. 2021 Dec 22;6(1):bvab164]. J. Endocr. Soc. 5(10), 124. https://doi.org/10.1210/jendso/bvab124 (2021).
Mirhosseini, N., Vatanparast, H. & Kimball, S. M. The association between Serum 25(OH)D status and blood pressure in participants of a community-based program taking vitamin D supplements. Nutrients 9(11), 1244. https://doi.org/10.3390/nu9111244 (2017).
Gibbons, J. B. et al. Association between vitamin D supplementation and COVID-19 infection and mortality. Sci. Rep. 12(1), 19397. https://doi.org/10.1038/s41598-022-24053-4 (2022).
Oristrell, J. et al. Vitamin D supplementation and COVID-19 risk: A population-based, cohort study. J. Endocrinol. Invest. 45(1), 167–179. https://doi.org/10.1007/s40618-021-01639-9 (2022).
Heaney, R. P., Davies, K. M., Chen, T. C., Holick, M. F. & Barger-Lux, M. J. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am. J. Clin. Nutr. 77(1), 204–210. https://doi.org/10.1093/ajcn/77.1.204 (2003).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline [published correction appears in J Clin Endocrinol Metab. 2011 Dec;96(12):3908]. J. Clin. Endocrinol. Metab. 96(7), 1911–1930. https://doi.org/10.1210/jc.2011-0385 (2011).
Crowe, F. L. et al. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: Results from the EPIC-Oxford study. Public Health Nutr. 14(2), 340–346. https://doi.org/10.1017/S1368980010002454 (2011).
Armas, L. A., Hollis, B. W. & Heaney, R. P. Vitamin D2 is much less effective than vitamin D3 in humans. J. Clin. Endocrinol. Metab. 89(11), 5387–5391. https://doi.org/10.1210/jc.2004-0360 (2004).
Mendes, M. M. et al. Impact of high latitude, urban living and ethnicity on 25-hydroxyvitamin D status: A need for multidisciplinary action?. J. Steroid Biochem. Mol. Biol. 188, 95–102. https://doi.org/10.1016/j.jsbmb.2018.12.012 (2019).
Kimball, S. M. & Holick, M. F. Official recommendations for vitamin D through the life stages in developed countries. Eur. J. Clin. Nutr. 74(11), 1514–1518. https://doi.org/10.1038/s41430-020-00706-3 (2020).
Palacios, C. & Gonzalez, L. Is vitamin D deficiency a major global public health problem?. J. Steroid Biochem. Mol. Biol. 144, 138–145. https://doi.org/10.1016/j.jsbmb.2013.11.003 (2014).
Esposito, S. et al. Vitamin D and growth hormone in children: A review of the current scientific knowledge. J. Transl. Med. 17(1), 87. https://doi.org/10.1186/s12967-019-1840-4 (2019).
Ceolin, G. et al. Adiposity and physical activity are among the main determinants of serum vitamin D concentrations in older adults: the EpiFloripa Aging Cohort Study. Nutr. Res. 111, 59–72. https://doi.org/10.1016/j.nutres.2023.01.004 (2023).
MacLaughlin, J. & Holick, M. F. Aging decreases the capacity of human skin to produce vitamin D3. J. Clin. Invest. 76(4), 1536–1538. https://doi.org/10.1172/JCI112134 (1985).
Chalcraft, J. R. et al. Vitamin D synthesis following a single bout of sun exposure in older and younger men and women. Nutrients 12(8), 2237. https://doi.org/10.3390/nu12082237 (2020).
Luo, J., Quan, Z., Lin, S. & Cui, L. The association between blood concentration of 25- hydroxyvitamin D and sarcopenia: A meta-analysis. Asia Pac. J. Clin. Nutr. 27(6), 1258–1270. https://doi.org/10.6133/apjcn.201811_27(6).0013 (2018).
Dudenkov, D. V., Mara, K. C., Petterson, T. M., Maxson, J. A. & Thacher, T. D. Serum 25-hydroxyvitamin D values and risk of all-cause and cause-specific mortality: A population-based cohort study. Mayo Clin. Proc. 93(6), 721–730. https://doi.org/10.1016/j.mayocp.2018.03.006 (2018).
World Health Organization (WHO). Aging and Health. 2021. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed May 2023.
Kim, S. H. et al. The factors associated with Vitamin D deficiency in community dwelling elderly in Korea. Nutr. Res. Pract. 12(5), 387–395. https://doi.org/10.4162/nrp.2018.12.5.387 (2018).
Solis-Urra, P. et al. Passive commuting and higher sedentary time is associated with vitamin D deficiency in adult and older women: Results from Chilean National Health Survey 2016–2017. Nutrients. 11(2), 300. https://doi.org/10.3390/nu11020300 (2019).
World Health Organization (WHO). Social Determinants of Health. New Delhi. 2008. https://apps.who.int/iris/bitstream/handle/10665/206363/B3357.pdf. Accessed May 2023.
Sobrino, M., Gutiérrez, C., Cunha, A. J., Dávila, M., & Alarcón, J. Desnutrición infantil en menores de cinco años en Perú: Tendencias y factores determinantes. [Child malnutrition in children under five years of age in Peru: trends and determinants]. Rev Panam Salud Pública. 35, 104–12 (2014). https://iris.paho.org/handle/10665.2/8432
Santos, A. et al. Vitamin D status and associated factors among Portuguese older adults: Results from the Nutrition UP 65 cross-sectional study. BMJ Open. 7(6), e016123. https://doi.org/10.1136/bmjopen-2017-016123 (2017).
ALbuloshi, T., Kamel, A. M. & Spencer, J. P. E. Factors associated with low vitamin D status among older adults in Kuwait. Nutrients 14(16), 3342. https://doi.org/10.3390/nu14163342 (2022).
Laird, E. et al. The prevalence of vitamin D deficiency and the determinants of 25(OH)D concentration in older Irish adults: Data from the irish longitudinal study on ageing (TILDA). J. Gerontol. A Biol. Sci. Med. Sci. 73(4), 519–525. https://doi.org/10.1093/gerona/glx168 (2018).
Chen, J. et al. Vitamin D status among the elderly Chinese population: A cross-sectional analysis of the 2010–2013 China national nutrition and health survey (CNNHS). Nutr. J. 16(1), 3. https://doi.org/10.1186/s12937-016-0224-3 (2017).
Orces, C. H. & Vitamin, D. Status among older adults residing in the Littoral and Andes mountains in Ecuador. ScientificWorldJournal. 2015, 545297. https://doi.org/10.1155/2015/545297 (2015).
Cotlear, D. et al. Overcoming social segregation in health care in Latin America. Lancet. 385(9974), 1248–1259. https://doi.org/10.1016/S0140-6736(14)61647-0 (2015).
Ministry of Health (Chile). National Health Survey 2016–2017. Vitamin D Report. 2018. https://goo.gl/oe2iVt. Accessed May 2023.
Ministry of Health (Chile). National Health Survey 2016–2017. 2018. http://epi.minsal.cl/bases-de-datos. Accessed March 2023.
Płudowski, P. et al. Guidelines for preventing and treating vitamin D deficiency: A 2023 update in Poland. Nutrients. 15(3), 695. https://doi.org/10.3390/nu15030695 (2023).
Dawson-Hughes, B., Harris, S. S. & Dallal, G. E. Plasma calcidiol, season, and serum parathyroid hormone concentrations in healthy elderly men and women. Am J Clin Nutr. 65(1), 67–71. https://doi.org/10.1093/ajcn/65.1.67 (1997).
Zemelman, V., von Beck, P., Alvarado, O. & Valenzuela, C. Sexual dimorphism in skin, eye and hair color and the presence of freckles in Chilean teenagers from two socioeconomic strata. Revista médica de Chile 130(8), 879–884. https://doi.org/10.4067/S0034-98872002000800006 (2002).
Alvear-Vega, S. & Vargas-Garrido, H. Social determinants of the non-utilization of the supplementary feeding program (PACAM) aimed at older adults’ nutritional support. Int. J. Environ. Res. Public Health. 19(21), 14580. https://doi.org/10.3390/ijerph192114580 (2022).
Petermann-Rocha, F. et al. Desde una mirada global al contexto chileno: ¿Qué factores han repercutido en el desarrollo de obesidad en Chile? (Parte 1) [From a global view to the Chilean context: What factors have impacted the development of obesity in Chile? (Part 1)]. Rev. Chil. Nutr. 47(2), 299–306. https://doi.org/10.4067/S0717-75182020000200299 (2020).
Žmitek, K., Hribar, M., Hristov, H. & Pravst, I. Efficiency of vitamin D supplementation in healthy adults is associated with body mass index and baseline Serum 25-hydroxyvitamin D level. Nutrients. 12(5), 1268. https://doi.org/10.3390/nu12051268 (2020).
Sollid, S. T., Hutchinson, M. Y., Fuskevåg, O. M., Joakimsen, R. M. & Jorde, R. Large individual differences in Serum 25-hydroxyvitamin D response to vitamin D supplementation: Effects of genetic factors, body mass index, and baseline concentration. Results from a randomized controlled trial. Horm. Metab. Res. 48(1), 27–34. https://doi.org/10.1055/s-0034-1398617 (2016).
Tsur, A., Metzger, M. & Dresner-Pollak, R. Effect of different dress style on vitamin D level in healthy young Orthodox and ultra-Orthodox students in Israel. Osteoporos. Int. 22(11), 2895–2898. https://doi.org/10.1007/s00198-010-1492-y (2011).
Agarwal, K. S. et al. The impact of atmospheric pollution on vitamin D status of infants and toddlers in Delhi, India. Arch. Dis Child. 87(2), 111–113. https://doi.org/10.1136/adc.87.2.111 (2002).
Nurbazlin, M. et al. Effects of sun exposure on 25(OH) vitamin D concentration in urban and rural women in Malaysia. Asia Pac. J. Clin. Nutr. 22(3), 391–399. https://doi.org/10.6133/apjcn.2013.22.3.15 (2013).
Author information
Authors and Affiliations
Contributions
R.B. designed the work, S.A. analyzed data and results, H.V. and S.A. wrote the manuscript. H.V., R.B., and S.A. reviewed literature and revised the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alvear-Vega, S., Benavente-Contreras, R. & Vargas-Garrido, H. Social determinants of serum 25-hydroxyvitamin D concentrations deficiency in older Chilean people. Sci Rep 13, 18355 (2023). https://doi.org/10.1038/s41598-023-45862-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45862-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.