Abstract
The anorectal malformation with long perineal fistula is a rare anomaly in the spectrum of anorectal malformations. Aim of the study is to describe the series of patients with anorectal malformation with long perineal fistula and compare the outcome with patient with standard perineal fistula. From March 2012 to January 2019, 7 patients who suffered from anorectal malformation with long perineal fistula were retrospectively reviewed. Three were operated on primarily by our department, and 4 cases were re-operated after a perineal anoplasty repair performed elsewhere. Four were operated by laparoscopy assisted anorectoplasty, and 3 cases were repaired by posterior sagittal anorectoplasty. The follow-up outcomes were compared with 71 cases of normal perineal fistula (NPF) in the same period. 7 cases have been followed up for 0.5–4 years (M = 2.57 ± 1.26) after definitive surgery. Their bowel function score was lower than normal perineal fistula (SPF = 12, range: 5–18; NPF = 18.5, range: 18–20). Four cases underwent anorectomanometry. The incidence of rectoanal inhibitory reflex was lower in the special type group. (p = 0.14). Three cases of contrast enema using barium: 2 cases of colorectal dilatation and thickening changes, 1 case showed no obvious abnormalities. Anorectal perineal fistula should be examined by distal colostogram at preoperation. This should be altered in: When suspecting a case of anorectal malformation type long perineal fistula a preoperative contrast enema could give insight of the anatomy befor performing a anoplasty.
Similar content being viewed by others
Background
Perineal fistula is one of the most common types of anorectal malformation in pediatric surgery. Most pediatric surgeons agree that this well recognized malformation can be repaired by perineal anoplasty1,2,3.
However, we experienced a rare case of a perineal fistula associated with dilatation of the bowel found at a high position. This special type of malformation (SPF) is characterized by a perineal fistula as the principal clinical manifestation but the fistula tube is slender and the proximal bowel is found at a high position. Therefore, if a full preoperative assessment is not performed, the diagnosis may be delayed leading to abnormal bowel function.
As Peña’s paper in 2017 emphasized, a distal colostogram is the single most important diagnostic study indicated in children with an imperforate anus prior to definitive repair4. The aim of this article is to explore the diagnosis and treatment of this special type of perineal fistula, and to improve its treatment outcomes.
Methods
From March 2012 to January 2019, seven patients who had a anorectal malformation with a special type of perineal fistula were either admitted or transferred to Department of Pediatric Surgery, Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine. There are six boys and one girl.
Among these patients, four were diagnosed with low rectal perineal fistula and had perineal anoplasty without undergoing a distal colostogram at a local hospital after birth. However, during the surgery, it was difficult to find the high positioned rectum, and therefore, the operation was terminated. After the perineum was sutured, a colostomy was performed. Thus, these patients only underwent colostomy before they were transferred to our institute after a period of three months. We performed a preoperative distal colostogram, which revealed that the fistula tube was slender, and the dilated proximal colon was located in front of the iliac crest (Fig. 1).
One patient was diagnosed with a rectal perineal fistula at the local hospital, and was treated with daily calibration. When she was 10 months old, she developed anal bleeding after anal sphincter treatment, and was subsequently transferred to our hospital. On the basis of a preoperative distal colostogram and magnetic resonance imaging (MRI), the patient was diagnosed with SPF, and initially underwent transverse colostomy.
The two other patients who came to our hospital after birth were diagnosed with SPF by a preoperative distal colostogram similar to the above case. Subsequently, colostomy was performed in our hospital.
Clinical evaluation was carried out by using the seven-item bowel function score (BFS) by Rintala5. Refer to the previous scale study, the maximum total score is 20, the reference value of normal children is 19 with 18 being the 10th percentile6,7. Therefore, in this study, a value of 18 (over 90% of the control group) was used as the lower limit of normality. In addition, the manometric evaluation was performed simultaneously with the high-resolution anorectal manometry. The parameters measured in this study were the sphincter resting pressure, squeeze pressure, and the presence of rectal inhibitory reflex (RAIR). The reference values for the normal sphincter resting pressure were 30 to 60 mmHg, and for the extrusion pressure were 50 to 120 mmHg8. The follow-up outcomes were compared with 71 cases of normal perineal fistula (NPF) in the same period.
A standard statistical software package (Windows version 23.0; SPSS Inc., Armonk [NY], US) was used to analyze the data. Continuous variables are expressed as medians (ranges) and compared using Mann–Whitney U test. Use the chi-square test to compare categorical variables. P value less than or equal to 0.05 is considered statistically significant.
Ethics approval and consent to participate
The study was approved by the ethical committee of the Institutional Review Board of Shanghai Jiao Tong University. Informed written consent was obtained from the parents of each participant. Study procedure was carried out in accordance with the approved guidelines.
Consent for publication
Written informed consent for publication was obtained from all participants. All parents of the study participants gave written consent for their clinical details along with identifying images to be published in this study.
Results
The time of these children’s diagnosis ranged from 2 days to 10 months after birth (mean [M] = 8.57 ± 107.70). The age at operation ranged from 2.7 to 12.6 months (median [M] = 5.10 ± 2.88). The weight of the patients ranged from 6.2 to 11 kg (M = 7.46 ± 1.59). More than 50% of the SPF patients had a demonstrable cardiac defect (patent foramen ovale, PFO). Additionally, three patients had spine syndrome and two had some degree of urological anomaly (Table 1). All seven children underwent anal anorectoplasty at our hospital. Four patients underwent laparoscopy assisted anorectoplasty (LAARP), and three cases were repaired using modified posterior sagittal anorectoplasty (PSARP). In all seven cases, the proximal dilatation of the bowel was found to be at a high position during the operation. Moreover, we found that the four children who underwent re-operation had serious scars at the original perineal surgery site and surrounding tissues. It was difficult to locate the external sphincter center point by electrical stimulation, and we finally completed the reconstruction surgery after combining with anatomical positioning (Table 2).
Finally, anorectoplasty was performed successfully in all seven cases. All seven cases were followed up for 0.5–4.0 years (M = 2.57 ± 1.26) after the definitive surgery. Six patients underwent regular outpatient follow-up, while one patient was followed up by telephone. During the follow-up, all seven patients had a seven-item bowel function score (BFS) and high-resolution anorectomanometry. Three cases also underwent contrast enema using barium.
There was no significant difference in the BFS between the different surgical approaches. Three patients who underwent only one operation had no obvious symptoms such as incontinence and constipation. However, the four patients who underwent more than two repair operations demonstrated a lower BFS. Among them, one patient had constipation, while the remaining two exhibited fecal incontinence. Their BFS values were only 8, 10, 8, and 14, which are far below the normal range (Table 2).
Regarding functional evaluation, the rate of constipation (as defined by the Rome III standard) was 14.3% (n = 1) and 7.0% (n = 5) (p = 0.44) in the SPF and NPF groups, respectively; however, this was not statistically significant. The rate of soiling (more than once per week) in the SPF group (n = 3, 42.8%) was higher than that in the NPF group (n = 5, 7.0%) (p < 0.05). The median BFS in the SPF group was significantly lower (SPF = 12.4, range: 8–18; NPF = 18, range: 16–20, p = 0.82), and there were fewer patients with normal BFS in the SPF group (SPF vs NPF = 42.9% vs 86%, p = 0.17) (Table 3).
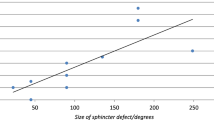
The median sphincter resting pressure in the SPF group was 23 mmHg (range: 21–26 mmHg), whereas in the NPF group it was 34 mmHg (range: 13–65 mmHg) (p = 0.10). Compared with the age-matched control group, patients in the NPF group had a normal sphincter resting pressure (SPF vs NPF = 0% and 72%, p < 0.05). There was no significant difference between the two groups with regard to the measurement of sphincter compression pressure (SPF = 50 mmHg, range: 29–68 mmHg; NPF = 56.3 mmHg, range: 13–115 mmHg, p = 0.59). However, RAIR was present in 0% (n = 0) and 50.7% (n = 36) of the patients in the SPF and NPF groups, respectively (p < 0.05) (Table 3).
Discussion
Perineal fistula is characterized by a slender perineal tube without nasal tube tissue. The definition of perineal fistula is undisputed and it is one of the most common anorectal malformations in pediatric surgery. However, the special type of perineal fistula (SPF) with a highly dilated colon is very rare and the number of cases reported in the literature is limited to date. In our patients with SPF, the dilated proximal colon was located in front of the iliac crest, which undoubtedly contributed to the complexity of the operation.
In this study, incidence of anorectal malformation with long perineal fistula was 8.97% (7/78). However, there were a few referrals of the long fistula type. So, the incidence should be lower. This incidence may reflect that surgeons often ignore to raise the importance of SPF. About 42.8% of all patients with SPF had spine syndrome of tethered cord which is far higher than NPF.
The diagnosis of perineal fistula is well recognized, and almost all neonates can be diagnosed at birth. A true perineal fistula is a narrow perineal orifice with no visible anal canal, and is located in the midline of the anal sphincter but is not completely surrounded by the sphincter mechanism9,10,11. In boys, the fistula is often found in the normal anal area and base of the scrotum. The fistula in girls is mostly located between the normal anal area and posterior labia. The clinical presentation of SPF is similar to that of a perineal fistula, but the position of the dilated colon is unlikely to be the same as in a normal perineal fistula. However, some surgeons do not perform a preoperative examination to get a correct understanding of the anatomical structure of these anorectal malformations, including the related fistula communication between the rectum and genitourinary tract. In our neonatal unit, all newborns with the anorectal malformation of a perineal fistula were screened by a distal colostogram to confirm the position of the distal rectum. We found that there was a special type of perineal fistula associated with a highly dilated colon. This special type of perineal fistula, if unrecognized preoperatively, may complicate surgical operations to repair anorectal deformities. Therefore, it is imperative that a thorough evaluation (e.g., distal colostogram) be performed to identify an SPF so that it can be correctly treated. There is a lack of consensus in the literature on the best imaging method for accurate anatomical diagnosis at birth. Some authors believe that perineal ultrasound is the best option, while others prefer MRI12,13. We believe that no matter which investigation is used to assess the anatomy of the anorectal malformation, preoperative evaluation is essential in children diagnosed with a perineal fistula to identify the possibility of a highly dilated colon. Therefore, we suggest a distal colostogram in the newborn period as well as a pelvic MRI to thoroughly evaluate the anatomy of the anorectal malformation.
Another important decision before surgery is to determine whether to transfer the patient to a center with extensive experience in pediatric surgery. Although there is no consensus on this point, there is strong evidence from adult studies that the surgeon’s technique is independently associated with better outcomes14,15,16. In some local hospitals, surgeons may lack awareness of anorectal malformations. Therefore, we recommend that if there is no pediatric surgeon available at a local hospital, patients should be transferred to a center with extensive pediatric surgery experience.
In most patients born with a SPF, management includes a diverting colostomy. Colostomy is valuable because it can avoid the complications of secondary colon dilation and pseudo-incontinence17. In our case series, all patients were managed with a diverting colostomy before the definitive repair.
Although it is the most straightforward anorectal malformation to repair18,19, perineal fistula remains a constant point of discussion. With regard to reconstructive surgery, it is essential to select an appropriate surgical approach that ensures optimal defecation function, as blind surgery can seriously affect the long-term defecation function. In this study, we introduced the procedure of correcting this abnormality using a posterior sagittal approach and laparoscopic approach, which can accurately expose the position of the distal rectum. These two approaches can avoid potential complications of a fistula, urethral injury, or intrasphincter anal dislocation.
Our postoperatively routine is to calibrate the anus 3 weeks after surgery and continue to expand it for several months every day. With regard to the postoperative outcome of anorectal malformation treatment, particularly regarding continence, it has been reported that 100% of the patients have bowel control in recto-perineal fistulas and the postoperative pain was also minimal3. In our study, 86% of the followed-up NPF patients were continent after the correction surgery at the end of the follow-up period. However, 57.1% of the SPF patients had abnormal bowel function, including constipation and fecal incontinence. Inadequate surgery, coupled with a natural propensity for constipation, can lead to severe fecal impaction that can cause substantial rectal dilation. This dilation can hamper rectal mobility and ultimately affect fecal control. In particular, when surgeons do not perform an adequate preoperative evaluation to accurately understand the anatomy of the anorectal malformation, including an associated fistulous communication between the rectum and the urogenital tract, it may affect the optimal surgical management. Due to this, patients may have to undergo multiple operations and may develop a defecation dysfunction. In our study, children who underwent more than two repair operations had lower BFS than those who had only one operation. In addition, the BFS in SPF patients was lower than that in NPF patients, although the difference was not statistically significant. Therefore, repeated operations and a highly dilated colon may be risk factors for abnormal defecation function in these patients. Although the majority of these patients can be managed with drugs, careful follow-up is vital (as with all patients who have anorectal malformations), so that the patients who need early management of their bowel function can be identified20.
Conclusions
In conclusion, this study reported anorectal malformation with long perineal fistula. Compared with NPF patients, the measurements of BFS and sphincter resting pressure on anorectal manometry were lower in SPF patients. To avoid a misdiagnosis, an anorectal perineal fistula should be examined by a distal colostogram before repair. Selecting an appropriate surgical approach is essential for ensuring optimal defecation function in these children as blind surgery can seriously affect the long-term defecation function.
Data availability
The data used to support the findings of this study are included within the article.
Change history
28 January 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41598-022-06056-3
Abbreviations
- SPF:
-
Special type of perineal fistula
- NPF:
-
Normal perineal fistula
- LAARP:
-
Laparoscopy assisted anorectoplasty
- PSARP:
-
Posterior aagittal anorectoplasty
- BFS:
-
Bowel function score
- RAIR:
-
Rectoanal inhibitory reflex
- PFO:
-
Patent foramen ovale
References
Rocourt, D. V., Kulaylat, A. S. & Kulaylat, A. N. Primary posterior sagittal anorectoplasty outcomes for rectovestibular and perineal fistulas using an accelerated pathway: a single institution study. J. Pediatr. Surg. 54(9), 1778–1781 (2019).
Bischoff, A., Martinez-Leo, B. & Peña, A. Laparoscopic approach in the management of anorectal malformations. Pediatr. Surg. Int. 31(5), 431–437 (2015).
Levitt, M. A., Bischoff, A. & Peña, A. Treatment of adults with unrecognized or inadequately repaired anorectal malformations: 17 cases of rectovestibular and rectoperineal fistulas. J. Pediatr. Adolesc. Gynecol. 26(3), 156–160 (2013).
Kraus, S. J., Levitt, M. A. & Peña, A. Augmented-pressure distal colostogram: the most important diagnostic tool for planning definitive surgical repair of anorectal malformations in boys. Pediatr. Radiol. 48(2), 258–269 (2018).
Rintala, R. J. & Lindahl, H. Is normal bowel function possible after repair of intermediate and high anorectal malformations?. J. Pediatr. Surg. 30(3), 491–494 (1995).
Kyrklund, K., Koivusalo, A. & Rintala, R. J. Evaluation of bowel function and fecal continence in 594 Finnish individuals aged 4 to 26 years. Dis. Colon Rectum 55(6), 671–676 (2012).
Jarvi, K. et al. Bowel function and gastrointestinal quality of life among adults operated for Hirschsprung disease during childhood: a population-based study. Ann. Surg. 252(6), 977–981 (2010).
Kumar, S. et al. Manometric tests of anorectal function in 90 healthy children: a clinical study from Kuwait. J. Pediatr. Surg. 44(9), 1786–1790 (2009).
Bischoff, A., Levitt, M. A. & Peña, A. Update on the management of anorectal malformations. Pediatr. Surg. Int. 29(9), 899–904 (2013).
Levitt, M. A. & Peña, A. Anorectal malformations. Orphanet J. Rare Dis. 2, 33 (2007).
Bischoff, A., Bealer, J. & Peña, A. Controversies in anorectal malformations. Lancet Child Adolesc. Health 1(4), 323–330 (2017).
Haber, H. P. et al. Transperineal sonography for determination of the type of imperforate anus. Am. J. Roentgenol. 189, 1525–1529 (2007).
Thomeer, M. G. et al. High resolution MRI for preoperative workup of neonates with an anorectal malformation: a direct comparison with distal pressure colostography/fstulography. Eur. Radiol. 25, 3472–3479 (2015).
Birkmeyer, J. D. et al. Surgeon volume and operative mortality in the United States. N. Engl. J. Med. 349, 2117–2127 (2003).
Birkmeyer, J. D. et al. Surgical skill and complication rates after bariatric surgery. N. Engl. J. Med. 369, 1434–1442 (2013).
Adam, M. A. et al. Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes?. Ann. Surg. 265, 402–407 (2017).
Levitt, M., Kant, A. & Peña, A. The morbidity of constipation in patients with anorectal malformations. J. Pediatr. Surg. 45(6), 1228–1233 (2010).
AbouZeid, A. A. & Mohammad, S. A. Lowtype anorectal malformations in the male: extent of deviation from the norm. J. Pediatr. Surg. 51, 1851–1858 (2016).
Whyte, C. et al. Anoplasty for low anorectal malformation. J. Pediatr. Surg. 10, 1602–1606 (2016).
Peña, A. Advances in the management of anorectal malformations. Am. J. Surg. 180(5), 370–376 (2000).
Acknowledgements
I am very grateful to my mentor, Dr. Jun Wang, for his careful guidance of my gradua-tion thesis in the past six months, which greatly improved my understanding of academic writing and taught me a lot of specific research skills. Thanks to the classmates who have given me care and support in life.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. Mr. S.L. conceptualized and designed the study, interpreted the data, and critically revised the manuscript. Prof. J.W. contributed to study design, interpreted the data, and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article, Sen Li was incorrectly listed as a corresponding author. The correct corresponding author for this Article is Jun Wang. Correspondence and request for materials should be addressed to wangjun@xinhuamed.com.cn. In addition, Jun Wang was incorrectly affiliated with ‘Department of Pediatric Surgery, Shanghai Children′s Hospital, Shanghai Jiao Tong University, No. 355, Luding Road, Shanghai, 200000, China’. Finally, the original version of this Article omitted an affiliation for Sen Li.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, S., Wang, J. Anorectal malformation with long perineal fistula: one of a special type. Sci Rep 11, 1706 (2021). https://doi.org/10.1038/s41598-021-81056-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81056-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.