Abstract
Globally, 43 million people are living with HIV, 90% in developing countries. Increasing life expectancy with combination antiretroviral therapy (cART) results in chronic complications, including HIV-associated neurocognitive disorders (HAND) and eye diseases. HAND screening is currently challenging. Our aim was to evaluate clinical utility of retinopathy as a screening measure of HAND in older cART-treated individuals in Tanzania and feasibility of smartphone-based retinal screening in this low-resource setting. A cross-sectional systematic sample aged ≥ 50-years attending routine HIV follow-up in Tanzania were comprehensively assessed for HAND by American Academy of Neurology criteria and received ophthalmic assessment including smartphone-based retinal imaging. HAND and ophthalmic assessments were independent and blinded. Diagnostic accuracy was evaluated by AUROC curves. Of 129 individuals assessed, 69.8% were visually impaired. Thirteen had retinopathy. HAND prevalence was 66.7%. Retinopathy was significantly associated with HAND but HIV-disease factors (CD4, viral load) were not. Diagnostic accuracy of retinopathy for HAND was poor (AUROC 0.545-0.617) but specificity and positive predictive value were high. We conclude that ocular pathology and HAND appear highly prevalent in this low-resource setting. Although retinal screening cannot be used alone identify HAND, prioritization of individuals with abnormal retinal screening is a potential strategy in low-resource settings.
Similar content being viewed by others
Introduction
Almost 43 million people are infected by the human immunodeficiency virus (HIV) globally, with 90% of cases in developing countries1. In sub-Saharan Africa (SSA), almost 25 million individuals currently live with HIV2. Increasing provision of combination antiretroviral therapy (cART) is resulting in both improving life expectancy and emergence of chronic HIV-related complications and chronic diseases as previously seen in high-income countries. HIV-associated neurocognitive disorders (HAND) affect up to 50% of people treated for HIV and are associated with increased morbidity and mortality3,4. HAND are classified by severity: asymptomatic neurocognitive impairment (ANI); mild neurocognitive disorder (MND) and; HIV-associated dementia (HAD)5. Early identification of HAND and subsequent prompt initiation of treatment, prior to progression of HAND stage, may reduce mortality and reverse neurocognitive deficits3. Screening for, and identification of HAND are currently challenging, in SSA and elsewhere. Difficulties include shortage of neurology and psychiatry specialist services in SSA, lack of accurate brief screening measures6 and current consensus diagnostic criteria requiring detailed neuropsychological assessment, impractical in busy clinical settings. Additionally, the use of mobile technologies to help address health and human resource shortages in low-resource settings is a recent and expanding area of research and has previously been evaluated for use in remote grading of ophthalmic disease in SSA7.
HIV-associated eye diseases occur in up to 70% of HIV positive individuals8. Early recognition and treatment can prevent or cure 80% of cases9. Features observed in the retina may provide insight about the systemic health of individuals10, such as in previous studies where ophthalmoscopy identified biomarkers of hypertension and its severity11. Vascular diseases are also common amongst older people living with HIV, and are often undertreated in SSA12. There appears to be a strong association between HIV and vasculopathies such as stroke13, and renal disease14 and retinal disease15. Retinal vascular changes has been shown to positively correlate with white matter microstructural changes observed using magnetic resonance imaging in non-HIV positive patients10. As white matter disease is also seen in both treated and untreated HIV cases and is associated with HAND16,17, we hypothesized that retinal imaging could help identify individuals at risk of HAND.
In this study we aimed to determine the clinical utility of retinopathy as a potential predictive biomarker of HIV-associated neurological complications in older cART-treated HIV positive individuals in Tanzania. A second objective was to determine if retinopathy could be a potential alternative to detailed neuropsychological assessment in a resource poor setting. In addition, we aimed to determine if remote retinal screening using a smartphone based retinal camera was a potentially useful strategy in this context.
Methods
A cross-sectional study at a single government-funded HIV clinic in Northern Tanzania.
Participant selection
This study was nested within a larger study of HAND prevalence within the clinic. For the larger study, a systematic sampling methodology was employed. Depending on daily predicted clinic attendance numbers, every second or third routine follow-up patient was systematically selected to take part in the study in order of arrival at the clinic. Participants underwent detailed neurocognitive and clinical assessment. Criteria for inclusion were: ≥ 50-years of age, HIV-positive, attending routine follow up and not acutely unwell. For this ophthalmic sub-study, all recruited participants were offered a subsequent ophthalmic assessment. Due to a wish to avoid participant burden and fatigue, ophthalmic imaging took place at a separate appointment with transport costs refunded and refreshments provided. Those who could not attend, or refused this additional appointment were excluded from the ophthalmic sub-study.
Informed consent
The purpose for the study and their specific involvement was explained to each potential participant and written informed consent was obtained. Where capacity was in doubt, consent was obtained from close relatives. Ethical approval was obtained from the National Institute for Medical Research (NIMR/HQ/R.8a/Vol. IX/21.36) and Kilimanjaro Christian Medical University College Research Ethics Committee (n.896). This study abides by the tenets of the declaration of Helsinki.
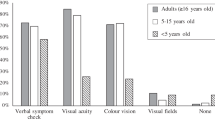
Assessment
Baseline sociodemographic data of participants, plus HIV disease severity data from standard data sheets, were collected (Table 4 in Appendix). A set of functional assessments were used, including Karnofsky Performance Status18, Rockwood Clinical Frailty Scale19, and Intervention for Dementia in Elderly Africans (IDEA) low-literacy brief cognitive screen, previously validated for dementia in SSA20. Hypertensive and diabetic status were recorded. We did not ask about illicit drug use for this study, as our previous study in this same older age group from the same clinic (n = 253) found no participant reported illicit drug use on the MINI screen and local clinicians advised this question to be inappropriate in an older population21. Alcohol history was obtained as previous studies did report alcohol use in this population. Visual acuity (Va) was assessed with available correction using the Landolt broken-ring low-literacy “C” chart with notations for testing at 3 m due to unknown rates of illiteracy amongst the study participants. Visual fields were tested using confrontation (quadrant finger counting) and colour vision with Ishihara charts.
All participants underwent direct ophthalmoscopic examination following pupil dilatation (1% tropicamide) and retinal images were obtained using the iNview retinal camera (VOLK, Cleveland, USA). This retinal camera attached to an iPhone 6 (8-megapixel iSight camera with 1.5µ pixels) was used throughout the study. The red-light reflex was observed and maintained throughout approaching the patient until focused on the retina, much like fundoscopy. Images were then taken automatically by the retinal camera. Images were independently reviewed by 3 ophthalmologists, 2 of whom were based in Tanzania (JR, LU) and 1 from the UK (JH).
HAND assessment and diagnosis
HAND was diagnosed by consensus using AAN 2007 gold standard criteria5 based on neuropsychological battery measures validated for cross-cultural use by the WHO, clinical/neurological examination findings, to determine if other psychiatric disorders better explained cognitive performance, and a collateral history from a close relative or friend. All participants underwent additional detailed locally-validated low-literacy neuropsychological tests of cortical function, the details of which have previously been published6. Domains assessed included working memory, verbal memory (learning, delayed recall and recognition memory), fine motor control, motor speed, visuoconstruction, executive function and comprehension. Data were collected in a separate room by research assistants and nurses who had been specifically trained, had previous experience and an annual update and harmonization of methods process lasting one week. Research assistants were blinded to whether patients had retinopathy. Practice trials and errors were managed according to a standardized protocol and tests selected were validated locally and/or in low literacy SSA settings. Neuropsychological test results were compared to performance means for those with and without 4 years of formal education generated in 2016 from a comparison group of similar age and education level attending the ophthalmology outpatient department of MRRH6,21. The collateral history and all clinical and neuropsychological information was used for a multi-disciplinary discussion of each participant by the research team to confirm diagnoses and record a detailed case summary. Diagnoses were confirmed or refuted by consensus panel of specialists in old age psychiatry with experience of HAND diagnosis.
Ophthalmologist criteria for defining eye disease
The definitions for visual impairment used followed those given in the National Sensory Impairment Partnership’s Framework22. Mild-moderate visual impairment was defined as LogMAR 0.3 < Va ≤ 0.8 and severe visual impairment was defined as LogMAR Va > 0.8. “glaucoma suspect” was termed if cup-to-disc ratio was > 0.623. A Tanzania-based ophthalmology trainee (JR) determined whether glaucoma could be diagnosed based on ICD-10 criteria23. Retinopathy was assumed if any of the following features were observed upon ophthalmoscopy: retinal haemorrhages; microaneurysms; areas of capillary non-perfusion; or cotton wool spots.
Statistical analysis
All statistical analyses were performed using IBM SPSS software V24.0. Normally distributed data were described using mean, standard deviation (SD) and 95% confidence intervals (CI). To assess the independent influence of age, gender, HIV severity, functional status, HAND severity and visual change on retinopathy status, univariate and multivariable logistic regression models were developed with retinopathy as the dependent (outcome) variable. Comparisons were made using independent t-tests. Non-normally distributed data were described using median, interquartile range (IQR) and frequency and compared using Mann–Whitney U test. Categorical variables were described using frequency and compared using chi-squared test and with the Fisher’s exact test correction where appropriate. The statistically significant variables were then considered as independent variables in a multivariable model examining their relationship to the outcome. A stepwise, backwards approach to model building was employed, based on their likelihood ratio. Only significant variables were retained in the final model. The validity and robustness of the model was checked by examining studentized residuals, eigenvalues and the tolerance. Statistical significance was defined as P ≤ 0.05.
The performance of the smartphone HIV retinopathy screen was investigated using Area Under the Receiver Operating Characteristic (AUROC) curve analysis. Diagnostic accuracy was analysed for HAND and symptomatic HAND (s-HAND, MND/HAD). To determine diagnostic accuracy for HAND, ANI/MND/HAD were coded 1 and all others coded 0. For S-HAND, MND/HAD were coded 1, and all others 0. Diagnostic accuracy was also analysed for HIV stage 3 or 4 coded as 1 and all others coded 0 as well as analysed for detectable viral load coded as 1 and undetectable as 0. When grouped together, the predictive value retinopathy to determine late HIV stage, detectable viral load as well as HAND and s-HAND was analysed.
Ethics approval and consent to participate
The purpose for the study and their specific involvement was explained to each potential participant and written informed consent was obtained. Where capacity was in doubt, consent was obtained from close relatives. Ethical approval was obtained from the National Institute for Medical Research (NIMR/HQ/R.8a/Vol. IX/21.36) and Kilimanjaro Christian Medical University College Research Ethics Committee (n.896).
Results
Population characteristics
Of the 762 individuals aged ≥ 50 years attending follow-up during the study period, 145 were systematically sampled and consented to inclusion. Of these, 129 completed the ophthalmologic assessment and had complete data (Fig. 1). One was unable to complete imaging due to discomfort. There was no significant difference in age, CD4 count or viral load between those who had complete data and those who did not.
Median patient age was 56 years (IQR: 53–61), 83 (64.3%) were female, 88 (68.2%) self-reported at least 5–7 years of primary-school education and 8 (6.2%) were illiterate. Median time since HIV diagnosis was 10.5 years (Range: 3 months to 23 years) and median nadir CD4 count was 168 cells/mm3 (IQR: 106–251). All but one participant was receiving antiretroviral treatment when enrolled in the study. HIV-disease appeared well managed with current median CD4 434 cells/mm3 and 76% with suppressed HIV viral load (defined as < 20 copies/ml). Twenty-one (16.3%) reported a prior hypertension diagnosis, 11 (52.4%) of whom were on anti-hypertensives. Thirty-eight (29.5%) of patients were hypertensive in clinic (blood pressure (BP) > 140/90 mm of mercury (mmHg). The mean BP in clinic was 134.5/81.2 mmHg with a maximum systolic of 219 mmHg. Seven (5.4%) patients reported being diabetic, 5 (71.4%) of whom were on treatment.
Forty-three patients (33.3%) did not meet HAND criteria, 41 (31.8%) met criteria for ANI, 43 (33.3%) met criteria for MND and 2 patients (1.6%) were diagnosed with HAD.
Overall prevalence of ophthalmic disease
Recent visual changes were self-reported by 71 patients (55%), but none reported having sought ophthalmological review.
Fifty-three patients (41.1%, 95% CI 32.6–49.6) had mild-moderate visual impairment (0.3 < Va ≤ 0.8) and 37 (28.7%, 95% CI 20.9–36.5) severe visual impairment (Va > 0.8). Six (4.7%) had a visual field defect, 4 (3.1%) cataracts and 5 (3.9%) abnormal colour vision. The cataracts were not considered too dense to prevent visualization of the retina. Fifty-eight patients (45%) had Va > 0.6 and abnormal fundal signs were seen in 53 patients (41.1%), including 16 (12.4%) referred for suspected glaucoma and 6 (4.7%) for suspected HIV retinopathy. One showed signs consistent with cytomegalovirus retinitis. Once reviewed by an ophthalmology specialist (JH), retinopathy was suspected in 13 patients (10.1%) and glaucoma was suspected in 19 patients (14.7%) (CDR > 0.6) but following diagnostic assessments only one patient was diagnosed with bilateral primary angle closure glaucoma. Sixty-seven patients (51.9%) were referred for full ophthalmic assessment.
HIV retinopathy and its association with HAND
Features of retinopathy were significantly associated with both HAND diagnosis and HAND severity (Table 1). Retinopathy was associated with patient-reported vision loss during the previous 3 months (χ2(1, n = 129): 5.111; p = 0.037).
Using logistic regression, HAND severity and self-reported visual change were assessed for significance against retinopathy. The significance intervals, odds ratios and confidence intervals are shown in Table 2. This shows HAND severity is associated with retinopathy, adjusting for co-variates (Nagelkerke R2 = 0.197, Hosmer and Lemeshow goodness of fit, X2 (4) = 0.647, p = 0.958).
Diagnostic accuracy
The predictive value of retinopathy for HAND, s-HAND, late HIV stage and detectable viral load are presented in Table 3. Overall diagnostic accuracy was poor. AUROC ranged from 0.545–0.617, with 95% CI spanning 0.5 for each variable. Specificity was high throughout whereas sensitivity was low. Positive predictive value (PPV) was high for HAND and HIV stage 3 whereas PPV for s-HAND and detectable VL was low. Of all the screening options evaluated, the highest screening accuracy was achieved for HAND using retinopathy screen (AUROC = 0.617, sensitivity 13.4%, specificity 95.7% and PPV 0.846).
Discussion
Our findings suggest that retinopathy may be associated with HAND in older adults receiving long term HIV treatment in this setting. However, identification of retinopathy does not appear to be a useful strategy for identifying those with HAND, or those with frailty. AUROC was not performed on clinical frailty scale as there was no statistically significant association with retinopathy. The high specificity of retinopathy screening may have implications for clinical practice because retinal imaging may show potential to ‘rule in’ which individuals with HIV are likely to be at risk of cognitive impairment. Those negative for retinopathy, have a higher probability of not meeting HAND criteria (normal cognition). In addition, a negative retinopathy assessment does not reliably exclude HAND. This means that retinopathy screening cannot be used alone to determine who might need assessment for HAND. However, retinal screening could allow staff to prioritize individuals with retinal signs, due to high PPV.
Although the relationship between retinopathy and HAND is unclear, there are commonalities in the pathogeneses of both HIV-related complications which may explain their relationship. HIV retinopathy most likely occurs secondary to microvasculopathy from either immune complex deposition, increased plasma viscosity or vascular endothelium invasion by HIV, opportunistic infections or malignancy24. HAND occurs through a number of mechanisms including opportunistic central nervous system (CNS) infections, direct neurotoxic effect of the HIV virus and neurotoxic effect of cART4. Contributory factors include HIV disease severity, accelerated vascular disease and frequent co-morbidities4.
The World Health Organization (WHO) advocates that screening for mental disorders be integrated into chronic disease monitoring to address the shortage of specialist personnel in low-resource settings25. Eye disease is currently a major cause of morbidity and disability in both HIV and non-HIV populations and disproportionately affects older people26. Cataracts, glaucoma, uncorrected refractive error and trauma are the major reported causes of visual impairment26. Identification and screening for ophthalmic disease in low-resource settings is currently challenged by similar issues to those noted for chronic complications of HIV. These include lack of specialist personnel, particularly in rural and remote areas, a focus on acute intervention rather than primary care and prevention, lack of integrated referral systems and access to affordable necessary equipment27,28.
Using mobile technologies to help address health and human resource shortages in low-resource settings is a recent and expanding area of research and is increasingly feasible given the rapid increase in smartphone use across SSA29. Low-cost smartphone applications have been evaluated for use in remote grading of ophthalmic disease in SSA7. Non-clinical imagers were able to capture images at a standard that enabled remote grading at the level of a desktop retinal camera7. In some regions of SSA there is only one ophthalmologist per 2.5 million people, so remote retinal imaging could ameliorate the impact of understaffing30.
In this study, we demonstrate a high prevalence of visual impairment in our study participants of HIV-positive patients, with 41.1% having mild-moderate visual impairment and 28.7% severe visual impairment. A previously published study reported that 11.2% of HIV-positive individuals aged 18 years or greater had a visual acuity of 0.2 or more in at least one eye31. One previous study in HIV-negative individuals aged 50 or greater report visual impairment of 13.6% in SSA32. Our prevalence was much higher. This difference may relate to our study participants being 50 years or older whereas other studies investigated younger sample. In addition, other explanations may include a risk of false positives from unidentified refractive causes of acuity loss, a lower threshold for diagnosis of visual impairment or our small sample size31. Factors relating to the willingness of patients to present with ophthalmic features may also contribute, perhaps due to lack of symptom knowledge, cost or impaired cognition. Since there is a high prevalence of eye disease in this study population, it is prudent to screen for it.
We suspect the high prevalence of visual impairment may be seen also in the background local population, due to lack of routine eye tests and low patient presentation, even when high quality, affordable services are available33. Rates of visual impairment in the remote and rural areas may in fact be worse than those regularly attending hospital due to cost and availability of transport. In addition, low-cost retinal imaging may enable the effective monitoring of patients with HIV-associated ophthalmic diseases and could address challenges in healthcare provision relating to the limited availability of healthcare professionals in these regions30.
Strengths and limitations of the study
To our knowledge, this is the only study on HIV retinopathy in Tanzania, thus providing unique data on visual impairment and ocular disease prevalence. Previous studies looking at disease amongst HIV-infected individuals in SSA, excluded patients with confusion or altered mental state31. Since this study was able to assess the link between HIV ophthalmic diseases and HAND, this was an additional strength.
There are several limitations to this study. Images obtained from VOLK iNview retinal camera were of low-to-moderate quality so subtle changes or more complex pathologies may have been missed. Therefore, there is a substantial reliance on external referrals to ensure a correct diagnosis is made.
There are non-HIV causes of the fundal signs used to define retinopathy, such as hypertensive and diabetic retinopathy. A large proportion of our study participants had a blood pressure over 140 mmHg, however ‘white-coat effect’ is relatively common in SSA34. Seven of the 13 (53.8%) suspected HIV retinopathy patients had hypertension in clinic; we cannot exclude hypertensive retinopathy in these individuals. Despite individuals not self-reporting as diabetic and being under regular clinic follow-up, we found that 9 patients had glycosuria, a clinical sign of undiagnosed or untreated diabetes. 5 of these 9 had retinal signs thought to be consistent with HIV retinopathy but without measuring HbA1c, we cannot exclude diabetic retinopathy in these individuals.
In addition, dementia and cognitive impairment might have in fact been due to other causes, such as vascular dementia, Parkinson’s disease dementia or alcohol related. To minimize this, however, the consensus diagnosis process considered these alternative differential diagnoses, taking into account the neurological examination, history, risk factors and cognitive profile. Those diagnosed with HAND met HAND criteria, following consensus panel review.
This research only relates to HIV positive adults aged 50-years or older. This may be a strength in that studies of this older cART-treated population are few in SSA, but limits generalizability.
Conclusions and recommendations for future work
Ocular pathology and HAND were both common in this patient population. We demonstrate that retinopathy is associated with the presence of HAND. This has implications for clinical practice as retinal imaging may have ‘rule in’ value in predicting which individuals with HIV are likely to be at risk of cognitive impairment and so could be used as a potential alternative to detailed neuropsychological assessment. Substantial clinical need for low-resource screening tools for HAND has been identified and although retinal screening cannot be used alone to determine who might need assessment for HAND, it may offer healthcare professionals a tool to enable patient prioritization and so therefore using a smartphone based retinal camera may potentially be a useful strategy in this context.
As early diagnosis of ocular pathology is crucial to allow for timely intervention, portable and affordable tools which image the retina and enable remote diagnosis and monitoring of ophthalmic conditions in HIV-positive individuals. As technology develops, such assessments will become more accurate and useful.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANI:
-
Asymptomatic neurocognitive impairment
- AUROC:
-
Area under receiver operating characteristic
- BP:
-
Blood pressure
- CI:
-
Confidence intervals
- CNS:
-
Central nervous system
- HAD:
-
HIV-associated dementia
- HAND:
-
HIV-associated neurocognitive disorder
- HIV:
-
Human Immunodeficiency Virus
- IDEA:
-
Intervention for dementia in elderly Africans
- IQR:
-
Interquartile range
- mmHg:
-
Millimetres of mercury
- MND:
-
Mild neurocognitive disorder
- PPV:
-
Positive predictive value
- SD:
-
Standard deviations
- SSA:
-
Sub-Saharan Africa
- s-HAND:
-
Symptomatic HAND
- Va:
-
Visual acuity
- WHO:
-
World health organisation
References
World Health Organization, UNAIDS, UNICEF. Global HIV/aids response: epidemic update and health sector progress towards universal access: Progress report. Published online 2011:224.
Kharsany, A. B. M. & Karim, Q. A. HIV infection and AIDS in Sub-Saharan Africa: Current status, challenges and opportunities. Open AIDS J. 10, 34–48. https://doi.org/10.2174/1874613601610010034 (2016).
Saylor, D., Nakigozi, G., Nakasujja, N., et al. HIV-associated Neurocognitive Disorder leads to Death. In: Hand: Biomarkers, Risks, Prevalence. 2019:99733. https://2jg4quetidw2blbbq2ixwziw-wpengine.netdna-ssl.com/wp-content/uploads/sites/2/posters/2019/1430_Sacktor_0425.pdf
Clifford, D. B. & Ances, B. M. HIV-associated neurocognitive disorder. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(13)70269-X (2013).
Antinori, A. et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology 69(18), 1789–1799. https://doi.org/10.1212/01.WNL.0000287431.88658.8b (2007).
Kellett-Wright, J. et al. Screening for HIV-associated neurocognitive disorder (HAND) in adults aged 50 and over attending a government HIV clinic in Kilimanjaro, Tanzania: Comparison of the international HIV dementia scale (IHDS) and IDEA six item dementia screen. AIDS Behav. 25, 542. https://doi.org/10.1007/s10461-020-02998-9 (2020).
Bastawrous, A. et al. Clinical validation of a smartphone-based adapter for optic disc imaging in Kenya. JAMA Ophthalmol. 134(12), 151–158. https://doi.org/10.1001/jamaophthalmol.2015.4625 (2016).
Chiotan, C. et al. Posterior segment ocular manifestations of HIV/AIDS patients. J. Med. Life. 7(3), 399–402 (2014).
World Health Organization. Blindness and visual impairment. Published 2018. https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. Accessed 03 July 2019.
Mutlu, U. et al. Retinal microvasculature and white matter microstructure: The Rotterdam Study. Neurology 87(10), 1003–1010. https://doi.org/10.1212/WNL.0000000000003080 (2016).
Jones, R. et al. Retinal imaging to identify target organ damage in older Africans: A pilot study. J. Clin. Hypertens. (Greenwich) 20(9), 1296–1301. https://doi.org/10.1111/jch.13352 (2018).
Benjamin, L. A. et al. HIV, antiretroviral treatment, hypertension, and stroke in Malawian adults. Neurology 86(4), 324–333. https://doi.org/10.1212/WNL.0000000000002278 (2016).
Walker, R. W. et al. Stroke risk factors in an incident population in urban and rural Tanzania: A prospective, community-based, case-control study. Lancet Glob. Health 1(5), 282–285. https://doi.org/10.1016/S2214-109X(13)70068-8 (2013).
Naftalin, C., Nathan, B., Hamzah, L. & Post, F. A. HIV-associated kidney disease in the context of an aging population. Sexual Health. 8(4), 485–492. https://doi.org/10.1071/sh10146 (2011).
Lima, B. Ophthalmic manifestations of HIV infection. Digital J. Ophthalmol. 10(3) (2004). http://www.djo.harvard.edu/site.php?url=/physicians/oa/674. Accessed 10 June 2019.
Hoare, J. et al. Clinical associations of white matter damage in cART-treated HIV-positive children in South Africa. J. Neurovirol. 21(2), 120–128. https://doi.org/10.1007/s13365-014-0311-1 (2015).
Alakkas, A. et al. White matter damage, neuroinflammation, and neuronal integrity in HAND. J. Neurovirol. 25(1), 32–41. https://doi.org/10.1007/s13365-018-0682-9 (2019).
Sperduto, P. W. et al. Summary report on the graded prognostic assessment: An accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J. Clin. Oncol. 30(4), 419–425. https://doi.org/10.1200/JCO.2011.38.0527 (2012).
Church, S., Rogers, E., Rockwood, K. & Theou, O. A scoping review of the clinical frailty scale. BMC Geriatr. 20(1), 1–18. https://doi.org/10.1186/s12877-020-01801-7 (2020).
Paddick, S. M. et al. Validation of the identification and intervention for dementia in elderly africans (IDEA) cognitive screen in Nigeria and Tanzania. BMC Geriatr. 15(1), 1–9. https://doi.org/10.1186/s12877-015-0040-1 (2015).
Flatt, A. et al. Prevalence and 1-year incidence of HIV-associated neurocognitive disorder (HAND) in adults aged ≥50years attending standard HIV clinical care in Kilimanjaro, Tanzania. Int. Psychogeriat. 1, 6 (2021).
Bowles, M., Bramhall, J., & Couch, D., et al. Eligibility framework for scoring support levels (2017). https://www.natsip.org.uk/doc-library-login/eligibility-framework/00-eligibility-framework-summer-2017-edition/916-eligibility-framework-document/file.
ICD-10 Glaucoma reference guide (2019).
Feroze, K., & Gulick, P. HIV retinopathy. StatPearls Publishing; 2019. https://www.ncbi.nlm.nih.gov/books/NBK470530/.
World Health Organization and Calouste Gulbenkian Foundation. Integrating the response to mental disorders and other chronic diseases in health care systems. Geneva, World Health Organization. Published online 2014:1–50. http://apps.who.int/iris/bitstream/10665/112830/1/9789241506793_eng.pdf?ua=1.
Pascolini, D. & Mariotti, S. P. Global estimates of visual impairment: 2010. Br. J. Ophthalmol. 96(5), 614–618. https://doi.org/10.1136/bjophthalmol-2011-300539 (2012).
Sommer, A. et al. Challenges of ophthalmic care in the developing world. JAMA Ophthalmol. https://doi.org/10.1001/jamaophthalmol.2014.84 (2014).
International Agency for the Prevention of Blindness. Human Resources for Health Strategy Consultation. Vol 126 (2014). http://www.who.int/workforcealliance/media/news/2014/7InternationalAgencyPreventionBlindness.pdf. Accessed 13 July 2019.
Betjeman, T. J., Soghoian, S. E., & Foran, M. P. mHealth in Sub-Saharan Africa (2013).
Resnikoff, S. et al. Estimated number of ophthalmologists worldwide (International Council of Ophthalmology update): Will we meet the needs?. Br. J. Ophthalmol. 104(4), 588–592. https://doi.org/10.1136/bjophthalmol-2019-314336 (2020).
Otiti-Sengeri, J. et al. The prevalence and causes of visual loss among HIV-infected individuals in Uganda. J. Acquir. Immune Defic. Syndr. 53(1), 95–101. https://doi.org/10.1097/QAI.0b013e3181c313f0 (2010).
Mathenge, W., Bastawrous, A., Foster, A. & Kuper, H. The Nakuru posterior segment eye disease study: Methods and prevalence of blindness and visual impairment in Nakuru, Kenya. Ophthalmology https://doi.org/10.1016/j.ophtha.2012.04.019 (2012).
Lewallen, S. et al. Increasing cataract surgery to meet Vision 2020 targets; experience from two rural programmes in east Africa. Br. J. Ophthalmol. 89(10), 1237–1240. https://doi.org/10.1136/bjo.2005.068791 (2005).
Ivy, A. et al. Ambulatory blood pressure monitoring to assess the white-coat effect in an elderly east african population. J. Clin. Hypertens. 17(5), 389–394. https://doi.org/10.1111/jch.12501 (2015).
Acknowledgements
We thank research assistants and coordinators: Dr Sengua Koipapi, Dr Jane Rogathi, Mr Aloyce Kisoli, Mr Dennis Clement, Ms Cecilia Chuwa, Ms Happiness Mosha alongside all staff, patients and carers attending Mawenzi Regional Referral Hospital HIV care and treatment centre and the MRRH hospital management for accommodating and hosting the study.
Funding
This work was supported by an Academy of Medical Sciences (AMS) start-up grant awarded to Dr Paddick.
Author information
Authors and Affiliations
Contributions
G.G. prepared the literature review, completed the study and wrote the first draft of the paper, assisted by D.M. H.J.H. analysed retinal imaging. J.B., S.U., J.R., L.U., C.B., G.H. and E.R. helped in study set up, protocol development and running of the study. R.W., W.G. and S.M.P. led on study design and concept, supervised and directed study implementation and supervised G.G. and D.M. in writing the paper. All authors approved the final manuscript submitted for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
George, G., Murphy, D.C., Hogg, H.D.J. et al. Evaluation of a low-resource screening strategy for ophthalmic pathologies and associated neurological morbidity in an older Tanzanian HIV-positive population. Sci Rep 12, 1434 (2022). https://doi.org/10.1038/s41598-022-04989-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-04989-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.