Abstract
Fibromyalgia is a heterogenous primary pain syndrome whose severity has been associated with descending pain modulatory system (DPMS) function and functional connectivity (FC) between pain processing areas. The brain-derived neurotrophic factor (BDNF) Val66Met single nucleotide polymorphism has been linked to vulnerability to chronic pain. In this cross-sectional imaging genetics study, we investigated fibromyalgia, the relationship between BDNF Val66Met heterozygous genotypes (Val/Met), and the functional connectivity (FC) response pattern to acute pain stimulus in the motor (MC) and prefrontal (PFC) cortex assessed by near-infrared spectroscopy (fNIRS) before and after a cold pressor test utilizing water (0–1 °C). Also, we assessed the relationship between this genotype with the DPMS function and quality of life. We included 42 women (Val/Val = 30; Val/Met = 12) with fibromyalgia, ages 18–65. The MANCOVA comparing Val/Met to Val/Val genotypes showed higher ΔFC between left(l)-PFC—l-MC (β = 0.357, p = 0.048), l-PFC—right(r)-PFC (β = 0.249, p = 0.012), l-PFC—r-MC (β = 0.226, p = 0.022), and l-MC—r-PFC (β = 0.260, p = 0.016). Val/Met genotypes showed higher efficiency of the DPMS and lower disability due to pain. Here we show that fibromyalgia patients carrying the Val/Met BDNF genotype presented an increased ΔFC across MC and PFC in response to acute pain associated with differences in acute pain perception and fibromyalgia symptoms.
Similar content being viewed by others
Introduction
Fibromyalgia (FM) is a chronic primary pain syndrome defined by widespread pain1 associated with fatigue, diffuse tenderness, hyperalgesia, sleep disorders, cognitive and mood difficulties, as well as psychological and psychiatric disorders2. It is a condition more prevalent in women than men3, affecting from 0.4 to 9.3% of the population worldwide4. Additionally, central sensitization (CS) seems to play a major role in FM pathology in as much as the pain hypersensitivity likely results from central nervous system (CNS) amplification of painful states due to higher pain facilitation over inhibition2,5. These central mechanisms related to CS may also explain the occurrence of cognitive, behavioral, and emotional symptoms in FM and its significant coexistence with mental illness2,5. Nevertheless, establishing objective biomarkers for FM remains an elusive task.
Many attempts to tackle the heterogeneity and non-specificity of FM manifestations have been made by describing this complex disease in terms of its subgroups, which vary in type and degree of physical and cognitive-affective symptoms6. The descending pain modulatory system (DPMS) facilitates or inhibits pain, comprising cortical and subcortical CNS regions such as the ventrolateral periaqueductal grey, rostroventral medulla, and anterior cingulate cortex, among other regions, with significant involvement of the prefrontal cortex (PFC) and motor cortex (MC)7,8. We previously reported that the dysfunction of the DPMS in women with FM was associated with higher functional connectivity (FC) between the left MC and bilateral PFC assessed by functional near-infrared spectroscopy (fNIRS)9. Higher severity of FM symptoms has been associated with dysfunction of the DPMS10, the latter assessed by a standardized quantitative psychophysical protocol known as the conditioned pain modulation (CPM) test7,10.
The relationship between PFC and MC with endogenous pain modulation remains an active area of research, with conflicting evidence for structure, functional, and organization changes in the primary motor cortex in chronic pain11. Both the PFC and the MC are therapeutic targets for non-invasive brain stimulation (NIBS), apparently resulting in the top-down modulation of the respectively emotional12 and sensory-discriminative components of pain perception11,12,13,14. PFC dysfunction in chronic pain is associated with changes in neurotransmitters, gene expression, and neuroinflammation and with alterations in structure, activity, and connectivity during acute and chronic pain15. Also, left PFC activation assessed by fNIRS after thermal stimuli seem to be a sensitive marker of FM patients with more severe clinical symptoms16.
Neuroplasticity is a fundamental biological process for CS, while the brain-derived neurotrophic factor (BDNF) is a candidate gene with a critical impact in regulating synaptic plasticity in human brains5,17. A single nucleotide polymorphism (SNP) in the BDNF gene (c.196G > A, dbSNP: rs6265) causes a valine to methionine substitution at amino acid residue 66 in the BDNF prodomain, which has been correlated to reduced activity-dependent BDNF-secretion18. The Val66Met polymorphism seems to moderate the relationship between stress and depression19, whereas Val66Met carriers with primary dysmenorrhea exhibited a diverse FC expression within the DPMS assessed by functional magnetic resonance imaging20. Finally, increased BDNF serum concentration in FM has been shown to positively correlate with a lower pain pressure threshold21 and the dysfunction of the DPMS10. Therefore, the BDNF may be an intermediate between the DPMS dysfunction and the emergent phenotypes characterized by CS and chronic pain, possibly underlying the functional pattern between cortical areas for pain processing and perception.
Regarding the fNIRS, it is particularly suitable for investigating cortical activation and assessing the hemodynamic response related to the coupling between transient neuronal activation and subsequent cerebral blood flow. Consequently, it is adequate for exploring the changes in functional cortical patterns associated with chronic and acute pain. It is not as expensive as fMRI, being amenable and versatile to interactive paradigms and presenting a better temporal resolution than fMRI22,23.
Based on the facts mentioned above, it is reasonable to test the hypothesis that FM patients with different genotypes of the BDNF Val66Met polymorphism present distinct cortical processing in response to acute pain indexed by changes in functional connectivity (ΔFC) parameters and that this is associated with DPMS efficiency and quality of life due to pain. For this reason, this imaging genetics and exploratory study assessed the relationship between BDNF Val66Met genotypes and change in response to a cold pressor test in FC set by fNIRS in the MC and PFC cortex (primary outcome). Also, we evaluated the relationship between the BDNF Val66Met genotype with the DPMS and the impact of symptoms on quality of life due to fibromyalgia (secondary outcomes).
Materials and methods
Procedure and participants
The Institutional Review Board approved this cross-sectional study under the number 2017–0329 of the Hospital de Clínicas de Porto Alegre (HCPA), Brazil, and registered in the Certificate of Presentation of Ethical Appreciation (CAAE registry No. 72793617.4.0000.5327), according to the Declaration of Helsinki. The protocol was developed following the Strengthening Reporting of Observational Studies in Epidemiology Checklist (STROBE). All participants provided written informed consent before their inclusion. The study enrollment period ranged from January 2018 to January 2021.
Participant recruitment
A convenient sample of forty-two females aged 18–65 years, right-handed, and diagnosed with FM were enrolled from the outpatients' chronic pain wards of the HCPA, Porto Alegre, Brazil, and also after digital media divulgation. FM was defined according to the 2016 diagnosis criteria of the American College of Rheumatology (ACR)24. The ACR score comprises two scales: the widespread pain index (WPI) and symptom severity score (SSS). Criteria were defined as: (i) WPI ≥ 7 and SSS ≥ 5 OR WPI 4–6 and SSS ≥ 9. (ii) Generalized pain: pain in 4/5 regions. (iii) Presence of symptoms ≥ three months. (iv) The FM diagnosis is irrespective of other conditions. ACR score evaluation was applied by physicians with more than ten years of experience in pain care. Patients had to present active clinically significant symptoms, so they should present daily disability for the routine activities due to FM during the three months preceding the enrollment. They needed to report a score of at least 50 mm on the 0–100 mm visual analog scale (VAS 0–100 mm) for the average day in the last three months. All examiners and patients were fluent in Portuguese. Only female patients were included due to the significantly higher prevalence of FM in women than in men3.
Subjects were excluded if they presented a positive history of rheumatoid arthritis, lupus, autoimmune disease, neurological or oncological disease, uncompensated clinical disease (e.g., ischemic heart disease, chronic kidney disease, and hepatic disease.). They were also excluded if they had used cannabis or recreational psychotropic drugs in the last six months.
Instruments and assessment outcomes
Dependent and independent variables
The dependent variables were the difference in ΔFC between the ipsi- and contralateral MC and PFC after and before a cold pressor test (CPT) assessed by fNIRS. Secondary outcomes included the efficiency of the DPMS—assessed by change on the numerical pain scale (NPS) during the conditioned pain modulation (CPM) test—and disability due to FM symptoms—evaluated by the fibromyalgia impact questionnaire (FIQ). The main interest independent variables were the BDNF polymorphisms. Covariates included the intensity of chronic pain, the BDNF serum levels, pain catastrophizing, depressive symptoms, sleep quality, sociodemographic characteristics, clinical and psychiatric chronic diseases, and psychotropic and analgesic medications.
fNIRS acquisition
Functional connectivity was evaluated by fNIRS, with a NIRx® continuous waveform NirScout® near-infrared spectroscopy device (NIRx Medical Technologies, Glen Head, NY, USA), with a scan rate of 15 Hz, dual-wavelength light-emitting diode sources (760 and 850 nm). Four sources and 14 detectors were spaced about 3 cm apart and placed over the scalp. The caps were bought from EASYCAP®. The montage was intended to create 16 channels and cover the bilateral dorsal prefrontal cortex as well as the bilateral MC. The international 10–10 electroencephalography system was employed to guide probe positioning (Fig. 1). In our montage, we placed sources (S) in the F3, F4, C3, and C4 locations and detectors (D) in the AF3, F5, FC3, F1, C5, CP3, C1, AF4, F6, FC4, F2, C6, CP4, and C2 locations.
We defined four ROIs: left (l-) PFC (S: F3; D: AF3, F1, FC3, F5), l-MC (S: C3; D: FC3, C1, CP3, C5), right (r-) PFC (S: F4; D: AF4, F6, F2, FC4), r-MC (S: C4; D: FC4, C6, CP4, C2). Software equipment was NIRStar® version 14.2 (NIRx Medical Technologies, Glen Head, NY, USA). The acquisition consisted of one session of admeasurement and fNIRS acquisition, starting with 7 min of resting state, followed by a CPT (water at 0–1 °C) and then another 7 min of resting state.
A black cover was placed over the adjusted NIRS cap on the scalp to reduce environmental light disturbance. Recordings were resumed only if source-detection calibration and recording-checked signal quality retrieved an “excellent” quality in at least 14 out of 16 channels, with tolerance for the other two channels to be at least "acceptable". A qualitative scale gauged signal quality based on gain, amplitude, coefficient of variation of noise, and dark noise. For fNIRS recording, subjects sat on a comfortable armchair and maintained a still position. They fixated their gaze on a black cross fixed on the front wall at eye level 1.5 m ahead of the armchair, and they were asked to try to think of nothing.
fNIRS and cold pressor test
The signal was recorded for 7 min in a resting state. The CPT was performed while recording the cortical activation. CPT consisted of right-hand immersion up to the wrist in cold water (0–1 °C, measured by a digital thermometer) for at least 10 s and until the maximum tolerated pain25,26. After they took out the hand, we measured the resting-state cortical activation for seven more minutes—with the right-hand volar aspect laying on a towel previously put on the subjects’ lap (Fig. 2).
Preprocessing and functional connectivity analysis
Raw data was analyzed through the Brain AnalyzIR® toolbox27 in the MATLAB environment (MathWorks, Natick, MA, USA). Raw data were downsampled to 1 Hz to adequately address the high level of temporal autocorrelation in fNIRS signals, then converted to optical density into relative oxyhemoglobin concentration variations (HbO) through the modified Beer-Lambert Law28,29. We have utilized the oxyhemoglobin signal in the analysis due to evidence that this variable is the most sensitive to inferring hemodynamic response based on neurovascular coupling30,31,32.
Structured noise (e.g., physiological noise) was corrected through an autoregressive pre-whitening model, whereas motion artifacts were treated through a robust regression using iterative reweighting. Both corrections used no band/high/low filtering33,34. This method was shown to effectively address serially correlated errors, colored noise, and motion artifacts33,35. All possible pairs of channels across the time series were correlated, resulting in Pearson correlation values that underwent a Fisher Z-transformation. The difference in ROI-ROI FC (ΔFC) for each patient was retrieved by subtracting the mean ROI-ROI Z-value before CPT from the mean ROI-ROI Z-value after CPT. The ΔFC was submitted to ROI-ROI group analysis (6 ROI-ROI pairs × 42 subjects)36.
Secondary outcomes
-
(a)
DPMS function was assessed through a CPM test—expressed by the difference in quantitative sensory testing (QST) before and concurrently to a CPT serving as a heterotopic nociceptive stimulus. First, a thermode was on the ventral non-dominant forearm to define the average of three temperatures (T0) corresponding to a patient’s QST report score of 6/10 (Numerical Pain Scale (NPS) 0–10). Second, after five minutes, subjects were asked to immerse their dominant hand up to their wrist into the water at a temperature of 0–1 °C for 15 s. QST was reassessed with a pain score NPS(T1) in relation to the evoked pain by the thermode applying the T0 temperature in the ventral non-dominant forearm (QST + CPM-test). Third, the CPM-test score was calculated by the difference in the pain score on NPS(T1) and the NPS(T0). Negative values in the CPM score represent a proper DPMS function, whereas CPM scores ≥ 0 represent an impaired function.
-
(b)
Fibromyalgia Impact Questionnaire (FIQ), adapted for use in Brazil37, was used to evaluate the impact of symptoms on quality of life. It comprises ten domains and items with higher scores indicating higher disability due to pain in performing routine daily living activities, including the presence of fatigue, morning stiffness, and mood and psychiatric symptoms.
Sociodemographic, clinical, and psychological measures
Demographic data, medical comorbidities, medications use, and daily doses were evaluated using a standardized questionnaire. Psychiatric diagnoses were assessed by the Mini-international Neuropsychiatric Interview (MINI)38. Depressive symptoms were assessed by the Beck Depression Inventory—Second Edition (BDI-II)39. All questionnaires were applied using the validated Portuguese version.
Central Sensitization Inventory (CSI) was used to assess the severity of symptoms related to CS40.
Pittsburgh Sleep Quality Index (PSQI) evaluated sleep quality and disturbances over the last month41.
The Brazilian Portuguese Pain Catastrophizing Scale (BP-PCS) was used to evaluate pain catastrophizing42.
Pain Visual Analogue Scale (VAS) was used to assess pain intensity on most days of the last three months ranging from zero to 100 mm (i.e., worst possible pain).
Serum BDNF and BDNF Genotype assessments
The BDNF serum levels were assessed by enzyme-linked immunosorbent assay (ELISA) monoclonal antibodies specific for BDNF (R&D Systems, MN, United States, ChemiKine BDNF Sandwich ELISA kit, CYT306, Chemicon/Millipore, Billerica, MA, USA), and the Enzyme-linked Immunosorbent. Essays were performed in duplicates to assess intra-assay variation. Inter-assay variation was addressed using two plates per kit over two different days within the same week. All protocols followed the manufacturer’s instructions. The lower detection limit for BDNF was 7.8 pg/ml. ELISA was measured by optical density with a wavelength of 450 nm (GloMax®-Multi Microplate Reader; Promega, WI, USA). Multiplexing assay measurements were conducted in the Bio-Plex®-200 instrument (Bio-Rad). Total protein was assessed using bovine serum albumin following the Bradford method.
Blood samples were collected in 4 ml tubes with ethylenediamine tetraacetic acid. Total DNA was extracted and purified using PureLink® Genomic DNA Kit (Invitrogen, ThermoFisher Scientific). A StepOnePlusTM Real-Time PCR System (Applied Biosystems Inc, Foster City, USA) was used for genotyping the Val66Met BDNF (rs6265) polymorphism. A predesigned TaqManTM SNP genotyping assay was employed (Thermo Fisher Scientific; catalog 4,351,379, assay ID_C1159275810). A representation of the structure of the human BDNF gene and its location on chromosome 11 can be seen in Fig. 3.
Representation of the BNDF location and structure. The Val66Met (rs6265) polymorphism of the BDNF gene consists of a substitution of valine for methionine in the BDNF prodomain. BDNF exons are represented by boxes noted with roman algorisms, while lines represent introns. The SNP locus is in the prodomain region of the IX exon. CDS coding DNA sequence. pA polyadenylation sites. ATG site initiation codon. BDNF brain-derived neurotrophic factor; Val/Val Val66Val homozygous. Val/Met Val66Met heterozygous.
Statistical analysis
Assessment of data distribution was performed using the Shapiro–Wilk test. Descriptive statistics were used to summarize the main characteristics of the sample. T-tests for independent samples were used to compare continuous variables between groups. Descriptive statistics were used to summarize the main socio-demographic features of the sample. The chi-squared and Fisher's exact tests were used to compare groups for categorical variables. Spearman's correlation was used to analyze the relationship between the six ROI-ROI ΔFC Z-values, serum BDNF, ACR-score, BDI-II, BP-PCS, and FIQ.
A multivariate covariance analysis (MANCOVA) model was used to explore the relationship between the ROI − ROI ΔFC Z-values according to the BDNF genotype. Independent linear regression analysis models using the best subset selection was used to identify the possible clinical severity symptoms and serum BDNF associated with the dependent variables (ROI-ROI ΔFC Z-values) independently. Bonferroni's correction was performed for multiple comparisons.
A generalized linear mixed model (GLMM) was used to compare the change in NPS (0–10) during the CPM-test and the FIQ scores between groups of Val homozygous for BDNF (Val/Val) and heterozygous for the Met allele (Val/Met), followed by Bonferroni's Multiple Comparison Test. The model was adjusted to ACR score and serum BDNF. All analyses were performed with two-tailed tests. We accepted a type I error of 5%. For all analyses, we considered a two-tailed type I error α = 0.05. Statistical analysis was performed by the IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, N.Y., USA).
Results
Patient characteristics
The sample was composed of 42 female subjects, 30 were homozygous for the BDNF (66)Val allele (Val/Val), and 12 were heterozygous for the Val66Met allele (Val/Met). The clinical and demographic characteristics are presented in Table 1. The groups differed regarding years of education, the WPI index, and the FIQ.
Univariate analysis
Comparisons of mean according to BDNF genotype on primary and secondary outcomes
The mean (standard deviation) of primary and secondary outcomes according to the Val/Met genotype are presented in Table 2. In the univariate analysis, we did not find a difference statistically significant between genotypes related to ΔFC intra- and inter-hemispheric. The heterozygotes showed lower scores on the QIF compared to homozygotes.
Analysis of the relationships between outcomes according to BDNF genotype
The Spearman correlation analysis was used to explore the relationship between the ROI-ROI ΔFC with the following covariates according to Val66Met genotypes: ACR score, PCS, BDI-II, FIQ, serum BDNF (ng/ml), and the CPM test score. These correlations are presented in Table 3. We found a positive and moderate correlation between serum BDNF in Val/Val genotype with ΔFC in l-PFC—l-MC and l-PFC—r-MC. In contrast, in Val/Met patients, the ACR score was moderately and positively correlated with the ΔFC in l-FC—l-MC, l-MC—r-FC, and r-FC—r-MC. The FIQ score positively correlated with the ΔFC in l-MC—r-MC.
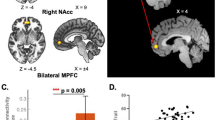
Multivariate analysis of the relationship between the ΔFC according to BDNF genotype
The MANCOVA model using Bonferroni's Multiple Comparison Test revealed a significant relationship between the Val/Met group and the outcomes related to FC (Hotelling's Trace = 1.76, F (6) = 5.47, p = 0.001). BDNF genotype Val/Met compared to genotype Val/Val showed higher ΔFC in the following areas: l-PFC—l-MC, l-PFC—r-PFC, l-PFC—r-MC, and l-MC—r-PFC. Regression analysis demonstrated that the serum BDNF was associated with all ΔFC differences between groups, except for the ΔFC between r-PFC—r-MC. In contrast, the ACR score positively correlated with ΔFC in l-MC—r-PFC and r-PFC—r-MC. Results can be seen in Table 4 and Fig. 4.
The difference in functional connectivity patterns in response to acute pain according to the BDNF genotype and its associations. The Val66Met (rs6265) polymorphism of the BDNF gene impacts the changes in FC in response to a cold pressor test in female fibromyalgia patients. Heatmaps presenting the difference in 7 min of resting-state functional connectivity assessed after and before a cold pressor test, in the Val/Val and Val/Met groups. The significant differences between groups of BDNF genotypes are presented with an asterisk. (A) Data regarding the Val/Val group. The blue edges between regions of interest represent a significant decrease in ΔFC between groups. (B) Data regarding the Val/Met group. The red edges represent a significant increase in ΔFC between groups. (C) Data associated with the Val/Met group. The Val/Met group presented a significantly ΔFC difference in response to acute pain in the cold pressor test, coupled with lower disability due to pain and performance associated with higher efficiency of the descending pain modulatory system assessed by the conditioned pain modulation test. The colored edges represent ΔFC values as indicated in the heatmap bar. BDNF brain-derived neurotrophic factor. Val/Val Val66Val homozygous. Val/Met Val66Met heterozygous. ΔFC functional connectivity delta-value. rs-FC resting state functional connectivity. PFC prefrontal cortex. MC motor cortex. -l left. -r right. *p < 0.05.
Secondary outcomes: multivariate analysis to examine the efficiency of DPMS, time of pain reactivity, and quality of life due to fibromyalgia symptoms according to genotypes
A generalized linear mixed model (GLMM) revealed a main effect according to the BDNF genotype in both DPMS evaluated by the change in the NPS (0–10) and quality of life assessed by the FIQ. The heterozygotes showed lower dysfunction on the DPMS. Despite the genotypes, the function of DPMS was negatively correlated with serum BDNF and ACR scores. In contrast, a higher score on the FIQ was positively correlated with a higher ACR score. Lower quality of life was directly related to the severity of ACR, a composite index by sums of the WPI index and SSS. Data are presented in Table 5.
Discussion
These findings reveal that the Val/Met group is associated with an increased ΔFC between the PFC and MC. In contrast, the Val/Val group showed a decreased interhemispheric connectivity in these areas, less active engagement of DPMS, and a higher impact of fibromyalgia symptoms on quality of life. Furthermore, we found that despite genotypes, the serum BDNF and scores on ACR are positively correlated to ΔFC in the PFC and MC areas. These results highlight that FM patients carrying the BDNF Val/Met polymorphism might be less prone to maladaptive neuroplasticity, as indicated by the higher efficiency of DPMS and less severe fibromyalgia symptoms. However, since the effects of BDNF in the nervous system are complex, it is possible that specific compensatory mechanisms, in terms of brain plasticity, may occur at least partially due to genetic differences43. Therefore, a single explanation for our findings is too ambitious, and parsimony is required to translate them into the clinical setting.
Our findings may be explained by the hypothesis that the increase in ΔFC associated with the BDNF Val66Met reflects a cortical response to pain in response to painful stimuli. Since earlier studies have found that the BDNF Val/Met polymorphism may be associated with the modulation of neuroplasticity44,45,46, the phenomenon described in the current study may be related to differences in neuroplasticity between both groups due to the BDNF function. Furthermore, Val/Met genotype was associated with a distinct propensity to FM symptoms, which seems to indicate that BDNF also could modulate the emergence of the FM phenotype. This hypothesis is corroborated by a growing body of evidence that subjects with BDNF Val66Met polymorphism display differences in brain plasticity expressions as induced by motor learning46, brain stimulation44, and experimental pain stimulation47. In line with the present results, it is reasonable to ask if BDNF Val66Met polymorphism may contribute to differences in the effect of neuromodulation therapeutic and behavior related to pain. Aligned with this perspective, the positive ΔFC in response to CPT expressed by Val/Met FM patients indicates that this genotype is significant for the PFC—MC activation map.
Remarkably, the current findings’ relevance lies in the fact that the BDNF Val66Met genotype significantly discriminates between two ΔFC patterns in response to acute pain stimulus. Thus, our findings give input on the criticality of this polymorphism as a differential factor for the functional fingerprint of acute pain response in female FM patients. This may explain the influence of BDNF on the degree and quality of response to treatment in various chronic pain conditions (e.g., tDCS, electroacupuncture, among others)48,49,50,51. The association between serum BDNF levels and the Val66Met polymorphism with DPMS function may be either due to an independent effect of both factors or because BDNF serum levels are linked with the respective polymorphism, which is plausible when considering that the Val66Met leads to changes in concentration of serum BDNF in some conditions52.
Moreover, the results indicate that serum BDNF was associated with increased FC in response to noxious stimulus across all but one of the ROI-ROIs analyzed, nominally ΔFC r-PFC—r-MC. This is paramount for representing a consistent direction towards which BDNF protein seems to influence changes in MC—PFC FC following acute pain, that is, as a positive function of its serum levels. The ACR score was positively associated with ΔFC in l-MC—r-PFC and ΔFC in r-PFC—r-MC, implying a higher widespread pain and symptom severity associated with an increase in this ROI-ROIs FC as a response to noxious stimulation. ACR was not associated with ΔFC in other ROI-ROIs but was unsurprisingly associated with lower quality of life (i.e., positive association with FIQ). Val/Val genotype had been previously associated with higher pain catastrophizing in FM53.
Consequently, this intricate pattern prevents the present study from putatively defining one of the genotypes (i.e., Val/Met or Val/Val) as related to more severe symptoms, with more studies being required to address this subject. For now, this polymorphism seems to have some impact on the functional response to pain as assessed by ΔFC across MC and PFC. Perhaps the effect that this differential pattern has on the global clinical status of FM patients will not be shown to be more than subtle. However, it might have value as a biomarker for follow-up and or response to treatment.
In this sense, it is remarkable that an SNP in a critical gene for neuroplasticity modulation is sufficient to cause different brain responses to acute noxious stimuli in patients with a chronic pain disease. Nevertheless, the influence of multiple genetic variants on brain states needs to be further explored. Further studies should investigate if these polymorphism-dependent differences in the functional fingerprint of FM patients are dynamically set throughout development by a continuous modulation of experience-dependent neuroplasticity46 or if they represent a consistent pattern since birth owing predominantly to genetic factors.
Although these results suggest an association between pain processing and brain functional signatures among the BDNF Val66Met polymorphism genotypes, several limitations of the present study must be considered. First, this is an exploratory analysis with a few participants compared to other neuroimaging genetics surveys. Second, this study compared functional connectivity, psychophysical, and clinical parameters between subgroups of patients with fibromyalgia. This is within the scope of characterizing clusters of a prototypical primary chronic pain disease by the severity of symptoms and looking for potential phenomena-related underlying mechanisms. This approach has as a limitation the absence of comparisons with healthy controls and, therefore, no extrapolation of these findings compared to the healthy population. Third, the effects of the BDNF Val66Met polymorphism on the noxious-evoked ΔFC between the MC and the PFC was our primary interest due to the critical role these ROIs have in NIBS, resulting in a montage focused on these cortical areas. Furthermore, although the optode positioning matches more specifically the DLPFC than other PFC regions, we chose to refer to this ROI more generically as PFC since fNIRS do not present a spatial resolution as high as other neuroimaging methods and since we did not utilize any neuronavigation device. Fourth, only Val/Val and Val/Met were included due to our population's low prevalence of individuals with the Met/Met genotype54. Fifth, only right-handed women were included in this study, hindering the assessment of results differentially associated with lateralization of brain function and the extrapolation of these results to male FM patients. Finally, this is a cross-sectional study; further research with larger sample sizes in longitudinal studies is needed to evaluate the dynamics of the Val66Met effects in FM, such as in response to treatment and symptom evolution.
These results indicate that the FM patients carrying the Val/Met genotype are prone to show increased FC across MC and PFC response to a standardized acute nociceptive stimulus. Besides, Val/Met genotype is related to the higher efficiency of DPMS and less severe fibromyalgia symptoms. These findings suggest that this genetic factor might contribute to individual differences when experiencing pain and perhaps affect the vulnerability to the emergence of chronic pain syndromes.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Treede, R. et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 160, 19–27 (2019).
Clauw, D. Fibromyalgia. JAMA 311, 1547 (2014).
Arnold, L. et al. AAPT diagnostic criteria for fibromyalgia. J. Pain 20, 611–628 (2019).
Queiroz, L. Worldwide epidemiology of fibromyalgia. Curr. Pain Headache Rep. 17(8), 1–6 (2013).
Woolf, C. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 152, S2–S15 (2011).
Martínez, M. et al. Fibromyalgia as a heterogeneous condition: Subgroups of patients based on physical symptoms and cognitive-affective variables related to pain. Span. J. Psychol. 24, E33 (2021).
Huynh, V. et al. Descending pain modulatory efficiency in healthy subjects is related to structure and resting connectivity of brain regions. Neuroimage 247, 118742 (2022).
Goksan, S., Baxter, L., Moultrie, F., Duff, E., Hathway, G., Hartley, C. et al. The influence of the descending pain modulatory system on infant pain-related brain activity. eLife. 7, e37125 (2018). https://doi.org/10.7554/eLife.37125.
de Oliveira Franco, Á. et al. Hyper-connectivity between the left motor cortex and prefrontal cortex is associated with the severity of dysfunction of the descending pain modulatory system in fibromyalgia. PLoS ONE 17, e0247629 (2022).
Soldatelli, M., Siepmann, T., Illigens, B., Souza dos Santos, V., Lucena da S Torres, I., Fregni, F. et al. Mapping of predictors of the disengagement of the descending inhibitory pain modulation system in fibromyalgia: An exploratory study. Brit. J. Pain. 15, 221–233 (2020).
Chang, W. et al. Altered primary motor cortex structure, organization, and function in chronic pain: A systematic review and meta-analysis. J. Pain 19, 341–359 (2018).
Zortea, M. et al. Transcranial direct current stimulation to improve the dysfunction of descending pain modulatory system related to opioids in chronic non-cancer pain: An integrative review of neurobiology and meta-analysis. Front. Neurosci. 13, 1218 (2019).
Gentile, E., Ricci, K., Delussi, M., Brighina, F. & de Tommaso, M. Motor cortex function in fibromyalgia: A study by functional near-infrared spectroscopy. Pain Res. Treat. 2019, 1–7 (2019).
Leite, J., Carvalho, S., Battistella, L., Caumo, W. & Fregni, F. Editorial: The role of primary motor cortex as a marker and modulator of pain control and emotional-affective processing. Front. Hum. Neurosci. 11, 270 (2017).
Ong, W., Stohler, C. & Herr, D. Role of the prefrontal cortex in pain processing. Mol. Neurobiol. 56, 1137–1166 (2018).
Donadel, D., Zortea, M., Torres, I., Fregni, F. & Caumo, W. The mapping of cortical activation by near-infrared spectroscopy might be a biomarker related to the severity of fibromyalgia symptoms. Sci. Rep. 11(1), 1–14 (2021).
Antal, A. et al. Brain-derived neurotrophic factor (BDNF) gene polymorphisms shape cortical plasticity in humans. Brain Stimul. 3, 230–237 (2010).
Miranda, M., Morici, J., Zanoni, M. & Bekinschtein, P. Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front. Cell. Neurosci. 13, 363 (2019). https://doi.org/10.3389/fncel.2019.00363.
Zhao, M. et al. BDNF Val66Met polymorphism, life stress and depression: A meta-analysis of gene-environment interaction. J. Affect. Disord. 227, 226–235 (2018).
Wei, S. et al. The BDNF Val66Met polymorphism is associated with the functional connectivity dynamics of pain modulatory systems in primary dysmenorrhea. Sci. Rep. 6(1), 1–11 (2016).
Zanette, S. et al. Higher serum S100B and BDNF levels are correlated with a lower pressure-pain threshold in fibromyalgia. Mol. Pain. 10, 1744–8069 (2014).
Huppert, T., Hoge, R., Diamond, S., Franceschini, M. & Boas, D. A temporal comparison of BOLD, ASL, and NIRS hemodynamic responses to motor stimuli in adult humans. Neuroimage 29, 368–382 (2006).
Naseer, N. & Hong, K. fNIRS-based brain-computer interfaces: A review. Front. Hum. Neurosci. 9, 3 (2015).
Wolfe, F. et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 46, 319–329 (2016).
Beltran Serrano, G. et al. Comparison of hypnotic suggestion and transcranial direct-current stimulation effects on pain perception and the descending pain modulating system: A crossover randomized clinical trial. Front. Neurosci. 13, 662 (2019).
Koltzenburg, M., Pokorny, R., Gasser, U. & Richarz, U. Differential sensitivity of three experimental pain models in detecting the analgesic effects of transdermal fentanyl and buprenorphine. Pain 126, 165–174 (2006).
Santosa, H., Zhai, X., Fishburn, F. & Huppert, T. The NIRS Brain AnalyzIR Toolbox. Algorithms 11, 73 (2018).
Cope, M. et al. Methods of quantitating cerebral near infrared spectroscopy data. Oxygen Transport to Tissue. X https://doi.org/10.1007/978-1-4615-9510-6_21 (1988).
Cope, M. & Delpy, D. System for long-term measurement of cerebral blood and tissue oxygenation on newborn infants by near infra-red transillumination. Med. Biol. Eng. Compu. 26, 289–294 (1988).
Hoshi, Y., Kobayashi, N. & Tamura, M. Interpretation of near-infrared spectroscopy signals: A study with a newly developed perfused rat brain model. J. Appl. Physiol. 90, 1657–1662 (2001).
Strangman, G., Culver, J., Thompson, J. & Boas, D. A quantitative comparison of simultaneous BOLD fMRI and NIRS recordings during functional brain activation. Neuroimage 17, 719–731 (2002).
Zama, T. & Shimada, S. Simultaneous measurement of electroencephalography and near-infrared spectroscopy during voluntary motor preparation. Sci. Rep. 5(1), 1–9 (2015).
Barker, J., Aarabi, A. & Huppert, T. Autoregressive model based algorithm for correcting motion and serially correlated errors in fNIRS. Biomed. Opt. Express 4, 1366 (2013).
Huppert, T. Commentary on the statistical properties of noise and its implication on general linear models in functional near-infrared spectroscopy. Neurophotonics. 3, 010401 (2016).
Barker, J., Rosso, A., Sparto, P. & Huppert, T. Correction of motion artifacts and serial correlations for real-time functional near-infrared spectroscopy. Neurophotonics. 3, 031410 (2016).
Santosa, H., Aarabi, A., Perlman, S. & Huppert, T. Characterization and correction of the false-discovery rates in resting state connectivity using functional near-infrared spectroscopy. J. Biomed. Opt. 22, 055002 (2017).
Marques, A. et al. Validação da versão brasileira do fibromyalgia impact questionnaire (FIQ). Rev. Bras. Reumatol. 46, 24–31 (2006).
Amorim, P. Mini International Neuropsychiatric Interview (MINI): Validação de entrevista breve para diagnóstico de transtornos mentais. Rev. Bras. Psiquiatr. 22, 106–115 (2000).
Gomes-Oliveira, M., Gorenstein, C., Neto, F., Andrade, L. & Wang, Y. Validation of the Brazilian Portuguese version of the beck depression inventory-II in a community sample. Rev. Bras. Psiquiatr. 34, 389–394 (2012).
Caumo, W. et al. The Central Sensitization Inventory validated and adapted for a Brazilian population: Psychometric properties and its relationship with brain-derived neurotrophic factor. J. Pain Res. 10, 2109–2122 (2017).
Bertolazi, A. et al. Validation of the Brazilian Portuguese version of the pittsburgh sleep quality index. Sleep Med. 12, 70–75 (2011).
Sehn, F. et al. Cross-cultural adaptation and validation of the Brazilian Portuguese version of the pain catastrophizing scale. Pain Med. 13, 1425–1435 (2012).
Bigos, K. & Weinberger, D. Imaging genetics—days of future past. Neuroimage 53, 804–809 (2010).
Cheeran, B. et al. A common polymorphism in the brain-derived neurotrophic factor gene (BDNF) modulates human cortical plasticity and the response to rTMS. J. Physiol. 586, 5717–5725 (2008).
Egan, M. et al. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell 112, 257–269 (2003).
Kleim, J. et al. BDNF val66met polymorphism is associated with modified experience-dependent plasticity in human motor cortex. Nat. Neurosci. 9, 735–737 (2006).
Di Lorenzo, C. et al. The Val66Met polymorphism of the BDNF gene influences trigeminal pain-related evoked responses. J. Pain 13, 866–873 (2012).
Betancur, D., Tarragó, M., Torres, I., Fregni, F. & Caumo, W. Central post-stroke pain: An integrative review of somatotopic damage, clinical symptoms, and neurophysiological measures. Front. Neurol. 12, 678198 (2021).https://doi.org/10.3389/fneur.2021.678198.
Brietzke, A. et al. Potency of descending pain modulatory system is linked with peripheral sensory dysfunction in fibromyalgia. Medicine 98, e13477 (2019).
Brietzke, A. et al. Large treatment effect with extended home-based transcranial direct current stimulation over dorsolateral prefrontal cortex in fibromyalgia: A proof of concept sham-randomized clinical study. J. Pain 21, 212–224 (2020).
Santos, V. et al. Cognitive effects of transcranial direct current stimulation combined with working memory training in fibromyalgia: a randomized clinical trial. Sci. Rep. 8(1), 1–11 (2018).
Han, J. et al. Brain-derived neurotrophic factor and obesity in the WAGR syndrome. N. Engl. J. Med. 359, 918–927 (2008).
da Silveira Alves, C., Caumo, W., Silvestri, J., Zortea, M., dos Santos, V., Cardoso, D. et al. Pain catastrophizing is associated with the Val66Met polymorphism of the brain-derived neurotrophic factor in fibromyalgia. Adv. Rheumatol. 60(1), 39 (2020). https://doi.org/10.1186/s42358-020-00141-9.
Petryshen, T. et al. Population genetic study of the brain-derived neurotrophic factor (BDNF) gene. Mol. Psychiatry 15, 810–815 (2009).
Acknowledgements
The authors thank the patient volunteers and the Hospital de Clínicas de Porto Alegre. We thank Maria Adelia de Aratanha, Ph.D., for the valuable technical support.
Author information
Authors and Affiliations
Contributions
Conceptualization: Á.d.O.F., G.d.O.V., C.F.d.S.A., I.L.S.T., F.F., and W.C.; Data curation: Á.d.O.F., G.d.O.V., C.F.d.S.A., R.L.A., P.V., L.R., R.T., S.B.M.; Formal analysis: Á.d.O.F. and W.C.; Funding acquisition: W.C.; Resources: W.C.; Writing – original draft: Á.d.O.F. and W.C.; Writing – review and editing: Á.d.O.F., C.F.d.S.A., F.F., and W.C. All authors contributed to the approval of the final version to be published. Dr. Wolnei Caumo agrees to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The funders had no role in study design, data collection and analysis, publication decision, or manuscript preparation. (i) Coordination for the Improvement of Higher Education Personnel (CAPES)—Grant No. 2018 to C.F.S.A. and L.R. for postdoc and to R.L. and P.V. for Ph.D. (ii) National Council for Scientific and Technological Development (CNPq)—Grant No. 302688/2017-0 to W.C. (iii) Fundo de Incentivo à Pesquisa e Eventos (FIPE) from the Postgraduate Research Group at the Hospital de Clínicas de Porto Alegre—Project No. 2017–0329. (iv) Brazilian Innovation Agency (Financiadora de Estudos e Projetos (FINEP))—process number 1245/13. (v) Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS)—Grant No 17/2551-0001 087-6 and 17/2551-0001 476-6 to W.C. (vi) Hospital de Clínicas de Porto Alegre/ CNPq—Bolsa de Iniciação Científica (IC) to R.T.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Oliveira Franco, Á., de Oliveira Venturini, G., da Silveira Alves, C.F. et al. Functional connectivity response to acute pain assessed by fNIRS is associated with BDNF genotype in fibromyalgia: an exploratory study. Sci Rep 12, 18831 (2022). https://doi.org/10.1038/s41598-022-23476-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-23476-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.