Abstract
Intraoperative indocyanine green (ICG) fluorescence angiography has gained popularity and acceptance in many surgical fields for the real-time assessment of tissue perfusion. Although vasopressors have the potential to preclude an accurate assessment of tissue perfusion, there is a lack of literature with regards to its effect on ICG fluorescence angiography. An experimental porcine model was used to expose the small bowel for quantitative tissue perfusion assessment. Three increasing doses of norepinephrine infusion (0.1, 0.5, and 1.0 µg/kg/min) were administered intravenously over a 25-min interval. Time-to-peak fluorescence intensity (TTP) was the primary outcome. Secondary outcomes included absolute fluorescence intensity and local capillary lactate (LCL) levels. Five large pigs (mean weight: 40.3 ± 4.24 kg) were included. There was no significant difference in mean TTP (in seconds) at baseline (4.23) as compared to the second (3.90), third (4.41), fourth (4.60), and fifth ICG assessment (5.99). As a result of ICG accumulation, the mean and the maximum absolute fluorescence intensity were significantly different as compared to the baseline assessment. There was no significant difference in LCL levels (in mmol/L) at baseline (0.74) as compared to the second (0.82), third (0.64), fourth (0.60), and fifth assessment (0.62). Increasing doses of norepinephrine infusion have no significant influence on bowel perfusion using ICG fluorescence angiography.
Similar content being viewed by others
Introduction
Fluorescence angiography, using indocyanine green (ICG) as a contrast agent, is increasingly applied by surgeons during surgical procedures, facilitating intraoperative decision-making. This imaging technique is fast (i.e., a matter of seconds to minutes), safe, and easy to perform, and multiple assessments can be performed during a single procedure1. Consequently, ICG fluorescence angiography is gaining popularity and is meeting acceptance in many surgical fields2,3,4,5, including colorectal surgery6,7.
Anastomotic leakage (AL) is one of the dreaded complications in colorectal surgery, with an incidence of up to 20% of cases6,8. It has been associated with an increased postoperative morbidity and mortality, and even when managed, it leads to a prolonged hospital stay and to increased healthcare costs7,8. As adequate perfusion is essential for optimal healing and AL prevention, an insufficient blood supply at the proximal or distal end of the anastomosis is one of several factors which have been associated with a greater risk of AL in case of an intraoperatively “water-tight” anastomosis. Accordingly, the assessment of bowel perfusion and intraoperative modification of the level of resection or anastomosis in case of insufficient perfusion may contribute to a reduced risk of AL7.
Traditionally, bowel perfusion is evaluated by the surgeon through a direct visualization of the anastomosis, including the evaluation of the serosal and mucosal color, bowel peristalsis, and pulsation of mesenteric arteries or bleeding at the cut edge of the bowel7,8. However, these subjective signs did not allow to evaluate microperfusion and were found to be unreliable since the accuracy of AL prediction by surgeons was low7,8,9. For this reason, ICG fluorescence angiography was proposed as an objective imaging technique which allows for the real-time assessment of bowel perfusion. After intravenous administration, ICG is bound to plasma protein. When exposed to near-infrared excitation, it re-emits a fluorescent light. Bowel perfusion may be quantified by using fluorescence intensity, which is proportional to bowel vascularization10. Recent systematic reviews demonstrated that ICG fluorescence angiography seems to reduce AL rates as compared to conventional techniques in colorectal surgery7,11. Liu et al. reported an AL rate of 3.8% in the ICG group as compared to 7.8% in the non-ICG group in a meta-analysis including a total of 4,037 patients12.
Nevertheless, the evaluation of fluorescence intensity remains a static measure with no consideration of ICG diffusion over time. Consequently, a dynamic fluorescence videography technique, which integrates near-infrared endoscopy and specific software called fluorescence-based enhanced reality (FLER), has been developed13. Dynamic fluorescence angiography allows for time-to-peak fluorescence intensity (TTP). It is found to be a promising tool for the real-time imaging of bowel perfusion in an easy and accurate way10,14. Additionally, FLER analyses were found to be correlated with local capillary lactate (LCL) levels, in the experimental10 and clinical setting15.
While vasopressors (e.g., norepinephrine) are often used during surgery to restore and maintain blood pressure levels in case of hypotension16, these substances have the potential to drastically reduce blood flow via vasoconstriction. Consequently, they may potentially preclude an accurate assessment of tissue perfusion when using ICG fluorescence angiography17,18.
To date, there is a limited number of studies which evaluated the effect of vasopressors on tissue perfusion assessment using ICG fluorescence angiography. The aim of this study was to investigate the effect of increasing doses of norepinephrine on bowel perfusion assessment using ICG fluorescence angiography in a porcine intestinal model.
Methods
This study, which is part of the Endoscopic Luminescent Imaging for Oncology Surgery (ELIOS) project, was performed according to the National Institutes of Health guidelines for the use of experimental animals, respecting the ARRIVE guidelines19.
Norepinephrine infusion
Before finalizing the study protocol, consideration was given to use either increasing boluses of norepinephrine or an increasing continuous norepinephrine infusion. Norepinephrine is a sympathomimetic amine with a primarily agonistic effect at alpha-1 and beta-1 receptors, which increases systemic vascular resistance and potentially increases cardiac output respectively20. Due to a short half-life of 2.5 min, an intravenous bolus injection of norepinephrine would only induce short-term hypertension and tachycardia. In this period of time, ICG fluorescence angiography could be performed. For this evaluation, and for ethical purposes, respecting the ‘3R’ (replace, refine, reduce) principles of animal research21, two pilot pigs used for educational purposes without causing any intestinal damage, were utilized to assess the effect of increasing doses of bolus injections versus increasing doses of continuous infusion of norepinephrine. In the ‘bolus injection pig’, a very short time period of vasopressor effect was observed as blood pressure and heart rate dropped within approximately two minutes during ICG fluorescence angiography assessment. In the ‘continuous infusion pig’, no decrease was observed as blood pressure and heart rate were maintained during infusion. For this logistical reason, it was decided to use increasing doses of continuous norepinephrine infusion in this study. Additionally, it was decided to use the following doses of norepinephrine of 0.1, 0.5, and 1.0 µg/kg/min, since these doses resulted in a relevant increase in blood pressure and are within the range of doses frequently used in the clinical setting.
Animal preparation
A total of five adult female large white pigs (Sus scrofa domesticus) were included. According to the design of the study, every animal served as its own internal control. All animals were fasted for 24 h with free access to water. A qualified anesthesiologist (EN and SD) performed every anesthesia-related steps of the procedure.
The animals were sedated with an intramuscular injection of zolazepam and tiletamine 10 mg/kg (Zoletil ND, Virbac, France). After general anesthesia induction using an intravenous administration of propofol 3 mg/kg (Propofol Lipuro ND, B Braun, France) and rocuronium 0.8 mg/kg (Esmeron ND, MSD, France), the animals were intubated and mechanically ventilated in a supine position. Anesthesia was maintained by means of a continuous inhalation of isoflurane 2% (Isoflurin ND, Axience, France) and a mixture of 50% nitrous oxide in oxygen. The dose of anesthetics was increased when necessary according to the reflex status of the animals (i.e., palpebral reflexes and jaw tone). Intravascular injections of buprenorphine (Buprecare ND, Axience, France) 0.01 mg/kg were used for analgesia. All animals were infused with Ringer’s lactate intravenously at a rate of 4 mL/kg/h.
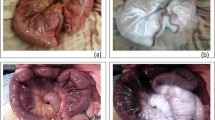
A midline laparotomy was performed to expose the small bowel (Fig. 1 for the study set-up). A 30 cm segment of the small intestine (250 cm from the pylorus) was loosely fixed to both sides of the abdominal wall with Vicryl sutures to guarantee bowel exposure during this study. No further bowel manipulation was performed. During the protocol, three increasing doses of continuous norepinephrine infusion (0.1, 0.5, and 1.0 µg/kg/min) were administered intravenously over a 25-min interval (Fig. 2 for the study flowchart). Heart rate and blood pressure were continuously monitored through an arterial line inserted into the femoral artery. At the end of the protocol, pigs were sacrificed under deep anesthesia (isoflurane 5%) with intravenous administrations of pentobarbital 40 mg/kg (Exagon ND, Axience, France).
ICG fluorescence angiography
In this study, an ICG fluorescence videography system integrated within a near-infrared endoscope (KARL STORZ GmbH & CO. KG, Germany) was used. It could detect the ICG-emitted fluorescence signal. After exposing the small bowel, the camera was fixed to an articulated arm in order to stabilize the image and allow for repetitive assessments (e.g., ensuring a stable distance and angle during ICG fluorescence angiography assessments). In a recent analysis of the European registry on fluorescence image-guided surgery (EURO-FIGS), an ICG dose of 0.1 to 0.2 mg/kg was identified as the most frequently used clinical dose for near-infrared fluorescence angiography22. To standardize the method of ICG administration, a bolus of ICG (Infracyanine, Laboratoires Serb, Paris, France) at a dose of 0.1 mg/kg was administered intravenously through a central venous catheter in the right internal jugular vein (Vygon, arterial LeaderCath, 6 French, 15 cm).
The ICG-emitted fluorescence signal was analysed using the ER-PERFUSION software (IRCAD, Strasbourg, France), which allowed for a virtual perfusion cartography based on time-to-peak fluorescence intensity (TTP; in seconds). TTP results from the velocity of the fluorescence signal until it reaches its maximum intensity peak in a specific region of interest (ROI) within the first 40 s following ICG injection23. This is a relatively short period following ICG injection, as a result of ICG administration via the central venous catheter. The virtual perfusion cartography is subsequently overlapped onto the images, providing fluorescence-based enhanced reality (FLER). In this study, TTP was measured from the time when there was 25% of fluorescence intensity to 75% of fluorescence intensity using the ER-PERFUSION software. In addition, the minimum and maximum absolute fluorescence intensities were measured in four randomly chosen ROIs on the bowel surface using the FLER software. TTP and absolute fluorescence intensity were analysed as mean of the four ROIs, together with the mean difference in maximum and minimum absolute fluorescence intensities.
Capillary lactate levels
Local bowel capillary lactate (LCL) levels were measured in the blood using an EDGE lactate analyser (ApexBio, Taipei, Taiwan, People’s Republic of China) by puncturing the bowel serosa in the chosen ROI with a needle. LCL levels were obtained during all five fluorescence videography assessments.
Statistical analysis
Continuous variables are presented as means with standard deviation (SD). Categorical data were reported as frequency and proportion. Fisher’s exact test was used to calculate P values for categorical variables. The paired sample T-test was used to analyse the differences in TTP fluorescence intensity (in seconds) and mean absolute fluorescence intensity in ROIs between the different vasopressor doses. All results were analysed using IBM SPSS Statistics for Windows, version 24 (IBM Corporation, Armonk, NY, USA). A p value < 0.05 was considered statistically significant.
Ethics approval
The protocol was approved by the local Ethical Committee on Animal Experimentation (ICOMETH No. 38.2020.02.003) and by the French Ministry of Superior Education and Research (MESR) under the following reference: APAFIS#8721-2017013010316298-v2. All animals used in the experimental laboratory were managed according to French laws for animal use and care and according to the directives of the European Community Council (ECC).
Results
The included animals had a mean weight of 40.3 ± 4.24 kg (range: 33.0 to 44.0 kg). During the protocol, all pigs underwent five ICG fluorescence angiographies, namely once at baseline, three times following increasing doses (0.1, 0.5, and 1.0 µg/kg/min) of norepinephrine infusion, and once following discontinuation of norepinephrine infusion. In general, blood pressure and heart rate increased gradually as the infusion dose increased. After discontinuation of norepinephrine infusion, a substantial decrease in blood pressure and heart rate was observed (Tables 1 and 2).
Time-to-peak fluorescence intensity (TTP)
Mean TTP of the four regions of interest after the first (4.23 ± 0.30 s) and second dose of norepinephrine (3.90 ± 0.16 s) were slightly lower as compared to baseline (4.41 ± 0.46 s) assessment (− 0.18 and − 0.51 s respectively). Conversely, mean TTP after the third dose (4.60 ± 0.68 s) and after discontinuation of norepinephrine infusion (5.99 ± 2.07) were higher as compared to baseline assessment (+ 0.19 and + 1.58 respectively) (Fig. 3). However, mean TTP did not significantly differ from baseline assessment (Table 3). In addition, mean TTP per ROI in the first, second, third dose assessment, and mean TTP in the assessment following discontinuation of norepinephrine infusion, did not significantly differ from baseline.
Mean time-to-peak (TTP) in seconds for all 5 pigs. Mean TTP (in black) with standard deviations (in grey). X-axis: ICGA assessment number, mean BP and HR for all pigs. Y-axis: mean TTP in seconds. ICGA indocyanine green angiography (I = baseline, II = after norepinephrine (NE) dose 1, III = after NE dose 2, IV = after NE dose 3, V = remnant measurement following discontinuation of NE), BP = blood pressure, HR = heart rate.
Absolute fluorescence intensity
Mean minimum fluorescence intensity of the four ROIs increased during the protocol from 0 at baseline to 62.7, 98.3 (+ 57% increase as compared to previous ICG fluorescence angiography), 127.1 (+ 29%), and 134.2 (+ 6%) after the first, second, and third dose, and after discontinuation of norepinephrine infusion respectively. Mean maximum fluorescence intensity of the four ROIs also increased from 101.4 at baseline to 146.6 (+ 45%), 150.4 (+ 3%), 162.1 (+ 8%), and 159.0 (− 2%) after the first, second, and third dose, and after discontinuation of norepinephrine infusion respectively. Since the maximum intensity increased in a slower manner as compared to the minimum intensity, the mean difference decreased from 101.4 to 24.8 (Fig. 4). Mean minimum fluorescence intensity in the first (p = 0.002), second (p = 0.002), third (p = 0.003), and remnant assessment (p ≤ 0.001) were significantly different as compared to the baseline assessment, as well as the maximum fluorescence intensity (p = 0.011, 0.016, 0.027, and 0.002 respectively).
Mean minimum, maximum, and difference in absolute fluorescence intensity (FI) for all 5 pigs. Mean fluorescence intensity (in black) with standard deviations (in grey). X-axis: ICGA assessment number, mean BP and HR for all pigs. Y-axis: mean fluorescence intensity. ICGA indocyanine green angiography (I = baseline, II = after norepinephrine (NE) dose 1, III = after NE dose 2, IV = after NE dose 3, V = remnant measurement following discontinuation of NE), BP blood pressure, HR heart rate.
Regarding the mean difference in fluorescence intensity, only the mean difference between fluorescence intensity in the first dose assessment did not significantly differ from baseline (p = 0.208, in contrast to the second (p = 0.006), third (p = 0.011), and remnant assessment (p = 0.003).
Local capillary lactate (LCL) levels
Local capillary lactate (LCL) levels at the time of the ICG fluorescence angiography assessment are presented in Table 3. LCL levels defined as ‘low’ represent a value between 0.1 and 0.59 mmol/L. In statistical analyses comparing baseline and the following ICG fluorescence angiographies, all ‘low’ LCL level results were regarded as 0.59 in order to prevent any underestimation bias. The subsequent LCL levels were 0.74, 0.82, 0.64, 0.60, and 0.62 from baseline to remnant assessment respectively. No significant difference in LCL levels was found.
Discussion
Although there were a few previous studies which evaluated the effect of vasopressors on free flap perfusion using ICGA, this is the first study evaluating the influence of increasing doses of intraoperative vasopressor use on ICG fluorescence angiography in a standardized porcine model24,25. Based on this model, no difference was found in mean time-to-peak fluorescence intensity (TTP) between baseline and increasing doses of norepinephrine infusion. Additionally, a significant increase in mean minimum and maximum absolute fluorescence intensities was observed, as well as a significant decrease in mean difference between these two measurements.
In gastrointestinal surgery, an adequate intraoperative assessment of bowel perfusion is mandatory in order to prevent anastomotic leakage. Over the last decade, ICG fluorescence angiography has gained popularity for the real-time assessment of bowel perfusion12. Likewise, ICG fluorescence angiography is more frequently applied to plastic and reconstructive surgery to objectively evaluate flap perfusion2. In that surgical field, it has been suggested that pharmacologically induced vasoconstriction could preclude an accurate estimation of tissue perfusion, while an adequate regulation of systemic blood pressure is fundamental during every surgical procedure18. Despite a suspicion supported by anecdotal reports in the literature, no previous study reported the effect of vasopressors, such as norepinephrine, on tissue perfusion assessment using ICG fluorescence angiography.
TTP as part of fluorescence-based enhanced reality (FLER) was considered the primary outcome in the current study. The measurement corresponds to the mean time elapsed for the fluorescence signal to reach its maximum intensity in a given area26. TTP offers two great advantages as compared to absolute fluorescence intensity values. First, TTP is independent of the distance between the ICG camera and the ROI, whereas absolute fluorescence intensity is highly dependent on distance1,14. In the current study, the distance between the camera and the bowel was kept constant throughout perfusion assessments. Nonetheless, it remains relevant in clinical perfusion assessments.
Theoretically, the ICG plasma half-life of approximately 3 to 5 min allows for multiple perfusion assessments throughout a surgical procedure1. However, in a previous preliminary test by Diana et al. concerning a series of ICG injections (0.125 mg/kg every 15 min) while focusing on a healthy small bowel loop, ICG accumulation was observed. On the other hand, the calculated TTP remained constant in each assessment14. As a result, a second and major advantage of TTP is that it truly allows for multiple and repetitive assessments. Only the additional signal is interpreted and the “noise” produced by the accumulation of fluorescent dye does not affect TTP. Consequently, we derive that increasing doses of norepinephrine, as explored in this experimental porcine model, have no effect on bowel perfusion assessment using ICG fluorescence. Notably, the TTP increased from 4.60 s after dose 3 to 5.99 s after norepinephrine discontinuation (“remnant assessment”). Although this is a substantial increase, the mean difference in TTP was not significant as compared to the baseline assessment. The impaired clinical condition of the pigs, with a mean blood pressure of 39/25 mmHg at the end of the study, resulting from the termination of continuous norepinephrine infusion, contributed to this increase in TTP.
When considering absolute fluorescence intensity in the current study, an increase in mean minimum and maximum fluorescence intensity is consistent with the aforementioned study14. Although a 25-min interval (except between ICG fluorescence angiography assessment IV and V) was maintained to ensure ICG wash-out following the ICG injections of 0.1 mg/kg, a significant ICG accumulation was observed. Consequently, there is more reason to believe that it is better to use a dynamic fluorescence videography technique, such as FLER analysis, over absolute fluorescence intensity in case of repeat perfusion assessments throughout a surgical procedure. Notably, a decrease in the mean difference in fluorescence intensity was noted. It is likely due to approaching an absolute maximum fluorescence intensity level as a result of dye accumulation within the tissue.
Local capillary lactate (LCL) levels reflect tissue oxygenation in bowel cells, and these were previously correlated with bowel perfusion using ICG fluorescence angiography. In a previous study, it was concluded that the mean LCL level in an ischemic bowel region (5.6 ± 2.8 mmol/L) was significantly higher than LCL levels in a bowel region at 25% of perfusion on ICG fluorescence angiography (3.7 ± 1.7 mmol/L) and in a bowel region at 75% of perfusion (2.9 ± 1.3 mmol/L)10. In the current study, low LCL levels were observed with no significant increase. This reflects the healthy state and non-ischemic condition of the bowel under investigation.
With regards to the infusion dose of norepinephrine, the effect on beta-1 adrenergic receptors may be more distinct at low doses (less than 2 µg/min), potentially leading to an increased cardiac output. In doses higher than 3 µg/min, the alpha-1 adrenergic effect may predominate, resulting in vasocontraction20. Since the minimum dose was 3.3 µg/min in the current study, this should result in vasoconstriction and in a dose-dependent increase in systemic vascular resistance. Due to this particular effect of norepinephrine, plastic and reconstructive surgeons have hypothesized that vasoconstriction comprises blood flow of superficial capillaries, reducing the potential of ICG fluorescence angiography in order to accurately assess flap perfusion in reconstructive surgery17,18. The results of the current study suggest that there was no alteration in bowel perfusion based on ICG fluorescence angiography. This might be a result of an increase in blood pressure, which leads to a compensation for the vasoconstrictive effect of norepinephrine. This finding is supported by previous studies in which norepinephrine was found to preserve intestinal microcirculatory blood flow27,28 and microcirculatory flap perfusion29,30. Conversely, another study found that norepinephrine decreased intestinal microcirculatory blood flow, despite significantly increased arterial blood pressure31. However, the design of the current study is different as compared to previous studies in which laser Doppler flowmetry (LDF) was used to evaluate microcirculatory blood flow27,28,29,30,31.
Although plastic and reconstructive surgery concerns a different surgical field, the principles of perfusion assessment remain similar. Two recent clinical studies in this particular field have evaluated the effect of vasopressor use on flap perfusion using ICGA assessment24,25. Anker et al. concluded that norepinephrine concentrations of 0.065 ± 0.020 μg/kg/min had no clinically significant impact on microperfusion24. Massaro et al. concluded that changes in mean perfusion of the free flap during the intraoperative period are nominal25. However, in contrast to the current study, both studies were not performed in a standardized fashion with regard to the vasopressor dose. While the results of the current standardized animal study are consistent with previous findings and suggest that increasing doses of norepinephrine may also have no effect on perfusion assessment using ICG fluorescence angiography in other types of tissue (e.g., adipocutaneous or musculocutaneous flap perfusion in reconstructive procedures), this should be confirmed in future studies.
Despite the novelty of this first experimental study reporting on the effect of increasing doses of norepinephrine on tissue perfusion assessment using ICG fluorescence angiography, some limitations need to be addressed. Five pigs constitute a small study population and only female pigs were used19. However, multiple ICGA measurements were obtained without unreasonable outliers. Although one of the animals had a considerably lower total body weight of 33.0 kg compared with the mean weight of 40.3 kg, we believe that the difference in total body weight does not influence outcomes, as all animals act as their own control.
In addition, only healthy small intestines were investigated in this study. Although no difference was found in mean TTP between baseline and increasing doses of norepinephrine infusion in the current study, we are unsure about the results in diseased bowel areas. It is our intention to study this clinically relevant problem in a future experimental animal model with an ischemic bowel model by clamping the arterial supply of bowel segments in combination with the use of vasopressors. Furthermore, the study is limited by the absence of a control group in which ICG fluorescence angiography is performed without any administration of norepinephrine. Conversely, this study is strengthened by the use of two ‘pilot pigs’ in advance, in order to assess the effect of bolus injections versus a continuous infusion of norepinephrine. Continuous infusion was chosen over bolus injections, since an increase in blood pressure and heart rate was maintained with a continuous infusion and its administration relates more to the daily clinical practice. In addition, two previous studies concerning the effect of vasopressors on intestinal blood flow and oxygen supply also used continuous norepinephrine infusion in doses ranging from 0.01 to 2.0 µg/kg/min28,31.
In conclusion, increasing doses of norepinephrine (0.1, 0.2, and 0.5 µg/kg/min respectively) have no statistically significant influence on bowel perfusion assessment as time-to-peak fluorescence intensity remains constant during the FLER analysis. Secondly, ICG accumulation was observed when using absolute fluorescence intensity, which is an important finding for future studies, reflecting the need for a dynamic fluorescence videography technique over absolute fluorescence intensity in case of repeat perfusion assessments.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Pruimboom, T. et al. Optimizing indocyanine green fluorescence angiography in reconstructive flap surgery: A systematic review and ex vivo experiments. Surg. Innov. 27, 103–119. https://doi.org/10.1177/1553350619862097 (2020).
Pruimboom, T., Schols, R. M., Van Kuijk, S. M., Van der Hulst, R. R. & Qiu, S. S. Indocyanine green angiography for preventing postoperative mastectomy skin flap necrosis in immediate breast reconstruction. Cochrane Database Syst. Rev. 4, Cd013280, https://doi.org/10.1002/14651858.CD013280.pub2 (2020).
Degett, T. H., Andersen, H. S. & Gögenur, I. Indocyanine green fluorescence angiography for intraoperative assessment of gastrointestinal anastomotic perfusion: A systematic review of clinical trials. Langenbecks Arch. Surg. 401, 767–775. https://doi.org/10.1007/s00423-016-1400-9 (2016).
Foster, C. H., Morone, P. J., Tomlinson, S. B. & Cohen-Gadol, A. A. Application of indocyanine green during arteriovenous malformation surgery: Evidence, techniques, and practical pearls. Front. Surg. 6, 70. https://doi.org/10.3389/fsurg.2019.00070 (2019).
Oldhafer, K. J. et al. Intraoperative fluorescence angiography and cholangiography with indocyanine green in hepatobiliary surgery. Chirurg 90, 880–886. https://doi.org/10.1007/s00104-019-01035-3 (2019).
Hayami, S. et al. Visualization and quantification of anastomotic perfusion in colorectal surgery using near-infrared fluorescence. Tech. Coloproctol. 23, 973–980. https://doi.org/10.1007/s10151-019-02089-5 (2019).
Blanco-Colino, R. & Espin-Basany, E. Intraoperative use of ICG fluorescence imaging to reduce the risk of anastomotic leakage in colorectal surgery: A systematic review and meta-analysis. Tech. Coloproctol. 22, 15–23. https://doi.org/10.1007/s10151-017-1731-8 (2018).
Kryzauskas, M. et al. The problem of colorectal anastomosis safety. Medicine (Baltimore) 99, e18560, https://doi.org/10.1097/md.0000000000018560 (2020).
Karliczek, A. et al. Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int. J. Colorectal Dis. 24, 569–576. https://doi.org/10.1007/s00384-009-0658-6 (2009).
Diana, M. et al. Intraoperative fluorescence-based enhanced reality laparoscopic real-time imaging to assess bowel perfusion at the anastomotic site in an experimental model. Br. J. Surg. 102, e169-176. https://doi.org/10.1002/bjs.9725 (2015).
van den Bos, J. et al. Near-infrared fluorescence imaging for real-time intraoperative guidance in anastomotic colorectal surgery: A systematic review of literature. J. Laparoendosc. Adv. Surg. Tech. A 28, 157–167. https://doi.org/10.1089/lap.2017.0231 (2018).
Liu, D., Liang, L., Liu, L. & Zhu, Z. Does intraoperative indocyanine green fluorescence angiography decrease the incidence of anastomotic leakage in colorectal surgery? A systematic review and meta-analysis. Int. J. Colorectal Dis. https://doi.org/10.1007/s00384-020-03741-5 (2020).
Diana, M. et al. Enhanced-reality video fluorescence: A real-time assessment of intestinal viability. Ann. Surg. 259, 700–707. https://doi.org/10.1097/SLA.0b013e31828d4ab3 (2014).
Diana, M. et al. Real-time navigation by fluorescence-based enhanced reality for precise estimation of future anastomotic site in digestive surgery. Surg. Endosc. 28, 3108–3118. https://doi.org/10.1007/s00464-014-3592-9 (2014).
D’Urso, A. et al. Computer-assisted quantification and visualization of bowel perfusion using fluorescence-based enhanced reality in left-sided colonic resections. Surg. Endosc. https://doi.org/10.1007/s00464-020-07922-9 (2020).
Lonjaret, L., Lairez, O., Minville, V. & Geeraerts, T. Optimal perioperative management of arterial blood pressure. Integr. Blood Press. Control 7, 49–59. https://doi.org/10.2147/ibpc.S45292 (2014).
Gurtner, G. C. et al. Intraoperative laser angiography using the SPY system: Review of the literature and recommendations for use. Ann. Surg. Innov. Res. 7, 1. https://doi.org/10.1186/1750-1164-7-1 (2013).
Munabi, N. C., Olorunnipa, O. B., Goltsman, D., Rohde, C. H. & Ascherman, J. A. The ability of intra-operative perfusion mapping with laser-assisted indocyanine green angiography to predict mastectomy flap necrosis in breast reconstruction: A prospective trial. J. Plast. Reconstr. Aesthet. Surg. 67, 449–455. https://doi.org/10.1016/j.bjps.2013.12.040 (2014).
Percie du Sert, N. et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. Br. J. Pharmacol. 177, 3617–3624, https://doi.org/10.1111/bph.15193 (2020).
Smith, M. D. & Maani, C. V. In StatPearls (StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC, 2020).
Kirk, R. G. W. Recovering the principles of humane experimental technique: The 3Rs and the human essence of animal research. Sci. Technol. Hum. Values 43, 622–648. https://doi.org/10.1177/0162243917726579 (2018).
Spota, A. et al. Fluorescence-based bowel anastomosis perfusion evaluation: Results from the IHU-IRCAD-EAES EURO-FIGS registry. Surg. Endosc. https://doi.org/10.1007/s00464-020-08234-8 (2021).
Barberio, M. et al. A novel technique to improve anastomotic perfusion prior to esophageal surgery: Hybrid ischemic preconditioning of the stomach. Preclinical efficacy proof in a porcine survival model. Cancers (Basel) 12, https://doi.org/10.3390/cancers12102977 (2020).
Anker, A. M. et al. Assessment of DIEP flap perfusion with intraoperative indocyanine green fluorescence imaging in vasopressor-dominated hemodynamic support versus liberal fluid administration: A randomized controlled trial with breast cancer patients. Ann. Surg. Oncol. 27, 399–406. https://doi.org/10.1245/s10434-019-07758-1 (2020).
Massaro, A. et al. Serial perioperative assessment of free flap perfusion with laser angiography. Craniomaxillofac. Trauma Reconstr. 14, 16–22. https://doi.org/10.1177/1943387520930608 (2021).
Diana, M. et al. Probe-based confocal laser endomicroscopy and fluorescence-based enhanced reality for real-time assessment of intestinal microcirculation in a porcine model of sigmoid ischemia. Surg. Endosc. 28, 3224–3233. https://doi.org/10.1007/s00464-014-3595-6 (2014).
Hiltebrand, L. B., Koepfli, E., Kimberger, O., Sigurdsson, G. H. & Brandt, S. Hypotension during fluid-restricted abdominal surgery: Effects of norepinephrine treatment on regional and microcirculatory blood flow in the intestinal tract. Anesthesiology 114, 557–564. https://doi.org/10.1097/ALN.0b013e31820bfc81 (2011).
Schwarz, B. et al. Effects of norepinephrine and phenylephrine on intestinal oxygen supply and mucosal tissue oxygen tension. Intensive Care Med. 27, 593–601. https://doi.org/10.1007/s001340100856 (2001).
Eley, K. A., Young, J. D. & Watt-Smith, S. R. Epinephrine, norepinephrine, dobutamine, and dopexamine effects on free flap skin blood flow. Plast. Reconstr. Surg. 130, 564–570. https://doi.org/10.1097/PRS.0b013e31825dbf73 (2012).
Chung, J. H. et al. Effects of vasopressors on circulation in the porcine abdominal island flap model. J. Plast. Reconstr. Aesthet. Surg. 72, 1653–1660. https://doi.org/10.1016/j.bjps.2019.06.009 (2019).
Krejci, V., Hiltebrand, L. B. & Sigurdsson, G. H. Effects of epinephrine, norepinephrine, and phenylephrine on microcirculatory blood flow in the gastrointestinal tract in sepsis. Crit. Care Med. 34, 1456–1463. https://doi.org/10.1097/01.Ccm.0000215834.48023.57 (2006).
Acknowledgements
The authors would like to thank Guy Temporal for his valuable assistance in proofreading this manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
M.A., T.P., R.S., N.B., L.S., R.H., J.M., and M.D. developed the study protocol. E.N. and S.D. performed the anesthesia-related steps of the procedure. M.A. and N.O. performed the surgical procedure, and the indocyanine green fluorescence (ICG) angiography assessments. M.K., T.C., and A.H. analysed the ICG fluorescence angiography assessment (fluorescence-enhanced reality). T.P. performed statistical analyses. M.A., T.P., and R.S. wrote the main manuscript and prepared all Figures and Tables. All authors critically reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
Michele Diana and Laurents Stassen are members of the Advisory Board of Diagnostic Green. Michele Diana is the recipient of the ELIOS grant. The other authors have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al-Taher, M., Pruimboom, T., Schols, R.M. et al. Influence of intraoperative vasopressor use on indocyanine green fluorescence angiography: first evaluation in an experimental model. Sci Rep 11, 9650 (2021). https://doi.org/10.1038/s41598-021-89223-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89223-2
This article is cited by
-
Clinical application of machine learning and computer vision to indocyanine green quantification for dynamic intraoperative tissue characterisation: how to do it
Surgical Endoscopy (2023)
-
Quantification of indocyanine green near-infrared fluorescence bowel perfusion assessment in colorectal surgery
Surgical Endoscopy (2023)
-
Experimental evaluation of laparoscopic laser speckle contrast imaging to visualize perfusion deficits during intestinal surgery
Surgical Endoscopy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.