Abstract
The intestinal microbiota has been implicated in the pathogenesis of complications following colorectal surgery, yet perioperative changes in gut microbiome composition are poorly understood. The objective of this study was to characterize the perioperative gut microbiome in patients undergoing colonoscopy and colorectal surgery and determine factors influencing its composition. Using Illumina amplicon sequencing coupled with targeted metabolomics, we characterized the fecal microbiota in: (A) patients (n = 15) undergoing colonoscopy who received mechanical bowel preparation, and (B) patients (n = 15) undergoing colorectal surgery who received surgical bowel preparation, composed of mechanical bowel preparation with oral antibiotics, and perioperative intravenous antibiotics. Microbiome composition was characterized before and up to six months following each intervention. Colonoscopy patients had minor shifts in bacterial community composition that recovered to baseline at a mean of 3 (1–13) days. Surgery patients demonstrated substantial shifts in bacterial composition with greater abundances of Enterococcus, Lactobacillus, and Streptococcus. Compositional changes persisted in the early postoperative period with recovery to baseline beginning at a mean of 31 (16–43) days. Our results support surgical bowel preparation as a factor significantly influencing gut microbial composition following colorectal surgery, while mechanical bowel preparation has little impact.
Similar content being viewed by others
Introduction
In 2020, an estimated 147,950 adults in the United States were diagnosed with colorectal cancer, for which the primary treatment is surgery1. Alternatively, diverticular disease, responsible for 200,000 inpatient admissions annually, is the leading cause of elective colon surgery, with an estimated 15% of patients eventually undergoing colectomy2,3. Three out of four patients with Crohn’s disease also ultimately undergo surgical resection, and half of these patient relapse and require additional surgery4. Thus, regardless of the disease, delivery of optimal patient care often requires bowel resection, ideally with anastomosis, that also requires an optimal environment for appropriate wound healing. However, complications, including surgical site infections (SSI), anastomotic leak, postoperative ileus (POI) and Clostridioides difficile (C. difficile) infection, following colorectal surgery remain major problems and sources of patient morbidity, mortality, and economic burden. In fact, colorectal surgery has among the highest rates of SSI, varying from 5 to 23% and a weighted mean of 11%5. Thus, there is an urgent need to identify strategies to prevent complications associated with colon and rectal surgery.
Postoperative complications occur despite optimal surgical technique and seemingly appropriate sterile conditions. It is likely that these complications arise from a combination of various host factors (i.e., comorbidities) as well as the activity and composition of the intestinal microbiota. Once believed to be a benign bystander, the microbiota contributes to host metabolism via multiple mechanisms including energy harvest, metabolite production, and induction of pro- and anti-inflammatory immune responses6. The intestinal microbiota has been proposed as a primary vehicle through which host genetics and environment interact to directly affect postoperative complications. Krezalek, et al.7 demonstrated that mice intestinally colonized with methicillin-resistant Staphylococcus aureus can develop surgical site infections by migration to the wound without sepsis or bacteremia. The intestinal microbiota also plays a causative role in anastomotic leak by antagonizing wound healing through collagenase production8. Furthermore, the occurrence of POI has been linked to increases in the relative abundances of bacteria shown to promote pathogenic inflammation9.
Complications, particularly those of bacterial origin, continue to plague the field of colon and rectal surgery. The theoretical role of mechanical bowel preparation (MBP) with oral antibiotics (OA) is to facilitate the function of the host immune defense system by decreasing intestinal bacterial density and to mechanically cleanse the intestine10. The most commonly implemented bowel regimen includes polyethylene glycol for MBP plus neomycin and metronidazole as OA, herein the combination of MBP + OA is referred to as surgical bowel preparation (SBP)11. Patients undergoing colorectal resection also commonly receive perioperative intravenous (IV) antibiotics up to 24 h postoperative for additional SSI prevention.
While many studies have evaluated and compared the utility of MBP with or without OA, there is a poor understanding of the impact of these interventions on the composition of the intestinal microbiome following colorectal surgery. In this study, our primary aim was to characterize the perioperative composition of the intestinal microbiome, including short-chain fatty acids (SCFA) and fecal immunoglobulin A (IgA), of patients undergoing colorectal surgery after receiving SBP with perioperative IV antibiotics and compare these results to patients undergoing colonoscopy after receiving MBP alone. Secondary outcomes included the identification of factors associated with postoperative complications.
Results
Study cohorts
Fecal samples were obtained from 15 patients who underwent colonoscopy after MBP alone, and 15 patients who underwent colorectal surgery after SBP with perioperative IV antibiotics. Patient demographics and clinical data are presented in Table 1. Patients who underwent surgery were older and had greater Charlson Comorbidity Index scores12 compared to patients who underwent colonoscopy. Surgery patients had a median length of hospital stay of 3 (0–11) days. The colonoscopy cohort included 7 patients (47%) who underwent screening colonoscopy and 8 patients (53%) who underwent diagnostic colonoscopy for hematochezia (n = 7) or chronic diarrhea (n = 1). The surgery cohort included 11 patients (73%) who underwent colorectal resection for colorectal cancer (n = 6) or diverticular disease (n = 5), and 4 patients (27%) who underwent non-resectional colorectal surgery for rectal prolapse (n = 2) or rectal neoplasia (n = 2). Operative details and clinical history of surgery patients are detailed in Table 2.
Microbial community composition and diversity
We performed 16S rRNA gene-based amplicon sequencing to characterize the taxonomic profiles of gut microbiota in pre-, intra-, and post-procedural or postoperative samples. Among all patients, the most abundant genera of bacteria included Bacteroides, Faecalibacterium, Alistipes, Parabacteroides, Blautia, Streptococcus, and Roseburia (Fig. 1). Significant changes in Shannon indices were not observed in samples from patients undergoing colonoscopy, while samples from surgical patients had significantly lower alpha diversity immediately following surgery (Supplemental Table S2; Tukey’s post-hoc P < 0.001). Among specimens from patients undergoing surgery, there were no significant difference in Shannon indices between resectional and non-resectional colorectal surgery patients over the study course (P = 0.142).
To assess the change in gut microbial composition in individual patients over the study course, we used SourceTracker2 software, and found that patients who underwent colonoscopy did not have significant changes in their overall microbial composition from that observed pre procedure (Fig. 2A). However, surgery patients experienced a substantial change in gut microbial composition within the early postoperative period up to 10 days (Fig. 2B). At T10, samples from nine surgery patients (60%) had < 35% similarity to pre-operative microbial community composition, of which four patients (27%) had < 2% similarity. Samples from two surgery patients were > 75% similar to pre-operative microbial composition. Patients within the surgery cohort experienced recovery of preoperative microbiota at varying frequencies. Three of nine patients (33%) with extreme early postoperative changes in gut microbial composition began to repopulate microbial communities by one month (T30), while compositional changes in three of these nine patients persisted at this timepoint.
Effects of OA in conjunction with MBP
Colonoscopy and surgery cohorts had significantly different bacterial community compositions at baseline (Fig. 3; ANOSIM, R = 0.13, P = 0.016), and were analyzed separately because of this. While no longitudinal changes in community composition were observed among patients who underwent colonoscopy (Fig. 3A), MBP alone significantly changed community composition intra-procedure (T0), which was dissimilar from pre-procedural (T<0) and late post-procedural (T30 and T180) samples (Table 3; ANOSIM, R = 0.17–0.27, P = 0.001–0.004). In contrast, communities from surgery patients showed a directional shift away from the preoperative assemblage in both the intra- and short-term postoperative samples (T0 and T10), which had greater abundances of Enterococcus, Lactobacillus, and Streptococcus (Fig. 3B). Samples in the intra- and short-term postoperative period (T10) showed significant dissimilarity from both preoperative (T<0) and late postoperative (T30 and T180) samples (Table 3; ANOSIM, R = 0.26–0.47, P = 0.001–0.004). Increased abundances of genera within the Firmicutes and Bacteroidetes phyla were observed in both preoperative (T<0) and late (T30 and T180) postoperative samples (Fig. 3B).
To further describe the differences in microbial composition between colonoscopy and surgery patients over the study course, we performed an analysis with splinectomeR (Supplemental Fig. S2). Over the study period, there were significant reductions in the relative abundances of Bacteroides, Faecalibacterium, and Roseburia in surgery patients compared to colonoscopy patients (P = 0.001). Furthermore, surgery patients had a significant increase in the relative abundance of Streptococcus compared to colonoscopy patients (P < 0.001).
Single patient with anastomotic leak
One patient, who underwent robotic low anterior resection for rectal adenocarcinoma, presented with postoperative anastomotic leak on postoperative day five, after discharging from the hospital. This patient was taken urgently to the operating room for pelvic washout, primary repair of the anastomotic defect and diverting loop ileostomy. Fecal samples from this patient showed < 1% similarity to preoperative microbial composition in the short-term post-operative period (T10; collected postoperative day 1), as determined by SourceTracker2, which persisted at one month (T30). Approximately five months after index operation, the patient underwent ileostomy reversal after receiving perioperative IV antibiotics without MBP or OA. A sample was collected at this time intraoperatively from the unprepped colon. This was observed to have 56% similarity to the initial preoperative sample and showed a shift toward the preoperative assemblage on PCoA (Supplemental Fig. S3). The microbial community in a subsequent sample, obtained on postoperative day one after ileostomy reversal, was 1.2% similar to preoperative composition by SourceTracker and resembled those of other early postoperative samples. A final sample, obtained six months after ileostomy reversal, was 63% similar to the initial preoperative sample and appeared to be similar to other 6-month post-operative samples.
Evaluation of short-chain fatty acids
Preoperative, T10, and T30 samples were further analyzed for SCFA composition (Table 4). Due to insufficient sample volume, intra-operative samples were excluded from analysis. Among T10 samples, one sample in the colonoscopy group and eight in the surgery group had SCFA concentrations within the range observed in the blanks (within the mean ± 1 standard deviation) and were excluded from statistical comparisons, as were two surgery samples at the T30 time point. Differences in detection of SCFA between colonoscopy and surgery groups did not differ significantly at any time point (χ2 P = 0.218). Among all time points, concentrations of butyric acid and valeric acid were significantly greater in the colonoscopy group (P = 0.010 and 0.031, respectively), but no other significant differences were observed. Subsequent longitudinal analysis using SplinectomeR indicated that the greatest difference in concentrations between treatment groups occurred at the T10 time point (Supplemental Fig. S4). Among the colonoscopy samples, concentrations of SCFA predominantly correlated with relative abundances of Alistipes and Akkermansia (Supplemental Table S3). Conversely, among the surgical samples, SCFA concentrations correlated with abundances of Parabacteroides and Blautia and negatively correlated with Streptococcus.
Fecal IgA and calprotectin
Although fecal IgA levels did not significantly change from preoperative (T < 0) to early postoperative (T10) samples among patients that underwent either colonoscopy or colorectal surgery (Supplemental Fig. S5; Tukey’s post-hoc P = 0.415), we found that concentrations of fecal IgA inversely correlated with microbial diversity by Shannon index (Spearman ρ = −0.69, P < 0.0001). Fecal calprotectin levels also did not significantly change from preoperative (T<0) to early postoperative (T10) samples among patients who underwent colonoscopy or colorectal surgery (Supplemental Fig. S6; P = 0.134).
Discussion
The composition of the intestinal microbiome appears to be a major contributor to the occurrence of postoperative complications including SSI, anastomotic leak, POI, and C. difficile infection6,8,9,13. However, the impact of important perioperative factors that are known to shape its composition have not been described. This study showed that while MBP alone does change the composition of the microbiome, the magnitude of this shift is small, and the gut microbiome composition reverts to baseline by ten days following colonoscopy. In contrast, patients who received SBP displayed acute shifts of greater magnitude, requiring at least 30 days to return to a composition similar to baseline. Colorectal surgery with or without bowel resection did not appear to significantly impact the gut microbiome among surgical patients, as changes were observed in all such patients, independent from underlying disease or type of colorectal resection. While the aim of our study was to assess perioperative shifts in the microbiota, our sample sizes and patient heterogeneity exclude specific conclusions related to type or surgery, disease, or patient outcome. In this study, MBP with OA was the single most influential factor in shaping the composition of the gut microbiome acutely and longitudinally following colon and rectal surgery.
These observations build on our previous work, that perioperative antibiotics most significantly impact acute postoperative changes in the microbiome, to a greater extent than caloric restriction or gastric resection, following vertical sleeve gastrectomy14. The impact of SBP is demonstrated longitudinally in the gut microbial composition with potential implications for postoperative complications in patients undergoing colon and rectal surgery. Communities from surgery patients showed a directional shift away from preoperative assemblages, with greater abundances of Enterococcus, Lactococcus, and Streptococcus. These changes are noteworthy as they may be associated with adverse post-operative outcomes. For example, Enterococcus has been mechanistically linked to the development of anastomotic leak via the production of matrix metalloproteinase 9, which degrades collagen leading to tissue breakdown8. Enterococcus and Streptococcus are also potent bacteriocin and lactic acid producing bacteria15,16, and may be general markers for dysbiotic stress in the clinical setting. These bacteria dominate the microbiota composition, disrupt the gut barrier, and are associated with the subsequent development of bacteremia in patients who received antibiotics for allogeneic hematopoietic stem cell transplantation (allo-HSCT). Patients who undergo allo-HSCT have shown to develop markedly reduced microbial diversity which is an independent predictor of mortality17. In fact, patients who are dominated by these particular organisms are at highest risk for bloodstream infections during allo-HCST18. Overall, our data are consistent with many of the deleterious changes observed in patients undergoing allo-HSCT.
We also observed a significant reduction in the relative abundance of critical genera including Bacteroides, Faecalibacterium, and Roseburia in surgery patients compared to colonoscopy patients. Anastomotic leak has been associated with a relative paucity of Faecalibacterium19. Abundances of both Faecalibacterium and Roseburia genera strongly correlate with microbial diversity, and their reduction has been suggested in the pathogenesis of ulcerative colitis19,20,21. Interestingly, we noted correlations between SCFA and butyrate producing Roseburia and Blautia among samples collected in the surgical arm, while Faecalibacterium negatively correlated with SCFA concentrations among patients undergoing colonoscopy. These results suggest that typically cited butyrate producers may act in a compensatory manner following surgery to promote healing, while normal microbial communities shift this function to members of Bacteroidetes (e.g., Alistipes), as observed in the colonoscopy group. This suggestion further highlights the need to explore microbial community interactions to better assess the role of the microbiome in postoperative healing and complications. It is noteworthy that fecal levels of butyric acid and valeric acid precipitously declined following surgery. Dysbiotic microbiota with depleted SCFA results in dysregulated immune function propagating intestinal and systemic inflammation and colitis impeding wound healing22. This likely has greater significance in the immediate postoperative phase in which colonic healing is actively taking place at a time when butyric acid and valeric acid are at their nadir levels.
Our singular anastomotic leak patient provides an effective case study for the effects of SBP. Preoperatively, the patient’s microbial composition was similar to that of the surgical cohort, and while the microbial composition shifted with MBP plus OA, the anastomotic leak patient’s composition was overwhelmingly dominated by Streptococcus. Notably, postoperative IgA levels were 16-fold higher in this patient compared to the perioperative sample, suggesting a significant and concomitant increase in gut inflammation. This patient displayed significant shifts in composition after each surgery, highlighting the impacts of SBP and perioperative IV antibiotics on the intestinal microbiome. This patient also highlights a potentially deleterious impact of SBP, and perhaps instead of protecting the patient, providing an ecologic advantage for streptococcal propagation of inflammation and anastomotic breakdown.
Our study does have important weaknesses, including the lack of mucosal microbiota, which may be different from the luminal microbiome reflected in stool23,24. Secondly, a larger cohort of patients is required to verify our observations. This would also enable the identification of more specific changes in the microbiome that correlate with postoperative outcomes. Additionally, we included patients undergoing a variety of different types of operations. While this broad inclusion makes it difficult to identify a relationship between SBP and compositional changes in the gut microbiome, it does strengthen one of the findings of this study—that type of colorectal surgery with or without bowel resection impacts the composition of the microbiome to a lesser extent than the profound impact of SBP. Also, while we did not observe a change in fecal IgA or calprotectin, we did identify a strong inverse correlation between IgA levels and alpha diversity, which is consistent with previous reports25. It remains possible that IgA levels and fecal calprotectin do change with postoperative shifts in the microbiome, but a larger cohort is required to investigate potential relationships. Future studies with more patients are required to answer these questions which were beyond the scope of this study.
In conclusion, this study showed that SBP with perioperative IV antibiotics has a significant impact on the postoperative composition of the gut microbiome following colon and rectal surgery. Although SBP represents a critical tool that has been associated with less intestinal microbial-driven complications, this mechanism of action via the microbiome remains unclear and requires further investigation. While effective, SBP remains a shotgun approach that does not consider the patient’s native microbiome, thus hindering a personalized approach to optimizing patient outcomes following surgery. The eradication of the intestinal microbiome acutely following surgery may represent a unique opportunity to intervene and sets forth a premise for the re-introduction of critical commensal bacteria that contribute to gut health and recovery at a time when the patient needs it most.
Methods
Patient cohort
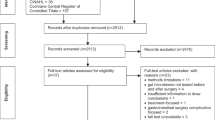
A total of 30 adult patients were recruited from March 2019 through October 2020 and underwent either colonoscopy (n = 15) or elective colorectal surgery (n = 15) at the University of Minnesota Medical Center. Fecal samples were obtained pre-procedural or preoperatively (T<0, mean 6 [1–33] days), intra-procedural or intraoperative (T0), post-procedure or postoperative within 10 days (T10, mean 3 [1–13] days), within 3–6 weeks (T30, mean 31 [16–43] days), and at 6 months (T180, mean 199 [188–246] days). Colonoscopy patients underwent MBP alone, while surgery patients underwent SBP composed of MBP with OA and 24 h of postoperative IV antibiotics. MBP included Miralax (238 g) plus Magnesium Citrate (296 mL; n = 27), GoLYTELY (236 g; n = 1), or two fleet enemas (n = 2). Oral antibiotics included neomycin (1 g q6h for 3 doses) plus metronidazole (500 mg q6h for 3 doses; n = 15), given with prophylactic Zofran (4 mg q6h for 3 doses) as an anti-nausea measure, given our previous experience with frequent nausea and vomiting thought to be caused by oral metronidazole. Perioperative IV antibiotics were initiated 1–2 h before incision and continued for up to 24 h postoperative and included ciprofloxacin (400 mg q12h) plus metronidazole (500 mg q8h; n = 10), trimethoprim/sulfamethoxazole (800–160 mg q24h) plus metronidazole (500 mg q8h; n = 1), and cefotetan (1–2 g q12h; n = 4) at the discretion of the surgeon. Diet is commonly restricted in patients following surgery. Post-operative diet consisted of clear liquids until evidence of return of bowel function which occurred between one to three days following surgery. Patients were then advanced to a low residue, low fiber diet which was continued for six weeks at which time dietary restrictions were lifted. Exclusion criteria included history of solid or liquid organ transplant, active immunosuppressive medication, chronic steroid use, any chemotherapy 12 months before colonoscopy or surgery, history of intra-abdominal or pelvic radiation, history of inflammatory bowel disease, history of previous colorectal resection, use of any antibiotic 30 days before enrollment, planned diverting ileostomy, and pregnancy. Human fecal specimens were obtained under approval by the Institutional Review Board of the University of Minnesota. Informed written consent was obtained from each study participant before enrollment.
Sample collection
Fecal samples were collected by patients in single-use specimen collector pans and transferred to 30 mL polystyrene fecal specimen containers (Globe Scientific, Inc., Paramus, NJ, USA). Patients stored samples in their home freezers prior to their clinic, procedure, or surgery visit, when samples were transferred to a − 80 °C freezer until use. Intra-procedural or intraoperative samples were collected by the treating surgeon via rigid proctoscopy, flexible sigmoidoscopy, or colonoscopy via endoscopic suction of colonic effluent from the rectum and sigmoid colon with as needed lavage using sterile water or saline solution in cases where no effluent was present in the colon or rectum. Specimens were placed in 30 mL polystyrene fecal specimen containers and immediately transferred to a − 80 °C freezer until processing.
DNA extraction and sequencing
DNA was extracted from 250 mg thawed fecal samples using the DNeasy PowerSoil kit (QIAGEN, Hilden, Germany) on the automated QIAcube platform following the inhibitor removal technology (IRT) protocol. The V4 hypervariable region of the 16S rRNA gene was amplified using the 515F/806R primer set26 by the University of Minnesota Genomics Center (UMGC, Minneapolis, MN, USA), as previously described27. Paired-end, dual-indexed sequencing at a read length of 300 nucleotides (nt) was performed on the Illumina MiSeq platform (Illumina, Inc., San Diego, CA, USA) by UMGC27. Negative sterile water controls were included in all sequencing runs and did not produce amplicons. Raw data were stored in the Sequence Read Archive under BioProject accession number SRP250717.
Bioinformatics
Amplicon sequence data were processed and analyzed using mothur software ver. 1.41.128 with our previously published pipeline for quality screening and taxonomic annotation29. Briefly, reads were paired-end joined, quality trimmed, and aligned against the SILVA database ver. 13830. Sequences were further cleaned using a 2% pre-clustering step31 and chimeric sequences were identified and removed using UCHIMER ver. 4.2.4032. Operational taxonomic units (OTUs) were binned at 99% similarity using the furthest-neighbor algorithm and taxonomic assignment was done against the Ribosomal Database Project ver. 1633. A mean (± standard deviation) of 18,058 ± 10,916 reads per sample were obtained. For unbiased statistical comparisons34, samples were rarefied to 4,500 sequence reads by random subsampling, and samples with fewer sequence reads were removed from the data set. After rarefaction, a mean estimated Good’s coverage of 98.14 ± 0.02% and a mean of 187 ± 90 OTUs were observed among all samples. The number of fecal samples included in comparisons among sample groups at each time point after normalization by rarefaction are shown in Fig. 1.
Sourcetracker2 was used with default parameters to assess the similarity of intra- and post-operative microbial composition of individual patients to their own pre-operative microbiota35. This software uses a Bayesian inference approach to determine what percent of the community of sink samples (intra- and post-operative samples) is derived from source (pre-operative) samples taking an OUT table as input.
Statistical analysis
A power calculation was done using the MicroPower package in R36. This package models OTU tables based on user-defined inputs and determines power to detect differences when using a PERMANOVA test. Communities were modeled based on study data from a pool of 5,000 OTUs among all samples, with 200 OTUs per sample and 25% OTU bin retention. Our sample size powered detection of a small effect size (ω2 = 0.03) at 1 − β = 1.00 and α = 0.05.
Alpha and beta diversity statistics were calculated in mothur. Alpha diversity was evaluated with the Shannon index37, which accounts for richness and evenness. Beta diversity was calculated using Bray–Curtis distances38 and was visualized by ordination using principal coordinate analysis (PCoA)39. Spearman correlations were calculated to determine abundant genera that were significantly associated with PCoA axis position using the corr.axes command in mothur. Differences in taxon abundances over the course of the study were determined using the permuspliner function of SplinectomeR40, a permutation-based package in R that uses weighted local polynomials to test for group differences in longitudinal microbiome data, with multiple time points per subject. The sliding_spliner function of SplinectomeR, a technique that divides the time axis into 100 segments and finds segments with larger contributions to the overall intergroup difference over time for a given taxon, was used to determine whether groups were significantly different at specific time points.
Patient demographic and clinical data were compared using Chi-squared analysis for categorical variables and Mann–Whitney-U test for continuous variables. Differences in Shannon index and SourceTracker analysis were determined using ANOVA with Tukey’s post-hoc test. Community compositions at different time points were compared using analysis of similarity (ANOSIM)41 with Bonferroni correction for pairwise comparisons. Analyses were conducted with XLSTAT (version 2020.2.3; Addinsoft, Belmont, MA, USA). All statistics were evaluated at α = 0.05.
Ethics approval
Approval for this study was given by the University of Minnesota Institutional Review Board (Protocol Number: 00005429). All subjects provided written informed consent for participation in the study and collection and analysis of data. All study procedures were in accordance with the ethical standards of the national research ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Data availability
Sequence data are deposited in the Sequence Read Archive under BioProject accession number SRP250717. Available at: https://www.ncbi.nlm.nih.gov/sra/?term=SRP250717.
Abbreviations
- SSI:
-
Surgical site infections
- POI:
-
Postoperative ileus
- C. difficile :
-
Clostridioides difficile
- MBP:
-
Mechanical bowel preparation
- OA:
-
Oral antibiotics
- SBP:
-
Surgical bowel preparation
- IV:
-
Intravenous
- SCFA:
-
Short-chain fatty acids
- IgA:
-
Immunoglobulin A
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2020. CA. Cancer J. Clin. 70, 145–164 (2020).
Morris, A. M., Regenbogen, S. E., Hardiman, K. M. & Hendren, S. Sigmoid diverticulitis: A systematic review. JAMA 311, 287–297 (2014).
Anaya, D. A. & Flum, D. R. Risk of emergency colectomy and colostomy in patients with diverticular disease. Arch. Surg. 140, 681–685 (2005).
Bernell, O., Lapidus, A. & Hellers, G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann. Surg. 231, 38–45 (2000).
Young, H. et al. Surgical site infection after colon surgery: National healthcare safety network risk factors and modeled rates compared with published risk factors and rates. J. Am. Coll. Surg. 214, 852–859 (2012).
Mulders, R. J. et al. Microbiota in obesity: Interactions with enteroendocrine, immune and central nervous systems. Obes. Rev. 19, 435–451 (2018).
Krezalek, M. A. et al. The intestinal microbiome and surgical disease. Curr. Probl. Surg. 53, 257–293 (2016).
Shogan, B. D. et al. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci. Transl. Med. 7, 286ra68 (2015).
Shogan, B. D. et al. Alterations of the rectal microbiome are associated with the development of postoperative ileus in patients undergoing colorectal surgery. J. Gastrointest. Surg. 24, 1663–1672 (2020).
Poggio, J. L. Perioperative strategies to prevent surgical-site infection. Clin. Colon Rectal Surg. https://doi.org/10.1055/s-0033-1351133 (2013).
Ioannidis, A., Zoikas, A. & Wexner, S. D. Current evidence of combination of oral antibiotics and mechanical bowel preparation in elective colorectal surgery and their impact on anastomotic leak. Surg. Innov. 27, 101–102 (2020).
Charlson, M., Pompei, P., Ales, K. & MacKenzie, C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40, 373–383 (1987).
Krezalek, M. A. et al. Can methicillin-resistant staphylococcus aureus silently travel from the gut to the wound and cause postoperative infection? Modeling the ‘trojan horse hypothesis’. Ann. Surg. 267, 749–758 (2018).
Nalluri, H. et al. Peri-operative antibiotics acutely and significantly impact intestinal microbiota following bariatric surgery. Sci. Rep. 10, 1–10 (2020).
Kommineni, S. et al. Bacteriocin production augments niche competition by enterococci in teh mammalian GI tract. Nature 526, 719–722 (2015).
Rashidi, A. et al. Gut dysbiosis during antileukemia chemotherapy versus allogeneic hematopoietic cell transplantation. Cancer 126, 1434–1447 (2020).
Taur, Y. et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood 124, 1174–1182 (2014).
Taur, Y. et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin. Infect. Dis. 55, 905–914 (2012).
Van Praagh, J. B. et al. Mucus microbiome of anastomotic tissue during surgery has predictive value for colorectal anastomotic leakage. Ann. Surg. 269, 911–916 (2019).
Sokol, H. et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. USA 105, 16731–16736 (2008).
Machiels, K. et al. A decrease of the butyrate-producing species roseburia hominis and faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut 63, 1275–1283 (2014).
Alam, A. et al. The microenvironment of injured murine gut elicits a local pro-restitutive microbiota. Nat. Microbiol. 1, 1–8 (2016).
Wang, Y. et al. Laser capture microdissection and metagenomic analysis of intact mucosa-associated microbial communities of human colon. Appl. Microbiol. Biotechnol. 88, 1333–1342 (2010).
Shogan, B. D. et al. Intestinal anastomotic injury alters spatially defined microbiome composition and function. Microbiome 2, 1–10 (2014).
Janzon, A., Goodrich, J. K., Koren, O., Waters, J. L. & Ley, R. E. Interactions between the gut microbiome and mucosal immunoglobulins A, M, and G in the developing infant gut. mSystems 4, 1–17 (2019).
Caporaso, J. G. et al. Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. ISME J. 6, 1621–1624 (2012).
Gohl, D. M. et al. Systematic improvement of amplicon marker gene methods for increased accuracy in microbiome studies. Nat. Biotechnol. 34, 942–949 (2016).
Schloss, P. D. et al. Introducing mothur: Open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl. Environ. Microbiol. 75, 7537–7541 (2009).
Staley, C. et al. Predicting recurrence of Clostridium difficile infection following encapsulated fecal microbiota transplantation. Microbiome 6, 166 (2018).
Pruesse, E. et al. SILVA: a comprehensive online resource for quality checked and aligned ribosomal RNA sequence data compatible with ARB. Nucleic Acids Res. 35, 7188–7196 (2007).
Huse, S. M., Welch, D. M., Morrison, H. G. & Sogin, M. L. Ironing out the wrinkles in the rare biosphere through improved OTU clustering. Environ. Microbiol. 12, 1889–1898 (2010).
Edgar, R. C., Haas, B. J., Clemente, J. C., Quince, C. & Knight, R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics 27, 2194–2200 (2011).
Cole, J. R. et al. The Ribosomal Database Project: improved alignments and new tools for rRNA analysis. Nucleic Acids Res. 37, D141–D145 (2009).
Gihring, T. M., Green, S. J. & Schadt, C. W. Massively parallel rRNA gene sequencing exacerbates the potential for biased community diversity comparisons due to variable library sizes. Environ. Microbiol. 14, 285–290 (2012).
Knights, D. et al. Bayesian community-wide culture-independent microbial source tracking. Nat. Methods 8, 761-U107 (2011).
Kelly, B. J. et al. Power and sample-size estimation for microbiome studies using pairwise distances and PERMANOVA. Bioinformatics 31, 2461–2468 (2015).
Shannon, C. E. & Weaver, W. The Mathematical Theory of Communication (The University of Illinois Press, 1949).
Bray, J. R. & Curtis, J. T. An Ordination of the Upland Forest Communities of Southern Wisconsin. Ecol. Monogr. 27, 325 (1957).
Anderson, M. J. & Willis, T. J. Canonical analysis of principal coordinates: A useful method of constrained ordination for ecology. Ecology 84, 511–525 (2003).
Shields-Cutler, R. R., Al-Ghalith, G. A., Yassour, M. & Knights, D. SplinectomeR enables group comparisons in longitudinal microbiome studies. Front. Microbiol. 9, 785 (2018).
Clarke, K. R. Non-parametric multivariate analyses of changes in community structure. Aust. J. Ecol. 18, 117–143 (1993).
Acknowledgements
Sequence processing and analysis were done using the resources of the Minnesota Supercomputing Institute.
Funding
This study was funded by the Hubbard Family private fund for advancing treatment practices to improve patient outcomes in colorectal surgery (fund 21692 – University of Minnesota).
Author information
Authors and Affiliations
Contributions
H.N., M.C.B., J.N., and S.B. did patient screening, sample coordination and processing, and data analysis. R.E., G.M.M., R.M., C.J., and W.B.G. acquired patient consent and provided clinical oversight. H.N. and M.C.B. drafted the manuscript. C.S. did bioinformatics processing. M.C.B., C.S., and W.B.G. designed the study. C.J., C.S., and W.B.G. directed research and contributed to analysis and writing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Wolfgang Gaertner is a consultant and proctor for Intuitive Surgical, a consultant and M.D. advisory board member of Coloplast and BD, and a consultant for Applied Medical. All remaining authors declare no competing of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nalluri-Butz, H., Bobel, M.C., Nugent, J. et al. A pilot study demonstrating the impact of surgical bowel preparation on intestinal microbiota composition following colon and rectal surgery. Sci Rep 12, 10559 (2022). https://doi.org/10.1038/s41598-022-14819-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-14819-1
This article is cited by
-
Effect of the gut microbiota and their metabolites on postoperative intestinal motility and its underlying mechanisms
Journal of Translational Medicine (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.