Abstract
Use of hijab can influence the scalp’s condition, including its microbiome. To date there has been no study comparing scalp microbiome in women wearing hijab to that in women not wearing hijab. This was a cross-sectional study conducted from August 2019 to April 2021. Healthy women aged 18 years old or older who had not undergone menopause were recruited. Those in the hijab group should wear hijab minimum 8 h a day for at least 5 years. After wash-out period, the sample was collected from the subject’s scalp. Next Generation Sequencing (NGS) was performed with primer V3-V4 region of 16S rRNA and ITS1 DNA for bacteria and fungi, respectively. Alpha diversity and beta diversity were identified, along with functional analysis. Actinobacteria and Ascomycota were the most dominant phyla on the scalp. S. capitis was more prominent in the hijab group while S. cohnii was more prominent in non-hijab group. Additionally, M. restricta was more common in hijab group while M. globosa was more common in non-hijab group. This study emphasizes the difference of scalp microbiome in women wearing hijab compared to women not wearing hijab, which indicated that women wearing hijab are more prone to seborrheic dermatitis.
Similar content being viewed by others
Introduction
The scalp skin is inhabited by abundant microorganisms, known as microbiota. The microbiota has a mutual relationship with the host as it plays a role in skin inflammatory responses and homeostasis. The equilibrium of microbiota-host relationship is necessary to keep the skin vigorous. The skin microbiota develops over the years with different dominant phyla each life stage. Also, different sites have different microbial communities. Multiple factors influence the skin microbiome, some of them are still unknown1. Gender, age, hair treatment, lifestyle, and geographical regions are several factors that are thought to influence the scalp microbiome2,3.
Dysbiosis of the scalp microbiome might influence the course of some disorders e.g., seborrheic dermatitis, androgenetic alopecia, alopecia areata, syphilitic alopecia, cicatricial alopecia, folliculitis decalvans, folliculitis, and tinea capitis3,4. In addition, dysbiosis of scalp microbiome was also reported in sensitive scalp which was characterized by various abnormal sensory symptoms (pruritus, pain, tingling, burning)5. Both fungal and bacterial communities in the scalp can interact with the host, leading to alteration of the scalp health. Hence, the scalp microbiome should also be given attention when managing scalp diseases3.
Indonesia is a tropical country in which majority of its citizens were Muslim. Most of the Muslim women have practice the use of hijab since they were a child. A hijab is worn to cover the hair and body with various styles6. The use of hijab, especially for a long time, might occlude the scalp which results in accumulation of sebum and scalp. These can predispose the women to itch and dandruff. In addition, some of the women who do not dry their hair and use hijab directly might cause the hair flat and damaged. Use of hijab can also reduce sunlight exposure to the scalp which reduces the vitamin D source7. A previous study also showed that use of hijab was associated with increased transepidermal water loss (TEWL) of the scalp8. Considering these changes, this study aims to compare the scalp microbiome of healthy women wearing hijab to those not wearing hijab.
Results
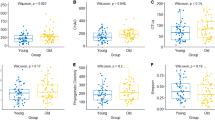
A total of 96 subjects were recruited to the study, comprising 48 healthy women wearing hijab and 48 healthy women not wearing hijab (Supplementary Fig. S1). Of all bacteria identified, the most abundance bacterial phyla on the scalp were Actinobacteria, Proteobacteria, Firmicutes, and Bacteroidetes (Fig. 1). The three most dominant species were Propionibacterium acnes, Staphylococcus capitis, and Staphylococcus cohnii. While the most abundance fungal phyla on the scalp were Ascomycota and Basidiomycota (Fig. 2). The most dominant species were Malassezia globosa and M. restricta. Post-hoc power analysis on the fungal findings showed 99.9% power while post-hoc power analysis on the bacterial findings showed 5.3% power, indicating lack of power for the bacterial study.
Bacterial taxonomic tree of all subjects (generated using GraPhlAn tools from https://huttenhower.sph.harvard.edu/graphlan/).
Fungal taxonomic tree of all subjects (generated using GraPhlAn tools from https://huttenhower.sph.harvard.edu/graphlan/).
Beta diversity of both groups showed different microbial dominance (Figs. 3 and 4). Both groups showed P. acnes dominance. However, S. capitis was more prominent in hijab group while S. cohnii was more prominent in non-hijab group. Additionally, M. restricta was more common in hijab group while M. globosa was more common in non-hijab group.
Comparison of bacterial species on scalp microbiome of healthy woman wearing hijab and not wearing hijab (generated using iTOL tools from https://itol.embl.de/ and Microsoft Excel).
Comparison of fungal species on scalp microbiome of healthy woman wearing hijab and not wearing hijab (generated using iTOL tools from https://itol.embl.de/ and Microsoft Excel).
Further functional analysis is shown in Figs. 5 and 6. According to KEGG pathway L2 analysis, the hijab group had statistically significant lower signaling molecules and interaction, enzyme families, digestive system, genetic information processing, and infectious diseases compared to non-hijab group. The non-hijab group had statistically significant lower cell growth and death, transcription, as well as xenobiotics degradation and metabolism compared to hijab group. According to KEGG pathway L3 analysis, the hijab group had statistically significant lower riboflavin metabolism, bacterial toxins, biotin metabolism, histidine metabolism, ascorbate and aldarate metabolism, restriction enzyme, amoebiasis, ether lipid metabolism, bacterial invasion of epithelial cells, transcription-related proteins, xylene degradation, lysine biosynthesis, novobiocin biosynthesis, alpha-linoleic acid metabolism, phosphotransferase system, fructose and mannose metabolism, galactose metabolism, ethylbenzene degradation, S. aureus infection, arginine and proline metabolism, as well as protein kinases compared to non-hijab group. On the other hand, the non-hijab group had significantly lower bisphenol degradation, chlorocyclohexane and chlorobenzene degradation, thiamine metabolism, primary bile acid biosynthesis, secondary bile acid biosynthesis, linoleic acid metabolism, butanoate metabolism, glycine, serine, and threonine metabolism, meiosis, valine, leucine, and isoleucine degradation, carbon fixation in photosynthetic organisms, polycyclic aromatic hydrocarbon degradation, peptidoglycan biosynthesis, lipid biosynthesis proteins, xenobiotics metabolism by cytochrome P450, biosynthesis of unsaturated fatty acids, sulfur metabolism, drug metabolism, glycolysis, retinol metabolism, cysteine and methionine metabolism, general function prediction, secretion system, aminobenzoate degradation, and DNA replication proteins.
Functional analysis of KEGG pathway L2 of scalp microbiome in hijab group vs. non-hijab group (generated using STAMP tools from https://beikolab.cs.dal.ca/software/STAMP).
Functional analysis of KEGG pathway L3 of scalp microbiome in hijab group vs. non-hijab group (generated using STAMP tools from https://beikolab.cs.dal.ca/software/STAMP).
Discussion
This study showed that Actinobacteria, Proteobacteria, Firmicutes, and Bacteroidetes were the dominant phyla in the scalp of healthy women. Similarly, Watanabe et al. reported that Actinobacteria, Proteobacteria, and Firmicutes were the dominant phyla in the scalp of 109 healthy males and females2. Actinobacteria, Firmicutes, and Proteobacteria are also the most dominant phyla in hair follicle4.
The three most dominant species were Propionibacterium acnes, Staphylococcus capitis, and Staphylococcus cohnii. Lousada et al. also reported that Propionibacteria, Staphylococci, and Pseudomonades were the dominant bacteria in the hair follicle4. Watanabe et al. also reported similar bacteria on the scalp hair shaft of healthy individuals2. These bacteria are found to be abundant on the vertex and occipital regions of the scalp. Propionibacteria is also predominant on the facial skin and axilla while Staphylococcus is predominant in axilla. Both species are associated with acne vulgaris and alopecia areata4.
Beta diversity of both groups showed different microbial dominance. Both groups showed P. acnes dominance. Propionibacterium resides in the hair follicle which is difficult to reach by disinfectant. Hence, its abundance is relatively constant4. P. acnes has the ability to hydrolyze triglycerides into free fatty acids. It also amplifies bacterial adherence and eliminates other strains with bacteriocins. It was also reported to increase significantly along with perturbed scalp microbiome in sensitive scalp. Sensitive scalp is characterized by pruritus, discomfort, tingling, tightness, and burning when the scalp is exposed to environment5. This was reported by women who used hijab7. From our findings, we can see that the dominant P. acnes species in scalp, might predispose the healthy women into sensitive scalp in both those wearing hijab and not wearing hijab.
However, S. capitis was more prominent in hijab group while S. cohnii was more prominent in non-hijab group. S. capitis is one of the coagulase-negative staphylococci which normally resides on the human mucous membranes and skin9. A previous study had isolated S. capitis from the foot’s skin of healthy subjects. S. capitis was proven to be beneficial by producing antimicrobial peptides, which was particularly effective on eliminating Gram positive organisms, such as S. aureus, P. acnes, Micrococcus luteus, and Bacillus subtilis. The produced peptides were proven not to be harmful towards human keratinocytes10,11. However, another study reported that S. capitis was linked to bloodstream infections. The pathogenesis of S. capitis infection is thought to be multifactorial, attributed to its ability to invade and destruct epithelial cells. Similarly, S. cohnii is a member of coagulase-negative staphylococci which has been linked to infections9. S. cohnii has two main subspecies, which are S. cohnii subsp. urealyticus and S. cohnii subsp. cohnii. While S. cohnii subsp. urealyticus is often identified in people who stay at home, S. cohnii subsp. cohnii is often identified in hospital staffs and hospitalized patients12. In spite of this finding, the latest study showed that S. cohnii might be beneficial by managing inflammation without affecting other microbiota13. With this finding, we hypothesize that inflammatory skin diseases, such as seborrheic dermatitis, are more often found in women wearing hijab compared to women not wearing hijab due to the more dominant S. cohnii findings in women not wearing hijab. On the other hand, bacterial skin infections might be more common in women not wearing hijab compared to women wearing hijab due to the more abundant S. capitis in women wearing hijab.
The most abundant fungal phyla on the scalp were Ascomycota and Basidiomycota. Previous study also reported that Ascomycota was dominant on scalp of healthy subjects while Basidiomycota was more common on scalp of subjects with dandruff14. The most dominant species were M. globosa and M. restricta. These species are predominant in the hair follicle. Malassezia is associated with seborrheic dermatitis, psoriasis, and androgenetic alopecia4. Park et al. reported that Malassezia spp. was identified 0.07% of the healthy scalps and higher (2%) in the scalps with dandruff. It was also stated that the most common fungal species identified in normal scalp were Acremonium spp., Didymella spp., and Cryptococcus spp14. Different geographical area, hair care, and use of hijab can influence these different findings in our study.
It was found that M. restricta was more common in hijab group while M. globosa was more common in non-hijab group. Increased abundance of M. restricta accompanied by decreased abundance of M. globosa was reported in seborrheic dermatitis patients4. However, another study reported that M. globosa was present in 52% of seborrheic dermatitis patients’ scalp in Indonesia15. Malassezia is known to produce triglyceride lipases which cleaves the triglycerides into free fatty acids. These free fatty acids will induce inflammation on the scalp and disrupt the skin barrier of the scalp. Presence of Staphylococcus can aid Malassezia in developing dandruff and seborrheic dermatitis through sebum hydrolyzation, which supplies nutrients for Malassezia3,4. Nevertheless, the occurrence of seborrheic dermatitis is influenced by various factors, not only the role of Malassezia3. Therefore, our study suggest that both women wearing hijab and not wearing hijab might be prone to seborrheic dermatitis due to the abundant Malassezia findings.
This study also conducted functional analysis with Kyoto Encyclopedia of Genes and Genomes (KEGG) Pathway (www.kegg.jp/kegg/kegg1.html). It focuses on 8 KEGG pathways level 2 and 46 KEGG pathways level 3. The results suggested that infectious diseases and S. aureus infection were more common in the non-hijab group. Several other pathways also had significant differences between both groups. However, these results should be further studied since this is the first study in Indonesia which compared the scalp microbiome in women wearing hijab to women not wearing hijab. Limitations of this study were small sample size and use only one primer for each fungal and bacterial analysis, so that a few organisms could not be identified. In addition, the analysis on the association between hijab materials and scalp microbiome was not conducted due to insufficient data.
This study emphasizes the difference of scalp microbiome in women wearing hijab compared to women not wearing hijab. Women wearing hijab were found to have more S. capitis and M. restricta on their scalps while women not wearing hijab were found to have more S. cohnii and M. globosa on their scalps. These findings indicated that women wearing hijab are more prone to seborrheic dermatitis compared to women not wearing hijab while women not wearing hijab are more prone to bacterial skin infections. Further studies are warranted to analyze the correlation between these microbiome findings with clinical and histopathological findings as well as to search the best method to improve the scalp microbiome in women wearing hijab.
Methods
Study design and ethical approval
This study was conducted with cross-sectional design from August 2019 to April 2021. Samples were collected from November 2019 to March 2020 during the dry season. This was a part of larger study analyzing the characteristics of scalp microbiome and clinical features in women wearing hijab versus women not wearing hijab. The study has been approved by ethics committee of Faculty of Medicine Universitas Indonesia (ethical approval number KET-888/UN2.F1/ETIK/PPM.00.02/2019). The study protocol has been registered in clinicaltrials.gov (NCT05267119). The investigation was performed in accordance with the Declaration of Helsinki.
Study criteria
Inclusion criteria were: (1) healthy women aged 18 years old or older who had not undergone menopause, (2) wearing hijab for at least 5 years with duration of use minimum 8 hours a day for the hijab group, and (3) providing consent to participate in the study. Exclusion criteria were: (1) had history of scalp or hair disorders (e.g. alopecia, trichotillomania, malignancy, infection), (2) currently using topical or systemic medications for hair and/or scalp, (3) currently using cytostatic agents for malignancy or other disorders, (4) had history of hypersensitivity towards shampoo’s basic ingredients, (5) pregnancy or breastfeeding, (6) currently using hair or scalp care products, (7) consuming vitamin D supplements for the past 6 months, (8) receiving topical vitamin D analogue therapy, and (9) had history of diabetes mellitus, liver disorders, renal disorders, vitiligo, and/or autoimmune diseases. All participants were asked to sign the informed consent form prior to the study. Subjects were recruited consecutively.
Study preparation
All participants were screened first and given instructions prior to the sample collection. Each participant received 1 bottle of regular shampoo (30 ml) to be used twice a week for 2 weeks. The last hair wash was 3 days before the sample collection.
Sample collection
Sample was collected in a sterile room. The room temperature was kept at 20 °C. The investigators used personal protective equipment (PPE), comprising surgical cap, surgical mask, disposable gloves, and disposable gown. A DNA/RNATM shield collection tube with swab was used to collect the sample. The investigator used a comb to reveal an area of 4 × 4 cm at the vertex. The area was marked. The swab was moistened with buffer solution. At each vertical, horizontal, left diagonal, and right diagonal direction, the premoistened swab was stroked 5 times. Each time comprised 10 motions back and forth. The sample was stored within the tube containing buffer solution. All samples were stored in a freezer at – 80 °C.
DNA extraction and sequencing
Dnaeasy® Powersoil® Pro Kit was used for DNA extraction. The process was based on the manufacturer’s handbook. The samples were homogenized with Vortex-Genie® 2. Following cell lysis, the supernatant was washed. Deoxyribonucleic acid (DNA) was then extracted. The extracted DNA was purified and precipitated. Following quality control, the DNA underwent sequencing with Illumina® MiSeq® Next Generation Sequencer. The primers were V3-V4 region of 16S rRNA and ITS1 DNA for bacteria and fungi, respectively. The whole sequencing process was performed based on the manufacturer’s protocol.
Bioinformatic analysis
The workflow of the bioinformatic analysis is shown in Fig. 7. We used FLASH v1.2.7 for paired end reads merger. Primer sequences were truncated. USEARCH package was used to filter the reads, calculate the abundance value, cluster operational taxonomic unit (OTU), and filter chimera. We referred to 16s sequence databases from Ribosomal Database Project for annotation. Alpha and beta diversities were analyzed with USEARCH package. Principal Coordinate Analysis (PCoA) was performed with R software (Version 2.15.3).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Luna, P. C. Skin microbiome as years go by. Am. J. Clin. Dermatol. 21, 12–17. https://doi.org/10.1007/s40257-020-00549-5 (2020).
Watanabe, K., Yamada, A., Nishi, Y., Tashiro, Y. & Sakai, K. Host factors that shape the bacterial community structure on scalp hair shaft. Sci. Rep. 11, 17711. https://doi.org/10.1038/s41598-021-96767-w (2021).
Lin, Q. et al. Malassezia and Staphylococcus dominate scalp microbiome for seborrheic dermatitis. Bioprocess Biosyst. Eng. 44, 965–975. https://doi.org/10.1007/s00449-020-02333-5 (2021).
Lousada, M. B. et al. Exploring the human hair follicle microbiome. Br. J. Dermatol. 184, 802–815. https://doi.org/10.1111/bjd.19461 (2021).
Ma, L. et al. Sensitive scalp is associated with excessive sebum and perturbed microbiome. J. Cosmet. Dermatol. 18, 922–928. https://doi.org/10.1111/jocd.12736 (2019).
Rehman, R., Mateen, M., Tripathi, R., Fahs, F. & Mohammad, T. F. Teledermatology etiquette and the hijab: Recommendations for culturally sensitive care. Int. J. Dermatol. https://doi.org/10.1111/ijd.16180 (2022).
Martini, L. A precious chance for muslim hijab women of all the world to keep their hair scalp safe and not to incur pracox alopecia. Our Dermatol. Online 7, 284–287. https://doi.org/10.7241/ourd.20163.76 (2016).
Etnawati, K. et al. The role of Malassezia sp, sebum level and Trans Epidermal Water Loss (TEWL) toward the dandruff severity between hijab and non hijab wearing subjects. J. Med. Sci. (Berkala Ilmu Kedokteran) https://doi.org/10.19106/JMedScie/0050032018011 (2018).
Szczuka, E., Jablonska, L. & Kaznowski, A. Coagulase-negative staphylococci: Pathogenesis, occurrence of antibiotic resistance genes and in vitro effects of antimicrobial agents on biofilm-growing bacteria. J. Med. Microbiol. 65, 1405–1413. https://doi.org/10.1099/jmm.0.000372 (2016).
Kumar, R., Jangir, P. K., Das, J., Taneja, B. & Sharma, R. Genome analysis of staphylococcus capitis TE8 reveals repertoire of antimicrobial peptides and adaptation strategies for growth on human skin. Sci. Rep. 7, 10447. https://doi.org/10.1038/s41598-017-11020-7 (2017).
O’Neill, A. M. et al. Identification of a human skin commensal bacterium that selectively kills cutibacterium acnes. J. Invest. Dermatol. 140, 1619-1628 e1612. https://doi.org/10.1016/j.jid.2019.12.026 (2020).
Soldera, J., Nedel, W. L., Cardoso, P. R. & d’Azevedo, P. A. Bacteremia due to Staphylococcus cohnii ssp. urealyticus caused by infected pressure ulcer: case report and review of the literature. Sao Paulo Med. J. Revista paulista de medicina 131, 59–61. https://doi.org/10.1590/s1516-31802013000100010 (2013).
Ito, Y. et al. Staphylococcus cohnii is a potentially biotherapeutic skin commensal alleviating skin inflammation. Cell Rep. 35, 109052. https://doi.org/10.1016/j.celrep.2021.109052 (2021).
Park, H. K. et al. Characterization of the fungal microbiota (mycobiome) in healthy and dandruff-afflicted human scalps. PLoS One 7, e32847. https://doi.org/10.1371/journal.pone.0032847 (2012).
Zoulba, E. N., Widaty, S., Krisanty, I. A. & Wahid, M. H. Identification of malassezia species and the severity of seborrheic dermatitis on scalp in Dr. Cipto Mangunkusumo Hospital Jakarta. Adv. Sci. Lett. 24, 6649–6652 (2018).
Acknowledgements
We would like to thank Paragon Technology and Innovation Co. Ltd. for their support during the study.
Author information
Authors and Affiliations
Contributions
All authors contribute equally to the study preparation, data collection, data analysis, and writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Widaty, S., Surachmiati, L., Legiawati, L. et al. Scalp microbiome of healthy women wearing hijab compared to those not wearing hijab: a cross-sectional study. Sci Rep 13, 11797 (2023). https://doi.org/10.1038/s41598-023-38903-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38903-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.