Abstract
Allogeneic hematopoietic cell transplantation between female donors and male recipients (female-to-male allo-HCT) is a well-established risk factor for inferior survival outcomes due to a higher incidence of graft-versus-host disease (GVHD). However, a clinical significance of anti-thymocyte globulin (ATG) in the female-to-male allo-HCT has not been elucidated. In this study, we retrospectively evaluated male patients who underwent allo-HCT between 2012 and 2019 in Japan. In the female-to-male allo-HCT cohort (n = 828), the use of ATG was not associated with a decreased risk of GVHD (HR of acute GVHD 0.691 [95% CI: 0.461–1.04], P = 0.074; HR of chronic GVHD 1.06 [95% CI: 0.738–1.52], P = 0.76), but was associated with favorable overall survival (OS) and a decreased risk of non-relapse mortality (NRM) (HR of OS 0.603 [95% CI: 0.400–0.909], P = 0.016; HR of NRM 0.506 [95% CI: 0.300–0.856], P = 0.011). The use of ATG in female-to-male allo-HCT resulted in survival outcomes that were almost equivalent to those in the male-to-male allo-HCT group. Therefore, GVHD prophylaxis with ATG might overcome the inferiority of survival outcomes in female-to-male allo-HCT.
Similar content being viewed by others
Introduction
Graft-versus-host disease (GVHD) is one of the most common complications after allogeneic hematopoietic cell transplantation (allo-HCT) and causes high morbidity and mortality1,2,3. Several efforts have been made to overcome the adverse impact of GVHD on survival outcomes2. In vivo T cell depletion with anti-thymocyte globulin (ATG) is a widely accepted procedure for GVHD prophylaxis. Several previous reports have shown a relationship between ATG and a reduced incidence of GVHD4,5,6,7. However, the immunosuppressive effect of ATG raises a concern about higher incidences of infectious complications and relapse, and the clinical impact of ATG on relapse, infection and overall survival is still a matter of debate.
Allo-HCT between female donors and male recipients (female-to-male allo-HCT) is a well-established risk factor for inferior survival outcomes8,9. Since male recipients have H-Y antigens, which are proteins encoded by the Y-chromosome and thus specific to males, these proteins are potential targets of GVHD in female-to-male allo-HCT, resulting in a higher incidence of chronic GVHD and non-relapse mortality (NRM)10,11. It may be reasonable to try to improve the survival inferiority of female-to-male allo-HCT by intensive GVHD prophylaxis. However, since previous reports have suggested a relationship between H-Y antigens and a graft-versus leukemia (GVL) effect10,12, an escalation of GVHD prophylaxis might induce an increased incidence of relapse in addition to infectious complications. We hypothesized that the use of ATG in female-to-male allo-HCT may contribute to a lower incidence of chronic GVHD and a higher incidence of relapse, and the prognosis in female-to-male allo-HCT may depend on which of these effects is predominant. Therefore, it is important to clarify an adequate GVHD prophylaxis for female-to-male allo-HCT. In this study, we evaluated the impact of ATG on survival outcomes in female-to-male allo-HCT.
Patients and methods
Data source and patient selection
Clinical data were obtained from the Transplant Registry Unified Management Program (TRUMP) of the Japanese Society for Transplantation and Cellular Therapy (JSTCT) and the Japanese Data Center for Hematopoietic Cell Transplantation (JDCHCT)13,14. This retrospective study was approved by the data management committee of JSTCT (approved number: WG20-64) and by the Institutional Review Board of Jichi Medical University Saitama Medical Center (approved number: S21-122), and performed in accordance with the Declaration of Helsinki and its later amendments. Written informed consent was obtained from all participants in this study.
This study included both adult and pediatric male recipients who were diagnosed as a standard risk disease status and who received their first allo-HCT from an unrelated human leukocyte antigen (HLA)-matched (8/8) or 1-locus mismatched (7/8) donor between January 2012 and December 2019 in Japan. Donor sources were limited to bone marrow (BM) or peripheral blood (PB). This study included acute myeloid leukemia (AML) in complete remission (CR 1, CR 2, CR 3-), acute lymphoblastic leukemia (ALL) in complete remission (CR 1, CR 2, CR 3-), myelodysplastic syndrome (MDS), chronic myeloid leukemia (CML) in chronic phase (CP 1, CP 2, CP 3-) and accelerated phase (AP), myeloproliferative neoplasm (MPN), malignant lymphoma (ML) in complete remission (CR 1, CR 2, CR 3-) including adult T cell leukemia/lymphoma (ATL). We excluded patients who were diagnosed with other diseases and for whom information on gender, survival and the last follow-up date were not available.
Definitions
Disease risk index (DRI) was classified according to a previous report15. With regard to cytogenetics of DRI, for AML, t(8;21), inv(16) and t(15;17) were classified as favorable, complex (≥ 4 abnormalities) was classified as adverse, and other karyotypes were classified as intermediate. For MDS, abnormal chromosome 7 and complex karyotype (≥ 4 abnormalities) were classified as adverse and the other karyotypes were considered intermediate. ATL was classified as high risk in DRI. The hematopoietic cell transplantation comorbidity index (HCT-CI) was assessed based on a previous report16. Conditioning regimens were classified according to the criteria from the Center for International Blood and Marrow Transplantation Research17. Briefly, myeloablative conditioning regimen (MAC) was defined as total body irradiation (TBI) > 8 Gy (fractionated) or > 5 Gy (single dose), melphalan > 140 mg/m2, intravenous busulfan > 7.2 mg/kg, and all other regimens were classified as reduced-intensity conditioning (RIC). Chronic GVHD was diagnosed and graded based on standard criteria18.
Statistical analysis
First, survival outcomes were compared between the female-to-male and male-to-male allo-HCT groups to validate the adverse impact of female-to-male allo-HCT in the entire cohort. Second, survival outcomes were compared between patients who received GVHD prophylaxis with and without ATG in the female-to-male allo-HCT cohort. Third, the impact of ATG was similarly analyzed in the male-to-male allo-HCT cohort. Subsequently, the effect of ATG was discussed based on the results in both the female-to-male and male-to-male allo-HCT cohort.
Categorical and continuous variables were compared by Fisher’s exact test and the Mann–Whitney U test, respectively. Overall survival (OS) was estimated by the Kaplan–Meier method and compared by the log-rank test. Cumulative incidences of relapse, NRM, and acute and chronic GVHD were estimated by Gray’s test. Relapse and NRM were treated as competing risks for each other. Death due to any cause was treated as a competing risk for acute and chronic GVHD. To adjust for the effect of early death, which can inappropriately lower the incidence of chronic GVHD, the cumulative incidence of chronic GVHD was evaluated among patients who survived without disease relapse for more than 100 days after allo-HCT. A Cox proportional hazard regression model was used for multivariate analyses of survival outcomes. Our interest of research questions was to confirm the adverse impact of sex-mismatched HCT and to pursue the effect of ATG in the limited cohort of sex-mismatched HCT. There were various confounding factors which affects donor selection and use of ATG. To address the potential confounding factors and ensure accurate results, multivariate analysis was performed in all survival analyses, regardless of the results of univariate analyses. Thus, the hazard ratios (HR) of types of sex-mismatched HCT or ATG were adjusted for the following pre-transplant clinical factors: age, disease type, DRI, HCT-CI, donor type and source, conditioning regimen, GVHD prophylaxis and allo-HCT year. A two-tailed P value < 0.05 was considered to be statistically significant. All analyses in this study were performed with EZR (http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmedEN.html, Jichi Medical University Saitama Medical Center, Saitama, Japan), which is a graphical user interface for R version 3.6.3 (The Foundation for Statistical Computing, Vienna, Austria)19.
Results
Patient characteristics
According to the eligibility criteria, 828 female-to-male allo-HCT patients and 2431 male-to-male allo-HCT patients were identified. The median follow-up duration for survivors was 39.2 months (range, 0.1–105.5) in the entire cohort, and was shorter in the ATG group (26.2 months in the ATG group vs 41.2 months in the non-ATG group, P < 0.001). The median age was 51 years (range, 0–75) in the female-to-male cohort, and 52 years (range, 0–74) in the male-to-male cohort. Out of the patients for whom we had information regarding ATG (n = 413), thymoglobulin (ATG-T, Sanofi, Paris, France) was administered to 408 patients, while anti-human T lymphocyte immunoglobulin (ATG-F, Fresenius Biotech GmbH, Munich, Germany) was administered to 4 patients. The information on ATG administration was unavailable for one patient. The median dose of ATG-T was 2.5 mg/kg (inter quartile range: 1.5–2.5). Among patients whose information about chronic GVHD severity according to NIH criteria20 was available (n = 2325), the ATG group tended to include fewer patients who were suffered from severe chronic GVHD compared with the non-ATG group (2 cases [0.6%] vs 45 cases [2.3%], P = 0.055). Patient characteristics are shown in Supplemental Table S1. The female-to-male cohort included more patients who were younger than 16 years old (79 cases [9.5%] vs 105 cases [4.3%], P < 0.001). The other characteristics were almost equivalent between these cohorts.
Confirmation of the adverse impact of female-to-male allo-HCT on survival outcomes
When survival outcomes were simply compared between the female-to-male and male-to-male allo-HCT groups, OS tended to be inferior to that for male-to-male allo-HCT (5-y OS 55.2% vs 59.4%, P = 0.11), and NRM and chronic GVHD of female-to-male allo-HCT tended to be higher than those of male-to-male allo-HCT (5-y NRM 28.2% vs 24.2%, P = 0.066; 5-y cGVHD 48.0 vs 42.8%, P = 0.059). Multivariate analyses revealed that female-to-male allo-HCT was significantly associated with the risk of inferior OS (HR 1.16 [95% confidence interval: 1.02–1.33], P = 0.027), and increased NRM (HR 1.20 [95% CI: 1.02–1.42], P = 0.030) and chronic GVHD (HR 1.19 [95% CI: 1.04–1.36], P = 0.010). On the other hand, the cumulative incidence of relapse (CIR) in female-to-male allo-HCT was not different from that in male-to-male allo-HCT (5-y CIR 19.3% vs 19.7%, P = 0.71; HR 0.996 [95% CI: 0.821–1.21], P = 0.97) (Supplemental Table S2). Regarding acute GVHD, grade II–IV acute GVHD (33.9% vs 40.8%, P < 0.001) seemed to be less common in female-to-male allo-HCT due to the greater mortality before the onset of acute GVHD in the current female-to-male allo-HCT cohort (27.8% vs 21.5%, P < 0.001).
Clinical impact of ATG in the female-to-male allo-HCT cohort
In the female-to-male allo-HCT cohort (n = 828), 117 patients received ATG as GVHD prophylaxis. The ATG group included more patients who underwent allo-HCT from an HLA mismatched donor, more patients who used PB as a donor source, more patients who received RIC as a conditioning regimen, and more patients who underwent allo-HCT after 2015 (Table 1).
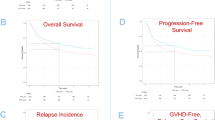
The ATG group showed favorable OS compared with the non-ATG group (5-y OS 63.8% vs 53.9%, P = 0.035, Fig. 1a). A multivariate analysis also demonstrated that the use of ATG was significantly associated with superior OS (HR 0.603 [95% CI: 0.400–0.909], P = 0.016) (Fig. 2, Supplemental Table S3). Similarly, NRM tended to be lower in the ATG group (5-y NRM 25.3% vs 28.9%, P = 0.11, Fig. 1b), although the difference was not significant. However, multivariate analysis revealed that the use of ATG was significantly associated with a reduced risk of NRM (HR 0.506 [95% CI: 0.300–0.856], P = 0.011). There was no significant difference in CIR between the ATG and non-ATG groups (14.8% vs 19.9%, P = 0.38, Fig. 1c), and a multivariate analysis also showed no significant relationship between the use of ATG and CIR (HR 0.760 [95% CI: 0.429–1.34], P = 0.34). Grade II–IV acute GVHD tended to be less common in the ATG group (26.7% vs 35.0%, P = 0.067, Fig. 1d), and the use of ATG seemed to be associated with a lower incidence of grade II–IV acute GVHD, but this difference was not statistically significant (HR 0.691 [95% CI: 0.461–1.04], P = 0.074). The cumulative incidence of chronic GVHD was equivalent between the ATG and non-ATG groups (5-y cumulative incidence of chronic GVHD 47.2% vs 48.2%, P = 0.99, Fig. 1e), and ATG was not associated with chronic GVHD in a multivariate analysis (HR 1.06 [95% CI: 0.738–1.52], P = 0.76).
Survival outcomes according to administration of anti-thymocyte globulin in the female-to-male cohort (a) Overall survival (b) Cumulative incidence of relapse (c) Non-relapse mortality (d) Cumulative incidence of acute graft-versus-host disease (e) Cumulative incidence of chronic graft-versus-host disease.
Cause of death in the female-to-male allo-HCT cohort
The cause of death was mainly infection and disease progression (Fig. 3). The ATG group showed a significantly lower incidence of death due to progression and non-infectious pulmonary complications (progression 5 of 117 cases [4.3%] vs 79 of 711 cases [11.1%], P = 0.020; non-infectious pulmonary complications 0 of 117 cases [0.0%] vs 30 of 711 cases [4.2%], P = 0.015) (Supplemental Table S4). Although the number of deaths due GVHD was lower in the ATG group, there was no significant difference between the groups (1 of 117 cases [0.9%] vs 21 of 711 cases [3.0%], P = 0.35). The other causes of death were comparable between the groups.
Clinical impact of ATG in the male-to-male allo-HCT cohort
ATG was administered to 314 patients in the male-to-male cohort (n = 2431). The ATG group included more patients who were younger than 16 years old, more patients who underwent allo-HCT from an HLA mismatched donor, more patients who used PB as a donor source, more patients who received RIC as a conditioning regimen and more patients who underwent allo-HCT after 2015 (Table 1).
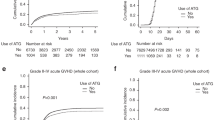
OS was favorable in the ATG group (5-y OS 64.1% vs 58.8%, P = 0.039, Fig. 4a; HR of ATG 0.747 [95% CI: 0.587–0.951], P = 0.018, Fig. 2, Supplemental Table S5). The ATG group tended to show lower NRM (5-y NRM 18.9% vs 24.9%, P = 0.051, Fig. 4b), and ATG was significantly associated with a reduced risk of NRM (HR 0.680 [95% CI: 0.494–0.937], P = 0.018). CIR was comparable between the ATG and non-ATG groups (5-y CIR 21.3% vs 19.4%, P = 0.65, Fig. 4c; HR 1.05 [95% CI: 0.775–1.41], P = 0.77). The cumulative incidence of grade II–IV acute GVHD was significantly lower in the ATG group (34.2% vs 41.8%, P = 0.0065, Fig. 4d), and the use of ATG was associated with a reduced risk of grade II–IV acute GVHD (HR 0.721 [95% CI: 0.581–0.895], P = 0.0031).The ATG group tended to show a lower incidence of chronic GVHD (5-y cumulative incidence of chronic GVHD 35.7% vs 43.8%, P = 0.059, Fig. 4e), and this tendency was also observed in a multivariate analysis (HR 0.802 [95% CI: 0.635–1.01], P = 0.065).
Survival outcomes according to administration of anti-thymocyte globulin in the male-to-male cohort (a) Overall survival (b) Cumulative incidence of relapse (c) Non-relapse mortality (d) Cumulative incidence of acute graft-versus-host disease (e) Cumulative incidence of chronic graft-versus-host disease.
In summary, the impact of ATG seemed to differ somewhat between the female-to-male and male-to-male allo-HCT groups (Fig. 2). The use ATG tended to be associated with a decreased risk of chronic GVHD only in the male-to-male allo-HCT cohort, whereas the impact of ATG on other survival outcomes was almost equivalent between the female-to-male and male-to-male allo-HCT cohorts.
Survival outcomes stratified according to sex-mismatch and ATG
Additionally, survival analyses were performed in the entire cohort according to the combination of sex-mismatch and ATG. When the female-to-male/ATG group was treated as a reference, the female-to-male/non-ATG group showed an increased risk of poor OS (HR 1.49 [95% CI: 1.03–2.18], P = 0.036), whereas the risk of overall mortality was similar to those in both the male-to-male/ATG and male-to-male/non-ATG groups (Supplemental Table S6). An increased risk of NRM also tended to be observed in the female-to-male/non-ATG group (HR 1.51 [95% CI: 0.940–2.42], P = 0.089), and the other groups showed a comparable risk of NRM. The risk of chronic GVHD was equivalent among these groups.
Discussion
In this study, the clinical significance of ATG was evaluated in female-to-male and male-to-male allo-HCT cohorts. In the female-to-male cohort, ATG was significantly associated with favorable OS. Although ATG was not associated with reduced incidences of acute and chronic GVHD in the female-to-male cohort, there was a significant relationship between ATG and favorable NRM. In the male-to-male allo-HCT cohort, ATG was associated with OS and NRM, and also tended to be associated with chronic GVHD.
The sex-mismatched combination of a male recipient and a female donor is recognized as a risk factor for an inferior prognosis in allo-HCT. An unfavorable effect of female-to-male allo-HCT has been reported by several studies since 19898,9,21,22. The sex-mismatched combination is also included in the EBMT score as an unfavorable risk factor23. Female-to-male allo-HCT is generally associated with increased incidences of NRM and chronic GVHD. On the other hand, some previous studies showed a reduced incidence of relapse which suggested the existence of a GVL effect due to sex-mismatch8,24,25,26. In fact, we previously reported that male recipients with deletion of Y-chromosome who underwent allo-HCT from a female donor showed a higher incidence of relapse12, suggesting attenuation of the GVL effect due to the loss of Y-chromosome. Thus, we initially hypothesized that the addition of ATG may contribute to a lower incidence of chronic GVHD and a higher incidence of relapse in female-to-male allo-HCT.
Based on the hypothesis that female-to-male allo-HCT gives inferior survival outcomes due to a higher incidence of chronic GVHD, it might be reasonable to intensify GVHD prophylaxis in female-to-male allo-HCT. In vivo T cell depletion with ATG is a widely accepted strategy for GVHD prophylaxis. Several randomized control trials have shown that GVHD prophylaxis with ATG was associated with a decreased risk of GVHD and NRM,4,5,6 and various studies have reported the clinical significance of GVHD prophylaxis with ATG7,27,28,29,30. However, the impact of ATG on OS remains controversial, since the intensification of GVHD prophylaxis with ATG was associated with an increased risk of infectious complications such as cytomegalovirus and Epstein-Barr virus reactivation31. Furthermore, intensive immunosuppression with ATG raises a concern about an increase of relapse, although a significant relationship between ATG and relapse has not been elucidated. The current study revealed an improvement of OS and NRM with ATG in female-to-male allo-HCT, even though ATG did not improve the incidence of chronic GVHD.
One potential explanation for the discrepancy between chronic GVHD and OS/NRM might be differences in severity and response to GVHD treatment. Severe or refractory GVHD is generally associated with an increased risk of mortality. Although several studies failed to show the direct adverse effect of chronic GVHD on NRM32,33,34, chronic GVHD was associated with inferior activities of daily living (ADL) and quality of life35,36,37, and severe chronic GVHD is more likely to impair ADL35. Since lower ADL is a risk factor for NRM after allo-HCT38,39 and all-cause mortality in various situation40,41, reducing the risk of severe chronic GVHD could potentially improve NRM. The current study found that the ATG group in the entire cohort tended to include fewer patients with severe chronic GVHD, although the severity in the female-to-male and male-to-male allo-HCT cohort could not be analyzed separately due to small sample size. The lower rate of severe chronic GVHD in the ATG group suggests that the ATG may reduce NRM by alleviating the severity of chronic GVHD even if it does not decrease the incidence of chronic GVHD. Additionally, the ATG group in the female-to-male allo-HCT cohort included fewer patients who died due to non-infectious pulmonary complication which suggests that ATG might reduce the incidence of fatal allogeneic immune reaction. Moreover, CIR was equivalent between the ATG and non-ATG groups in the female-to-male allo-HCT cohort, and ATG was not adversely associated with relapse. Anyway, the true reason for the discrepancy of the ATG impact between GVHD and NRM remains to be elucidated, and further investigation is required for any conclusion.
According to the result of the additional analysis based on a combination of sex-mismatch and ATG, the administration of ATG might reduce the adverse impact of female-to-male allo-HCT and improve OS and NRM, resulting in outcomes comparable to those with male-to-male allo-HCT. For the further improvement of survival outcomes, additional GVHD prophylaxis might be required in female-to-male allo-HCT. A promising approach to GVHD prophylaxis is posttransplant cyclophosphamide (PTCY). PTCY was reported as a highly effective GVHD prophylaxis in previous reports42,43,44. Several studies have shown that PTCY provides superior progression-free survival and GVHD/relapse-free survival compared with ATG45,46. Additionally, there have been several attempts to develop a combination therapy with ATG and PTCY47,48. Although we should be careful regarding a risk of infection and relapse, further investigation is also warranted to elucidate the clinical significance of PTCY in female-to-male allo-HCT.
The current study has several limitations due to its retrospective nature. First, the number of patients who underwent allo-HCT with ATG has recently increased. Therefore, the median follow-up duration in the ATG group was slightly shorter than that in the non-ATG group. A longer follow-up might reveal additional favorable and/or adverse impacts of ATG. Second, due to the limited sample size, we could not perform various subgroup analyses according to HLA-match/mismatch, donor source or disease type. Third, although the background condition was compensated by DRI and HCT-CI, the use of ATG might be avoided in patients who were at high risk of disease relapse or in poor general condition.
In conclusion, GVHD prophylaxis with ATG in female-to-male allo-HCT was significantly associated with superior OS and a reduced risk of NRM, despite no significant relationship with chronic GVHD. The use of ATG in female-to-male allo-HCT resulted in survival outcomes that were almost the same as those in the male-to-male allo-HCT group. GVHD prophylaxis with ATG might overcome the inferior survival outcomes in female-to-male allo-HCT.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Ferrara, J. L. M. & Chaudhry, M. S. GVHD: Biology matters. Blood Adv. 2, 3411–3417. https://doi.org/10.1182/bloodadvances.2018020214 (2018).
Hamilton, B. K. Current approaches to prevent and treat GVHD after allogeneic stem cell transplantation. Hematol. Am. Soc. Hematol. Educ. Prog. 228–235, 2018. https://doi.org/10.1182/asheducation-2018.1.228 (2018).
Cutler, C. S., Koreth, J. & Ritz, J. Mechanistic approaches for the prevention and treatment of chronic GVHD. Blood 129, 22–29. https://doi.org/10.1182/blood-2016-08-686659 (2017).
Kröger, N. et al. Antilymphocyte globulin for prevention of chronic graft-versus-host disease. N. Engl. J. Med. 374, 43–53. https://doi.org/10.1056/NEJMoa1506002 (2016).
Soiffer, R. J. et al. Prospective, randomized, double-blind, phase III clinical trial of anti-T-lymphocyte globulin to assess impact on chronic graft-versus-host disease-free survival in patients undergoing HLA-matched unrelated myeloablative hematopoietic cell transplantation. J. Clin. Oncol. 35, 4003–4011. https://doi.org/10.1200/jco.2017.75.8177 (2017).
Chang, Y. J. et al. Antithymocyte globulin for matched sibling donor transplantation in patients with hematologic malignancies: A multicenter, open-label, randomized controlled study. J. Clin. Oncol. 38, 3367–3376. https://doi.org/10.1200/jco.20.00150 (2020).
Fuji, S. et al. Disease-specific impact of anti-thymocyte globulin in allogeneic hematopoietic cell transplantation: a nationwide retrospective study on behalf of the JSTCT, transplant complications working group. Bone Marrow Transpl. 57, 479–486. https://doi.org/10.1038/s41409-022-01569-x (2022).
Nakasone, H. et al. Risks and benefits of sex-mismatched hematopoietic cell transplantation differ according to conditioning strategy. Haematologica 100, 1477–1485. https://doi.org/10.3324/haematol.2015.125294 (2015).
Nannya, Y. et al. The negative impact of female donor/male recipient combination in allogeneic hematopoietic stem cell transplantation depends on disease risk. Transpl. Int. 24, 469–476. https://doi.org/10.1111/j.1432-2277.2011.01229.x (2011).
Nakasone, H. et al. Allogeneic HY antibodies detected 3 months after female-to-male HCT predict chronic GVHD and nonrelapse mortality in humans. Blood 125, 3193–3201. https://doi.org/10.1182/blood-2014-11-613323 (2015).
Paul, J. et al. A confirmation of chronic graft-versus-host disease prediction using allogeneic HY antibodies following sex-mismatched hematopoietic cell transplantation. Haematologica 104, e314–e317. https://doi.org/10.3324/haematol.2018.199646 (2019).
Tamaki, M. et al. Deletion of Y chromosome before allogeneic hematopoietic stem cell transplantation in male recipients with female donors. Blood Adv. 6, 1895–1903. https://doi.org/10.1182/bloodadvances.2021006456 (2022).
Atsuta, Y. Introduction of transplant registry unified management program 2 (TRUMP2): Scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int. J. Hematol. 103, 3–10. https://doi.org/10.1007/s12185-015-1894-x (2016).
Kanda, J. Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int. J. Hematol. 103, 11–19. https://doi.org/10.1007/s12185-015-1907-9 (2016).
Armand, P. et al. Validation and refinement of the disease risk index for allogeneic stem cell transplantation. Blood 123, 3664–3671. https://doi.org/10.1182/blood-2014-01-552984 (2014).
Sorror, M. L. et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: A new tool for risk assessment before allogeneic HCT. Blood 106, 2912–2919. https://doi.org/10.1182/blood-2005-05-2004 (2005).
Giralt, S. et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol. Blood Marrow Transpl. 15, 367–369. https://doi.org/10.1016/j.bbmt.2008.12.497 (2009).
Sullivan, K. M. et al. Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin. Hematol. 28, 250–259 (1991).
Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transpl. 48, 452–458. https://doi.org/10.1038/bmt.2012.244 (2013).
Schneider, S. et al. Erratum to: "Reduced-intensity conditioning combined with (188)rhenium radioimmunotherapy before allogeneic hematopoietic stem cell transplantation in elderly patients with acute myeloid leukemia: The role of in vivo T cell depletion. Biol. Blood Marrow Transpl. 23, 533. https://doi.org/10.1016/j.bbmt.2016.12.626 (2017).
Gahrton, G. Risk assessment in haematopoietic stem cell transplantation: Impact of donor-recipient sex combination in allogeneic transplantation. Best Pract. Res. Clin. Haematol. 20, 219–229. https://doi.org/10.1016/j.beha.2006.09.007 (2007).
Schetelig, J. et al. Risk factors for treatment failure after allogeneic transplantation of patients with CLL: A report from the European Society for Blood and Marrow Transplantation. Bone Marrow Transpl. 52, 552–560. https://doi.org/10.1038/bmt.2016.329 (2017).
Gratwohl, A. The EBMT risk score. Bone Marrow Transpl. 47, 749–756. https://doi.org/10.1038/bmt.2011.110 (2012).
Randolph, S. S., Gooley, T. A., Warren, E. H., Appelbaum, F. R. & Riddell, S. R. Female donors contribute to a selective graft-versus-leukemia effect in male recipients of HLA-matched, related hematopoietic stem cell transplants. Blood 103, 347–352. https://doi.org/10.1182/blood-2003-07-2603 (2004).
Gratwohl, A. et al. Female donors influence transplant-related mortality and relapse incidence in male recipients of sibling blood and marrow transplants. Hematol. J. 2, 363–370. https://doi.org/10.1038/sj.thj.6200117 (2001).
Gahrton, G. et al. The impact of donor gender on outcome of allogeneic hematopoietic stem cell transplantation for multiple myeloma: reduced relapse risk in female to male transplants. Bone Marrow Transpl. 35, 609–617. https://doi.org/10.1038/sj.bmt.1704861 (2005).
Shiratori, S. et al. Low-dose anti-thymocyte globulin for GVHD prophylaxis in HLA-matched allogeneic peripheral blood stem cell transplantation. Bone Marrow Transpl. 56, 129–136. https://doi.org/10.1038/s41409-020-0985-3 (2021).
Shiratori, S. et al. Graft-versus-host disease prophylaxis using low-dose antithymocyte globulin in peripheral blood stem cell transplantation-A matched-pair analysis. Transpl. Cell Ther. 27(995), e991-995.e996. https://doi.org/10.1016/j.jtct.2021.08.029 (2021).
Arai, Y., Jo, T., Matsui, H., Kondo, T. & Takaori-Kondo, A. Efficacy of antithymocyte globulin for allogeneic hematopoietic cell transplantation: A systematic review and meta-analysis. Leuk Lymphoma 58, 1840–1848. https://doi.org/10.1080/10428194.2016.1266624 (2017).
Ratanatharathorn, V. et al. Low-dose antithymocyte globulin enhanced the efficacy of tacrolimus and mycophenolate for GVHD prophylaxis in recipients of unrelated SCT. Bone Marrow Transpl. 50, 106–112. https://doi.org/10.1038/bmt.2014.203 (2015).
Kang, H. M., Kim, S. K., Lee, J. W., Chung, N. G. & Cho, B. Efficacy of low dose antithymocyte globulin on overall survival, relapse rate, and infectious complications following allogeneic peripheral blood stem cell transplantation for leukemia in children. Bone Marrow Transpl. 56, 890–899. https://doi.org/10.1038/s41409-020-01121-9 (2021).
Ohwada, C. et al. A prospective, longitudinal observation of the incidence, treatment, and survival of late acute and chronic graft-versus-host disease by national institutes of health criteria in a Japanese cohort. Biol. Blood Marrow Transpl. 26, 162–170. https://doi.org/10.1016/j.bbmt.2019.09.016 (2020).
Ringdén, O. et al. Effect of acute and chronic GVHD on relapse and survival after reduced-intensity conditioning allogeneic transplantation for myeloma. Bone Marrow Transpl. 47, 831–837. https://doi.org/10.1038/bmt.2011.192 (2012).
Miflin, G. et al. An analysis of the effect of chronic GvHD on relapse and survival following allogeneic PBSC transplantation. Cytotherapy 2, 423–428. https://doi.org/10.1080/146532400539369 (2000).
Yu, J. et al. Patient-reported symptom burden and impact on daily activities in chronic graft-versus-host disease. Cancer Med. 12, 3623–3633. https://doi.org/10.1002/cam4.5209 (2023).
Inamoto, Y. et al. Ocular graft-versus-host disease after hematopoietic cell transplantation: Expert review from the late effects and quality of life working committee of the CIBMTR and transplant complications working party of the EBMT. Bone Marrow Transpl. 54, 662–673. https://doi.org/10.1038/s41409-018-0340-0 (2019).
Pidala, J. et al. Patient-reported quality of life is associated with severity of chronic graft-versus-host disease as measured by NIH criteria: Report on baseline data from the Chronic GVHD Consortium. Blood 117, 4651–4657. https://doi.org/10.1182/blood-2010-11-319509 (2011).
Lin, R. J. et al. Burden and impact of multifactorial geriatric syndromes in allogeneic hematopoietic cell transplantation for older adults. Blood Adv. 3, 12–20. https://doi.org/10.1182/bloodadvances.2018028241 (2019).
Salas, M. Q. et al. Pilot prospective study of frailty and functionality in routine clinical assessment in allogeneic hematopoietic cell transplantation. Bone Marrow Transpl. 56, 60–69. https://doi.org/10.1038/s41409-020-0979-1 (2021).
O’Súilleabháin, P. S., Gallagher, S. & Steptoe, A. Loneliness, living alone, and all-cause mortality: The role of emotional and social loneliness in the elderly during 19 years of follow-up. Psychosom. Med. 81, 521–526. https://doi.org/10.1097/psy.0000000000000710 (2019).
Takata, Y. et al. Activities of daily living dependency and disease-specific mortality during 12-year follow-up in an 80-year-old population. Aging Clin. Exp. Res. 25, 193–201. https://doi.org/10.1007/s40520-013-0029-6 (2013).
Luznik, L. et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol. Blood Marrow Transpl. 14, 641–650. https://doi.org/10.1016/j.bbmt.2008.03.005 (2008).
Kanakry, C. G. et al. Multi-institutional study of post-transplantation cyclophosphamide as single-agent graft-versus-host disease prophylaxis after allogeneic bone marrow transplantation using myeloablative busulfan and fludarabine conditioning. J. Clin. Oncol. 32, 3497–3505. https://doi.org/10.1200/jco.2013.54.0625 (2014).
Mielcarek, M. et al. Posttransplantation cyclophosphamide for prevention of graft-versus-host disease after HLA-matched mobilized blood cell transplantation. Blood 127, 1502–1508. https://doi.org/10.1182/blood-2015-10-672071 (2016).
Nykolyszyn, C. et al. Posttransplantation cyclophosphamide vs. antithymocyte globulin as GVHD prophylaxis for mismatched unrelated hematopoietic stem cell transplantation. Bone Marrow Transpl. 55, 349–355. https://doi.org/10.1038/s41409-019-0682-2 (2020).
Battipaglia, G. et al. Posttransplant cyclophosphamide vs antithymocyte globulin in HLA-mismatched unrelated donor transplantation. Blood 134, 892–899. https://doi.org/10.1182/blood.2019000487 (2019).
Law, A. D. et al. Reduced-intensity conditioning and dual T lymphocyte suppression with antithymocyte globulin and post-transplant cyclophosphamide as graft-versus-host disease prophylaxis in haploidentical hematopoietic stem cell transplants for hematological malignancies. Biol. Blood Marrow Transpl. 24, 2259–2264. https://doi.org/10.1016/j.bbmt.2018.07.008 (2018).
Sun, X. et al. Low-dose antithymocyte globulin plus low-dose posttransplant cyclophosphamide combined with cyclosporine and mycophenolate mofetil for prevention of graft-versus-host disease after HLA-matched unrelated donor peripheral blood stem cell transplantation. Bone Marrow Transpl. 56, 2423–2431. https://doi.org/10.1038/s41409-021-01358-y (2021).
Acknowledgements
The authors are grateful for the work of all of the physicians and data managers at the centers that contributed valuable data on transplantation to the JSTCT. We would also like to thank all of the members of the Transplant Registry Unified Management committees at JSTCT for their dedicated data management. M. Tamaki received a grant for JMU Graduate Student Start-Up Award and H.N. received a grant for JSPS KAKENHI (JP21K07070).
Author information
Authors and Affiliations
Contributions
M.T. and H.N. conceived the original idea. M.T. designed the study, analyzed data, and wrote the manuscript. Y. Akahoshi., M.A., M.Y. and K.Y. advised on methods and wrote the manuscript. S.K., S.W.K., Y.O., S.I.F., S.K., K.I.M., M.S. and Y. K. collected data and revised the manuscript. M.O, Y. K., and T.F. collected data, revised the manuscript, and were responsible for data management at JSTCT. Y. A. managed the unified registry database and revised the manuscript. H.N. designed the study, advised on the methods, analyzed data, wrote and revised the manuscript, and was responsible for this project of JSTCT Transplant Complications Working Group. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
Y. Akashoshi received a grant for the Japan Society for the Promotion of Science Postdoctoral Fellowship for Research Abroad. Y.M. received honoraria from Abbvie. SI.F. received honoraria from Astellas Pharma, Chugai Pharmaceutical, Kyowa Kirin, Nippon Shinyaku, Novartis Pharma, Pfizer and Sanofi. S.K. received honoraria from Sanofi. M.S. received honoraria from Chugai Pharmaceutical, Pfizer, Astellas Pharma, Nippon Shinyaku, Ono Pharmaceutical, MSD, Bristol-Myers Squibb, Kyowa Kirin, Asahi Kasei Pharma, Novartis Pharma, Eisai, Otsuka Pharmaceutical, Daimippon Sumitomo Pharmaceutical, Sanofi, Takeda Pharmaceutical, Celgene, Mochida Pharmaceutical, Shire, Mundi Pharma, Abbvie, CSL Behring, SymBio, Janssen Pharmaceutical, Astra Zeneca, Daiichi Sankyo Pharmaceutical and Glaxo Smith Kline. Y.Atsuta. received honoraria from Novartis Pharma, Kyowa Kirin, Abbvie, Astellas Pharma, Mochida Pharmaceutical and Meiji Seika Pharma. H.N. received honoraria from Takeda Pharmaceutical, Sanofi, Otsuka Pharmaceutical, Bristol-Myers Squibb, Celgene, Pfizer, Novartis Pharma, Janssen Pharmaceutical, Eisai, Chugai Pharmaceutical and Nippon Shinyaku. The remaining authors declare no competing financial interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tamaki, M., Akahoshi, Y., Ashizawa, M. et al. Impact of anti-thymocyte globulin on survival outcomes in female-to-male allogeneic hematopoietic stem cell transplantation. Sci Rep 13, 7166 (2023). https://doi.org/10.1038/s41598-023-34442-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34442-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.