Abstract
Local and general anesthesia are the main techniques used during percutaneous kyphoplasty (PKP); however, both are associated with adverse reactions. Monitored anesthesia with dexmedetomidine may be the appropriate sedative and analgesic technique. Few studies have compared monitored anesthesia with other anesthesia modalities during PKP. Our aim was to determine whether monitored anesthesia is an effective alternative anesthetic approach for PKP. One hundred sixty-five patients undergoing PKP for osteoporotic vertebral compression fractures (OVCFs) were recruited from a single center in this prospective, non-randomized controlled study. PKP was performed under local anesthesia with ropivacaine (n = 55), monitored anesthesia with dexmedetomidine (n = 55), and general anesthesia with sufentanil/propofol/sevoflurane (n = 55). Perioperative pain was assessed using a visual analogue score (VAS). Hemodynamic variables, operative time, adverse effects, and perioperative satisfaction were recorded. The mean arterial pressure (MAP), heart rate, VAS, and operative time during monitored anesthesia were significantly lower than local anesthesia. Compared with general anesthesia, monitored anesthesia led to less adverse anesthetic effects. Monitored anesthesia had the highest perioperative satisfaction and the lowest VAS 2 h postoperatively; however, the monitored anesthesia group had the lowest MAP and heart rate 2 h postoperatively. Based on better sedation and analgesia, monitored anesthesia with dexmedetomidine achieved better patient cooperation, a shorter operative time, and lower adverse events during PKP; however, the MAP and heart rate in the monitored anesthesia group should be closely observed after surgery.
Similar content being viewed by others
Introduction
Percutaneous kyphoplasty (PKP) is a safe and effective minimally invasive surgical treatment for osteoporotic vertebral compression fractures (OVCFs)1,2. Because of the rapid onset, precision, and cost-effectiveness, local anesthesia has been widely used during PKP. Nevertheless, local anesthetics cannot be injected into the vertebral body, thus, some patients experience severe pain that can even be intolerable, especially during PKP, which is more complex than percutaneous vertebroplasty3. General anesthesia is an important medical application that is used during PKP to provide a comfortable surgical condition for both patients and physicians; however, general anesthesia is likely to increase the risk of anesthetic adverse effects, hospital stay, and costs4. In recent years, dexmedetomidine, a highly selective α2 adrenergic agonist, has gradually been adopted for clinical therapy. Monitored anesthesia with dexmedetomidine delivers intraoperative sedation and analgesia, thus enabling intraoperative nerve injury assessment through intraoperative painful arousal, and rarely cause respiratory depression5. Monitored anesthesia with dexmedetomidine has rarely been used during PKP, and no study comparing monitored anesthesia with local and general anesthesia has been reported. In view of the known disadvantages with local and general anesthesia, we determined if monitored anesthesia is an effective alternative anesthetic approach during PKP. Therefore, a prospective, non-randomized controlled trial was conducted to compare the effects of the three different anesthesia modalities during PKP.
Materials and methods
A prospective, non-randomized controlled study was conducted. All patients underwent PKP for a single-level OVCF from August 2015 to November 2019. The patients were free to choose the anesthetic method based on their preference. All patients were provided written informed consent. The study was approved by the Human Research Ethics Committee at Honghui Hospital (201506001). Clinical trial registration: ChiCTR2100046162, 1st August 2015. Written informed consent was obtained from all patients. The methods were carried out in accordance with the relevant guidelines and regulations. Demographic data were shown in Table 1.
The inclusion criteria were as follows: (1) a single-level OVCF was diagnosed by MRI and bone density (T score < − 2.5); (2) severe back pain associated with an OVCF, and unresponsive to analgesic medication for at least 2 weeks; and (3) the presence of a ≥ 15% height loss of the fractured vertebra6. The exclusion criteria were as follows: (1) compression of the spinal cord and nerve roots; (2) inability to cooperate, such as Alzheimer’s disease and other forms of dementia; and (3) pathologic fractures, such as vertebral metastatic cancer or osteomyelitis.
Anesthesia method
The patients were divided into three groups based on the anesthetic method: local anesthesia group; monitored anesthesia group; and general anesthesia group. The detailed methods were as follows:
Oxygen was delivered at 3 L/min by conventional mask; and electrocardiographic data, pulse oxygen saturation, respiratory rate, heart rate, and blood pressure were monitored.
Local anesthesia group
The skin and subcutaneous tissue at the insertion site was infiltrated with 3–5 mL of 0.4% ropivacaine.
Monitored anesthesia group
In addition to the above local anesthesia procedure, patients received an intravenous injection of 5 mg of dezocine based on weight and age. Subsequently, anesthesia was induced by 0.5 μg/kg of intravenous dexmedetomidine as a loading dose, and maintained thereafter via a continuous intravenous infusion of dexmedetomidine (1 μg/kg/h).
General anesthesia group
Anesthesia was induced with 0.2 μg/kg of intravenous sufentanil, 1 mg/kg of intravenous propofol, and 0.2 mg/kg of intravenous cisatracurium to facilitate endotracheal intubation, then anesthetized by inhalation of 1% sevoflurane. The maintenance of anesthesia was achieved with remifentanil (0.15 μg/kg/min). Ten minutes before the estimated end of surgery, 5 μg of sufentanil was administered intravenously.
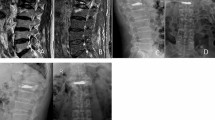
Surgical procedure
All PKP procedures were performed by experienced surgeons, as described in a previous study (KMC; Kinetic Medical Co., LTD, Shanghai, China)7. The patient assumed the prone position. A unilateral transverse process-pedicle approach was adopted to perform all PKPs. The needle puncture through the pedicle and into the anterior one-third of the vertebral body was performed under fluoroscopy. Then, a balloon was inserted into the vertebral body and expanded. Finally, bone cement was injected into the vertebral body under lateral fluoroscopy guidance. Intraoperative nerve injury was evaluated by motor evoked potentials (MEPs) in the general anesthesia group.
Outcome evaluation
The mean arterial pressure (MAP), heart rate, and visual analogue score (VAS) were recorded at the following times: 1 h before anesthesia (time point 1); trocar puncture into the vertebral body (time point 2); injection of bone cement into the vertebral body (time point 3); 2 h postoperatively (time point 4); and 1 day postoperatively (time point 5). The operative time, bone cement leakage, neurologic injuries, adverse anesthetic reactions, and perioperative satisfaction were assessed.
The operative time was measured from the time of needle puncture to wound closure. Postoperative neurologic injuries were assessed based on symptoms and MEPs. Adverse anesthetic reactions were defined as vomiting, drowsiness, hypotension (a MAP < 60 mmHg), bradycardia (heart rate < 60/min), hypoxemia, and pharyngalgia. Perioperative satisfaction was assessed using a 5-point Likert scale at the time of hospital discharge8.
Statistical analysis
A blinded method was adopted to analyze the experimental data. SPSS statistical software (version 19.0; SPSS, Inc., Chicago, IL, USA) was used. A repeated measures ANOVA was used in three group comparisons with repeated measurement data. One-way ANOVA was used in three group comparisons with univariate data. Enumeration data were evaluated using a chi-square test or Fisher’s exact test. A P value < 0.05 was considered statistically significant.
Results
One hundred sixty-five patients who underwent PKP were included in the study; the number of patients in each group was 55. There were no changes in the anesthetic plan for any patient; the data collection was completed in all patients. There were no significant differences in demographic data between the three groups (Table 1).
MAP and heart rate
The MAP and heart rate are shown in Figs. 1 and 2. No statistical differences existed between the three groups with respect to MAP and heart rate 1 h before anesthesia and 1 day postoperatively. Analysis of variance showed that these differences in the MAP and heart rate were statistically significant at the time of trocar puncture into the vertebral body, injection of bone cement into the vertebral body and 2 h postoperatively. The local anesthesia group had the highest MAP and heart rate at the time of trocar puncture into the vertebral body, injection of bone cement into the vertebral body, and 2 h postoperatively. There were no statistically significant differences in the MAP and heart rate between the monitored and general anesthesia groups at the time of trocar puncture into the vertebral body and injection of bone cement into the vertebral body. The monitored anesthesia group had a significantly lower MAP and heart rate than the general anesthesia group 2 h postoperatively (P < 0.01); however, hypotension and bradycardia were not observed in the monitored anesthesia group.
Visual analogue score
The VAS data are listed in Table 2. There were no statistically significant differences between the groups with respect to VAS 1 h before anesthesia and 1 day postoperatively. The intraoperative VAS could not be assessed in the general anesthesia group. The VAS was significantly lower in the monitored anesthesia group than the local anesthesia group at the time of trocar puncture into the vertebral body and injection of bone cement into the vertebral body (P < 0.01). The monitored anesthesia group had the lowest VAS 2 h postoperatively; however, no statistically significant differences in VAS were observed between the other two groups 2 h postoperatively.
Operative time, cement leakage, nerve injuries, adverse effects during anesthesia, and perioperative satisfaction
The operative time, cement leakage, nerve injuries, adverse effects during anesthesia, and perioperative satisfaction data are listed in Tables 3 and 4. The local anesthesia group had the longest operative times and the lowest perioperative satisfaction among the three groups. Nevertheless, the local anesthesia group had the lowest adverse anesthetic reactions. Perioperative satisfaction was highest in the monitored anesthesia group. There were no statistically significant differences in the operative times between the monitored and general anesthesia groups. The differences in intraoperative nerve injuries and the rate of cement leakage were not statistically different among the three groups.
Discussion
OVCFs usually occur in elderly patients with osteoporosis. The mean age of the patients in our study was 76 years. Severe dynamic pain caused by an OVCF affects the quality of life, and can even lead to long-term bed rest among these patients, which then increases the risk of pneumonia, thromboses, and bedsores. Moreover, some patients are admitted to the hospital with Kummell disease, further causing vertebral collapse and increasing the difficulty of treatment9,10. A PKP provides early, effective vertebral stabilization and pain relief among elderly patients11. In the current study, the VAS scores decreased from 6.6 preoperatively to 1.7 one day postoperatively. Apan et al.12 recently reported that segmental epidural anesthesia offered better advantages than general anesthesia in terms of postoperative analgesia, analgesic consumption, and early recovery; however, patients must maintain a lateral and flexed position during administration of epidural anesthesia, which may aggravate a vertebral fracture. In addition, epidural anesthetics may infiltrate into the subarachnoid space and cause total spinal anesthesia or respiratory inhibition. Dexmedetomidine has been effectively used in minimally invasive surgeries13. The results in the current study are consistent with the literature; dexmedetomidine was shown to provide effective sedation and analgesia without affecting communication between the physician and patient. Detailed discussions are presented as follows.
Application of local anesthesia
Injection of lidocaine for local anesthesia has been widely used during PKP14,15. Low-dose ropivacaine induces a conduction block of sensory function without motor dysfunction5. Therefore, we applied 0.4% ropivacaine for local anesthesia during PKP. Compared with the other two groups, local anesthesia in this study had the lowest adverse anesthetic reactions. Local anesthesia also effectively prevented intraoperative neurologic injuries by performing the PKP in the awake state. Because local anesthetics cannot be injected into the vertebral body, the VAS in the local anesthesia group was highest during trocar insertion and bone cement injection, which caused the highest intraoperative MAP and heart rate among the three groups. Unbearable intraoperative pain caused poor patient cooperation, and further led to the longest operative time. Injection of lidocaine into the intravertebral body is contraindicated because local anesthetics may be disseminated to the entire body via the vertebral vessels, thus, causing respiratory inhibition or death12. No differences were observed between the groups with respect to cement leakage. Indeed, it is likely that cement leakage is most often associated with the type of vertebral fracture.
Application of general anesthesia
General anesthesia has been widely used for open surgeries. General anesthesia is not utilized in most PKPs because of the longer preoperative preparation time and higher hospitalization costs3,4. Our study showed that the general anesthesia group had the highest rate of adverse anesthetic effects. Of the patients who received general anesthesia, 29.1% had postoperative vomiting and 38.2% had pharyngalgia secondary to the intubation. The nerve injury rate in the general anesthesia group was not statistically different compared to the other two groups due to MEP monitoring, but MEP increases the economic burden for the patients. Compared to local anesthesia, general anesthesia can maintain a more stable MAP and heart rate. Surgeons could also perform the surgery in less time. Some studies have reported that PKP without MEP monitoring might be performed under general anesthesia by more experienced surgeons3,12.
Application of monitored anesthesia
Dexmedetomidine produces hypnosis by eliminating the inhibitory effect of the locus coeruleus on basal forebrain γ -amino butyric acid, and sedation caused by dexmedetomidine is similar to the sedation caused by natural sleep, from which a patient is easily aroused during monitored anesthesia with dexmedetomidine16. As an opioid receptor agonist, dezocine provides analgesia without respiratory depression. Dezocine is commonly used to enhance the analgesic effect of dexmedetomidine.
Patients had the highest perioperative satisfaction with monitored anesthesia because monitored anesthesia had a significantly lower intensity of pain sensation compared to local anesthesia and fewer adverse anesthetic reactions compared to general anesthetic. Based on better patient cooperation during trocar insertion and bone cement injection, monitored anesthesia had the shortest operative time compared to local anesthesia. Moreover, severe pain can easily awaken a patient when a nerve is touched, which could effectively prevent intraoperative neurologic injury.
Because of the continuous postoperative analgesic and sedative effects, the VAS in the monitored anesthesia group was the lowest 2 h postoperatively; however, the central and peripheral sympatholytic effects of dexmedetomidine may lead to bradycardia and hypotension17,18. In the current study, the MAP and heart rate in the monitored anesthesia group were significantly lower than the local and general anesthesia groups 2 h postoperatively. Tanriverdi et al.19 suggested that low doses of dexmedetomidine (loading dose, 1 μg/kg; continuous dose, 0.7 μg/kg/h) might reduce the rate of hypotension and bradycardia19, which was in agreement with our findings.
Limitations of the study
The limitations of the current study were as follows: (1) non-random allocation may contribute to selection bias; (2) a lack of blinding in patients and surgeons may lead to performance bias; (3) dexmedetomidine may induce the risk of hypotension and bradycardia, thus, more patients are needed to analyze the side effects of dexmedetomidine; and (4) the radiation dose and injection volume of bone cement among the three anesthesia groups should be compared in future studies.
Conclusions
Compared to local anesthesia, monitored anesthesia achieved better intraoperative sedation and analgesia, and had a shorter operative time. Compared to general anesthesia, monitored anesthesia led to fewer adverse anesthetic effects. In addition, monitored anesthesia resulted in better perioperative satisfaction than the other two anesthetic methods. Therefore, monitored anesthesia might be a suitable alternative for PKP.
References
Wu, A. M. et al. The existence of intravertebral cleft impact on outcomes of nonacute osteoporotic vertebral compression fractures patients treated by percutaneous kyphoplasty: A comparative study. J. Spinal Disord. Tech. 27(3), E88-93 (2014).
Nakamae, T. et al. Risk factors for cement loosening after vertebroplasty for osteoporotic vertebral fracture with intravertebral cleft: A retrospective analysis. Asian Spine J. 12(5), 935–942 (2018).
Luginbuhl, M. Percutaneous vertebroplasty, kyphoplasty and lordoplasty: Implications for the anesthesiologist. Curr. Opin. Anaesthesiol. 21(4), 504–513 (2008).
Civelek, E. et al. The retrospective analysis of the effect of balloon kyphoplasty to the adjacent-segment fracture in 171 patients. J. Spinal Disord. Tech. 27(2), 98–104 (2014).
Harned, M. E. et al. Novel use of intraoperative dexmedetomidine infusion for sedation during spinal cord stimulator lead placement via surgical laminectomy. Pain Phys. 13(1), 19–22 (2010).
Heran, M. K., Legiehn, G. M. & Munk, P. L. Current concepts and techniques in percutaneous vertebroplasty. Orthop. Clin. N. Am. 37(3), 409–434 (2006).
Zhang, L. G. et al. Unilateral or bilateral percutaneous vertebroplasty for acute osteoporotic vertebral fracture: A prospective study. J. Spinal Disord. Tech. 28(2), E85-88 (2015).
Sullivan, G. M. & Artino, A. R. Analyzing and interpreting data from likert-type scales. J. Grad. Med. Educ. 5(4), 541–542 (2013).
Muratore, M. et al. Osteoporotic vertebral fractures: Predictive factors for conservative treatment failure. A systematic review. Eur. Spine J. 27(10), 2565–2576 (2018).
Li, H., Liang, C. Z. & Chen, Q. X. Kummell’s disease, an uncommon and complicated spinal disorder: A review. J. Int. Med. Res. 40(2), 406–414 (2012).
Kaemmerlen, P. et al. Percutaneous injection of orthopedic cement in metastatic vertebral lesions. N. Engl. J. Med. 321(2), 121 (1989).
Apan, A. et al. Segmental epidural anesthesia for percutaneous kyphoplasty: Comparison with general anesthesia. Turk. J. Med. Sci. 46(6), 1801–1807 (2016).
Majumdar, M., Wilks, B. & Charlesworth, D. Safe and efficacious use of dexmedetomidine over a prolonged duration for anxiolysis and as an adjunct to analgesia during end-of-life care. J. Palliat. Care. 31(4), 265–267 (2015).
Sheng, S. et al. Improvement in pulmonary function of chronic obstructive pulmonary disease (COPD) patients with osteoporotic vertebral compression fractures (OVCFs) after kyphoplasty under local anesthesia. Int. Surg. 100(3), 503–509 (2015).
Brinjikji, W. et al. Local anesthesia with bupivacaine and lidocaine for vertebral fracture trial (LABEL): A report of outcomes and comparison with the Investigational Vertebroplasty Efficacy and Safety Trial (INVEST). AJNR Am. J. Neuroradiol. 31(9), 1631–1634 (2010).
Hsu, Y. W. et al. Dexmedetomidine pharmacodynamics: Part I: Crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology 101(5), 1066–1076 (2004).
Carollo, D. S., Nossaman, B. D. & Ramadhyani, U. Dexmedetomidine: A review of clinical applications. Curr. Opin. Anaesthesiol. 21, 457–461 (2008).
Terao, Y. et al. Comparison between propofol and dexmedetomidine in postoperative sedation after extensive cervical spine surgery. J. Anesth. 26, 179–186 (2012).
Tanriverdi, T. B., Koceroglu, I., Devrim, S. & Celik, M. G. Comparison of sedation with dexmedetomidine vs propofol during hysteroscopic surgery: Single-centre randomized controlled trial. J. Clin. Pharm. Ther. 44(2), 312–317 (2019).
Acknowledgements
The authors would like to acknowledge the participating patients, surgeons and anesthetists who were involved in this research. This work was supported by Shaanxi Postdoctoral Science Foundation project funds (2017BSHQYXMZZ20).
Author information
Authors and Affiliations
Contributions
L.D., CY.G., X.C.W. and Z.J.G. designed the research program. Z.W.X. and D.J.H. analyzed the data. C.Y.G. and L.D. were responsible for the main body of manuscript. All authors reviewed and commented on drafts of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ge, C., Wu, X., Gao, Z. et al. Comparison of different anesthesia modalities during percutaneous kyphoplasty of osteoporotic vertebral compression fractures. Sci Rep 11, 11102 (2021). https://doi.org/10.1038/s41598-021-90621-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-90621-9
This article is cited by
-
Effect of epidural dexmedetomidine in single-dose combined with ropivacaine for cesarean section
BMC Anesthesiology (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.