Abstract
Whether the fascia iliaca compartment block (FICB) involves the obturator nerve (ON) remains controversial. Involvement may require that the injectate spreads deep in the cranial direction, and might thus depend on the site of injection. Therefore, the effect of suprainguinal needle insertion with five centimeters of hydrodissection-mediated needle advancement (S-FICB-H) on ON involvement and cranial injectate spread was studied in this radiological cadaveric study. Results were compared with suprainguinal FICB without additional hydrodissection-mediated needle advancement (S-FICB), infrainguinal FICB (I-FICB), and femoral nerve block (FNB). Seventeen human cadavers were randomized to receive ultrasound-guided nerve block with a 40 mL solution of local anesthetic and contrast medium, on both sides. Injectate spread was objectified using computed tomography. The femoral and lateral femoral cutaneous nerves were consistently covered when S-FICB-H, S-FICB or FNB was applied, while the ON was involved in only one of the 34 nerve blocks. I-FICB failed to provide the same consistency of nerve involvement as S-FICB-H, S-FICB or FNB. Injectate reached most cranial in specimens treated with S-FICB-H. Our results demonstrate that even the technique with the most extensive cranial spread (S-FICB-H) does not lead to ON involvement and as such, the ON seems unrelated to FICB. Separate ON block should be considered when clinically indicated.
Similar content being viewed by others
Introduction
Regional anesthesia (RA) techniques, such as fascial plane blocks and peripheral nerve blocks, have become a central component of multimodal analgesic strategies1. Benefits, in theory, include superior pain control, improved patient satisfaction, prevention of postoperative delirium, and reduced opioid consumption2,3,4. The use of RA is particularly relevant for (lower) extremity surgery due to its painful characteristics5. Numerous injection techniques targeting the hip, anterior thigh and knee have been developed, one of which is the fascia iliaca compartment block (FICB).
The origins of FICB can be traced back to Winnie’s 3-in-1 block, an anterior landmark approach to the lumbar plexus that targets the femoral nerve (FN), lateral femoral cutaneous nerve (LFCN) and obturator nerve (ON)6. Reports of inconsistent LFCN and ON blockade then led to studies that investigated the anatomical relations of the inguinal region, and local anesthetic distribution during 3-in-1 block7,8. These studies ultimately resulted in the establishment of a loss-of resistance technique, now known as FICB, targeting the fascia iliaca compartment (FIC)8. Later modifications of the technique include the incorporation of ultrasound guidance and more recently, the growing popularity of suprainguinal (S-FICB) over infrainguinal (I-FICB) injection sites9,10,11. However, although S-FICB was developed to acquire more consistent results when compared to I-FICB, debate persists over clinical superiority regarding coverage of the ON12,13,14,15,16,17,18,19,20.
Similar to other fascial plane blocks, FICB provides analgesia on the assumption that an injectate can open the potential space between the fascia iliaca (FI) anteriorly and the psoas major and iliacus muscles posteriorly, and spread towards the nerves within by means of bulk flow and diffusion21. However, recent anatomical reports have shown that the ON does not transverse the FIC, but rather passes through the psoas, retro-psoas and retroperitoneal compartments (Fig. 1)12,13. Consequently, local anesthetic (LA) is required to spread outside of the FIC in order to involve this nerve. While these studies agree on the closure of the FIC on its posteromedial border, they offer conflicting views on the existence of a cranially located opening to the retroperitoneal compartment and ON12,13. If this cranial path indeed exists, successful blockade of the ON with FICB would likely mandate overflowing the FIC, or a cranial injection site within the FIC.
A cross-sectional image, cut at the level of the anterior superior iliac spine, explaining the anatomical location of the obturator nerve (ON). The ON arises from the anterior divisions of the second, third and fourth lumbar spinal nerves in the psoas compartment. It then enters the retro-psoas compartment at the posteromedial border of the psoas major muscle, posterior to the iliac arteries and vein. Here, it is separated from the FIC (shown in green) by the psoas major and iliacus muscles, and the fascia transversalis (TF; shown in cyan). The parietal peritoneum is shown in purple. Subsequently, the ON enters the retroperitoneal compartment by invaginating the TF, and runs down the pelvis until it exits through the obturator canal. Thus, the FIC never encompasses the ON, but whether it has a cranial opening that offers a route to the retroperitoneal compartment and ON remains debated. The figure is reprinted with permission from Thomas Fichtner Bendtsen13. RPC retroperitoneal compartment, GFN genitofemoral nerve, LFCN lateral femoral cutaneous nerve, FN femoral nerve, eia external iliac artery, iia internal iliac artery, civ common iliac vein, ON obturator nerve, r-psoas-c retro-psoas compartment, LST lumbosacral trunk.
Therefore, we set up a radiological cadaveric study to determine the effect of a cranial injection deep under the FI using suprainguinal needle insertion with five centimeters of additional hydrodissection-mediated needle advancement (S-FICB-H) on coverage of the ON. Further, we measured cranial injectate spread and involvement of the FN and LFCN. Results were compared with S-FICB without additional hydrodissection-mediated needle advancement, I-FICB, and femoral nerve block (FNB). We hypothesized that the injectate would reach most cranial for S-FICB-H, but that none of the nerve block techniques would result in reliable coverage of the ON.
Methods
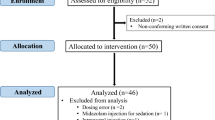
A convenience sample of 17 fresh, unfrozen and unembalmed adult human cadavers was included in this study. Cadavers were bequeathed to the Amsterdam University Medical Centers (location AMC) to serve research and educational purposes. Written informed consent for donation was given during life, in accordance with the Dutch Burial and Cremation act (BWBR0005009). The Medical Ethical Committee of the Amsterdam University Medical Centers (location AMC) provided a waiver for approval of this study. Further, experiments were performed according to relevant international and institutional regulations and ethics guidelines. The presented findings are reported according to the Anatomical Quality Assurance (AQUA) checklist22.
Nerve block technique
Nerve blocks were performed bilaterally, but each side was randomized individually. Thus, totaling eight or nine nerve blocks per injection technique (Table 1). The injectate was a mixture of 38 mL of LA and 2 mL of contrast medium (Visipaque™, GE Healthcare, Eindhoven, The Netherlands) for all techniques. This total volume was chosen as it reflects routine clinical practice, while previous research suggests that this volume may be able to reach the target nerves, including the ON17,23. Ultrasound guidance was used to visualize the different anatomical structures, to guide the needle tip to the correct plane, and to observe injectate spread. Nerve blocks were placed by two anesthesiologists specialized in regional anesthesia (WtH, HMB). Study procedures were completed within six hours of arrival at the Amsterdam University Medical Centers.
S-FICB was applied by puncturing the skin approximately one centimeter cranial to the inguinal ligament in caudal to cranial fashion9. In the S-FICB-H group, we subsequently advanced the needle tip an additional five centimeters under the FI (using hydrodissection) in order to achieve a pronounced cranial position not previously documented in the literature for a single-shot technique. I-FICB was performed at the lateral third of the line connecting the pubic tubercle and the anterior superior iliac spine, one centimeter caudal to the inguinal ligament10. The injection was placed at the inguinal crease, adjacent to the FN, in case of (ultrasound-guided) FNB.
Outcome parameters and data analysis
The primary outcome parameter of this study was ON coverage. Additionally, we measured cranial injectate spread as a function of the injectate’s ability to migrate to the debated cranial opening (in the FIC) and ON12,13. Further, FN and LFCN coverage were other secondary outcome parameters.
Injectate spread was documented 15 min after injection using whole-body computed tomography (CT) (Siemens SOMATOM Force, Siemens Healthineers, Forchheim, Germany; CT collimation 0.6 mm, dual energy 100/Sn150 kVp, 486/244 mA, pitch 0.6, slice thickness 1.0 mm, soft kernel). A musculoskeletal radiologist blinded to the injection technique assessed the locoregional contrast medium spread. Perineural presence of contrast was assessed by visualization and inspection of the anatomical location of the relevant structures in axial, sagittal and coronal planes, with additional reformatting when deemed necessary. For example, the full path of the ON between its origin and exit through the obturator foramen was inspected. Cranial diffusion was measured in coronal reformatted images from the femoral head (in centimeters) and is also described in relation to the corresponding vertebra.
Data for cranial injectate spread was tested for normality using histograms and the Shapiro–Wilk test, and is presented as mean ± standard deviation. Cranial injectate spread was subsequently compared across the study arms by applying one-way ANOVA and Tukey post-hoc testing. Other outcome measures were summarized as frequencies with percentages. A P-value smaller than 0.05 was deemed statistically significant. IBM SPSS Statistics, Version 28.0.1.0, was used for statistical analysis (IBM Corp., Armonk, NY, USA).
Results
Cadavers were predominantly male (12 of 17, 71%). Further baseline characteristics and details about prior medical history were unavailable, due to the anonymous nature of the body donation program.
Nerve involvement
The ON was involved in one (S-FICB) of 34 nerve blocks, while none reached the lumbar plexus. The nerve block that did reach the ON was found to involve this nerve in the retroperitoneal compartment, at a level corresponding to the first sacral vertebra (Fig. 2). This was also the maximum height reached by the contrast for this block. Medial injectate spread was limited in other cases and did not reach the ON, as exemplified in Fig. 3 after bilateral S-FICB-H.
Coronal (a) and axial (b) CT imagery of the S-FICB case wherein the contrast mixture reached the ON (left side). The injectate was found to involve the ON in the retroperitoneal compartment at the level of the first sacral vertebra, which was also the maximum height that was reached. Dashed arrows point to the ON, while solid arrows point to contrast.
Axial CT slices detailing typical spread of injectate after (bilateral) S-FICB-H. The LA-based contrast mixture was determined to reach a maximum height corresponding to the fifth lumbar vertebra on the left side and the intervertebral disc of lumbar vertebrae four-five on the right side. Medial spread of contrast stayed anterior to the iliopsoas muscles and iliac arteries. As such, contrast remained removed of the location of the lumbar plexus and ON, both in the cranial and medial directions. Dotted arrows point to the iliac arteries, solid arrows point to the contrast. l lumbar vertebra, s sacral vertebra, ac acetabulum, cfa common femoral artery, pf proximal femur, P psoas muscle, I iliacus muscle, IP iliopsoas muscle.
The FN and LFCN were consistently involved in S-FICB-H, S-FICB and FNB, while these structures were considerably less often involved in I-FICB (22.2% and 44.4% of cases, respectively). Details of nerve involvement are summarized in Table 1. Figure 4 depicts a volume rendering reconstruction of a cadaver with typical injectate distribution patterns after bilateral S-FICB-H.
A 3D volume rendered reconstruction of CT-imaging of a specimen that was randomized to receive bilateral S-FICB-H. Contrast reached a maximum height equal to the level of the fifth lumbar vertebra on the left side and the intervertebral disc of lumbar vertebrae four-five on the right side. The arrows point to the contrast.
Cranial injectate spread
Spread of the injectate towards the lumbar plexus was measured in relation to the femoral head. Truncal spread was found in only two of nine (22%) I-FICBs and as such, I-FICB was excluded from statistical analysis. The mean cranial spread of S-FICB-H (14.00 ± 3.16 cm) was significantly more than that of S-FICB (10.28 ± 2.95 cm, p = 0.046), or FNB (5.30 ± 2.86 cm, p ≤ 0.001). Injectate reached higher for S-FICB than for FNB (p = 0.008). Similar distribution patterns were observed when cranial injectate spread was related to the vertebral column, as shown in Table 2, and demonstrated for S-FICB-H in Fig. 3.
Discussion
This radiological cadaveric study supports the hypothesis that S-FICB-H leads to the most cranial injectate spread of the techniques targeting the FIC. Concurrently, however, our findings also demonstrate that pronounced cranial injectate spread will not result in reliable blockade of the ON. I-FICB resulted in less involvement of the FN and LFCN than S-FICB-H, S-FICB and FNB.
The ON is a mixed sensory and motor nerve that derives from the anterior divisions of the second, third and fourth lumbar spinal nerves. Its branches innervate the adductor muscles of the thigh, and the hip and knee joints. Further, the ON contributes, in some patients, to the sensory innervation of a section of the medial thigh. Therefore, inclusion of ON blockade in FICB would improve analgesia after lower extremity procedures, such as hip fracture surgery.
However, it is still debated whether the ON can indeed be covered during FICB. Clinical examination after FICB may be ambiguous due to the highly variable cutaneous innervation of the ON and co-innervation to the adductor muscles24. Meanwhile, (both primary and secondary) cadaveric dissection is prone to disrupt the integrity of fascial layers, and is therefore at risk of false positive research results. This study therefore applied CT-imaging of a LA-based contrast mixture, as it allowed for precise and objective (numerical) measurements of injectate spread. Additionally, CT-imaging allowed us to include 34 samples, a number which would have been unrealistic to obtain with dissection (or magnetic resonance imaging; MRI). Further, the advanced CT scanner used here provided us with similar information as would have been obtained with MRI.
The data presented here for S-FICB (both with and without additional needle advancement) deviates from previously reported success rates of ON involvement, but is closely aligned to reported rates of FN and LFCN blockade9,11,17. Literature details differing success rates for I-FICB8,10,17,25,26,27,28,29,30. Interestingly, our results are similar to that of authors who performed I-FICB based on the description that was also the foundation of the technique applied in this study17,28. The current study supports the conclusion that S-FICB leads to more cranial spread and better FN and LFCN involvement than I-FICB, yet our results indicate less cranial distribution patterns for conventional S-FICB and I-FICB than previously reported in a volunteer study17. The 40 mL injectate allowed FNB to behave as a field block, while the inguinal injection site might have facilitated more efficient migration towards the FN and LFCN than possible for I-FICB.
The ON’s path between its origin and the obturator foramen is of importance as the aforementioned nerve block approaches are all based on the presumption that the ON can be reached by an injectate in the FIC6,8,9,10,11. However, anatomical reports have shown that the ON does not travel within the FIC and suggested an alternative mechanism of action: cranial diffusion from the FIC to the retroperitoneal compartment12,13. Assuming this path exists, lack of ON involvement can be hypothesized to be caused by either an inadequate injection volume and injection force, or a too distal injection site, placing the LA out of reach from the retroperitoneal compartment. This scenario could explain the unusually high—compared to the FIC’s capacity of 23 mL—minimum effective volume of 62.5 mL found in a recent cadaver dissection study that applied a step-up, step-down algorithm to determine the optimal injectate volume12,14. However, it is as of yet unknown what effect a large injectate volume, or high injection pressure, has on fascial plane integrity (while concurrently the clinical relevance and utility of a nerve block approach that requires injection of a large number of ampoules can be debated). Similar to needle misplacement in the retroperitoneal compartment, disruption of the fascial compartment could lead to creation of an artificial opening in the FI and diffusion towards the ON15. This, however, would not be a true fascial plane block and constitutes a different mechanism than sought after with a FICB. We speculate that this mechanism is the explanation for the case in which the ON was successfully involved in our study, and the underlying reason for the limited replicability of studies.
Alternatively, this investigation assessed whether advanced needle insertion into the cranial direction would result in ON involvement. The lack thereof shown here contradicts the existence of an easily accessible cranial route from the FIC to the retroperitoneal compartment. Further, as reported in other studies, posteromedial spread was limited and remained removed from the ON19,25. Thus, overall, achieving reliable ON blockade using a FIC approach seems not possible, as illustrated by the presented data, the considerable number of published methodological variations, and the differences in reported success rates between studies that applied the same injection technique.
A limitation of this study is the reliance on (human) cadavers as tissue quality might have deteriorated after death. However, specimens were fresh, unfrozen and unembalmed, allowing for near-normal block procedures as shown by the pattern of spread after nerve blocks.
Conclusion
In summary, neither S-FICB-H nor any other technique targeting the FIC leads to reliable ON involvement, and as such the ON seems to be unrelated to fascial plane blocks targeting the FIC. Addition of a separate ON block to S-FICB (or large volume FNB) should be considered when clinically indicated.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Wick, E. C., Grant, M. C. & Wu, C. L. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: A review. JAMA Surg. 152, 691–697. https://doi.org/10.1001/Jamasurg.2017.0898 (2017).
Joshi, G., Gandhi, K., Shah, N., Gadsden, J. & Corman, S. L. Peripheral nerve blocks in the management of postoperative pain: Challenges and opportunities. J. Clin. Anesth. 35, 524–529. https://doi.org/10.1016/J.Jclinane.2016.08.041 (2016).
Mouzopoulos, G. et al. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: A randomized placebo-controlled study. J. Orthop. Traumatol. 10, 127–133. https://doi.org/10.1007/S10195-009-0062-6 (2009).
Kim, C. H. et al. The effect of regional nerve block on perioperative delirium in hip fracture surgery for the elderly: A systematic review and meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 108, 103151. https://doi.org/10.1016/J.Otsr.2021.103151 (2022).
Gerbershagen, H. J. et al. Pain intensity on the first day after surgery: A prospective cohort study comparing 179 surgical procedures. Anesthesiology 118, 934–944. https://doi.org/10.1097/Aln.0b013e31828866b3 (2013).
Winnie, A. P., Ramamurthy, S. & Durrani, Z. The inguinal paravascular technic of lumbar plexus anesthesia: The “3 in 1 block”. Anesth. Analg. 52, 989–996 (1973).
Marhofer, P., Nasel, C., Sitzwohl, C. & Kapral, S. Magnetic resonance imaging of the distribution of local anesthetic during the three-in-one block. Anesth. Analg. 90, 119–124. https://doi.org/10.1097/00000539-200001000-00027 (2000).
Dalens, B., Vanneuville, G. & Tanguy, A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth. Analg. 69, 705–713 (1989).
Desmet, M. et al. A longitudinal supra-inguinal fascia iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg. Anesth. Pain Med. 42, 327–333. https://doi.org/10.1097/Aap.0000000000000543 (2017).
Dolan, J., Williams, A., Murney, E., Smith, M. & Kenny, G. N. Ultrasound guided fascia iliaca block: a comparison with the loss of resistance technique. Reg. Anesth. Pain. Med. 33, 526–531. https://doi.org/10.1016/J.Rapm.2008.03.008 (2008).
Hebbard, P., Ivanusic, J. & Sha, S. Ultrasound-guided supra-inguinal fascia iliaca block: A cadaveric evaluation of a novel approach. Anaesthesia 66, 300–305. https://doi.org/10.1111/J.1365-2044.2011.06628.X (2011).
Xu, Z. et al. Fibrous configuration of the fascia iliaca compartment: An epoxy sheet plastination and confocal microscopy study. Sci. Rep. 10, 1548. https://doi.org/10.1038/S41598-020-58519-0 (2020).
Bendtsen, T. F. et al. Anatomical considerations for obturator nerve block with fascia iliaca compartment block. Reg. Anesth. Pain Med. 46, 806–812. https://doi.org/10.1136/Rapm-2021-102553 (2021).
Kantakam, P. et al. Cadaveric investigation of the minimum effective volume for ultrasound-guided suprainguinal fascia iliaca block. Reg. Anesth. Pain Med. 46, 757–762. https://doi.org/10.1136/Rapm-2021-102563 (2021).
Bendtsen, T. F. et al. Suprainguinal fascia iliaca block: Does it block the obturator nerve?. Reg. Anesth. Pain Med. 46, 832. https://doi.org/10.1136/Rapm-2021-102712 (2021).
Tran, Q. et al. Reply to Dr Bendtsen and colleagues. Reg. Anesth. Pain Med. 46, 832–833. https://doi.org/10.1136/Rapm-2021-102782 (2021).
Vermeylen, K. et al. Supra-inguinal injection for fascia iliaca compartment block results in more consistent spread towards the lumbar plexus than an infra-inguinal injection: A volunteer study. Reg. Anesth. Pain Med. 44, 483. https://doi.org/10.1136/Rapm-2018-100092 (2019).
Vermeylen, K., Leunen, I. & Desmet, M. Response to the letter to the editor by Bendtsen et al. “Supra-inguinal injection for fascia iliaca compartment block results in more consistent spread towards the lumbar plexus than an infra-inguinal injection: A volunteer study”. Reg. Anesth. Pain Med. 45, 243–244. https://doi.org/10.1136/Rapm-2019-100725 (2020).
Bendtsen, T. F., Pedersen, E. M. & Peng, P. Course of the obturator nerve. Reg. Anesth. Pain Med. 44, 1039. https://doi.org/10.1136/Rapm-2019-100655 (2019).
Tran, D. Q., Boezaart, A. P. & Neal, J. M. Reply to Dr Wilson. Reg. Anesth. Pain Med. 43, 564–565. https://doi.org/10.1097/Aap.0000000000000800 (2018).
Chin, K. J., Lirk, P., Hollmann, M. W. & Schwarz, S. K. W. Mechanisms of action of fascial plane blocks: A narrative review. Reg. Anesth. Pain Med. 46, 618–628. https://doi.org/10.1136/Rapm-2020-102305 (2021).
Tomaszewski, K. A. et al. Development of the anatomical quality assurance (aqua) checklist: Guidelines for reporting original anatomical studies. Clin. Anat. 30, 14–20. https://doi.org/10.1002/Ca.22800 (2017).
Vermeylen, K. et al. The effect of the volume of supra-inguinal injected solution on the spread of the injectate under the fascia iliaca: A preliminary study. J. Anesth. 32, 908–913. https://doi.org/10.1007/S00540-018-2558-9 (2018).
Bouaziz, H. et al. An evaluation of the cutaneous distribution after obturator nerve block. Anesth. Analg. 94, 445–449. https://doi.org/10.1097/00000539-200202000-00041 (2002).
Swenson, J. D. et al. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: The pattern of distribution and effects on the obturator nerve. J. Clin. Anesth. 27, 652–657. https://doi.org/10.1016/J.Jclinane.2015.07.001 (2015).
Capdevila, X. et al. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: Clinical and radiographic analysis. Anesth. Analg. 86, 1039–1044. https://doi.org/10.1097/00000539-199805000-00025 (1998).
Morau, D. et al. Comparison of continuous 3-in-1 and fascia iliaca compartment blocks for postoperative analgesia: Feasibility, catheter migration, distribution of sensory block, and analgesic efficacy. Reg. Anesth. Pain Med. 28, 309–314. https://doi.org/10.1016/S1098-7339(03)00183-4 (2003).
Shariat, A. N. et al. Fascia lliaca block for analgesia after hip arthroplasty: A randomized double-blind, placebo-controlled trial. Reg. Anesth. Pain Med. 38, 201–205. https://doi.org/10.1097/Aap.0b013e31828a3c7c (2013).
Foss, N. B. et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: A randomized, placebo-controlled trial. Anesthesiology 106, 773–778. https://doi.org/10.1097/01.Anes.0000264764.56544.D2 (2007).
Lopez, S., Gros, T., Bernard, N., Plasse, C. & Capdevila, X. Fascia iliaca compartment block for femoral bone fractures in prehospital care. Reg. Anesth. Pain Med. 28, 203–207. https://doi.org/10.1053/Rapm.2003.50134 (2003).
Author information
Authors and Affiliations
Contributions
W.H., P.S., H.B., J.H., L.B., R.O., P.M., P.L., M.H. designed the experiments; W.H., H.B., L.B., P.L. performed the experiments; W.H., P.S., J.H., L.B., R.O., P.M., P.L., M.H. analyzed and interpreted the data; P.S. and W.H. drafted the manuscript; W.H., P.S, H.B., J.H., L.B., R.O., P.M., P.L., M.H. critically revised the manuscript. All authors reviewed and approved the manuscript for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
ten Hoope, W., Smulders, P.S.H., Baumann, H.M. et al. A radiological cadaveric study of obturator nerve involvement and cranial injectate spread after different approaches to the fascia iliaca compartment block. Sci Rep 13, 12070 (2023). https://doi.org/10.1038/s41598-023-39041-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-39041-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.